While there are numerous studies comparing open-view autorefractors to subjective refraction or other open-view autorefractors, most studies between closed and open-view autorefraction tend to focus on children rather than young adults. The aim of this study was to determine the concordance in non-cycloplegic refractive error between two modern objective autorefractors: the closed-view monocular Topcon TRK-2P and the binocular open-view Grand Seiko WR-5500.
MethodsFifty young adults aged 20–29 years (mean age 22 ± 1.6 years) underwent non-cycloplegic autorefraction using the Grand Seiko WAM-5500 (open view) and Topcon TRK-2P (closed-view) autorefractors on both eyes. Findings were expressed as the isolated spherical component and were also converted from clinical to vector notation: Mean Spherical Error (MSE) and the astigmatic components J0 and J45.
ResultsMean MSE ± SD was −1.00 ± 2.40D for the Grand Seiko WAM-5500 compared to −1.23 ± 2.29D for the Topcon TRK-2P. Up to seventy-six percent of the cohort had mean spherical errors from the Topcon TRK-2P which fell within ±0.50D of the Grand Seiko reading and 58% fell within ±0.25D. Mean differences between the two instruments were statistically significant for all components (J0, spherical, and MSE) (p < 0.01), except J45 (p > 0.05).
ConclusionsThe differences in non-cycloplegic MSE between these two instruments are small, but statistically significant. From a clinical perspective the Topcon TRK-2P may serve as a useful starting point for subjective refraction, but additional work is needed to help further minimise differences between the instruments.
In the late 1930s, Collins described the design of an ‘electronic refractionometer’ which he proposed would, through use of infra-red light, measure refractive error with minimal operator influence.1 It took approximately a further 20 years for such an instrument to become commercially available.2 Since those early models, autorefractors have progressed in design and availability3–9; and while subjective refraction remains the gold standard, autorefraction has firmly established a vital ancillary role within optometric and ophthalmological clinical and research settings.
Closed-field autorefractors with internal fixation targets, typically found in clinical practice, are generally inexpensive, and widely available in a range of models. Within research settings, particularly in the areas of refractive error and ocular accommodation, open-view autorefractors, with external fixation targets, such as the Shin Nippon or Grand Seiko models are generally advocated.10 When an appropriate distant fixation target is used, and fixation maintained, the use of open-view binocular autorefractors can reduce the risk of proximal accommodation.4
Viewing through such open-view binocular autorefractors is considered a more natural task which permits a ‘real world’ situation within a laboratory or clinical setting.3 Open-view instruments also allow measurements to be obtained while presenting accommodative targets and can be adapted to facilitate peripheral refractive measurements.11 Measurements recorded using various iterations of the popular instruments such as the Shin-Nippon and Grand Seiko open-view autorefractors have generally compared favourably to subjective refraction in adults,3,4,12 and cycloplegic refraction and measurements in children.13,14
While there are numerous studies comparing open-view autorefractors to subjective refraction or other open-view autorefractors,3–5,15 most studies between closed and open-view autorefraction tend to focus on children rather than young adults.7,14 Furthermore, studies in this field are generally of limited use once the autorefractor in question ceases to be commercially available.16
Whilst open-view autorefractors continue to retain a role in child refractive error research, it is less clear whether there is a need to maintain use of open-view autorefractors to investigate refractive error in young adults i.e. individuals who are likely to have lower levels of accommodation compared to young children, but significantly more than early presbyopes. The aim of this study was to determine the concordance in non-cycloplegic refractive error between two modern, objective autorefractors: the closed-view monocular Topcon TRK-2P and the binocular open-view Grand Seiko WAM-5500. We hypothesise that due to the lower levels of accommodation found in young adults compared to children there will be a high degree of agreement between the two techniques. A secondary aim was to determine whether a simple correction factor can be applied to the estimates of refractive error to render the two measurements equivalent. Establishing whether results from closed- and open-view autorefraction are interchangeable would open up the possibility of combining datasets from multiple studies where different instrumentation has been used. Interchangeability may also broaden the scope for practice-based research where there may be limited availability of open-view autorefractors.
Materials and methodsParticipantsTo increase the likelihood of including only adults with active accommodation, exclusion criteria limited the age range to 18–40 years and excluded those with a history of ocular surgery. All contact lenses were removed prior to obtaining measurements.
The study adhered to the tenets of the Declaration of Helsinki and was granted approval by the departmental ethics committee. All participants provided informed consent prior to participation.
