Symptoms experienced when using digital devices are known as digital eyestrain (DES) or computer vision syndrome. They can be categorised as either external (associated with dry eye) or internal (related to refractive, accommodative or binocular vision anomalies). In a large cohort of adults with DES, we investigate the prevalence of binocular and accommodative anomalies, contrasting different diagnostic approaches, to evaluate potential mechanisms for the benefit from +0.75D addition lens that has been previously reported.
MethodsParticipants (20−40y) were selected using the Computer Vision Syndrome Questionnaire (CVS-Q) tool as suffering with DES. A comprehensive eye examination was given to each participant, and this paper concentrates on “internal factors”, detected with a refraction and comprehensive testing of binocular and accommodative functions. The effects of low-powered addition lenses (+0.50D, +0.75D, +1.25D; and plano controls) were assessed by double-masked testing with the Wilkins Rate of Reading Test (WRRT) and by subjective preference.
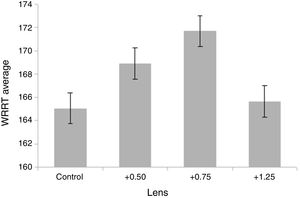
ResultsAs previously reported, most participants showed a subjective preference for one of the three convex lenses we used, with +0.75D chosen most frequently. Performance at the WRRT was significantly improved with +0.50D and +0.75D, but not +1.25D. Using a variety of diagnostic criteria, there were no strong associations between WRRT results or CVS-Q scores and any binocular or accommodation functions. The one finding of significance is that a disproportionate number of participants who benefited from adds had an eso-fixation disparity on the near Mallett unit, although this only affected 5% of the population.
ConclusionsDES is a collection of diverse symptoms that have a multifactorial aetiology. In the sample described here, binocular and accommodative anomalies do not seem to be a major cause of DES. Nevertheless, in view of the multifactorial aetiology it is recommended that patients with the symptoms of DES are assessed with a comprehensive eye examination. Patients with an esophoric fixation disparity on the near Mallett unit are particularly likely to benefit from near additions.
Digital eye strain (DES) is the term used to describe visual and ocular symptoms experienced by users of digital displays and has replaced the previous term, computer vision syndrome (CVS). This change of terminology reflects the broader use of digital devices (e.g., smart-phones, tablet computers, e-book readers) in addition to conventional desktop and laptop computers. The prevalence of DES varies widely depending on diagnostic criteria,1–3 with a review citing recent estimates of prevalence from 31 to 69%.4 There is now a considerable body of work on DES with several thorough reviews.3–8
Typical DES symptoms include eyestrain, ocular discomfort, tired eyes, headaches, blurred vision at both distance and near, double vision and dry eyes.3–7 These symptoms can be divided into two groups: those relating to dry eye issues (burning, tearing, dryness, irritation) and classed as external3–7 and those that emanate from internal factors (anomalies of refraction, accommodation, binocular vision).8,9 This paper concentrates on internal factors contributing to DES, since a previous publication addresses external factors.10 Internal factors contributing to DES can be thought of as any ocular strain or discomfort as a result of straining to maintain good clear and single vision when using a digital device. In summary, these result from uncorrected or under-corrected refractive errors, or binocular and/or accommodative disorders. For example, low levels of uncorrected astigmatism (0.50–1.00DC) can produce a significant increase in DES symptoms11 which is also true for contact lens wearers.12 Accommodative problems can cause asthenopia13,14 and it has been shown that there is little difference between viewing digital devices and hard copy.15 Binocular vision anomalies are a known cause of asthenopia13,14 and have been associated with digital eyestrain.3 There are other possible causes of DES which will not be discussed but include pupil effects,16 blue light exposure,17 and text pattern and monitor flicker causing a form of visual stress.18,19
There are several different approaches to the classification and diagnosis of binocular and accommodative anomalies.20 One approach is to compare patient data with age-related normative values. Well known studies conducted over 70 years ago21–23 collected normative data for both accommodative and binocular measurements. The results of one of these studies21 are commonly referred to as ‘Morgan’s norms.’ It is interesting to note that Morgan defined the normal range as the mean±0.5 standard deviations, which is much more lenient than the usual statistical convention of mean±2 standard deviations24 (see next paragraph). Since then, these values have been readdressed25 and also more binocular and accommodative tests have been developed with studies giving the normative data for these functions (e.g., accommodation facility).26 One of the limits of the older studies is that most evaluate Caucasian populations,21–23,25 and there has been a recent trend to address this issue.27–30
