To evaluate the efficacy of multifocal soft contact lenses (MFSCLs) and defocus incorporated multiple segments lenses (DIMS) to limit myopic progression in children with high myopia.
MethodsThis retrospective study included 249 children (aged 8-16 years) with high myopia (non-cycloplegic spherical equivalent [SE] −6.00 to −10.00 D, astigmatism < 2.00 D). Selected participants were those treated with DIMS (N=81), MFSCLs (DISC, N=60), or single-vision spectacles (SVLs, N=108, control group). Myopic progression was assessed based on the 1-year SE change from baseline, categorized as slow (<−0.25 D), moderate (−0.25 to −0.75 D), or rapid (> −0.75 D). The multiple linear regression evaluated the association between myopic progression and characters.
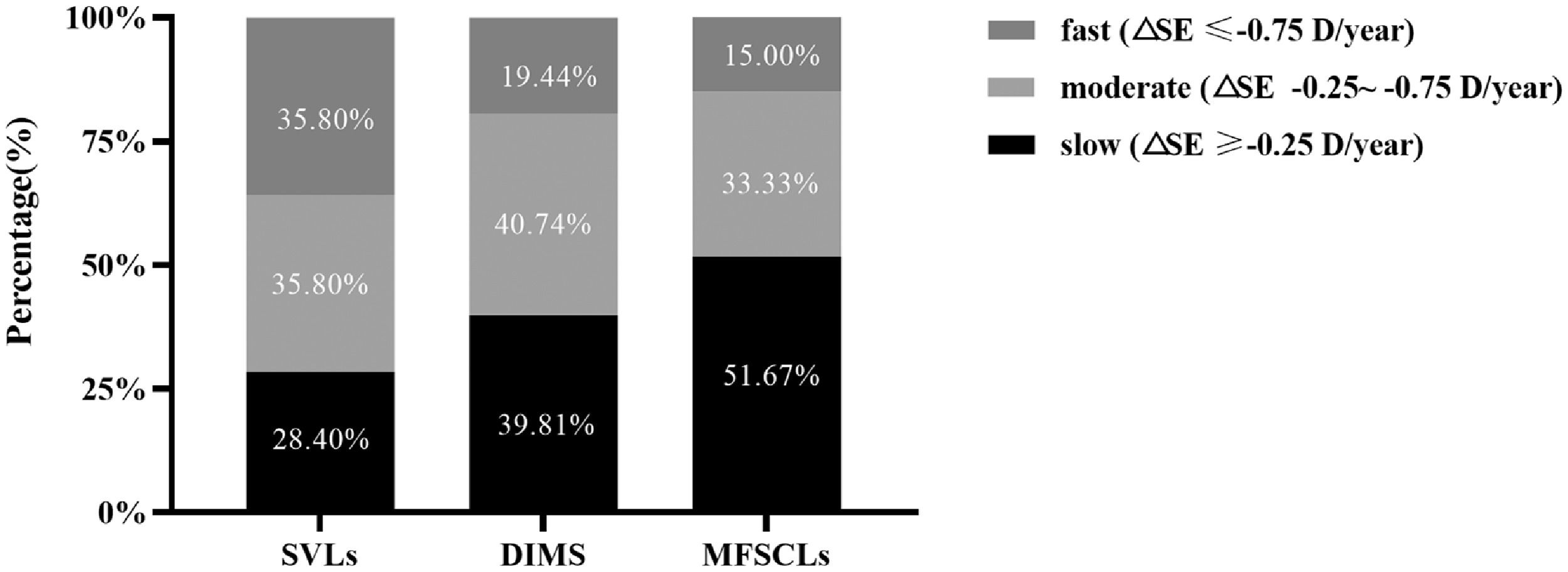
ResultsNo significant differences in age, SE, or sex were found among the groups at baseline. At one year, the magnitude of myopic progression was significantly smaller in the DIMS (−0.47 ± 0.39 D, 33.8 %) groups and MFSCLs (−0.39 ± 0.47 D, 45.1 %) compared to the SVL group (−0.71 ± 0.54 D; P < 0.001). The proportion of slow progressors was 28.40 % (SVLs), 39.81 % (DIMS), and 51.67 % (MFSCLs). Age was associated with the myopic progression in the DIMS (β=0.108, P < 0.001) and SVLs (β=0.120, P < 0.001) group, but not in the MFSCLs (P=0.776) group. MFSCLs were preferred for children under 12 years, while DIMS and MFSCLs showed comparable efficacy for those over 12 with high myopia.