Instrumentation and procedureThe Grand Seiko WAM-5500 binocular open-view infra-red autorefractor was used to obtain non-cycloplegic refractive error measurements on both eyes of participants. The measurement range extends ±22D for the spherical and ±10D for cylindrical measurements. A non-accommodative white spotlight at a distance of 6 m was used to aid fixation and a minimum of three readings were taken for each eye.
The process was repeated using the Topcon TRK-2P (closed-view) autorefractor, with participants instructed to fixate on the internal picture fixation target. The autorefractor employs an auto fogging system and what is referred to by the manufacturer as ‘rotary prism technology’. While the manufacturer’s specification did not provide detailed descriptions, an earlier paper described the Topcon KR-8000 model as using a Badal system that was first focussed in one meridian and then measurements taken through 180° using a rotating prism system.16 The manufacturer’s specifications advise the refractive measuring range as −30D to +25D for the spherical component and ±12D for the cylindrical component. Three readings were obtained per eye.
Both autorefractors had recently been checked for calibration, and any appropriate corrections were made (an undercorrection of myopia by −0.25 dioptres (D) by the Grand Seiko for the spherical component only). To maximise equivalence between procedures, vertex distance was set at 12 mm for both instruments. Measurement increments were set at 0.01D for the Grand Seiko and 0.25D for the Topcon.
Clinical measurements were then expressed as vector components (as described by Thibos et al.)17: Mean Spherical Error (MSE), J0 (orthogonal) and J45 (oblique) astigmatism.
Statistical analysisThe Shapiro–Wilk test showed that not all data were normally distributed, thus the Wilcoxon signed-rank test was used to test for statistical differences between the open- and closed-view autorefractors. Power statistics revealed that a sample size of 45 was needed to detect a standardized difference of 0.40, using 80% power at 5% significance level. This calculation was based on an estimated significant mean difference in sphere or MSE of 0.25 with group SDs of 0.62D. Statistical significance was accepted at the 95% confidence level (p < 0.05). Mean-difference, Bland-Altman, plots evaluated the agreement between the instruments.18
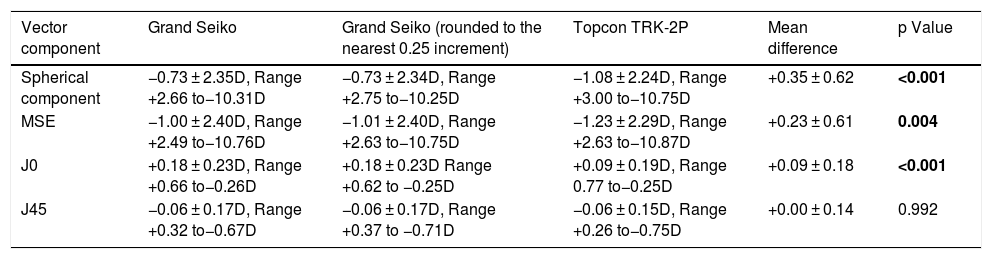
ResultsAs the Grand Seiko increments were set to 0.01D and the Topcon TRK-2P to the nearest 0.25D, data from the Grand Seiko were also rounded to the nearest 0.25D and analysed separately (see Table 1). Unless indicated otherwise, Grand Seiko data measured to the nearest 0.01D are presented below.
Summary of average MSE, J0, and J45 vector components (mean ± standard deviation in D) using each instrument, rounded to the nearest 2 decimal points. Statistical significance is presented in bold.
| Vector component | Grand Seiko | Grand Seiko (rounded to the nearest 0.25 increment) | Topcon TRK-2P | Mean difference | p Value |
|---|---|---|---|---|---|
| Spherical component | −0.73 ± 2.35D, Range +2.66 to−10.31D | −0.73 ± 2.34D, Range +2.75 to−10.25D | −1.08 ± 2.24D, Range +3.00 to−10.75D | +0.35 ± 0.62 | <0.001 |
| MSE | −1.00 ± 2.40D, Range +2.49 to−10.76D | −1.01 ± 2.40D, Range +2.63 to−10.75D | −1.23 ± 2.29D, Range +2.63 to−10.87D | +0.23 ± 0.61 | 0.004 |
| J0 | +0.18 ± 0.23D, Range +0.66 to−0.26D | +0.18 ± 0.23D Range +0.62 to −0.25D | +0.09 ± 0.19D, Range 0.77 to−0.25D | +0.09 ± 0.18 | <0.001 |
| J45 | −0.06 ± 0.17D, Range +0.32 to−0.67D | −0.06 ± 0.17D, Range +0.37 to −0.71D | −0.06 ± 0.15D, Range +0.26 to−0.75D | +0.00 ± 0.14 | 0.992 |
Fifty young-adults aged 20–29 years (mean age 22 ± 1.6 years) were recruited from a university staff-student population. A Wilcoxon signed-rank test for Grand Seiko measurements, and separately for Topcon TRK-2P measurements, did not reveal any statistically significant inter eye differences (p > 0.05 for both instruments). Right eye data are presented.
