This review aims to analyse the application of the measure methods and measure contents of the outcomes reported in studies on slowing myopia, and the associations between outcomes and study characteristics.
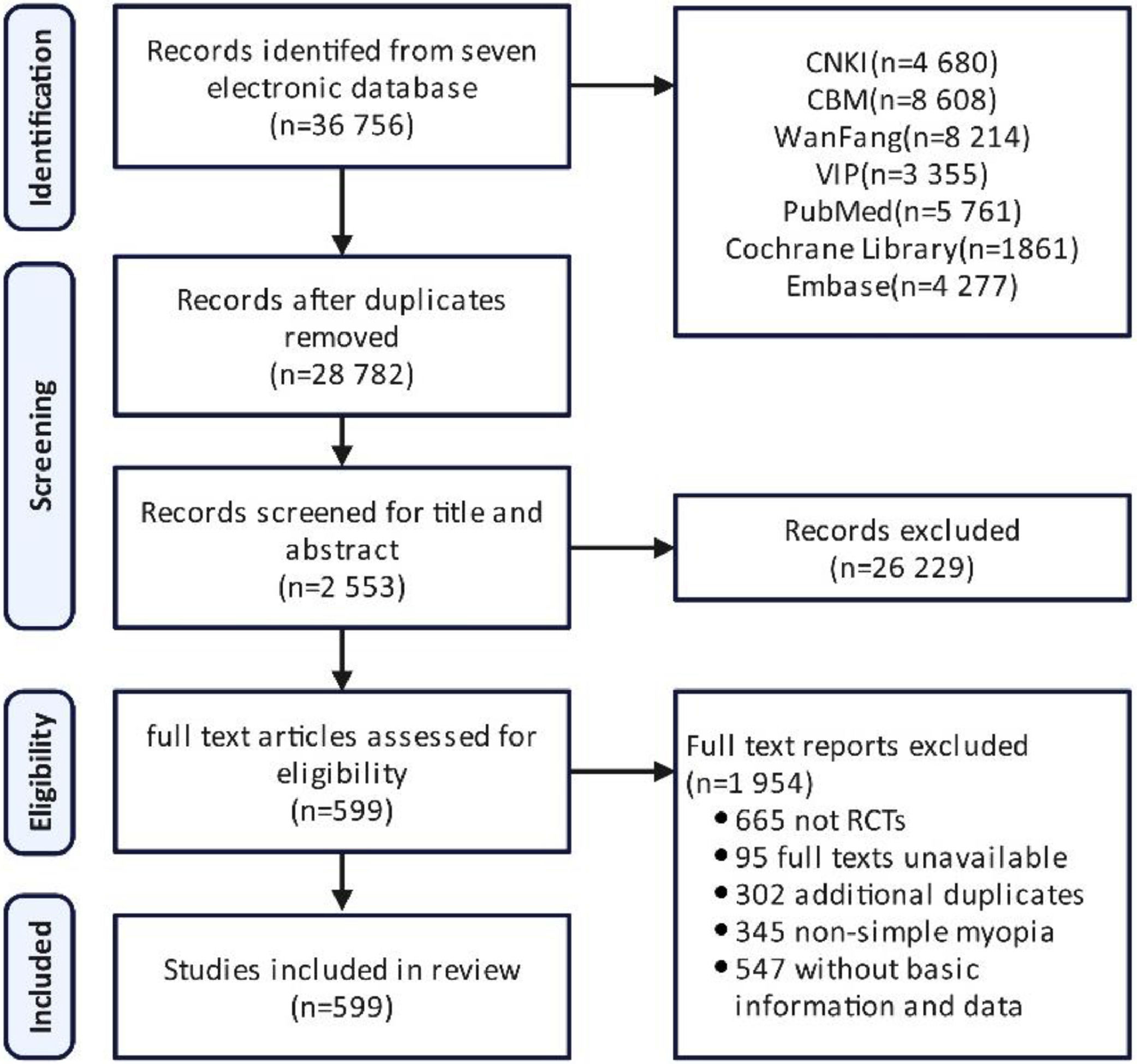
MethodsPublications were identified by a search of seven electronic databases including China National Knowledge Infrastructure, China Biology Medicine, Wanfang database, CQVIP database, PubMed, Cochrane Library and Excerpta Medica Database, for relevant terms like myopia and randomized controlled trial from construction to Sept. 15th, 2023. The basic information of studies was extracted, including publishing time, region, intervention duration, sample size, intervention and outcome. Additionally, the measurements of outcomes were explored. The risk of bias of all studies included were assessed.