ConclusionsBoth MFSCLs and DIMS have demonstrated efficacy in delaying myopic progression in children with high myopia. The MFSCLs will give children better control up to the age of 12; after that, they remain a good option.
The rising global prevalence of both myopia and high myopia (myopia > −6.00 D) have caused both conditions to become major public health concerns.1 It is predicted that high myopia will affect nearly 10 % of the global population by 2050 if the phenomenon of myopic progression is left unaddressed.2 This is of most concern in East and Southeast Asia, where the reported prevalences of high myopia range from 10–20 %.3 High myopia is an irreversible eye disease often accompanied by complications such as retinal detachment, macular degeneration, posterior staphyloma, choroidal neovascularization, and glaucoma.4,5 The risk of myopia-related complications increases with each diopter of myopia;6 thus, slowing or halting myopia progression, even in high myopes, is crucial. Therefore, developing interventions to slow the progression of myopia and reduce the incidence of high myopia has become an urgent problem to be solved.
Optical devices provide a safe and convenient method for myopia correction. Many myopia control strategies are based on the peripheral defocus theory, which has led to the development of specially spectacle lenses and multifocal contact lenses. Currently, novel spectacle lenses incorporating peripheral myopic defocus have demonstrated efficacy in slowing myopia progression. Defocus Incorporated Multiple Segments Lenses (DIMS) lenses have shown promising results in achieving effective myopia control in one year or long-term visit.7–9 Lam et al. reported significantly shower myopia progression with DIMS lenses compared to single-vision spectacles, with mean annual changes of −0.17±0.05 D versus −0.55±0.04 D (1-year data) and −0.41±0.06 D versus −0.85±0.08 D (2-year follow-up).7 The 3-year follow-up demonstrated sustained efficacy, with SE and AL changes of −0.52±0.69 D and 0.31±0.26 mm, respectively.8 The 6-year cohort maintained consistent control, showing comparable progression rates between initial and later periods (SE: −0.52±0.66 vs −0.40±0.72 D; AL: 0.32±0.26 vs 0.28±0.28 mm; both p > 0.05).9 In clinical practice, efforts have been made to expand the scope of DIMS applications. Domsa P et al. study10 assessed the effectiveness of DIMS lenses in managing myopia up to −8.25 D and astigmatism up to −3.25 D, reporting a one-year spherical equivalent (SE) change of −0.40 ± 0.05 D (n = 62) and an axial length (AL) change of 0.16 ± 0.03 mm (n = 33). However, the study did not exclusively assess the efficacy of DIMS lenses in controlling high myopia. Previous studies reported decreasing efficacy of DIMS lenses with increasing spherical equivalent (SE) among children,11 or no significant difference compared to the SVLs,12 suggesting that there was limited effect of DIMS for children with high myopia. Thus, developing more effective interventions for managing high myopia is essential.
Recently, multifocal soft contact lenses (MFSCLs), known for their acceptability, comfort, and greater efficacy, have been well-received by children. Previous studies have reported that the effectiveness of MFSCLs in reducing myopic progression over one year ranges from 38 % to 74 %13–16 in low to moderate myopia. The amount of myopic progression, determined by computing annual shifts in SE, ranges from 0.22 to 0.81 D in those wearing multifocal soft contact lenses and from 0.50 to 1.45 D in control groups who wore single-vision spectacles or single-vision contact lenses over at least 1 year.17 A similar soft multifocal design, daily disposable defocus incorporated soft contact lenses (DISC), feature a concentric ring design with a central corrective zone and alternating defocus zones (+2.50 D add), was also effective in reducing axial length elongation (52.3 %) compared to single vision contact lenses over a 2-year follow-up period in Hong Kong schoolchildren.13 Although multifocal soft contact lenses can correct myopia up to −20.00 D,18–20,22 their efficacy as an intervention in children with high myopia remains underexplored. To date, some studies19,20 have evaluated this, involving 96 Caucasian children with myopia ranging from −0.75 D to −10.00 D who were fitted with Extended Depth of Focus (EDOF) soft contact lenses. A 2-year follow-up showed a myopia control effect of −0.62 ± 0.30 D with MYLO lenses, compared to −1.13 ± 0.20 D with SVLs.19 At 3 years, the corresponding values were −0.90 ± 0.36 D (MYLO) and −1.64 ± 0.26 D (SVLs).20 However, it should be noted that high myopia cases represented <5 % of the study population. Moreover, races variations in treatment response to multifocal soft contact lenses may exist among myopia children.