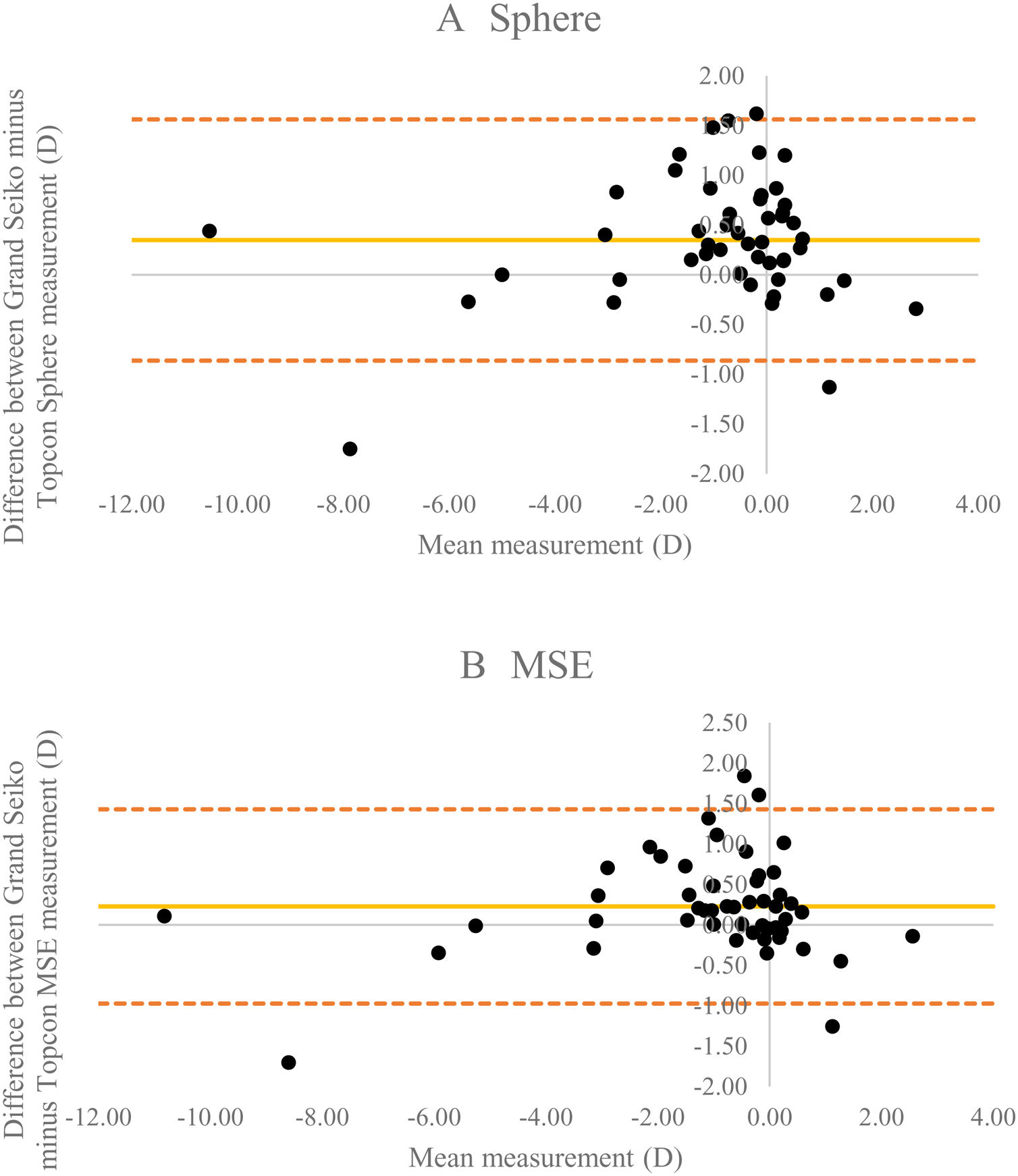
Spherical componentThe average spherical component measurements (in D ± standard deviation [SD]) for 50 right eyes was −0.73 ± 2.35D with the Grand Seiko and −1.08 ± 2.24D with the Topcon TRK-2P (see Table 1). Differences between instruments were statistically significant (p < 0.01) with a mean difference of 0.35 ± 0.62D (see Fig. 1 and 2A). Thirty-eight participants (76%) were found to have readings which were either identical or more hyperopic with the Grand Seiko compared to the Topcon TRK-2P. Sixty percent of the participants had readings from the Topcon TRK-2P which fell within ±0.50D of their Grand Seiko reading and approximately 32% within ±0.25D of one another if Grand Seiko measurements rounded to the nearest 0.01D were used. Seventy percent of the participants had readings from the Topcon TRK-2P which fell within ±0.50D of the Grand Seiko reading and 50% within ±0.25D of one another if rounding Grand Seiko measurements to the nearest 0.25D. Despite the increase in agreement due to rounding measurements to 0.25D with the Grand Seiko, significant differences remained for the spherical component.