ResultsAltogether, 599 randomized controlled trials were included, including vision (52.75 %), refraction (64.94 %), eye axial length (47.25 %) and response rate (38.23 %). Since 478 studies (79.80 %) were published in Chinese, the included studies were divided into subgroups according to the study language. The number of research published in Chinese was surged since 2005. The rate of refraction was gradually increased from 27.27 % before 2005 to 71.08 % in the past 2 years. 121 studies in English were included in this study. The usage frequency of refraction was ≥75 % in each period and that of eye axial length kept at more than half. In the studies lasting >6 months, the usage frequencies of refraction and axial length were >90 %. They accounted for 91.30 % and 82.61 % in the studies using contact lenses, and both 94.12 % in the studies using spectacles.
ConclusionMore and more attention is paid in slowing myopia, and the reported outcomes are diverse. Based on the analysis of the outcomes, there is a lack of an agreed-upon standardised set of outcomes in clinical trials for slowing myopia.
Myopia is a refractive error, refers to a condition where in the light entering the eye is focused in front of the retina when ocular accommodation is relaxed.1 It is a global public health problem,2 and particularly prevalent among the younger generation in East and Southeast Asia.3 The global prevalence of myopia is currently 33 % and it is still increasing, which is expected to reach approximately 50 % by 2050.2 Altogether, 95 %–99.5 % of myopic patients have non-pathological myopia,4 which is characterised by the absence of pathological change in the eye fundus, and slow progression.5 Interventions for myopia include optical procedures,6–9 medicine,10–14 environment (behaviour),15–18 surgical,19–21 complementary interventions as well as alternative medicine22 among others.
Randomised controlled trial (RCT) has been regarded as the gold standard for evaluating the efficacy of clinical diseases,23,24 and a large number of RCTs for slowing the progression of myopia have been conducted recently.25 The patient, intervention, comparison and outcome are four important elements in an RCT.26,27 The outcome is important for evaluating therapy, so the selection of appropriate outcomes is crucial when designing clinical trials to directly compare the efficacy of different interventions.28 However, the heterogeneity in the outcome selections of RCTs is commonly similar to studies on slowing myopia according to our previous research.29–31 This leads to difficulties in integrating studies to gain high-quality clinical evidence-based evidence, such as in systematic reviews and meta-analysis.30 Moreover, it is also necessary to establish an agreed-upon standardised set of outcomes for decreasing outcome heterogeneity.28–31
Therefore, our study aimed to perform a systematic review and create a comprehensive summary of outcomes previously reported in the RCTs. The basic study characteristics including publishing time, region, intervention duration, sample size, intervention type and outcome were extracted and counted. Additionally, we also sought to explore the associations among the reported outcomes and measurement of outcomes.
MethodsInclusion and exclusion criteriaThe studies were included if (1) the enrolled patients were diagnosed with myopia (myopia is the term referring to a condition in which the spherical equivalent refractive error of an eye is ≤−0.50 D when ocular accommodation is relaxed) without limitations of country, region, race, sex and age; and (2) they were RCTs.
Studies were excluded if they (1) were repeatedly published literature; (2) were animal experiments or other non-human clinical trials; (3) were unable to obtain full-text literature; (4) included patients were diagnosed with pathologic myopia with structural changes in the posterior segment of the eye (including posterior staphyloma, myopic maculopathy, and high myopia-associated optic neuropathy) or other retinopathies; (5) intervention measures were surgical; (6) had unclear diagnostic criteria; and (7) basic information and data of documents were incomplete or unavailable.
Patient and public involvementIt was not appropriate to involve patients or the public in the design, or conduct, or reporting, or dissemination plans of our research.
Search strategySeven databases including China National Knowledge Infrastructure, China Biology Medicine, Wanfang database, CQVIP database, PubMed, Cochrane Library and Excerpta Medica Database (EMBASE) were comprehensively searched. The retrieval time was from the establishment of the database to September 15th, 2023. The retrieval strategy was performed by combining title words with free words, and the logical combination of search words was adjusted according to the characteristics of each database. Retrieval strategy details could be found in Tables S1–S7 in the electronic supplementary material.
Study selectionAfter the removal of duplicates, two authors (Tianlin Wang and Wanying Xia) independently reviewed the titles and abstracts of all retrieved articles based on the inclusion and exclusion criteria. Full-text documents were reviewed and independently assessed for inclusion by the three reviewers (Nan Chen, Xuanling Zeng and Yiyang Xu). Three researchers solved problems in the article selection process through discussion. If the problem was still unsolved, further discordance was then settled by the senior author (Xingyue Yang).
Data extractionTo ensure that the participating authors were searching for similar results, we designed an information extraction form and pilot-tested a sample of 20 articles before formally extracting information, then we modified the form according to the situation. The three researchers (Nan Chen, Xuanling Zeng and Yiyang Xu) independently performed data extraction. Data were extracted relating to the aims of this review including intervention duration, outcomes, explanations of outcome measurements and time point were extracted.