Therefore, we aimed to preliminarily evaluate the efficacy of MFSCLs and DIMS lenses in Chinese children with high myopia by retrospective study and to identify potential factors influencing their effectiveness.
Material and methodsStudy design and subjectThis retrospective analysis examined medical records of Chinese children with high myopia fitted with either DIMS or MFSCLs between February 2020 and February 2022 and presented for follow-up for at least 12 months. All medical records were derived from Tianjin Eye Hospital Optometric Center. A control group of spectacle-corrected highly myopic children, matched for age, gender, and SE, were selected from the same period. Records were selected based on the following inclusion criteria: children with ages between 8 and 16 years, non-cycloplegic spherical equivalents between − 6.00 D and − 10.00 D, astigmatism ≤ 2.00D, and best-corrected visual acuity (BCVA) of 0.8 or better (Snellen chart). Standard exclusion criteria defined in each investigation were as follows: obvious strabismus, amblyopia, abnormal eye movements; BCVA <0.8 (Snellen chart); combined with other control strategies (e.g., low-concentration atropine eye drops, repeated low-level red-light therapy); moderate to severe dry eye; discontinuations of MFSCLs wear for >1-month during the follow-up period. Only the right eye was included for analysis. The study met the tenets of the World Medical Association’s Declaration of Helsinki and was approved by the Medical Ethics Committee of Tianjin Eye Hospital (No. 2022,068).
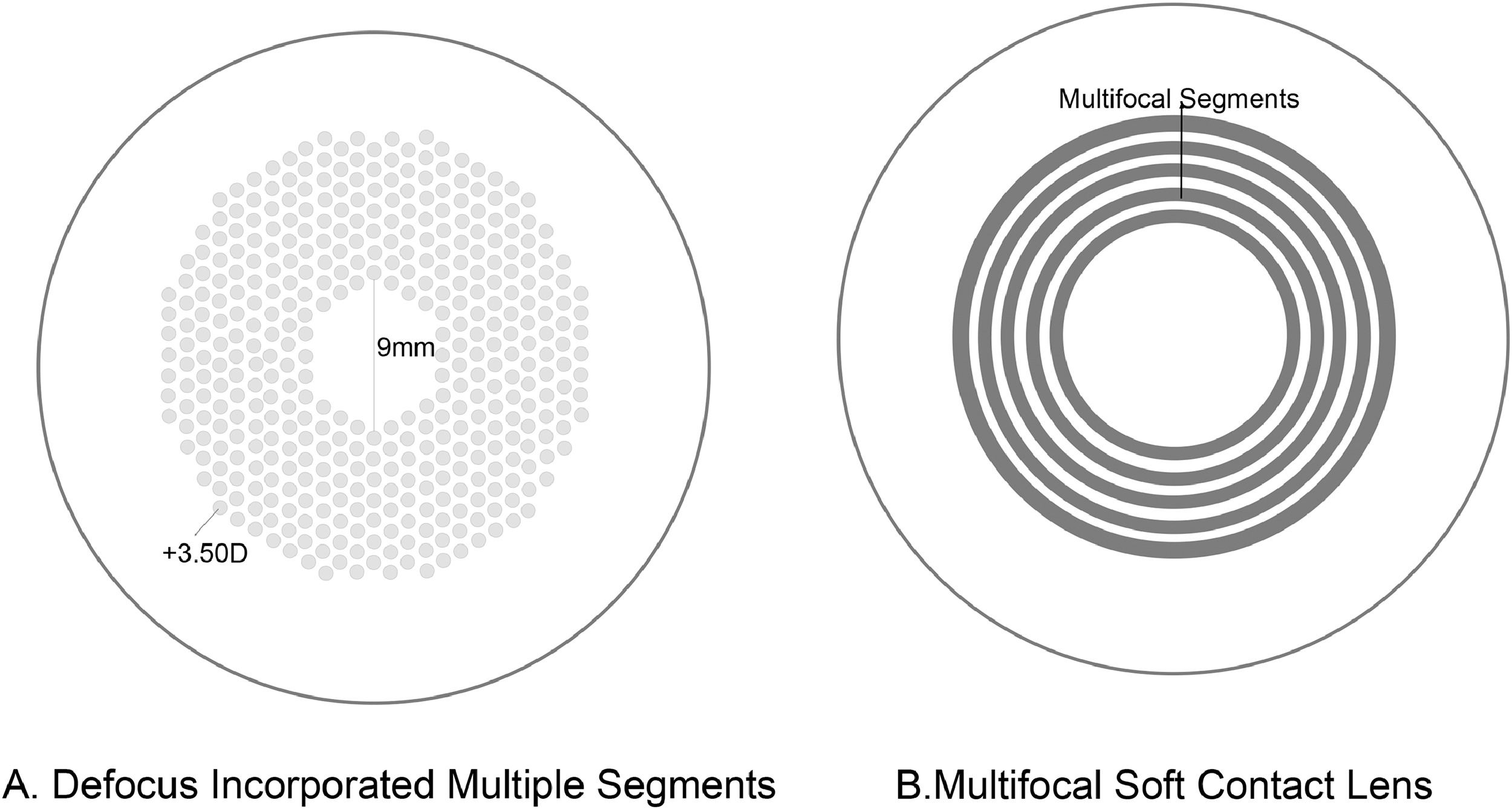
Lens designChildren in the treatment group were fitted with DIMS spectacle lenses (MiyoSmart, Hoya lens), which feature a central zone (9 mm in diameter) providing myopic refractive correction for clear vision, surrounded by a zone of lenslets (+3.50 D) designed to create myopic defocus in the mid-periphery of the retina (Appendix Fig. 1A). Each lenslet segment has a diameter of 1.03 mm. This design simultaneously induces myopic defocus while ensuring clear vision at all viewing distances. The myopic defocus generates multiple focal points on a plane in front of the retina, perceived as blurred images on the retina.