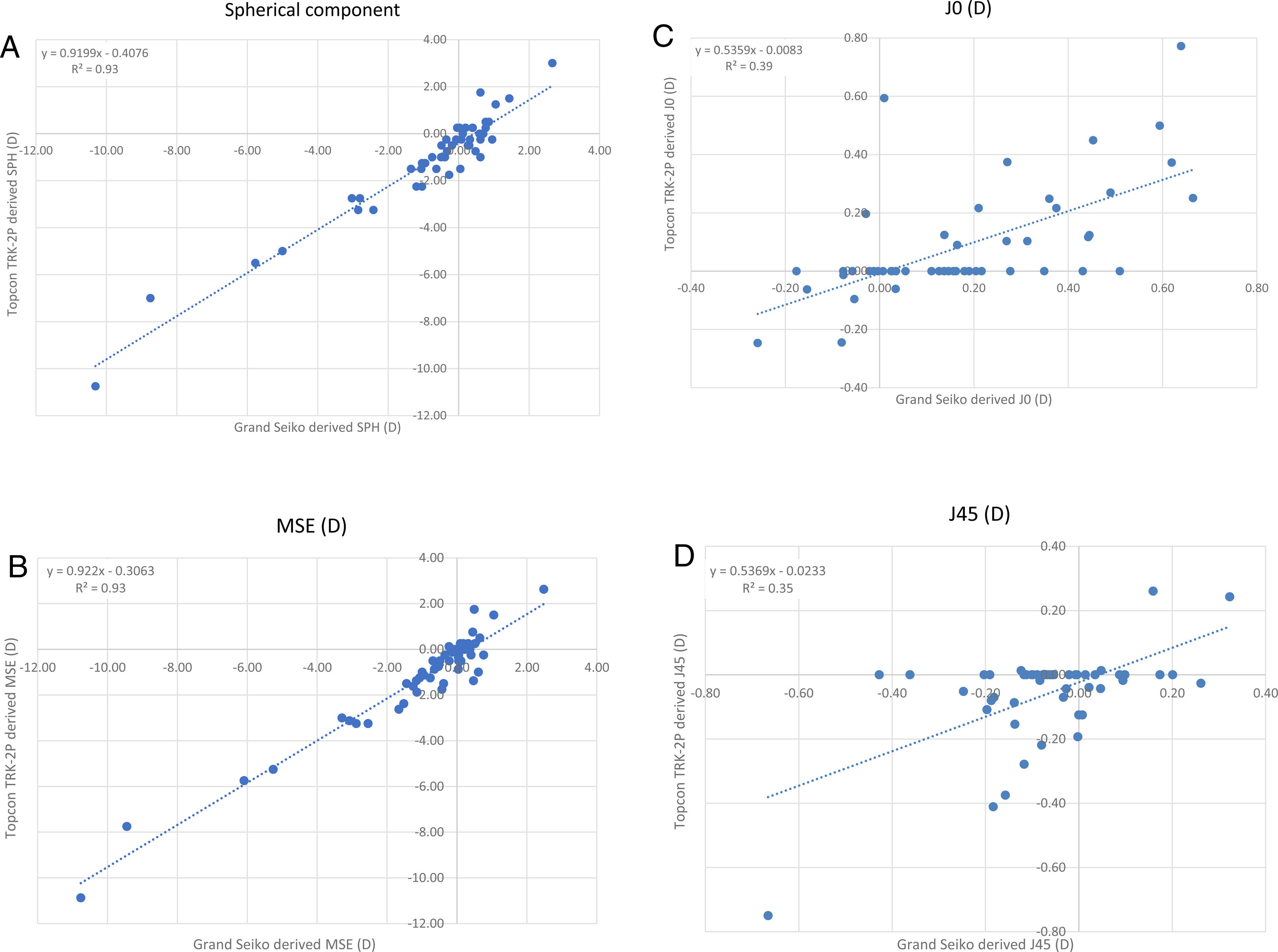
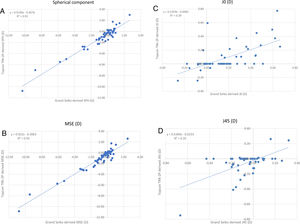
Scatterplots for the Spherical component (A) Mean Spherical Error (MSE) (B) J0 (C) and J45 (D) (Grand Seiko to nearest 0.01D). (A) Closed versus open view autorefractor spherical component results. (B) Closed versus open view autorefractor MSE results. (C) Closed versus open view autorefractor J0 results. (D) Closed versus open view autorefractor J45 results.