A different approach to diagnosing binocular vision and accommodative anomalies is to adopt a syndromic approach: recognising a pattern of symptoms and test results that characterises a syndrome. Indeed, Morgan did not advocate using his norms in isolation, but rather in detecting syndromes.21 Typically, accommodative anomalies are classified into five groups:13 accommodation paralysis, accommodation insufficiency, ill-sustained accommodation (fatigue), accommodation excess (spasm) and accommodation infacility. Binocular anomalies can be classified with the Duane-White classification to give seven groups: convergence insufficiency, convergence excess, fusional vergence dysfunction (binocular instability), divergence insufficiency, divergence excess, basic exophoria and basic esophoria. More recently, this classification has been modified to three subgroups14 using the distance phoria and AC/A ratio to give low, average or high AC/A groups. This system has been fully described elsewhere.14 Note that some terms described in this classification are not interchangeable with those used in the United Kingdom (UK). For example, in the UK, an isolated finding of a remote near point of convergence (NPC) is referred to as a convergence insufficiency and the Duane-White syndrome of decompensated near exophoria is described as convergence-weakness.13 Additionally, in the UK a greater emphasis is placed on whether the heterophoria is compensated, rather than on its classification.13
Other strategies have been developed to determine whether binocular or accommodative anomalies are significant. One study found that analysing both accommodative and vergence facility tests gave a good indicator to the presence of symptoms when phorias at both distance and near appeared normal.31 Evans13 reviewed the diagnosis of symptomatic heterophoria, which is virtually synonymous with decompensated heterophoria. He noted that in the UK the condition is typically diagnosed using the Mallett fixation disparity test, which has been shown to have reasonable sensitivity and specificity for symptomatic heterophoria.32,33 In North America, where fixation disparity tests are less useful because they tend not to include a foveal fusion lock, Sheard’s and Percival’s criteria may be used.34,35 Evans combined these approaches in a diagnostic algorithm,13 a modified version of which is shown in Table 1. This algorithm has been used in previous research.36,37
Modified Evans Algorithm, as modified for the present research.
| Q1. Are there symptoms? Graded using CVS-Q scores;6−10 score + 1 point11−20 score + 2 points>20 score + 3 points |
| Q2. Is the patient orthophoric on near cover test? If no, score + 1 point. |
| Q3. Is the cover test recovery rapid and smooth? If no, score +2 (+1 if borderline) |
| Q4. Is the Mallett horizontal aligning prism: <1 prism dioptre? If no score +2 |
| Q5. Is the Mallett aligning prism stable (Nonius strips stationary with any required prism)? If no score +1 |
| Q6. Sheard’s criterion: Is the blur point (or break point when blur is absent) opposing the phoria at least twice the size of the measured phoria? If no score +2 |
| Q7. Percival’s criterion: Compare both BO and BI break points. Is the larger break point at least twice the size of the opposing smaller break point? If no score +1 note; BO-base out, BI-base in |
| Q8. Is the dissociated heterophoria stable or unstable (varying over a range of ±2 prism) If unstable, score +1 |
| Q9. Do BO break and BI break points total 20 prism dioptres? If no add score +1 |
| Add total score. If > 5, then decompensated heterophoria or binocular instability |
The CVS-Q38 is a validated questionnaire, has psychometric properties that fit the Rasch model, and has adequate validity and reliability. It can be used to quantify the prevalence of visual and ocular discomfort associated with using a digital display. Thus, it may give an estimate of the severity of DES; but it does not differentiate between internal or external causes. In the present research, the severity of dry eye was assessed with, the “Symptom Assessment in Dry Eye” (SANDE)39 tool and clinical tests based on the 2007 Dry Eye Workshop (DEWS).10,40
The Wilkins Rate of Reading Test (WRRT)41 is a visually demanding test designed to assess visual factors that may impact on reading. It uses simple well-known words so that only very basic reading skills are required, and language skills should have a minimal influence. The WRRT has been used in an assortment of studies,42–44 and has become a widely used test for evaluating visual performance when reading. In dry eye patients, the WRRT has revealed an inverse relationship between severity of dry eye and reading rate.45,46 Previously, it was reported that, on average, participants suffering with DES performed better on the WRRT using +0.75DS near addition lenses and also subjectively preferred these.10
The aim of the present study is to determine if any binocular or accommodative factors could explain why participants suffering with DES both performed better on the WRRT and also subjectively preferred +0.75DS near addition lenses.10 This is investigated in two ways; first by examining individual binocular or accommodative functions. For example, it would make sense if a participant with a near esophoria performed better using +0.75DS addition lenses on the WRRT as these lenses are thought to aid in this condition.13,14 Second, in examining binocular and accommodative functions, there are several diagnostic approaches to determine whether a non presbyopic patient may benefit from the use of near addition lenses and in this study we look at three such approaches.
MethodsParticipantsRecruitment and selection criteria are described elsewhere.10 In summary, participants were aged between 16 and 40 years, had a score of 6 or more (suggestive of DES) on the CVS-Q, spent at least 6h per week on a digital device, and exhibited no recent onset incomitancy or constant strabismus.
ProcedureThe research was approved by the Institute of Optometry Research Ethics Committee and follows the tenets of the Declaration of Helsinki. The procedure has been previously described10 and is summarised below.