All patients in the MFSCL group wore the same soft multifocal contact lens. The DISC (St. Shine Optical Co., Ltd. (Taiwan, China) features a concentric-ring, dual-focus design for myopia management. These lenses are made from hydroxyethyl methacrylate with 38 % water content, a base curve of 8.6 mm, and a total diameter of 14.2 mm, and are available in powers ranging from −1.00 to −10.00 DS. The design includes a central optical zone of 3.0 mm diameter for spherical distance correction and alternating concentric rings with either the spherical distance correction or an addition of +2.50 D The corrective zones, each 0.25 mm wide, are distributed in a 50:50 ratio. The lens provides an oxygen permeability (Dk) of 8.4 × 10⁻¹¹ (cm2/s) ·[mlO2/(ml·mm Hg)], ensuring sufficient corneal oxygenation, and is optimized for both visual correction and peripheral defocus, potentially slowing myopia progression. Similar to the mechanism of DIMS lenses, the central zones provide clear distance vision, while the concentric defocus zones deliver sustained myopic defocus across the peripheral retina, which is believed to help retard axial elongation (Appendix Fig. 1B).
Sample sizeIn this study, high myopia progression was defined as >0.25D/year.11,21 Based on expected progression rates (SVL: 60 % vs DISC: 30 %), with 80 % power and α=0.05 (two-tailed), the calculated minimum sample size was 40 subjects per group. Only right eyes were analyzed. The DIMS group showed comparable sample size to the multifocal contact lens group.
Group and follow-upA total of 249 eyes were included: 108 in the DIMS group, 60 in the MFSCLs group, and 81 in the SVLs control group. The subjects in the SVLs and DIMS groups were instructed to wear the spectacles full-time (at <12 h per day) and returned for detailed ophthalmological examination after 12 months. Subjects in the MFSCLs groups were fitted with contact lenses by experienced optometrists. They were instructed to wear the lenses during daytime hours at least 6 days per week and for at least 8 to 10 h per day. During the remaining time, patients wear standard glasses. Follow-up examinations were performed at 1 week and 1 month after dispensing the lens, and every 3 months thereafter.