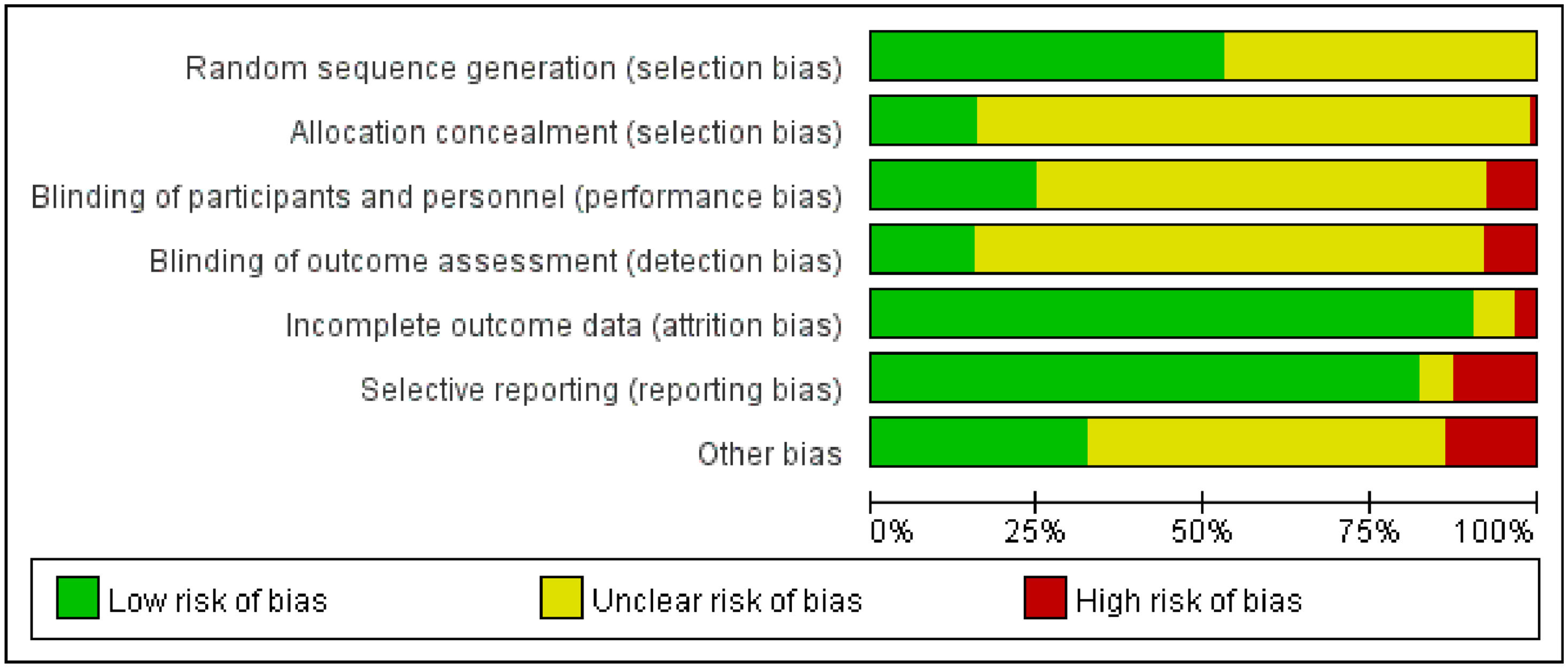
Risk of bias assessmentAll trials were assessed for the risk of bias using the Cochrane risk-of-bias tool for randomised trials (RoB 1.0). The tool was structured into the following seven domains: (1) selection bias arising from the random sequence generation; (2) selection bias in allocation concealment; (3) performance bias due to blinding of participants and personnel; (4) detection bias due to blinding of outcome assessment; (5) attrition bias due to incomplete outcome data; (6) reporting bias in selective reporting; and (7) other biases. The risk of bias for each study was independently assessed by three reviewers (Nan Chen, Xuanling Zeng and Yiyang Xu). If there were differences in the assessment results, the senior author (Xingyue Yang) would read the full text and make the final assessment again.
Statistical analysisTo reduce the selection bias, the included studies were classified into subgroups according to the study language. Descriptive analysis was carried out on the publication time, publication country, intervention duration, sample size, intervention type and application of outcomes of the studies included in each subgroup. Data was extracted in EXCEL (WPS Office 13.28.0, Kingsoft) and reported as n ( %). The figures were drawn using EXCEL (WPS Office 13.28.0, Kingsoft). The apriori algorithm was made on SPSS Modeller 18.
ResultsIncluded studiesThe literature search initially identified 36 756 citations. Following the removal of duplicate citations, 28 782 unique citations were identified. The titles and abstracts were reviewed for eligibility, with 26 229 citations excluded. Altogether, 599 studies were included for inclusion in the final analysis by reading the full text. The complete screening process is illustrated in Fig. 1.