All enquirers to the study were given both a copy of the CVS-Q and the SANDE tools and those who fulfilled the entry criteria were invited to attend for an eye examination. A full internal and external examination was carried out, including ophthalmoscopy, slit lamp biomicroscopy for the assessment of dry eye, retinoscopy, subjective refraction and a battery of accommodation and binocular tests (Table 2). If any pathology requiring medical attention was detected or it was felt that the participant would best be managed under the care of their local optometrist, for example a decompensating phoria requiring treatment, the participant was excluded. Only one person was excluded from this study, due to previous refractive surgery.10
Expected norms for accommodation and binocular vision tests. For normally distributed variables, the mean±1 SD is shown (for non-parametric, see first footnote) and the figures are Morgan’s values, except for where a reference is given.
| Accommodation tests | Expected norms |
| amplitude of accommodation (push up method); mean of right and left amplitudes | 18−1/3 age ±2 |
| accommodative facility (±1.50DS)# | 10±5 (Measured binocularly then repeated monocularly on those who did not reach 10. If pass monocularly, considered binocular problem and not included in facility analysis) |
| accommodation lag (MEM) | +0.25 to +0.7514 |
| Binocular vision tests | |
| cover test distance | 1 exo ±2 |
| cover test near | 3 exo ±3 |
| distance phoria (von Graeffe technique) | 1 exo ±2 |
| near phoria (Howell near phoria card) | 3 exo ±3 |
| near point of convergence (NPC) | 2.5±2.5cm |
| near fusional reserve: | |
| base In | blur 13±4, break 21±4, recovery 13±5 |
| base Out | blur 17±5, break 21±6, recovery 11±7 |
| vergence facility (12 base out, 3 base in, flipper form) | 15±314 |
| Eye Genius (Hoya international) version of the Near Mallett fixation disparity aligning prism* | pre-presbyopes: 1Δ or more is abnormal13 |
| Stereopsis | |
| Eye Genius; Pola Test | 40s of arc |
For several tests, results are non-parametric: for the Mallett aligning prism, the normal range quoted is based on the best cut-off for detecting symptomatic patients; for heterophoria tests, results typically only loosely approximate a normal distribution but by convention are described by parametric statistics.
At the conclusion of the examination, the subjective refraction was placed in a trial frame centred both horizontally and vertically, and the WRRT was used to determine the immediate effect of low plus addition lenses. This was done under four conditions using trial lenses (interventions) of plano (control), +0.50, +0.75 and +1.25 lenses worn additionally to the subjective refraction. Neither the participant nor the examiner knew the identity of the lenses during each condition so this process was double masked. Each intervention was randomly assigned a letter (A–D) and the intervention order was ABCDDCBA. The WRRT score is the rate at which each participant read during the WRRT, expressed as the number of correctly read words per minute and determined by the average of two readings per condition; A and A, B and B, C and C, and D and D.10 For each participant, the lens which gave the fastest reading rate was compared to the control condition and the percentage improvement determined to give a WRRT score (%WRRT). If the fastest lens was the control condition, the %WRRT score was recorded as zero. The %WRRT variable therefore indicates the extent to which performance was improved by adds.
Part 1Binocular and accommodative functionsCorrelations were investigated between each function and both the %WRRT and CVS-Q scores. Here, the aim was to determine if a defect in one binocular or accommodative function that could be helped with near addition lenses (eg, near esophoria) could explain both the improvement in reading rates with plus lenses and also higher (more symptomatic) CVS-Q scores. For correlations with amplitude of accommodation, two measurements were examined; since amplitude of accommodation is dependent on age, the age adjusted relative amplitude of accommodation was used (amplitude of accommodation less the expected age norm value) for analysis as well as the overall amplitude. Near phoria was analysed using three approaches: first, by assigning esophores as positive and exophores as negative to give one group and as such determine if there is a correlation between phoria and %WRRT or phoria and CVS-Q. Second, by examining exophoria and esophoria separately to investigate whether either exophoria or esophoria correlated with %WRRT or CVS-Q scores. Third, the direction of phoria was ignored and only the absolute magnitude considered for correlation purposes.
Another way to determine if binocular or accommodative functions play a role in explaining the benefit of low plus addition lens on the WRRT is to look at population norms. As these are widely used in determining whether an accommodative or binocular function is within normal limits, we divided each of the above functions into two groups; one group containing values that fell within or exceeded expected norms (normal group) and the other group containing values which were more than one standard deviation below the expected norm (abnormal group). Although this process of dichotomising continuous variables is in some respects undesirable,47 this was undertaken because normative data are commonly used in this way clinically. Using this method, the normal and abnormal groups were compared with respect to both %WRRT and CVS-Q scores.
