Laser Vision Correction is not always possible for the treatment of myopia. The aim of this paper is to present results after MyoRing implantation in myopic eyes who in their majority were not eligible for LVC. Safety, effectivity and patient selection is discussed. The aim of the treatment was to be spectacle independent in everyday-life.
Materials and methods19 myopic eyes of 12 patients ranging from −2.25 to −16.5 dioptres (D) in sphere and from 0 to −4D in cylinder were analyzed.
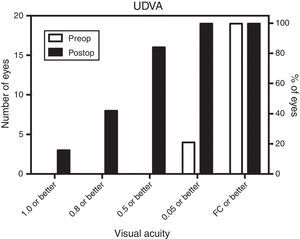
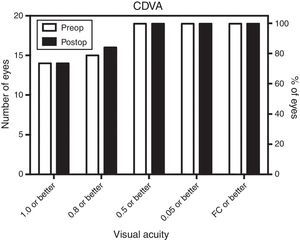
ResultsAfter treatment, 84% of the eyes reached uncorrected distance visual acuity (UDVA) of 0.5 or better, 42% reached UDVA of 0.8 or better and 16% reached UDVA of 1.0 or better. Before treatment, no eye reached UDVA of 0.5 or better. Corrected distance visual acuity (CDVA) preoperatively and postoperatively did not differ. The treatment changed the average spherical equivalent from −10.27D to −0.93D. Efficacy index was 0.76 and safety index was 1.02.
ConclusionMyoRing implantation for myopia is safe and effective with highly satisfied patents in a particular subgroup of myopic patients. Patient selection is important.
La corrección de la visión con láser (CVL) no es siempre posible en el tratamiento de la miopía. El objetivo de este artículo es presentar los resultados tras la implantación de MyoRing en ojos miopes que, en su mayoría, no son aptos para la CVL. Se tratan cuestiones tales como la seguridad, la efectividad y la selección de los pacientes. El objetivo del tratamiento fue el de eliminar el uso de gafas en la vida diaria.
Materiales y MétodosSe analizaron 19 ojos miopes de 12 pacientes, con un rango de -2,25 a -16,5 dioptrías (D) de esfera, y de 0 a -4 D de cilindro.
ResultadosTras el tratamiento, el 84% de los ojos logró una agudeza visual lejana sin corrección (UDVA) de 0,5 o superior, el 42% logró una UDVA de 0,8 o superior, y el 16% logró una UDVA de 1,0 o superior. Con anterioridad al tratamiento, ningún ojo logró una UDVA de 0,5 o superior. La agudeza visual lejana corregida (CDVA) no difirió con anterioridad y posterioridad a la operación. El tratamiento modificó el equivalente esférico medio de -10,27 D a -0,93 D. El índice de eficacia fue de 0,76 y el índice de seguridad de 1,02.
ConclusiónLa implantación de MyoRing en pacientes miopes es segura y efectiva, con elevada satisfacción por parte de un subgrupo específico de pacientes miopes. Es importante la selección de los pacientes.
Laser Vision Correction (LVC) offers a safe and effective treatment of myopia.1 However, a significant number of patients seeking for LVC are not eligible for that treatment. One reason is the risk of severe long-term complications such as corneal ectasia.2 Risk factors include thin cornea and high myopia.3 In high myopia, postoperative ectasia can develop in up to 2.5% of the cases.4 Implantation of phakic intraocular lenses (pIOL) is often considered as an alternative option in many cases of high myopia. Complications after pIOL include clinically significant cataract formation in some 7%, glaucoma in some 7% and endothelial decompensation.5–7
Corneal intrastromal implantation surgery (CISIS) with MyoRing implantation into a corneal pocket has been demonstrated to be able to treat keratoconus8–11 and to correct moderate to high myopia successfully.12 Here I report about a sample of mild, moderate and high myopic cases I have treated by means of CISIS with MyoRing.
Materials and methodsNineteen myopic eyes of 12 patients without any topographic sign of manifest keratoconus are included in this study. This is a retrospective study which enrolls patients whom I treated during the past 8 years and who had a postoperative examination in my center between July 1 and December 31, 2015. Informed consent was obtained from every patient prior to surgery.