The two sets of measurements were significantly correlated (r = 0.96, p < 0.001) (see Fig. 1A).
Mean Spherical Error (MSE)Mean MSE ± SD was −1.00 ± 2.40D for the Grand Seiko compared to −1.23 ± 2.29D for the Topcon TRK-2P, a difference which was statistically significant (p = 0.004; see Table 1 and Fig. 2B).
Measurements obtained using the Grand Seiko were, on average, more hyperopic, although this was not the case for all participants (see Fig. 2B); seventeen participants (34%) were found to be more myopic using the Grand Seiko compared to the Topcon TRK-2P. For the MSE component, 70% of participants had readings from the two autorefractors which fell within ±0.50D of one another and 46% within ±0.25D of one another if Grand Seiko measurements to the nearest 0.01D were used. Seventy-six percent of the participants had readings from the TRK-2P which fell within ±0.50D of the Grand Seiko reading and 58% within ±0.25D of one another if rounding Grand Seiko measurements to the nearest 0.25D. Despite the increase in agreement due to rounding measurements to 0.25D with the Grand Seiko, significant differences remained for the MSE (p < 0.05).
The two sets of measurements were significantly correlated (r = 0.97, p < 0.001) (see Fig. 1B).
Astigmatic vectorsMaximum cylindrical error was −1.40D (mean ± SD −0.56 ± 0.38D) with the Grand Seiko and −1.75D (mean ± SD −0.32 ± 0.43D) with the Topcon TRK-2P.