Accommodation/binocular functions and fastest lensThe lens which gave the fastest rate of reading was analysed with respect to each of the accommodation and binocular functions. Here, we sought to determine whether one lens condition led to better %WRRT scores in participants with deficient binocular/accommodative functions. This analysis was applied to 102 participants who read fastest with one lens only (5 individuals, read equally fast with more than one lens and were not included). First, the 102 participants were sorted into four groups according to the lens with which they read fastest (either control, +0.50, +0.75 or +1.25). Then, the results for each accommodative/binocular function test was compared in these four groups. Near heterophoria was further analysed by dividing participants into two groups, esophoria and exophoria.
Part 2The relevance of different methods of diagnosing binocular and accommodative anomaliesIn this section, the relationship between %WRRT and CVS-Q scores and binocular and accommodative anomalies are again considered, in the context of different methods of diagnosing binocular and accommodative anomalies. The three diagnostic approaches that are considered are the syndromic approach,14 combined vergence and accommodative facility,31 and the Evans algorithm.13
Syndromic approachParticipants were classified into either a binocular or accommodative subclass using the syndromic approach outlined above. Specifically, this classification was based on the horizontal heterophoria results at distance and at near without considering the AC/A ratio. Each function was determined to be in the normal range only if the results were within 1 SD of the norm (Table 2). Normal and subnormal functions were then grouped together according to which syndrome they most likely belong in the usual classification of accommodative anomalies and Duane-White classification of vergence anomalies as specified by Scheiman and Wick.14 The category “Other” is used for participants whose results did not fit any diagnostic category and “Normal” represents those whose results were normal or who only had one subnormal binocular/accommodative function which was considered insignificant (e.g., an isolated low base in recovery value). %WRRT and CVS-Q scores were then determined for each syndrome.
Vergence and accommodation facility combinedThe finding of Gall and Wick31 that the near vision binocular and accommodative tests that best predict symptomatic cases when distance and near phorias are normal, is a combination of vergence and accommodative facility was investigated in three ways. First, the diagnostic criteria recommended by Gall and Wick were applied to the present data and the participants divided into two groups, normal and abnormal. The abnormal group comprised participants who failed either the vergence or accommodative facility test. %WRRT and CVS-Q scores were compared for the two groups. Second, vergence and accommodation facility results were combined by summing the number of cycles per minute at each test for each participant. Here, correlations were sought between the summed scores and both %WRRT and CVS-Q scores. Third, the second analysis above was repeated but taking account of the prediction that some accommodative problems (all accommodative anomalies except spasm) are likely to be helped by the plus addition lens whilst for a binocular problem, a near esophore would be expected to perform better with plus addition lenses and a near exophore would be expected to perform worse. The correlation between the summed facility score and the %WRRT variable was repeated, but excluding all participants with an exophoria or accommodative spasm.
Evans algorithm analysisThe modified Evans algorithm (Table 1) was used to quantify the extent to which participants had decompensated heterophoria. As esophores would be expected to perform better on the WRRT test with low plus lens and exophores worse, WRRT scores were analysed separately for participants with exophoria and esophoria as previously. Correlations were sought for both %WRRT and CVS-Q scores. For correlations with CVS-Q scores, the first question of the Evans algorithm was deleted as this is derived from the CVS-Q.
ResultsThe results of the dry eye analysis including the SANDE and DEW scores have been discussed previously, as has the analysis of subjective lens preference.10
Descriptive summary of study populationOverall, 107 participants were seen in this study, two thirds of whom were females (64%). The mean age was 31y (SD 5.25; range 20–40). For binocular and accommodative function assessment, one person with an intermittent vertical strabismus was excluded from the analysis of binocular vision data, but not accommodation analyses.
The refractive data are summarised in Table 3.
Summary of refractive data. SER, spherical equivalent refraction.
| Variable | Median (D) | IQR (D) | Range (D) |
|---|---|---|---|
| SER of RE | −0.25 | 1.88 | −7.00 to +3.00 |
| SER of LE | −0.25 | 2.00 | −7.62 to +2.75 |
| Cylinder of RE | −0.25 | 0.50 | −2.50 to 0.00 |
| Cylinder of LE | −0.25 | 0.50 | −2.75 to 0.00 |
SER-spherical equivalent refraction, IQR-interquartile range.
CVS-Q scores did not follow a normal distribution (Shapiro–Wilk test, p<0.001). The median was 16 (IQR 12, range 6–36).
WRRT scoresUnder each of the four conditions (control, +0.50, +0.75, +1.25), the scores did not differ significantly from a normal distribution (Shapiro–Wilk, p>0.07). The reading rate was significantly faster with both +0.75 (p<0.0001) and +0.50 (p<0.001) near addition lenses than with the control lenses (Figs. 1 and 2).10
Binocular and accommodative functionsThe binocular and accommodative data are summarised in Table 4. All correlations investigated between each binocular or accommodative function and either %WRRT or CVS-Q scores were low (τ<0.15) and non-significant (p>0.05).
