To compare objective peripheral refraction measured with an open-field autorefractor without cycloplegia with the values obtained with fogging lenses or with cycloplegia to inhibit accommodation.
MethodsFor one hundred and sixty young adults aged 18 to 28 (mean 21.5±2.3 years) their refraction was measured with the Grand Seiko (GS) autorefractor at the center and at four peripheral locations in the nasal and temporal directions under three different conditions: 1) without cycloplegia (GS); 2) without cycloplegia, but using a +2.00D fogging lens (GS_2D) and 3) with cycloplegia (GS_cycl).
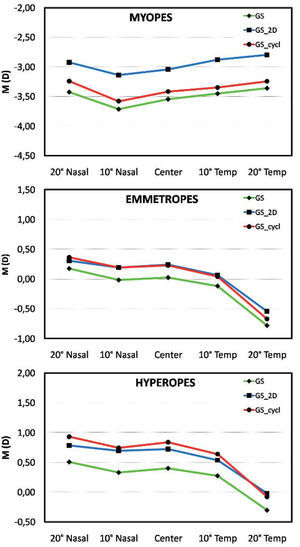
ResultsMean spherical equivalent refraction (M) was significantly more negative with the GS method in the hyperopic group for central and peripheral refraction, and only at the center and at 10° nasal eccentricity for the emmetropic group (P<0.05, Kruskal-Wallis). Paired comparison showed that differences of M values across techniques were larger for the GS-vs.-GS_2D comparison in myopes and emmetropes, and for the GS-vs.-GS_cycl one in hyperopes (P<0.001, Wilcoxon Signed Ranks Test). The gap between M values for all paired comparisons remained almost constant across all eccentric positions under analysis.
ConclusionsFogging lenses used with open-field autorefraction up to 20° in the nasal and temporal fields seem to provide similar accommodative relaxation to that provided by a cycloplegic. This is particularly important when refracting emmetropes and hyperopes. Moreover, this behavior seems to be independent of the eccentricity at which measurements are taken.
Comparar las medidas objetivas de refracción periférica realizadas sin cicloplégico con los valores obtenidos con “lentes de miopización” o con cicloplegia, ambas técnicas utilizadas para inhibir la acomodación.
MétodosSe midió la refracción a 160 adultos jóvenes, con edades comprendidas entre 18 y 28 años (media=21,5± 2,3 años), con un autorrefractómetro Grand Seiko (GS), tanto en el centro del campo visual como en 4 regiones de la periferia situadas nasal y temporalmente, y todo ello en 3 condiciones diferentes: 1) sin cicloplegia (GS); 2) sin cicloplegia, pero utilizando una lente translúcida de +2.00 D (GS_2D) y 3) con cicloplegia (GS_cycl).
ResultadosLa media del equivalente esférico de la refracción (M) resultó ser significativamente más negativa en la condición GS en el grupo de los hipermétropes en lo que respecta a refracción central y periférica, mientras que en el grupo de los emétropes sólo ocurrió esto en el centro y a una excentricidad de 10° nasal (P<0,05, Kruskal-Wallis). La comparación por pares de muestras relacionadas reveló que la mayor diferencia de M entre distintas condiciones se obtuvo al comparar GS y GS_2D en el grupo de los miopes y en el de los emétropes, y al comparar GS y GS_cycl en el de los hipermétropes (P<0,001, contraste de Wilcoxon de rangos con signo). La discrepancia entre valores de M para las distintas comparaciones por pares se mantiene prácticamente constante para todas las excentricidades analizadas.
ConclusionesLas lentes de miopización, utilizadas con un autorrefractómetro con ventana de observación para medir excentricidades de hasta 20° en las direcciones nasal y temporal parece que logran una relajación acomodativa similar a la que proporciona el agente cicloplégico. Esto resulta especialmente relevante cuando se evalúa la refracción en emétropes e hipermétropes. Además, este comportamiento parece ser independiente de la excentricidad en la que se realiza la medida.
The primary function of the peripheral retina is motion detection. This region is considered to have low ability for detail resolution, dominated by a considerable amount of astigmatism and field curvature.1
Peripheral refraction has been thoroughly studied over the last years, partly because myopia progression is considered to be associated to the hyperopic defocus of the images produced on the peripheral retina2,3 and to the potential influence on the emmetropization process of the human eye.2,4,5 On monkeys, it was possible to verify that the peripheral retina plays a role in myopia development during form deprivation.6-8
Even though early reports on peripheral refraction date back as early as the 1930's,9 this subject has been more extensively studied since the 1970's. The techniques of subjective refraction and retinoscopy were approached by Rempt et al., Millodot and Lamont and Wang et al.10-12 Peripheral refraction was also studied by means of objective and manual optometers; 13,14 open-field autorefractors,15,16 photorefraction,4 double pass method,17 and clinical aberrometers.18 Several factors with the potential to affect peripheral refraction were also analyzed; namely age,2,19 refractive error,4,20 eccentric horizontal and vertical retinal locations,21 different fixation distance22 and the impact of anterior cornea reshaping with orthokeratology16 or LASIK.23
Several of the cited studies were intended to analyze peripheral refraction using a number of instruments,24 either under cycloplegia24 or without cycloplegic agents.21
Peripheral refraction has also been studied with the goal of obtaining a theoretical model of the ophthalmic lenses that could correct the peripheral refractive error.25
Refractive error in the peripheral retina, as compared to central refraction, shows a myopic trend in emmetropes and hyperopes. On the other hand, myopes present a peripheral refraction that is less myopic or more hyperopic than the central measurement;4,5,26 this fact has been more intensively studied for the horizontal meridian of the eye.21
The application of autorefractors to obtain peripheral refraction data raises the question of which is the effect of accommodation and which is the validity of such measures without cycloplegia. Other alternatives to the use of a cycloplegic, such as the use of fogging lenses, have demonstrated to be effective in evaluating central refraction.27 However, when it comes to peripheral refraction, the effectiveness of fogging lenses to avoid the accommodation effects in young adults being measured with an open-field autorefractor has not been investigated yet. The goal of this study is to evaluate whether or not peripheral measurements with an open-field autorefractor, up to 20°, are affected by the use of a fogging lens to inhibit the accommodative action, particularly in emmetropic and hyperopic young-adult populations.