Risk of bias of included studiesAltogether, 599 RCTs were assessed using the Cochrane risk-of-bias tool for randomised trials (RoB 1.0). Further details are shown in the methodological quality graph (Fig. 2). In the random sequence generation, 335 items (55.92 %) were assessed as having a low risk of bias. In the allocation concealment, 88 items (14.69 %) were assessed as having a low risk of bias and 5 items (0.83 %) were assessed as having a high risk of bias. Among the studies with blinding of participants and personnel, 130 items (21.70 %) were assessed as having a low risk of bias and 34 items (5.68 %) were assessed as having a high risk of bias. Altogether, 112 items (18.70 %) were assessed as having a low risk of bias and 35 items (5.84 %) were assessed as having a high risk of bias in the blinding of outcome assessment. In the incomplete outcome data, 560 items (93.49 %) were assessed as having a low risk of bias, and 15 items (2.50 %) were assessed as having a high risk of bias. In selective reporting, 527 items (87.98 %) were assessed as having low risk of bias, and 55 items (12.59 %) were assessed as having a high risk of bias. In other biases, 145 items (24.20 %) were assessed as having a low risk of bias, and 58 items (9.68 %) were assessed as having a high risk of bias.
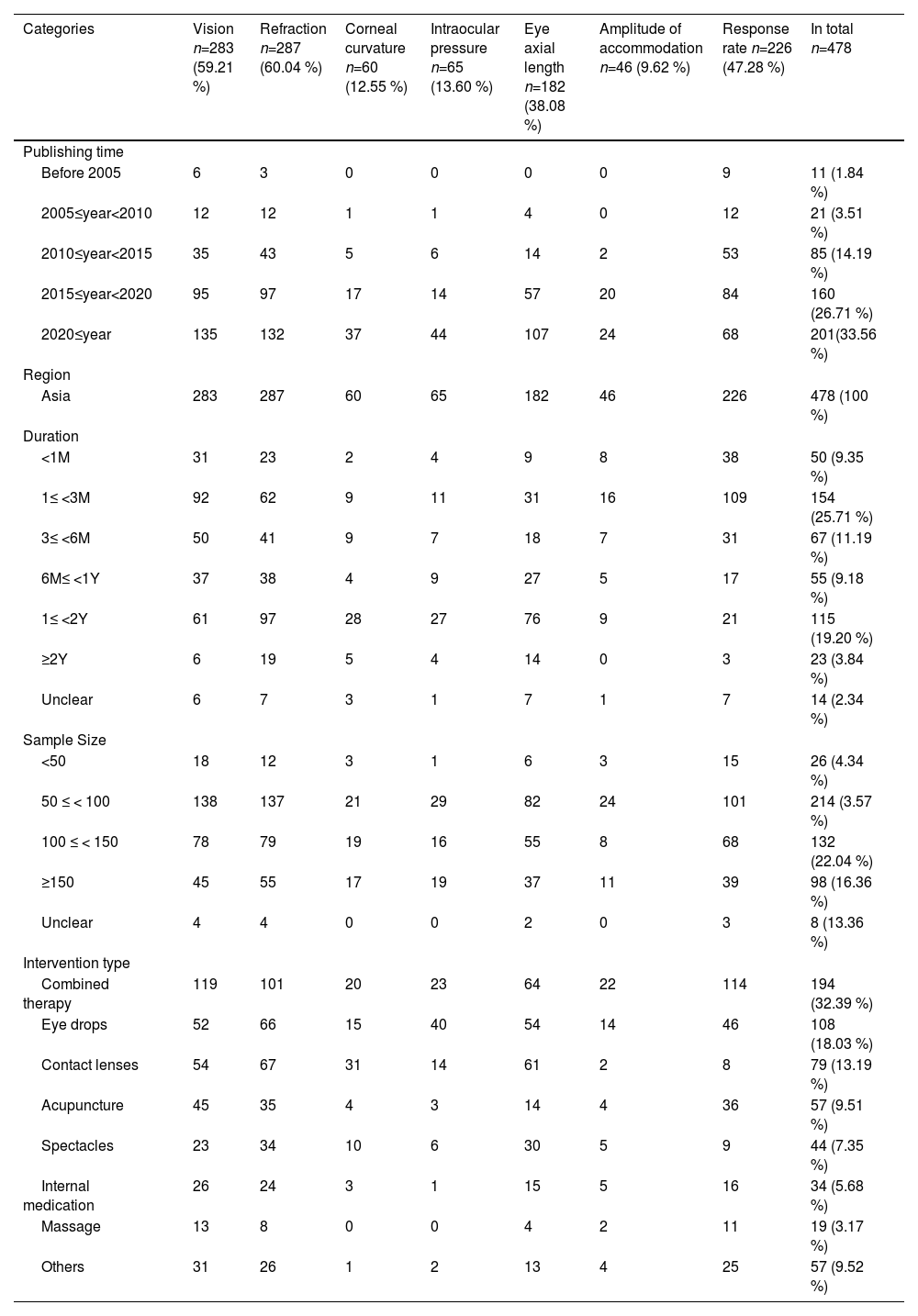
The basic study characteristicsThe basic study information including publishing time, region, intervention duration, sample size, intervention type and outcome was extracted and counted. All the detailed information obtained from 599 RCTs is shown in Table S8 in the electronic supplementary material. According to the study characteristics, all these studies were classified into five discussion dimensions. We selected the seven commonly used outcomes as the horizontal classification, including vision (n = 316; 52.75 %), refraction (n = 389; 64.94 %), corneal curvature (n = 83; 13.86 %), intraocular pressure (n = 79; 13.19 %), eye axial length (n = 283; 47.25 %), amplitude of accommodation (n = 59; 9.85 %), response rate (n = 229; 38.23 %). Adverse event (n = 159; 26.54 %) and compliance (n = 26; 4.34 %), which are important outcomes of reaction safety and reliability, had also been extracted and counted. Since 478 studies (79.80 %) were published in Chinese, the included studies were divided into two subgroups according to whether the study language was Chinese or English when analysing the specific data in the Tables 1–2.