Spherical equivalent measurementAt baseline and the 12-month follow-up visit, each child in each of the three groups (i.e., DIMS, MFSCLs, and SVLs) had their non-cycloplegic subjective refraction determined by experienced ophthalmologists, according to the principles of Maximum Plus Maximum Visual Acuity (MPMVA). The spherical equivalent (SE) of this subjective refraction was used to determine the amount of myopic progression after twelve months (▵SE, ▵SE=SEone-year-SEbaseline). The subjects were divided into three post-hoc myopia progression groups according to the ▵SE: slow progression (▵SE≥−0.25D), moderate progression (▵SE −0.25 to −0.75D), and fast progression (▵SE≤−0.75D).23
Statistical analysisData from the right eye were chosen for statistical analysis. All parameters were tested for normality, and the normal and approximately normal distribution parameters were expressed as mean ± standard deviation (M ± SD). Differences in myopic progression among three treatment groups were assessed by a one-way ANOVA, and Post-hoc comparisons using Bonferroni corrections. Chi-square tests were used to proportional data. Multivariate linear regression analyses were used to investigate the covariates associated with myopia progression. All analyses were performed using R and R Studio (R., 4.4.1, 2024.). A P-value <0.05 is considered as statistical significance.
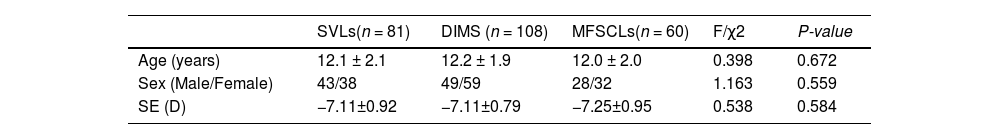
ResultsThe baseline characteristics of the study subjects are shown in Table 1. The subjects’ age ranged from 8 to 16 years (12.1 ± 2.0 years). Age distribution was as follows: 8 years (n = 9), 9 years (n = 21), 10 years (n = 25), 11 years (n = 47), 12 years (n = 39), 13 years (n = 37), 14 years (n = 46), 15 years (n = 18), and 16 years (n = 7). The baseline SE ranged from −6.00 to −10.00 D (−7.15 ± 0.88 D). There were no significant differences in age, sex, and SE between each group at baseline (all P > 0.05). No adverse events (e.g., corneal infection) occurred during follow-up.
Baseline characteristics of SVLs, DIMS, and MFSCLs groups (Mean ± standard deviation).
Note: SE, spherical equivalent; D, diopter. χ2 = test statistic from a Chi-square; F = test statistic from an ANOVA.
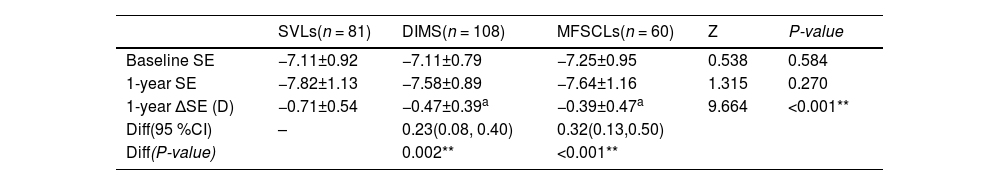
Table 2 shows the changes in SE in each group. Myopic progression tended to occur in each group: the mean change in spherical equivalent (∆SE) was −0.71±0.54D (SVLs), −0.47±0.39D (DMIS) and −0.39±0.47D (MFSCLs). The between-group difference was statistically significant (Z = 9.664, P < 0.001). The efficacy of myopia control, defined as the difference between the change in SE in single-vision spectacle vs. myopia intervention, was 0.23 D for DIMS and 0.32 D for MFSCLs. Table Appendix 1 presents the one-year SE changes stratified by age group for all three treatment modalities (SVLs, DIMS, and MFSCLs).
Changes of one-year SE in SVLs, DIMS, and MFSCLs groups (Mean ± standard deviation).
Note: SE, spherical equivalent; Z = Standardized test statistic from Dunn’s post-hoc test (following Kruskal-Wallis ANOVA), with Bonferroni-adjusted P-values, a represents a difference from SVLs. Diff represents the difference between the DIMS and MFSCLs groups compared to the SVLs group. 95 % CI denotes the 95 % confidence interval; * indicates P-value < 0.05; ** indicates P-value < 0.01.
To further compare myopic progression between each group, we examined the proportion of slow, moderate, and fast progressors in each lens modality group and found significant differences (χ2=13.221, P = 0.010). The Fig. 1 demonstrated that while the SVLs group showed nearly equal distribution across fast (▵SE≤−0.75D/year), moderate (▵SE −0.25D to −0.75D/year), and slow (▵SE≥−0.25D/year) progression categories (each ∼33 %), the DIMS group exhibited a significant shift toward slower progression (slow: 39.81 %, moderate: 40.74 %, fast: 19.44 %; P = 0.035), with an even more pronounced slow-progression shift observed in the MFSCLs group (slow: 51.67 %, moderate: 33.33 %, fast: 15.00 %; P < 0.001).