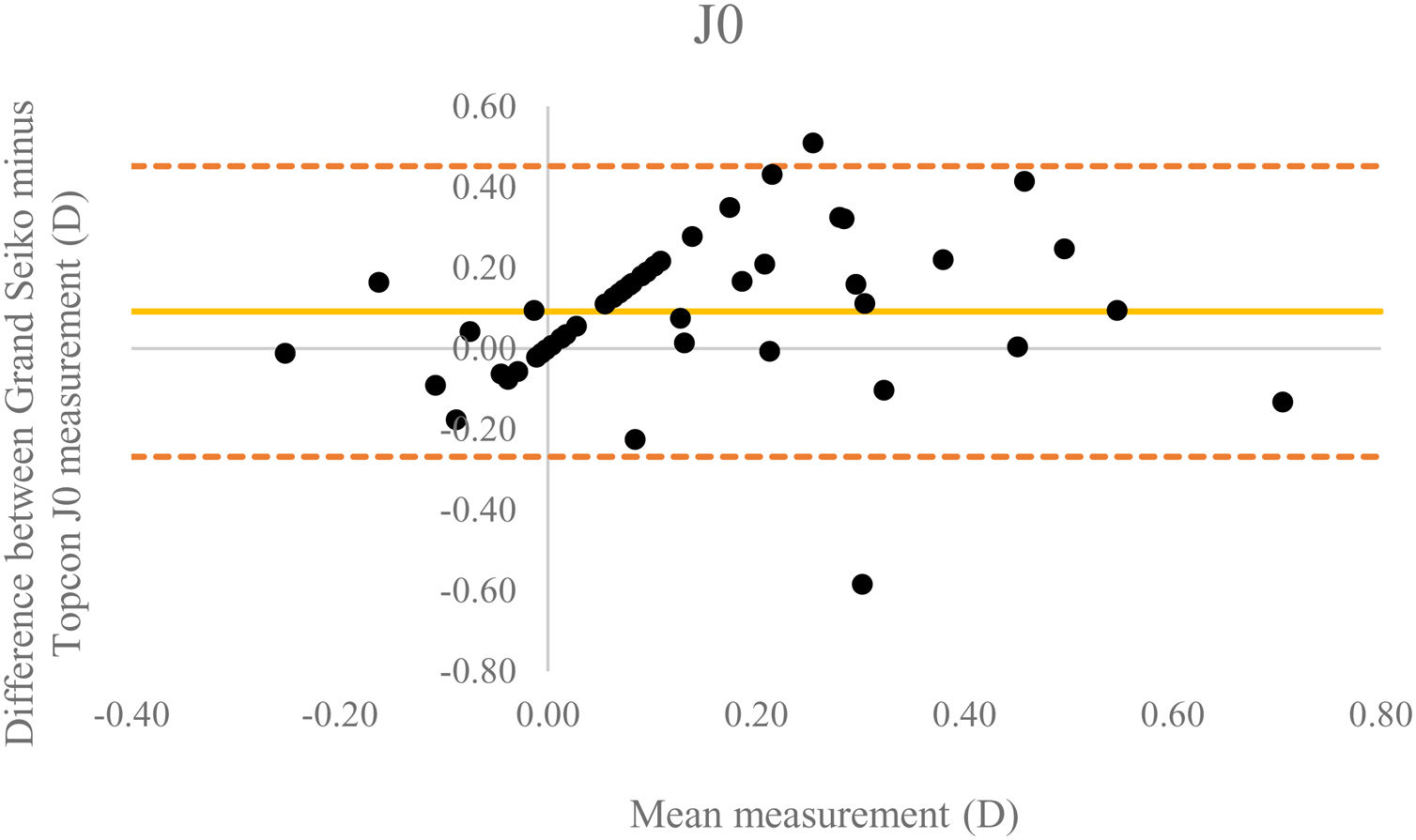
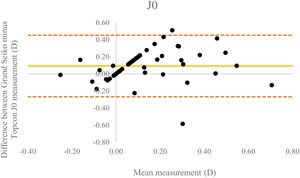
We observed a significant difference in J0 between autorefractors (p < 0.01) whereby the mean measurements obtained using the Grand Seiko were, once again, more plus powered (mean ± SD: +0.09 ± 0.18D). There appeared to be some evidence of proportional bias, with differences between instruments increasing as a function of increasing refractive error (see Fig. 3).
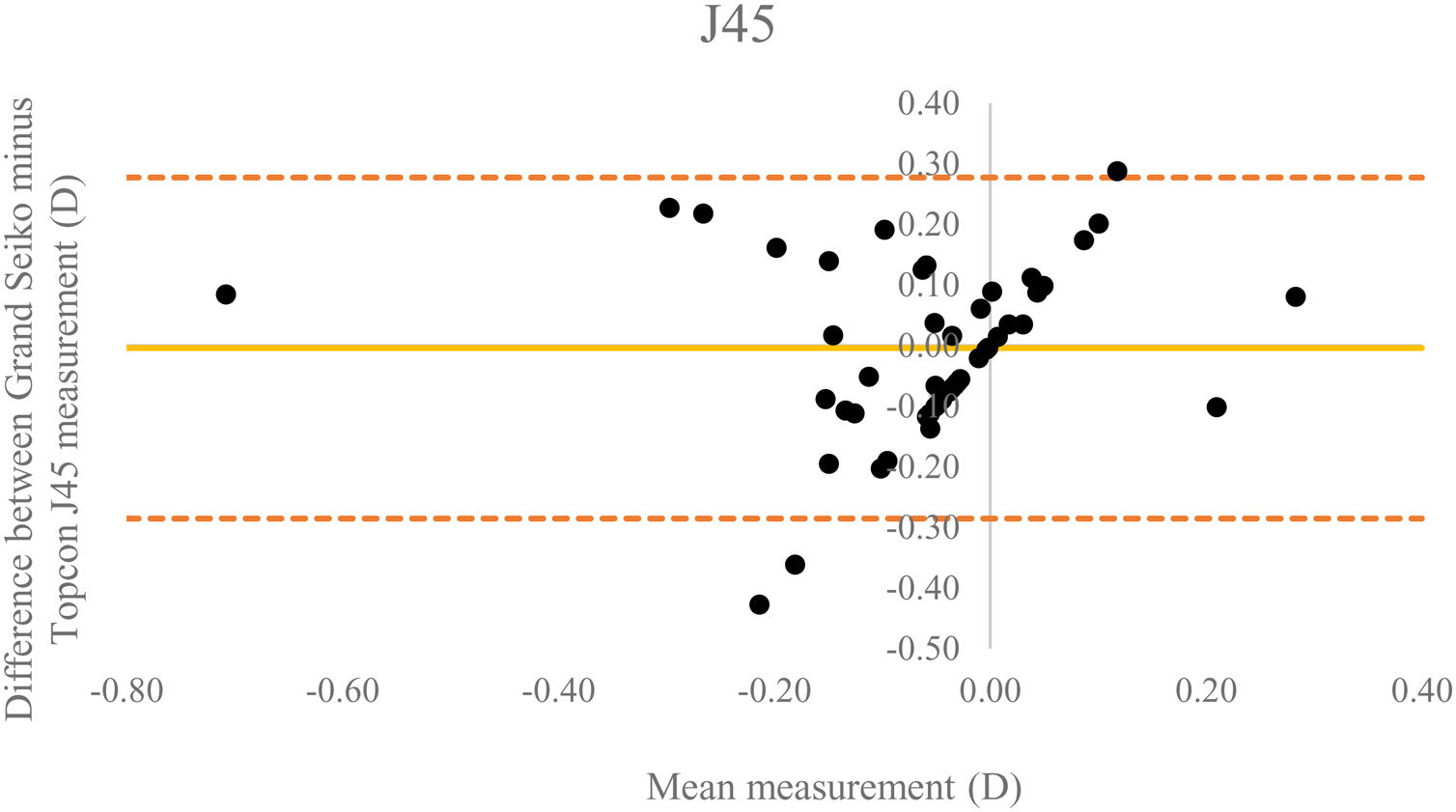
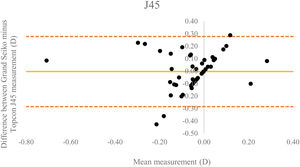
There were no significant differences in J45 between instruments (p > 0.05). As with the J0 vector component, some evidence of proportional bias was observed with differences increasing as a function of increasing refractive error (see Fig. 4). Rounding Grand Seiko outcomes still led to a significant difference between Grand Seiko and TRK-2P measurements for J0 (p < 0.05) and no significant differences for J45 (p > 0.05).
The two sets of measurements were found to be highly correlated for both J0 (r = 0.63, p < 0.001) and J45 (r = 0.60, p < 0.001), although the scatterplot only showed a weak linear correlation (see Figs. 1C and D).
DiscussionThe difference between open-view and closed-view autorefraction readings was found to be statistically significant for all vector and spherical refractive components except J45. For most components, the differences found were not systematic, thus