Descriptive statistics for accommodative and binocular functions and Kendall's tau correlation with both %WRRT and CVS-Q scores.
| Mean/median | SD/IQR 25%–75% Qrt. | Range | Kendall's tau correlation | ||
|---|---|---|---|---|---|
| %WRRT | CVS-Q | ||||
| Amplitude of | 7.00 | 4.50 | 3.00–15.00 | 0.101, | −0.114, |
| Accommodation | 5.50–10.00 | p=0.145 | p=0.102 | ||
| Age adjusted Relative Accommodation | −0.60 | 0.26 | −5.86 to 7.35 | 0.062, p=0.349 | 0.009, p=0.893 |
| Accommodation lag | 1.00 | 1.00 0.50–1.50 | −1.50 to 2.75 | −0.014, p=0.839 | 0.048, p=0.487 |
| ±1.50 facility | 13.00 | 6.0010.0–16.0 | 0.00–24.00 | −0.036,p=0.599 | −0.013,p=0.132 |
| Phoria Distanceeso=plus, exo=minus | 0.00 | 2.001.00–1.00 | −5.00 to 5.00 | −0.047,p=0.492 | −0.005,p=0.946 |
| Phoria Neareso=plus, exo=minus | −2.00 | 5.00−1.00 to 4.00 | −17.00 to 9.00 | −0.047,p=0.492 | −0.005,p=0.946 |
| Exo Nearn=59 | 4.00 | 4.002.00 to 6.00 | 1.00 to 17.00 | 0.094,p=0.330 | −0.071,p=0.946 |
| Eso Nearn=47 | 1.00 | 3.000.00 to 3.00 | 0.00 to 9.00 | 0.079,p=0.473 | −0.041,p=0.692 |
| Near phoria amount(Absolute phoria) | 2.00 | 5.001.00 to 6.00 | 0.00 to 17.00 | −0.070,p=0.319 | 0.085,p=0.226 |
| NPC (near point of convergence) | 3.00 | 3.002.00–5.00 | 2.00–17.00 | 0.002,p=0.973 | −0.006,p=0.935 |
| Vergence facility | 15.00 | 5.0012.00–17.00 | 0.00–25.00 | −0.079,p=0.248 | −0.021,p=0.764 |
| Near aligning prism | 0.00 | 0.000.00 to 0.00 | −9.00 to 3.00 | 0.110,p=0.165 | 0.068,p=0.398 |
| Base in blur | 10 | 6.006.00–12.00 | 2.00–18.00 | 0.108,p=0.300 | 0.123,p=0.241 |
| Base in break | 14 | 810.00–18.00 | 2.00–50.00 | −0.018,p=0.802 | −0.084,p=0.231 |
| Base in recovery | 10 | 6.008.00 to 14.00 | 0.00–30.00 | −0.050,p=0.483 | −0.125,p=0.078 |
| Base out blur | 16 | 15.0010.00–25.00 | 2.00–50.00 | 0.094,p=0.405 | 0.043,p=0.696 |
| Base out break | 30 | 17.0018.00–35.00 | 2.00–50.00 | −0.053,p=0.449 | −0.078,p=0.337 |
| Base out recovery | 25 | 14.0016.00–30.00 | 0.00–30.00 | −0.077,p=0.269 | −0.052,p=0.526 |
In the mean/median column, italic numbers give the mean otherwise numbers represent the median. Similarly, in the spread column, numbers in italic give the standard deviation otherwise the interquartile range (IQR) followed by the 25% and 75% quartiles. For Exo Near and Eso Near, n gives the numbers per group (as describing a sub-group). Kendall's tau correlation is given followed by significance levels.
There was no significant difference between those placed in the normal and abnormal groups for either %WRRT or CVS-Q scores in any binocular or accommodative function examined. Of the 107 subjects examined, 83 were found to have at least one of the three accommodative functions more than 1SD below the expected norm, and for binocular functions, 100 out of 106 were found to have at least one function that was more than 1SD below the expected norm. Note that one participant had an intermittent vertical strabismus and for this individual, many binocular tests could not be performed due to suppression.
As previous research has found that a 15% improvement in the WRRT to be significant for children with reading difficulties,49,50 we examined this subgroup and found there were 9 participants who read more than 15% faster with low plus adds. These 9 participants did not demonstrate a higher prevalence of binocular anomalies than the rest of our population. However, seven of these participants had reduced age adjusted relative amplitude of accommodation. For the 9 participants, the average difference of accommodative amplitude from the age-expected norms (−0.95±1.94) did not differ significantly (p=0.700) from the average for the entire study population (−0.60±0.26).
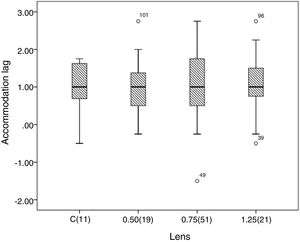
Accommodation/binocular functions and fastest lensFor each accommodation/binocular function, a Kruskal–Wallis analysis showed no difference between the accommodative/binocular variable in the four groups classified according to the lens that gave the fastest WRRT (p>0.175). An example is given in Fig. 3 which shows accommodation lag for the four groups that read fastest with each add. Near heterophoria was also analysed by dividing participants into two groups, esophoria and exophoria and in both groups, there was no difference between the magnitude of the phoria and the lens which gave the fastest WRRT (Kruskal Wallis, p>0.665).