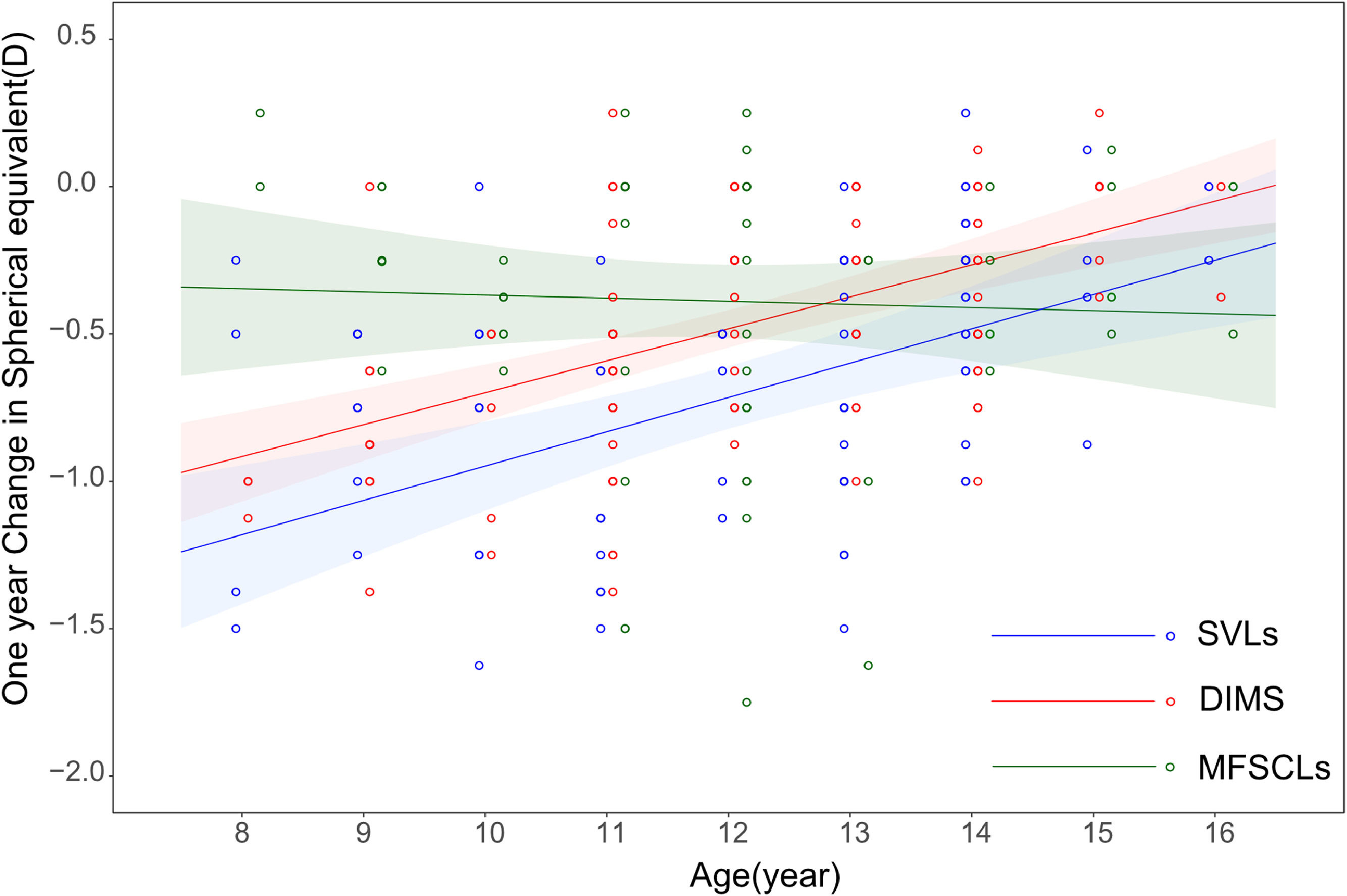
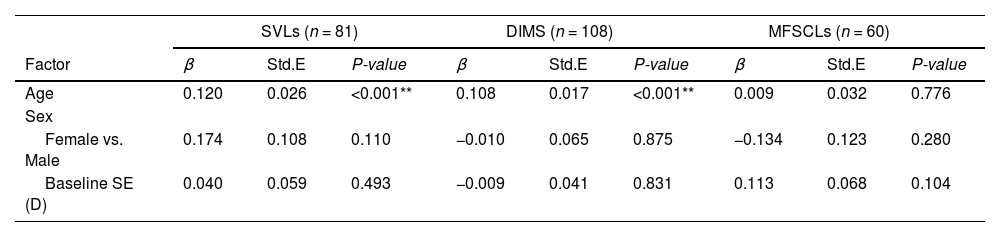
Multiple linear regression analyses indicated baseline age, but not sex and SE, was the covariate most associated with 1-year myopia progression in both SVLs and DIMS groups (Table 3, β=0.120, β=0.108, all P < 0.001). The older subjects showed slower myopia progression in those groups. In contrast, for the MFSCLs group, baseline age did not appear to be associated with myopia progression in children with high myopia.