The basic study characteristics of the outcomes of studies in Chinese.
The basic study characteristics of the outcomes of studies in English.
In the studies published in Chinese, approximately 91.11 % of the studies were published in the recent decade, and this number had been increasing. Since 2005, the number of studies surging in 2010–2014 years, the increase was approximately four-fold that in 2005–2019 years, and in 2015–2019 years, this was approximately twice that in 2010–2014 years. Refraction was the most used outcome in 389 studies (64.94 %). The frequency of this outcome has gradually increased from 27.27 % before 2005 to 71.08 % in the past 2 years. Compared with the period from 2015 to 2019 and the past 2 years, the use of eye axial length had increased significantly, from 35.625 % to 54.21 %. Altogether 229 (38.23 %) studies used the response rate as the outcome, but the usage frequency of this outcome has gradually decreased from 81.82 % before 2005 to 42.17 % in the past 2 years.
In the studies published in English, approximately half of the studies were published in the past 5 years, and this number had also been increasing. As the most used outcome, the usage frequency of refraction was ≥75 % in each period. The usage frequency of eye axial length has also been maintained in more than half of the studies, with the highest usage frequency of 94.74 % observed in the past 2 years. In the past 10 years, the response rate has not been used as an outcome.
RegionsAll the studies published in Chinese were distributed in China and Asia. The frequencies of vision and refraction were both >50 % (52.75 % and 64.94 % respectively), with refraction showing the highest rate of usage. The usage of eye axial length as study outcome was also observed in one-third of the studies.
In the studies published in English, they were mainly distributed in Asia (n = 87; 71.90 %) and North America (n = 18; 14.88 %). In the studies distributed in Asia, the usage frequency of refraction was as high as 96.42 %, and that of eye axial length was as high as 89.29 %, and that of these two outcomes in Europe, Oceania, and South America was 100 %. Only 3 studies used the outcome of response rate outcome.
DurationThe study duration ranged from immediate to 4 years. The duration of the Chinese studies was mainly concentrated in 1 to 3 months (n = 154; 25.71 %) and 1 to 2 years (n = 115; 19.20 %), and it of the English studies was mainly concentrated in 1 to 2 years (n = 40; 33.06 %) and >2 years (n = 56; 46.28 %).
In studies published in Chinese, the usage frequency of response rate decreased with the increase in intervention time, from 80.49 % in studies with a duration of <1 month to 10 % in studies with a duration of more than 2 years. The usage frequencies of vision, refraction and eye axial length were the highest in the study with duration of 3 to 6 months, 6 months to 1 year and 1 to 2 years at 70.73 %, 70.73 % and 66.28 %, respectively.
In the studies published in English with a duration of >6 months, refraction and eye axial length were the most important outcomes, and the usage rates were > 90 %. In the study with a duration of >2 years, they reached 97.56 % and 95.12 % respectively.
Sample sizeThe studies to be included in this review were divided into five categories according to the sample size: <50, 50 to 100, 100 to 150, >150 and unclear. In the studies published in Chinese, >95 % studies had >50 samples, and the studies with a sample size of 50–100 accounted for 35.72 % of the studies. In the studies published in English, the studies with a sample size of >150 were the most common, accounting for 42.98 % of the studies.
InterventionThe interventions in the studies included combined therapy, eye drops, contact lenses, acupuncture, spectacles, internal medicine, massage, and other therapies, with rates of 34.56 %, 23.87 %, 21.04 %, 9.52 %, 10.18 %, 5.84 %, 3.17 % and 12.19 %, respectively.