reducing the likelihood of applying a correction factor to make data more comparable. Nevertheless, 76% of mean spherical errors calculated from the Topcon TRK-2P readings fell within 0.50D of the corresponding Grand Seiko WAM-5500 readings (when Grand Seiko WAM-5500 readings were rounded to the nearest 0.25D), thus still providing a clinically useful starting point for subjective refraction.
We found a mean difference in MSE between instruments of 0.23D, which is lower than that reported by several earlier investigations of closed and open view autorefraction. Previous work by Gwiazda et al.6 compared non-cycloplegic closed (Nidek ARK 700-A; Nidek Ltd., Tokyo, Japan) versus open view autorefraction (Canon R-1 by Canon Europa, N.V., The Netherlands, and the Grand Seiko WR-5100K) in adults (mean age 30.5 years, range 18–59 years). Mean MSE was reported as more plus powered using the Grand Seiko WR-5100K, with a mean difference of 0.65D. Similar outcomes were reported by Rosenfield and Ciuffreda who,9 despite testing a much younger cohort (mean age 11.3 years, 5−17 year olds), found a mean pre-cycloplegic difference in MSE between the Righton Retinomax-3 (Righton Ophthalmic Instruments, Tokyo, Japan) hand-held, closed-view autorefractor and the Grand Seiko WAM-5500 of 0.65D (with the Grand Seiko measuring extra plus power). The study reported a post-cycloplegic mean difference of 0.32D.