Fastest lens and accommodation lag.
Dark lines give the median, the box shows inter-quartile range, the whiskers give the maximum and minimum values, circles indicate outliers, and bracketed figures give the number of subjects who read the fastest under each lens condition. The groups are the individuals who read fastest with each of the conditions on the x-axis (plano lens (control, C), +0.50, +0.75, +1.25). Note, no significant difference between 4 lens conditions (Kruskal–Wallis, χ2(3)=0.997, p=0.802.
Concerning the Mallett fixation disparity (FD) test, seven participants (7%) were found to have a significant horizontal fixation disparity, indicated by a near horizontal aligning prism (associated phoria). Of these, five read faster with an add than without, and for four of the five participants, the aligning prism was base out prism (not worn in the WRRT). This is an unexpected finding because of the higher prevalence in the general population of exophoria at near.51 Therefore, the literature was searched for studies that provide Mallett unit data on the proportion of participants with a near horizontal fixation disparity (requiring an aligning prism of 0.5Δ or more) who have an eso-disparity (eso-FD). These data are presented in Table 5, which includes a chi-squared comparison with data from the present research, where 80% of those with a near horizontal FD have an eso-disparity. These analyses indicate, the research population with DES had a higher than usual prevalence of significant eso-FD on the near Mallett unit.
Comparison of near horizontal aligning prism data with norms.
| Study | Study population | Near FD results | X2 comparison |
|---|---|---|---|
| Pickwell et al.33 | Total N=383 aged 5−89y (mean age not given) | Symptomatic group: 2 eso-FD, 87 exo-FD, so 2% eso-FD | Symptomatic group: p<0.0001 |
| Asymptomatic group: 8 eso-FD, 46 exo-FD; so, 15% eso-FD | Asymptomatic group: p=0.0005 | ||
| O’Leary and Evans44 | N=58 with exo-FD, mean age 43y | 15 eso-FD, 58 exo-FD, | p=0.0027 |
| N=15 with eso-FD, mean age 16y | So, 21% eso-FD | ||
| Karania & Evans52 | N=105, mean age 37y (SD 18.5y) | 11 eso-FD, 19 exo-FDSo, 37% eso-FD | p=0.0700 |
| Conway et al.53 | N=500, mean age 42y (SD 12y) | Approx.*: 10 eso-FD, 200 exo-FDSo, ∼5% eso FD | p<0.0001 |
| Parmar et al.54 | 34 participants with FD selected from 80, mean age 50y (range 18−92y). | 6 eso-FD, 28 exo-FDSo, 18% eso-FD | P=0.0030 |
Only 1 person required a near vertical prism and this person read significantly faster with +1.25 addition lenses (16% improvement on the WRRT test).
The relevance of different methods of diagnosing binocular and accommodative anomaliesSyndromic approachAs described in the Methods, the cut-off criteria in Table 2 were applied to the data for each participant to determine whether they fell into a syndromic category, according to the usual classification of accommodative anomalies and Duane-White classification of vergence anomalies as specified by Scheiman and Wick.14Table 6 shows the mean or median for the %WRRT and CVS-Q in each of these groups. No differences between the groups were found in either %WRRT scores (χ2 (10)=4.113, p=0.942, Kruskal Wallis test) or CVS-Q scores (χ2 (10)=13.100, p=0.218, Kruskal Wallis test).
%WRRT and CVS-Q data when participants are classified according to the syndromic system.
| SYNDROME | %WRRT | CVS-Q |
|---|---|---|
| Normal (n=34) | 6.71±4.66 | 15.97 (12.50) |
| Basic exophoria (n=0) | ||
| Divergence excess exophoria (n=0) | ||
| Convergence insufficiency exophoria (n=12) | 5.57± 4.32 | 18.07 (11.00) |
| Basic esophoria (n=1) | 3.73* | 36.00* |
| Divergence insufficiency esophoria (n=3) | 8.67±10.78 | 14.00* |
| Convergence excess esophoria (n=18) | 7.06±5.76 | 18.50 (8.75) |
| Fusional vergence dysfunction (n=3) | 0.00 (median)* | 13.00* |
| Accommodative insufficiency (n=16) | 6.39±5.62 | 15.50 (8.50) |
| Accommodative infacility (n=9) | 8.12±4.26 | 10.00 (18.50) |
| Accommodative excess (n=2) | 11.64±14.07 | 11.50 (7.00) |
| Ill sustained accommodation (n=3) | 6.17±4.92 | 18.00 (12.00) |
| Other (n=5) | 4.48±3.86 | 8.00 (5.50) |
Mean±SD or, if non-parametric, median and IQR. n gives the number in each subclass. Note, 5 in group Other consisted of 5 individuals with an isolated finding of high accommodative lag.