In all studies published in Chinese, the studies with combined therapy as the intervention type were the most common (n = 194; 32.39 %). The frequencies of vision used as study outcome in studies utilising contact lenses and eye drops were the highest, both reaching 19.08 %, whereas, in studies using massage, it was the lowest at only 4.59 %. The studies utilising contact lenses (n = 67; 23.34 %) and eye drops (n = 66; 22.30 %) were more likely to use refraction as the study outcome. Compared with studies using other intervention types, studies using eye drops (n = 14; 30.43 %) were more likely to use intraocular pressure as the study outcome. Studies using combined therapy (n = 114; 50.44 %), eye drops (n = 46; 20.35 %) and acupuncture (n = 36; 15.93 %) preferred to use response rate as the outcome.
Among the studies published in English, none used acupuncture or massage as the intervention, and only one study used internal medications. The interventions of the studies mainly included contact lenses (n = 47; 38.84 %), eye drops (n = 35; 28.93 %) and spectacles (n = 17; 14.05 %). The studies in English mainly selected two outcomes, refraction and eye axial length. The usage frequencies of the refraction and eye axial length in those studies using eye drops, contact lenses, and spectacles were 27.45 % and 39.22 %, 23.76 % and 41.58 % respectively.
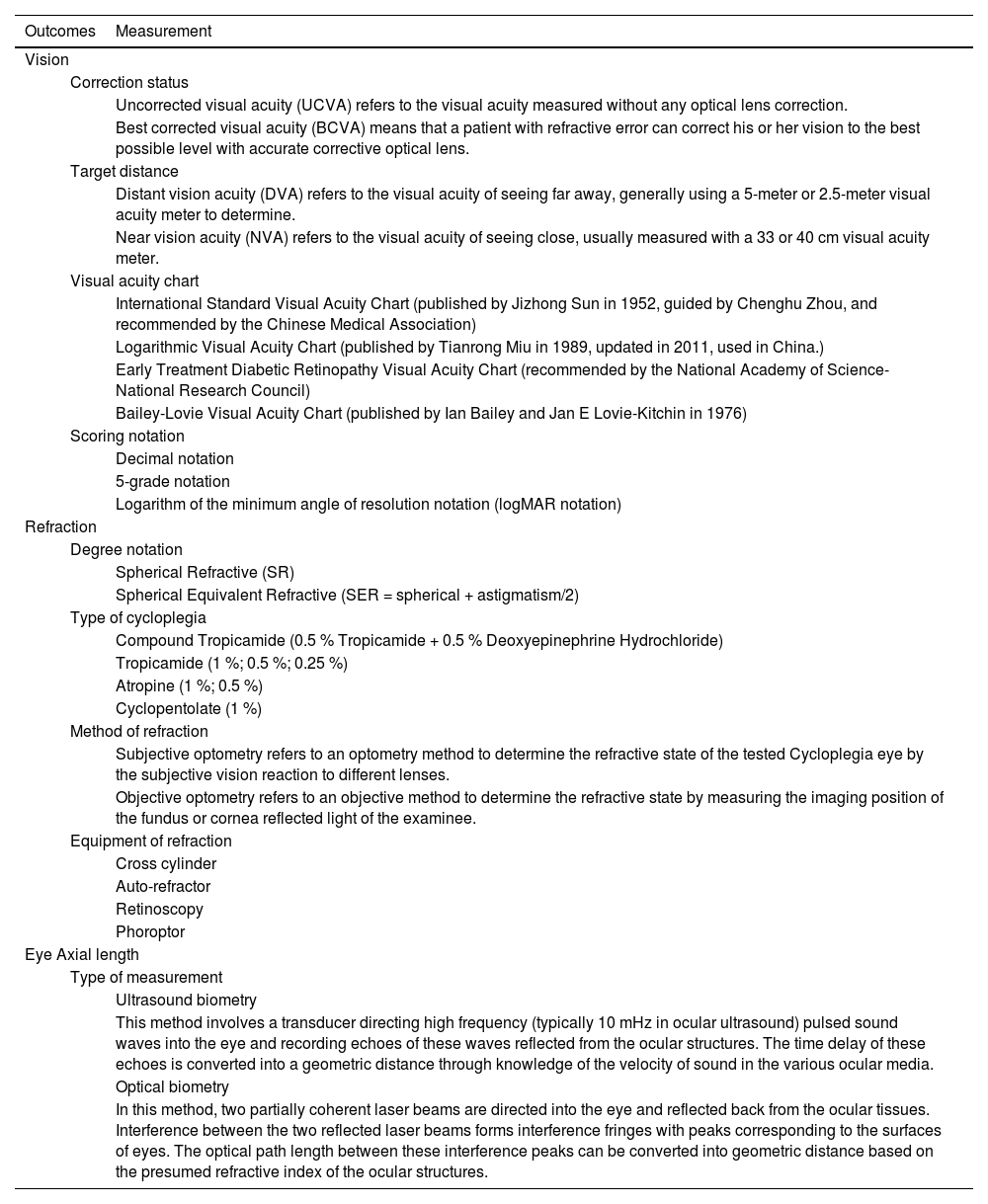
Outcome measurementAmong 599 studies, the measurement methods of vision (n = 316), refraction (n = 389) and eye axial length (n = 283) included multiple dimensions. When measuring vision, the dimensions of measurement included the state of vision, the distance to measure, the type of visual acuity chart used and the scoring notation for vision. The degree notation, type of cycloplegia, method and equipment of refraction were diverse for measuring refractive error. Moreover, for eye axial length, the measurements were classified into ultrasound biometry and optical biometry. Table 3 lists the outcome measures used in the included studies.