Similar results have been reported for younger cohorts. Choong et al.14 reported non-cycloplegic estimates of spherical equivalent in children aged 7–12 years (mean age 9.6 years), obtained using the Grand Seiko WR-5100K and the Retinomax K plus 2 autorefractor (Retinomax K plus 2, Nikon Corp, Japan). A mean difference of approximately 0.76D was found which reduced to a difference of 0.10D with cycloplegia. Ying et al.7 also compared cycloplegic measurements using the Grand Seiko and the Retinomax for children, aged approximately 4–6 years old, a mean difference of approximately 0.34D was reported. Thus such findings may, at least in part, be attributable to reduced proximal accommodation found with open view autorefraction.
Even in cases where differences between subjective refraction and open view autorefraction are found to be statistically significant, they may remain clinically insignificant.4 As such, the purpose for which autorefraction is being undertaken, is crucial when choosing an instrument. In research, where refractive error is a main outcome and even small refractive changes may be of importance, particularly within longitudinal clinical and interventional trials, a key consideration should be whether the potential margin of error associated with the autorefractor could mask any interventional/treatment effect. While MSE is often the metric of choice in studies of refractive error, it is noteworthy that in our study isolating spherical error measurements showed a greater mean difference between the readings from each instrument than MSE alone. Furthermore, a proportional bias for astigmatic components could have also affected the MSE calculated.
In this study, the differences between astigmatic vectors were only significant for J0 but not J45. Based on previous literature, it appears outcomes related to astigmatic components can be inconsistent between studies, with several showing significant differences between subjective refraction and open view autorefraction for J03,5 while others do not.4 Similarly, while some literature suggests good agreement between the astigmatic component between closed versus open view autorefraction6 others have noted significant inter-instrument differences for the J45 component.9 Differences may arise due to dissimilarities in cohort refractive errors, specifically the cylindrical component. It is, however, clear that such differences are very small (see Table 1). The intertest variability of J45 with the Grand Seiko WAM-5500 has previously been reported as a mean difference of 0.01 ± 0.14D5 i.e. the disparities between the various study outcomes may simply be due to an attempt to measure a very small metric which approaches the limit of the instrument’s capability.
Further erroneous measurements may stem from the size of each fixation target, for example, whereby a larger target may encourage poorer fixation leading to unreliable measurements. The angle subtended by each target will vary depending on refractive error and could also impact fixation accuracy. Lastly, the participant many have been fixating on a point completely outside the target area e.g. with the open-view autorefractor the participant could fixate on the observer instead of the target, introducing proximal accommodation and causing a myopic shift in measurements.
A possible limitation of our study is that the increments for measuring refractive error differed between autorefractors. However, we show by rounding to the nearest 0.25D and thus making the outcomes from each instrument more comparable, significant differences for MSE, J0, and the spherical component between instruments remained. It is worth highlighting that the overall proportion of Topcon TRK-2P readings that fell within ±0.50D and ±0.25D of Grand-Seiko outputs increased when Grand Seiko readings were rounded to the nearest 0.25D. Nevertheless, possible proportional bias makes it challenging to apply a correction factor to readings, thus it is difficult to render the two autorefractor outputs comparable. A further limitation of our study could be that our cohort refractive range was limited; we did not include moderate-high hyperopes or high astigmats, and only a few high myopes. No exclusion criteria were applied to the range of refractive error included in this study to remain representative of the population sampled. Based on the means and standard deviations found, the sample size is adequate for the spherical component, MSE, and J0; however, a larger cohort would be preferable for completely studying oblique astigmatism J45. Despite such limitations, the characterisation of our measurements highlights the differences between both autorefractors to users, researchers and clinicians.
ConclusionsIn summary, outputs from The Grand Seiko WAM-5500 and the Topcon TRK-2P are not found to be interchangeable when used on young adults without cycloplegia due to statistically significant differences. This implies that data from studies using these specific types of autorefractors cannot be easily compared when investigating refractive error in young adults. The differences are, however, small from a clinical perspective and smaller than those reported by several previous studies which have compared closed-view autorefractors to those from the Grand Seiko series. Thus, the Topcon TRK-2P may provide an excellent starting point for clinical refraction. Further work is required to determine the impact of cycloplegic agents, age, and fixation targets to understand whether there is scope for increasing the concordance between these two instruments.
Conflicts of interestThe authors have no conflicts of interest to declare.
FundingThis research did not receive any specific funding.
N/A.