Using the diagnostic criteria of Gall and Wick (see Methods),31 28% of the study population were abnormal. When the normal and abnormal groups were compared for both %WRRT and CVS-Q, these variables were not significantly different in the groups (p>0.24). Similarly, combining both the vergence and accommodation facility for a summed scored did not give significant correlations with either %WRRT or CVS-Q. Finally, excluding participants who had either an exophoria or accommodation spasm, in the remaining subgroup there was no significant correlation between the summed vergence and accommodative facility and %WRRT scores.
Evans algorithm analysisThe correlations between the Evans algorithm scores and %WRRT were low and not significant for both the esophoria (τ=−0.09, p=0.39) and exophoria (τ=0.10, p=0.31) sub-groups. For the CVS-Q scores, the correlation between the algorithm score (excluding first question) and CVS-Q for all participants was low and insignificant (τ=−0.02, p=0.73).
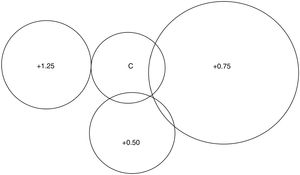
DiscussionIn this population of over 100 adults with DES, 80% expressed a preference for reading with low plus adds, and 88% read faster with the adds. Fifty-one percent of study participants read fastest with an add of +0.75.10 The present manuscript investigates whether binocular and accommodative anomalies explain the benefit from adds. There is a variety of approaches to the diagnosis of binocular vision anomalies, and the results were therefore analysed in different ways. Only one approach yielded a significant finding: a higher than expected proportion of participants exhibited a near eso-fixation disparity on the Mallett unit, indicated by a significant base out aligning prism (associated phoria). However, this only affected five participants, so does not provide an explanation for the many participants who read faster with adds.
In most respects, the analyses of binocular vision and accommodation variables were unproductive in terms of explaining the benefit from low plus adds. For example, the syndromic approach would predict that the greatest benefit from adds would be exhibited by participants with accommodation insufficiency or convergence excess esophoria. This was not found to be the case according to the Duane-White classification and Evans’ algorithm also did not explain the results. Using the Mallett fixation disparity test, five participants had an abnormal eso-fixation disparity and benefited from plus. This indicates that in some cases low plus adds are helpful in DES owing to their correction of a decompensated esophoria, but this only applied to 5% of the population with DES.
A previous randomised controlled trial of the Mallett aligning prism at improving speed of reading (WRRT) found a significant effect in exophoric participants.44 A similar effect was not apparent for esophoria, although there were only 15 participants with an esophoric aligning prism. The effect of low plus on WRRT has been investigated in a randomised controlled trial and a significant effect in presbyopes, but not pre-presbyopic hyperopes was found.55 However, participants were not differentiated into those with esophoria or symptoms. The three adds used in the present research (+0.50, +0.75, +1.25) are in the range of adds typically prescribed to neutralise eso-fixation disparity on the Mallett unit.13
The number of participants with a fixation disparity on the near Mallett unit is small (7 had a horizontal fixation disparity, one a vertical). For the horizontal disparity, 4 out of the 5 who performed best with one of the addition lenses needed base out prism which suggests that the plus addition lenses were neutralising the eso-disparity. The one participant with vertical prism read the fastest with the +1.25 lens and it may be speculated that this lens improved the clarity of the image with an associated improvement in sensory fusion.13
The improvement in WRRT with low plus adds was modest10: 24% read more than 10% faster with adds and 8% read more than 15% faster. In research with the WRRT for children with reading difficulties, two independent research groups have found the 15% criterion to be most appropriate,49,50and this agrees with a Delphi study of practitioners who commonly use the WRRT.56 In the present research, the results for the 9 participants who read more than 15% faster with low plus adds were examined and seven participants had reduced amplitude of accommodation compared to the equivalent age expected norm. However, for this group the age-expected norms did not differ significantly from the population average (p=0.70).
The WRRT tasks each take one minute, although the small crowded text is designed to make the test sensitive to problems that with larger text only occur after reading for a prolonged period.41 Nonetheless, it is possible that the short duration of the WRRT or some other feature of its design makes it insensitive to binocular/accommodative anomalies. For example, adults may be able to exert extra effort for a brief period to overcome binocular/accommodative anomalies. Such an effort could be at the expense of symptoms, causing DES symptoms which fail to correlate with improvement at WRRT. However, this hypothesis is disconfirmed by other research revealing a significant improvement in WRRT performance in adults when decompensated heterophoria44 or when early presbyopic refractive errors55 are corrected. Also, the absence of a significant association between CVS-Q symptoms and binocular/accommodative anomalies in the present data suggest, these anomalies are not a major factor in most cases of DES.