Measurements of the main outcomes.
In previous studies, due to the undefined mechanisms of myopia and the diversity of interventions, the effectiveness of interventions has been evaluated by various outcomes. This situation leads to difficulties in conducting meta-analyses of different studies for forming high-quality clinical evidence-based evidence. Moreover, adverse events and compliance were both important for assessing the safety and reliability of a clinical intervention. They should be clearly and comprehensively reported in the literature according to the Consolidated Standards of Reporting Trials’ (CONSORT) reporting guidelines.32 However, adverse events, including dry eyes, eye soreness, visual abnormalities, corneal injury, conjunctivitis and other adverse symptoms, were recorded in only 156 (26.04 %) studies, whereas compliance was used in only 25 (4.17 %) studies. According to our study data of this study, we believe that researchers should pay more attention to these two outcomes and report them.
Association between outcomes and study characteristicsWe analysed the relationships between the applications of outcomes and study characteristics, including publishing time, intervention duration and intervention methods. Given that 478 studies (79.80 %) were published in Chinese, the included studies were divided into subgroups according to the study language. In general, the number of studies on slowing myopia has surged since 2005, and this phenomenon and trend may be related to the increase of the global myopia morbidity.2 Socioeconomically, refractive errors, particularly if uncorrected, can affect school performance, limit employability and impair an individual’s quality of life. Thus, myopia has been widely valued and researched worldwide. The absolutely dominant distribution area of the studies is Asia, which may be related to the fact that Asia especially East Asia has the highest myopia rate.3 Outdoor time has been proven to be the strongest environmental factor that can delay myopia onset, whereas near-work was a risk factor for myopia. It has been suggested that a probable causative role in the development of myopia is the competitive and stressful education system leading to less outdoor time and more near work in some East Asian countries.33
According to clinical myopia control trials and instrumentation report by the International Myopia Institute (IMI), the minimum length of a clinical trial was 3 years, with the third year being the period without treatment (or with only a control treatment) to assess the effectiveness and rebound effect of treatments for slowing and controlling myopia.34 The intervention duration of the included studies ranged from immediate to 4 years, and the treatment duration in only 79 (13.19 %) studies was >2 years. Besides, studies with short intervention duration tended to use response rate and vision as outcomes, whereas long-duration studies were more likely to use eye axial length and spherical equivalent refraction. Combined with the IMI standard intervention duration, a range of structural and functional aspects of the eye, such as eye axial length, tends to require longer interventions compared to improvements in visual acuity and visual fatigue symptoms contained by response rate. Studies, in humans and animal models, has shown that this increased eye axial length is predominantly a consequence of increased vitreous chamber depth, which was a more stable structural change and not easy to affect.35,36 Future research should take a longer period of at least two years of treatment and 1 year of follow-up to assess the effect and rebound effect of the interventions.
Combining the statistics of all reported outcomes and the association between them and intervention types, we found that there was a high frequency of response rate in studies published in Chinese, which was a composite outcome for more intuitive clinical effectiveness, including vision acuity, refraction and visual fatigue level.37 This was mainly reported in the studies using acupuncture and massage, because these two intervention methods that stimulate the acupoints around the eyes could improve the sympathetic nerve excitability, regulate the extra ocular muscles, pupil sphincter and other muscles, and relieve the spasm of the ciliary muscle.38 Therefore, they may alleviate visual fatigue to a large extent. However, after deeper exploration, we found that it may be too general, subjective and varied to objectively reflect their effectiveness. The studies published in English that utilised eye drops, contact lenses and spectacles more commonly used eye axial length,39 spherical equivalent refraction and concrete indicators as outcomes which could more objectively to show the progression of myopia. Because these interventions are more likely to affect the changes in eye structure, more attention should be given to slow myopia from the perspective of the myopia mechanism.40 But these outcomes perhaps lead to heterogeneity of assessing efficacy. We believe that the two approaches, using the response rate or using concrete indicators such as eye axial length, should be applied in combination, considering the strengths of each indicator.