Multivariable Factors were relevant to myopia progression for one year in SVLs, DIMS, and MFSCLs.
Note: SE, spherical equivalent. Std.E, Standard Error. * indicates P-value < 0.05; ** indicates P-value < 0.01.
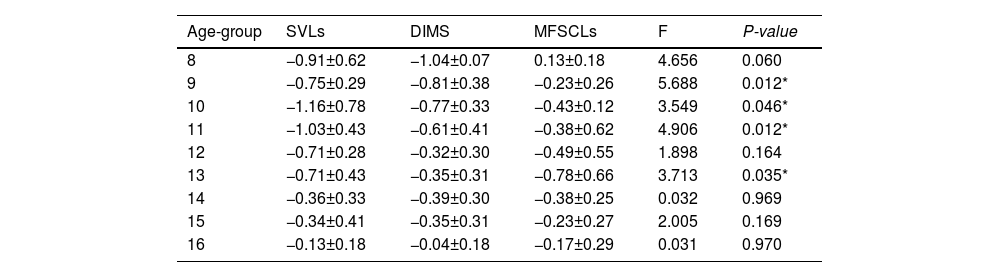
We analyzed age-related myopia progression in high myopia children. Fig. 2 compares progression rates across groups at a fixed age. The slopes of those two groups appeared the same, indicating that the DIMS group achieved a similar advantage over the SVLs group at all ages. However, the flat regression line of the MFSCLs group suggests that the ▵SE varied little across different ages. The confidence intervals for the DIMS and MFSCL groups began to overlap around age 12, with the predicted regression lines for the two groups intersecting at approximately age 13. In children younger than 12, the MFSCLs group achieved better myopia control than DIMS and SVLs. After 12 years of age, MFSCLs advantage gradually disappeared.
DiscussionTo the best of our knowledge, this is the first study to analyses and compare the efficacy of MFSCLs and DIMS in slowing myopia progression in children with high myopia. Previous studies conventionally focused on low-to-moderate myopia wearing bifocal or multifocal contact lenses, effective between 37 % and 74 %.6,13–16 This study found numerically similar efficacies for either MFSCLs (45.1 %) towards the retardation of myopia progression in children with high myopia. The 1-year myopia progression was −0.39 ± 0.47 D in the MFSCLs group compared to −0.71 ± 0.54 D in the SVLs group. Additionally, MFSCLs have shown greater efficacy in slowing myopic progression, with half of the subjects with an annual refractive change of <0.25 D. We hypothesize that MFSCLs, compared to spectacle lenses, reduce the vertex distance, allowing the multifocal imaging to align more accurately on the retina. However, the distribution and effect of defocus signals on the retina require further investigation. There is limited to no evidence regarding the efficacy of either multifocal soft contact lenses in controlling high myopic progression.19,20 The study by Diaz-Gomez et al. reported that after 2 years treatment, the EDOF soft contact lens group showed significantly less myopia progression than single-vision spectacles in children aged 6–13 years with myopia ranging from −0.75 to −10.00D Mean changes were −0.62±0.30D SE and 0.37±0.04 mm AL for EDOF lenses versus −1.13±0.20D SE and 0.66±0.03 mm AL for spectacles (p < 0.001).19 After three years of treatment, the mean changes in SE and AL were −0.90 ± 0.36 D and 0.55 ± 0.04 mm in the EDOF group, compared to −1.64 ± 0.26 D and 0.97 ± 0.03 mm in the spectacle group, respectively (all p < 0.001).20 The study did not perform subgroup analyses based on baseline refractive error, particularly for high myopia cases (≤−6.00D), which precludes definitive conclusions about treatment efficacy in this specific population. Our study aimed to provide theoretical support for MFSCLs as a potential intervention for high myopia.