A potential limitation is that for participants who read fastest with the control (plano) condition, %WRRT was recorded as zero rather than as a negative value. This approach was taken because plano lenses would not be considered as an intervention. Nonetheless, this approach meant that variance relating to the slowing effect of adds for these participants was discarded. This is unlikely to have a significant impact on the analyses because there were only 11 participants who read faster with plano and two who read equally fast with a low plus lens and plano. Of the 11, 7 were exophoric, three esophoric, and one orthophoric. Another limitation is the lack of a control group without DES.
It is likely that a variety of reasons account for the benefit from low plus adds. The placebo effect is a consideration, although this effect is variable and should not be exaggerated.57 Accommodative relief from low plus may have been beneficial in some cases even in the absence of accommodative anomalies. The WRRT was performed at the end of a long examination which many participants reported to be tiring. Further, most participants attended during their normal work hours or at the end of a work day, further exacerbating the tiredness they would experience as a result of the eye examination. Of those that showed significant improvement (>15%), 7 out of the 9 had reduced amplitude of accommodation further suggesting that overall accommodative relief may be one mechanism involved. Another potential explanation for the benefit of low plus adds is that tear film instability interacted with real-time accommodation in a way that caused low plus lenses to help. However, a study that recorded accommodation objectively when participants with DES read with +0.50 found no such effect.58
Previously for this present population, we found that dry eye disease contributed to the DES symptoms by finding a correlation between CVS-Q scores and two dry eye tools.10 DES is comprised of both external factors (dry eye) and internal factors (refractive/binocular/accommodative anomalies). No correlations were found between the CVS-Q tool and any binocular or accommodative function, even considering different methods of diagnosing these anomalies. One explanation may be that the CVS-Q tool is better at detecting dry eye symptoms than internal symptoms (binocular/accommodative). Further, it may be that in some cases, both external and internal symptoms are required for DES symptoms to become significant. The difficulty in disentangling the symptoms of dry eye from those of binocular vision anomalies is highlighted by one study which found that the CISS questionnaire (designed to detect symptoms of a binocular vision anomaly) shows a higher correlation with a dry eye questionnaire (CLDEQ-8) than the correlation of CLDEQ-8 with a different dry eye questionnaire (OSDI).59 Previous research has found only a low correlation between symptoms and some binocular vision parameters.60,61 In summary, it seems likely that dry eye is a greater contributor than internal factors to the symptoms of DES in the present population. Although reading rates have been shown to be slower with dry eye,45,46 it seems unlikely that dry eye can explain the preference for low plus adds and their beneficial effect on rate of reading.
Notwithstanding the lack of significant associations between most binocular/accommodative functions and %WRRT or CVS-Q scores, the prevalence of binocular/accommodative anomalies was high. Seventy-seven percent (83) participants had at least one subnormal accommodative function and 93% had one subnormal vergence function. When test results are combined, the model of Scheiman and Wick14 gave 32% of participants classified as normal, Gall and Wick31 facility analysis gave 72% as normal, and Evans’ algorithm13 for decompensated heterophoria and binocular instability gave 73% as normal (this algorithm does not include accommodative anomalies). The present work should not be interpreted as critical of any model and each has merits.
Although the present data indicate that binocular anomalies are not a major cause of DES, the results indicate they may be a contributory factor in some cases. A full eye examination, including an assessment for dry eye and binocular and accommodative anomalies, seems appropriate in patients bothered by the symptoms of DES. Although the CVS-Q scores showed good correlation with two dry eye tools,10 the results of this study should be taken with care as this questionnaire has yet to be validated in English. This is a recommended topic for future research.
Compared with the control condition, 51% of participants performed better with +0.75 and 19% performed better with +0.50 addition lenses. It can be inferred that these additions may help reading and near tasks and may be a helpful prescription for some patients with DES.
ConclusionsLow plus addition lenses are appreciated by many DES sufferers who also read faster with them. For a small proportion (∼5%) of these cases, this benefit seems to be attributable to the correction of a decompensated near esophoria, as revealed by the Mallett unit. Otherwise, although binocular and accommodative anomalies are prevalent in DES, they cannot explain the benefit of low plus addition lenses. It is possible that the accommodative relief offered by these lenses is a simple explanation of their benefit. Finally, dry eye as well as binocular and accommodative anomalies, is common in people with the multifactorial condition of DES. A comprehensive eye examination is warranted to detect these problems.
DisclosureThe research was funded by Hoya Holdings NV, the Netherlands. Hoya as funder had no role in the data collection and analysis or preparation of the manuscript.
Conflicts of interestBE has received honoraria from Hoya for lectures and participation in KOL events.
The authors are grateful for Hoya Holdings NV for funding and to Dr Natalia Vlasak and Olga Prenat for their support. Gratitude is also expressed to Dr. María del Mar Seguí and Dr Elena Ronda of the University of Alicante for permission to use the CVS-Q and to Mr Ojas Mehta of Massachusetts Eye and Ear for permission to use the SANDE questionnaire.