In general, from the current outcomes in the included study, we found that the effective clinical outcomes for evaluating the prevention and control of myopia were lack of agreement and were confusing, which was not conducive to the development of clinical trials. Further classification of the core outcome indicators would help in the development of clinical trials in the future. Additionally, axial length measured by optical biometry and refractive error under cycloplegia were strongly recommended by IMI to be assessed as the primary outcomes in myopia control studies.34 Other secondary and exploratory outcomes were also suggested to be reported for different purposes.34
Outcome measurementIn the specific analysis, we found that the measurements of outcome were diverse among the studies. In fact, many researchers were vague about or avoided them. More than 60 % of the studies included used visual acuity as an outcome. Factors to be considered when measuring visual acuity include which correction method to choose, target distance, visual acuity chart and visual acuity representation to use.41 There are considerable differences in the presentation of vision measurements (logMAR and decimal records are easily confused). However, many studies included in the present review neglected the detailed description of visual acuity chart and visual acuity testing methods. Since vision testing methods have a great impact on vision results, sufficient details of the process should be provided in the study according to the CONSORT reporting guidelines, so that other researchers can obtain the same results.34
The measurements of refraction and eye axial length also changed over the years. In the analysis, 6017 right eyes of children aged 4–15 years found that the non-cycloplegia was (0.63 ± 0.65) D more myopic than the ciliary paralysis optometry in the direction of myopia. These results suggest that non-cycloplegia optometry would overestimate the degree of myopia in children.42 However, <30 % of the included studies clearly reported refraction with cycloplegia when it was measured. Additionally, the most commonly used myopia screening methods are uncorrected visual acuity examination and non-cycloplegia paralysis refraction examination at present.43 Spherical equivalent refraction has gradually replaced spherical refractive as a more rigorous outcome. The algorithm of spherical equivalent refraction is a spherical dioptre plus half of the cylindrical dioptre, and cylindrical diopre, which refers to the degree of astigmatism.
Simultaneously, the occurrence and development of myopia are usually caused by excessive growth of the eye axial length,44 and many studies have confirmed that the length of the eye axis is closely associated with refractive error.45,46 The measurement of individual eye axial length changes has been gained importance as a major even primary outcome in myopia clinical trials over time.
Strengths and limitationsThe strength of this study was the Chinese and English RCTs on slowing myopia were comprehensively and systematically searched and included the analysis. This review included a rigorous data extraction process, with predefined outcome categorization. Moreover, there was an assessment of study characteristics that may influence the interpretation of outcomes, and changes in outcomes over time were assessed. Therefore, our study could not only show the status of the reporting outcomes, but also reflect the trend in the change of indicator application.
However, this review still has several limitations. Firstly, only a few included studies had a treatment duration of more than 2 years and follow-up time information was not extracted, which limited the analysis of long-term effects. Secondly, approximately 90 % of the included articles were published in Asian countries and approximately 84 % of the included RCTs were published in Chinese, which partially limit the generalisability of the study findings. Third, in the process of assessing the risk of bias for each research, there were some unclear points. We have not contacted the corresponding author of the study by email or telephone to make a more accurate assessment. Fourth, the criteria and examination techniques for myopia diagnosis have not been standardised across countries and practices, and the included studies showed inconsistencies in their diagnostic standards. Future studies should consider further standardisation of the diagnostic criteria and generalisability of the study results through the inclusion of participants of different ethnic groups, longer observation durations, and use of standardised guidelines for myopia diagnosis, such as those proposed by the IMI.1
Implications for future researchOur results suggest a lack of consensus that outcomes should be reported when evaluating the non-surgical intervention of slowing myopia. Future studies will reduce our comprehensive list to a smaller core set of important outcomes, which could then be measured and reported by future investigators. Standardising outcomes in this way could reduce reporting bias and improve reproducibility and external validity. Besides, it could also aid in evidence synthesis into meta-analysis and help guide clinical decision-making going forward.
ConclusionMore and more attention is paid in slowing myopia, and the reported outcomes are diverse. Based on the analysis of the outcomes, there is a lack of an agreed-upon standardised set of outcomes in clinical trials for slowing myopia.
Ethics approval and consent to participateNot applicable.
Consent for publicationNot applicable.
Funding sourcesThis work was supported by the National Natural Science Foundation of China [Grant Numbers 81,904,063 to XYY] and Key Discipline of High-level Acupuncture of the National Administration of Traditional Chinese Medicine [zyyzdxk-2023254].
Author contributionsYiyang Xu, Nan Chen and Xingyue Yang contributed to the study conception and design. Literature review, analysis, and chart making were performed by Yiyang Xu. Nan Chen, Fei Zhang, Xuanling Zeng, Tianlin Wang and Wanying Xia. The draft of the manuscript was written by Yiyang Xu, Nan Chen and Xingyue Yang. All authors read and approved the final manuscript.
Availability of data and materialsThe datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
RegistrationThe review was not registered.
The authors have no conflicts of interest to declare.
All authors hereby express their gratitude to www.enago.cn for external language editing services.