Eighteen of 19 eyes were not eligible for LVC and 1 was treated just because he wanted neither LVC nor pIOL but a safe and reversible treatment. Sixteen of the 18 eyes not eligible for LVC were treated because of thin cornea and/or high myopia, while 2 because of rheumatoid arthritis (RA). Although RA is also mentioned as a contraindication in the instruction for use (IFU) of MyoRing, the patient insisted in having any kind of surgical correction and we achieved consent to perform MyoRing implantation with short follow-up periods to be able to detect a possible ring extrusion early and to remove the ring immediately when it seems to happen in order to avoid harming the cornea. The analyzed follow-up period ranged from 2 months to 24 months (median 6 months). The age of the patients ranged from 21 to 46 years at the time of treatment (median 28 years). Table 1 shows the nomogram used in the study.
The nomogram shows the dimensions of the MyoRing used for a certain refractive correction and the number of eyes treated with each MyoRing dimension.
| MyoRing diameter (mm) | MyoRing thickness (microns) | SE range (dioptres) | Number of treatments |
|---|---|---|---|
| 5 | 280 | −9.0 to −13.0 | 14 |
| 6 | 280 | −5.5 to −6.5 | 3 |
| 7 | 280 | −2.5 to −3.5 | 2 |
The treatment were perfomed using the PocketMaker Ultrakeratome (DIOPTEX GmbH, Austria) for the creation of the corneal pocket followed by MyoRing (DIOPTEX GmbH, Austria) implantation as described elsewhere.8
ResultsPreoperative sphere ranged from −2.25 to −16.5 dioptres (D) and preoperative cylinder ranged from 0 to −4.0D. Table 2 shows comparison between preoperative and postoperative spherical equivalent and the corrective power for every MyoRing dimension used. The corrective power corresponds well to the change in central average K reading. Table 3 shows sphere and cylinder pre- and postoperatively for every MyoRing dimension used.
Preoperative and postoperative spherical equivalent (SE) and corrective power in dioptres for each MyoRing dimension used in the study.
| MyoRing diameter (mm) | MyoRing thickness (microns) | SE preoperatively (dioptres) | SE postoperatively (dioptres) | Corrected power (dioptres) |
|---|---|---|---|---|
| 5 | 280 | −11.72±2.6 | −0.88±1.2 | 10.8±1.4 |
| 6 | 280 | −6.83±0.8 | −0.67±0.8 | 6.17±0.2 |
| 7 | 280 | −2.81±0.3 | +0.5±0.0 | 3.31±0.3 |
The values show mean and standard deviation.
Preoperative and postoperative sphere (sph) and cylinder (cyl) in dioptres for each MyoRing dimension used in the study.
| MyoRing diameter (mm) | MyoRing thickness (microns) | sph preoperatively (dioptres) | cyl preoperatively (dioptres) | sph postoperatively (dioptres) | cyl postoperatively (dioptres) |
|---|---|---|---|---|---|
| 5 | 280 | −11.00±2.7 | −1.45±1.2 | −0.45±0.4 | −0.88±0.9 |
| 6 | 280 | −7.58±2.5 | −1.75±1.3 | −1.42±2 | −1.33±0.6 |
| 7 | 280 | −2.5±0.4 | −0.63±0.2 | 1.0±0.4 | −1.0±0.7 |
The values show mean and standard deviation.
Uncorrected distance visual acuity (UDVA) improved significantly from 1.77±0.5 to 0.23±0.3 (logMAR) in average. As a measure of the effectivity of the treatment, postoperative UDVA was in average 1.8 lines below preoperative CDVA which resulted in an efficacy index of 0.76. Fig. 1 shows the distribution of preoperative and postoperative UDVA. While before treatment only 21% of the eyes had UDVA of 0.05 or better and no eye (0%) had 0.5 or better, after treatment 84% of the eyes had UDVA of 0.5 or better and even 16% had 1.0 or better.
Corrected distance visual acuity (CDVA) remained practically unchanged between preoperative and postoperative examination resulting in a safety index of 1.02. Preoperatively, all eyes (100%) had CDVA of 0.5 or better, 80% had 0.8 or better and even 74% had CDVA of 1.0 or better. Fig. 2 shows the distribution of preoperative and postoperative CDVA. Only one eye changed from CDVA (decimal) less than 0.8 to 0.8 or better. Table 4 shows the visual acuity before and after treatment.