Some studies have shown that myopia continues to progress in children with high myopia.24 In Xu's study,25 children with a mean age of 12.54 ± 2.53 years exhibited an annual myopia progression of −0.76 ± 0.46 D and an axial length growth (ALG) of 0.23 ± 0.14 mm. High myopia progression remains a concern, and interventions such as DIMS spectacle lenses have been introduced to address this issue. Liu et al.11 reported a one-year follow-up in highly myopic individuals, showing a change in SE of −0.50 ± 0.41 D in the DIMS group compared to −0.46 ± 0.76 D in the SVL group, with no significant difference between the two groups. The absolute SE change observed with DIMS in their study is similar to our research findings. In clinical practice, some researchers have combined DIMS lenses with low-concentration atropine to enhance their myopia control efficacy. Among children aged 6–14 years with myopia less than −4.00 D, the combination of DIMS lenses and low-concentration atropine achieved better axial length control (0.15 ± 0.15 mm) compared to the DIMS-only group (0.22 ± 0.14 mm).26 In clinical practice, for DIMS lens wearers, regular axial length monitoring is essential. Combination therapy should be considered if progression remains significant despite treatment.27
Previous studies have demonstrated an association between age and myopia progression,11,28 a phenomenon observed in the DIMS and SVL groups. The age-dependent efficacy of MFSCLs suggests that in children younger than 12 years, the MFSCL group exhibited superior myopia control compared to the DIMS and SVLs groups. However, this advantage progressively declined after the age of 12. Therefore, this study suggests that for children under 12 years of age, MFSCLs may be a preferred option for myopia control. For children over 12 years with high myopia, DIMS and MFSCLs demonstrate comparable efficacy and are both viable options. Additionally, previous studies have shown that initial SE can influence myopia progression.10–12 However, our findings indicate that in individuals already classified as having high myopia, myopia progression is no longer affected by SE but is instead influenced solely by the age at the time of intervention. This underscores the importance of early intervention. The absence of a relationship between the initial spherical equivalent and myopic progression suggests that each individual’s “final” amount of myopia that develops is unique. In other words, the initial presence of high myopia does not rule out the possibility of continued progression.
LimitationThe noticeable limitation of our study was the relatively short follow-up period (one year): longer-term follow-up durations are ideal for assessing the year-over-year efficacy of myopia control interventions. In addition, it is not available in the study. The study did not have data on axial length because it was not a routine measurement in clinical practice. Moreover, because this study was retrospective, prospective studies are now necessary to confirm the efficacy of MFSCLs and/or DIMSs in slowing myopic progression in high myopes. We did not use a questionnaire to document the children's daily wearing time. Still, we retrospectively selected participants with good compliance, which offers some assurance regarding adherence to the prescribed wearing regimen.
ConclusionIn summary, MFSCLs and DIMS both effectively limit myopic progression in highly myopic children aged 8–16. This study suggests that MFSCLs may be preferred for children under 12, while DIMS and MFSCLs show comparable efficacy for those over 12 with high myopia. Our findings suggest clinicians may choose appropriate lenses for children with high myopia to achieve ideal myopia control effects.
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Changes of one-year SE grouped by age in SVLs, DIMS, and MFSCLs groups (Mean ± standard deviation).
Note: SE, spherical equivalent; F = Standardized test statistic from one way ANOVA, with P-values. * indicates P-value < 0.05; ** indicates P-value < 0.01.
These authors contributed equally.
Conflict of Interest: The authors have no proprietary or financial interests in the materials and methods used in this study.
Fundings: This research received funding support from Tianjin Key Medical Discipline (Specialty) Construction Project (No. TJYXZDXK-016A), the National Program on Key Research Project of China(2022YFC2404502), The Open Project of Institute of Optometry and Vision Science in Nankai University (Xiaoyan Yang, NKSGY202304, Mengdi Li, NKSGP202307).