The aim of the treatment were not to guarantee emmetropia but to be able to handle daily life, including car driving without wearing spactacles or contact lenses. The patients were informed preoperatively that it may happen that they have to wear spectacles in a low diopter range for special occasions such as night driving.
A total of 20% of the cases reported night vision problems and halos during an initial period of time after surgery without spectacles which usually disappeared or were not recognized anymore after 3 months.
No relevant complications happened during or after surgery. Deposits were seen occasionally at the implant edge but were of no clinical relevance. There was also no stromal thinning or dry eye symptoms.
DiscussionThe ideal range of myopia treatment by means of CISIS with MyoRing implantation is around −10D sphere with cylinder values of less than −2D. These patients are extremely happy when preoperatively selected in the right way. Patient selection is mainly based upon the expectation of the patient. If the patient is happy with contact lenses and it is important for him to have visual acuity of 20/20 or better in everyday life, this option of treatment is not the adequate. These patients will not be happy at all and will ask for MyoRing removal. Since implantation as well as removal of the MyoRing is almost as simple as handling a contact lens without the need of a suture, it might be not a big problem in wrong chosen cases, because the quick, easy and painfree way of MyoRing removal (reversibility) is usually one of the main criteria of the patients for choosing that treatment option. Removing the MyoRing is just less than a one minute job and starts with opening of the corneal tunnel by means of a Sinskey hook and reopening the pocket by means of a spatula. Then, the MyoRing can easily be extracted by means of the Sinkey hook. The corneal tunnel is self sealing and requires no suture.
The right patients are those who have good CDVA but want to be able to handle daily life, including car driving without wearing spectacles or contact lenses but are willing to wear spectacles in a low diopter range for special occasions such as for instance night driving. In particular, those patients out of that group who are around −10D (−8 to −13D) of spherical equivalent (SE) are usually extremely happy and do not report relevant side effects postoperatively. A second group of excellent candidates who almost always tolerate the treatment very well without any reports of relevant side effects are those cases of moderate and high myopia who preoperatively do not reach CDVA 0.8 or better. Most probably, this is because these patients are less sensitive to additional visual disturbances such as halos.
Regarding the visual results, it is important to note that after MyoRing implantation, more than 84% had UDVA of 0.5 and better, 42% had UDVA of 0.8 or better and even 16% had UDVA of 1.0 or better while preoperatively 100% of the eyes reached CDVA of 0.5 or better, but only 84% reached CDVA of 0.8 or better and only 73% reached CDVA of 1.0 or better. These data are shown graphically in Figs. 1 and 2. It should be noted that these data include also those cases where the correction of anisometropia was the aim and not being close to emmetropia. Those 2 eyes (10%) who did not reach intended UDVA of 0.5 or better postoperatively, reached UDVA of 0.4. These eyes had preoperatively −16.0 sphere and −0.5 cylinder and −13.5 sphere and −3.0 cylinder. Both patients were postoperatively happy and denied removing the MyoRing.
Interestingly, it seems that pupil size does not play that role in patient selection as patient's expectations do. There were even patients with relatively large pupils who tolerated the (transparent) MyoRing very well without complaining about halos or other visual disturbances.
A limitation of that retrospective analysis is that it considers an arbitrarily selected group of patients who visited the private practice for postoperative follow-up during a certain period of time (between July 2015 and December 2015) but whose treatment have been completed already successfully much earlier. Since many of the treated patients are from a distant area, it was difficult to recruit a large group of treated patients for follow-up after completing the treatment The cases presented are considered a random sample of the eyes treated according to the reported selection criteria. It does therefore not include those cases who required removal of the implant for not reaching the visual results they expected. That number of patients, however, can be kept very low if the right patient selection and an appropriate teaching of the patients as described above take place preoperatively. The presented data therefore describe the visual results which can be achieved by that method if the patients are properly selected according to the criteria described above. In agreement with the experience with the treatment of keratoconus, no intra- or postoperative complications have been observed in the treatment of myopia.8–11
In conclusion, MyoRing treatment is a safe, effective and fully reversible refractive surgery procedure which gives excellent results in a particular group of myopic patients suffering from moderate and high myopia.
FinancialThe author has a financial interest in DIOPTEX GmbH.
Conflict of interestThe author has an investment interest in DIOPTEX GmbH.