MethodsThe population under test consisted of one hundred and sixty young university students, whose ages ranged from 18 to 28 years (mean ± SD: 21.5 ± 2.3 years). Of them, 114 were female (71.3%) and 46 male.
In order to separately analyze the potential effect of fogging lenses and cycloplegia on accommodation during refraction, three refractive groups were established according to their spherical equivalent [M=Spherical+Cylinder/2, where the values correspond to central refraction measurements under cyclopegia], as follows: myopes (M≤-0.50; n=56; 35.0%), emmetropes (-0.5028;29
After explaining them the nature of the study, each patient signed a consent form before being enrolled. The research followed the Declaration of Helsinki rules and was reviewed and approved by the Scientific Committee of the School of Sciences of Minho University (Portugal). The inclusion criteria required that the subjects did not suffer from any current eye disease or injury, were not taking any ocular or systemic medication that could affect the accommodative response and had best corrected visual acuity of 20/20 or better in each eye. The intraocular pressure was checked with a noncontact tonometer (Nidek Model NT-4000).30
The autorefraction data was obtained with an open-field instrument, the Grand Seiko Auto Ref/Keratometer WAM-5500 (Grand Seiko Co., Ltd., Hiroshima, Japan). This instrument had been used and tested by a number of authors to measure refraction in the central and peripheral retina.19,31
The illumination of the room was adjusted so that the pupil size was greater than 4mm, which was achieved in all cases with and without cycloplegic agent. The fixation target was placed at a distance of 5 meters from the patient's corneal vertex and consisted of a 5 LED arrangement in the horizontal direction: a central one, two to its right and two to its left. Each LED was separated from the adjacent ones by an angular distance of 10°, measured at the patient's position. The subject was seated with the head stabilized by a chin-rest so that the eye was aligned with the central LED. For the right eye, the fixation of an object positioned at the right hand of the central point (nasal visual field in the eye's primary position) matches the temporal retina measures. For the right eye of each individual and for each retinal location under analysis, three readings were taken and averaged, considering the center of the pupil as the reference point of measurement. The left eye was able to see the same target under the same conditions (naked eye, with a +2.00 D fogging lens or under cycloplegia).
The refraction measurements were carried out in three different conditions, and always in this sequence: 1) without cycloplegia (GS); 2) without cycloplegia with the +2.00 D fogging lenses placed 12 mm away from corneal vertex (GS_2D), and 3) with cycloplegia (GS_cycl). Following the measurement with fogging lenses, cycloplegia was achieved by instilling twice in each eye one drop of 1% cyclopentolate, with a 5 minute interval between drops. After a 35 min wait we were able to perform the measurements corresponding to the cycloplegia condition.
Participants were not wearing their correction; they were only wearing the fogging spectacle lens (+2.00 D), consisting of convex-concave (meniscus) lenses. The fogging lenses were mounted on a trial frame and placed at a distance of 12 mm from the corneal vertex. The naso-pupilar distance was adjusted for each subject. In a recent study, the authors have shown how additional relaxation of accommodation can be achieved using +2.00 D fogging lenses for central refraction using as well an open-field autorefractor.27
Descriptives (mean±SD) were obtained for the refraction vector components M, J0 and J45 emerged from the Fourier expansion of the refraction function, as recommended by Thibos.32
For those measurements obtained with the +2.00D fogging lenses, this dioptric value was subtracted from the spherical component of the refraction in clinical notation before converting to vector components. This value is the equivalent refraction in the ocular plane for a working vertex distance of 12 mm.
The SPSS statistical package v.15 (SPSS Inc., Chicago, IL, USA) was used to conduct the statistical analysis. The Kolmogorov-Smirnov Test was applied to evaluate the normality of data distribution. The Kruskal-Wallis Test and ANOVA were completed to evaluate if different conditions yielded statistically different values of M, J0 and J45 for non-parametric and parametric variables. When normality could not be assumed, the Wilcoxon Signed Ranks Test was used to perform a paired comparison between techniques, whereas the Paired-Samples Test was used for normally distributed variables.
ResultsThe central objective refraction obtained under cycloplegia for the whole sample, GS_cycl, ranged between -9.00 D and +2.25 D for the value of the sphere, with a maximum astigmatism of -2.25 D. The mean value of the spherical equivalent (M) refraction was -0.85±2.27 D (GS_cycl). A total of 35.0% of the sample had myopia (M=-3.42±2.05D), 32.5% had emmetropia (M=+0.23±0.34D) and 32.5% had hyperopia (M=+0.84±0.31D) according to the criteria defined above, under the methods section.
Table 1 presents the mean and standard deviation of the M component obtained both for the entire sample as well as for each of the three refractive groups, and under the different measuring conditions (GS, GS_2D and GS_cycl). This table also presents the statistical significance for comparisons among different measuring techniques and eccentric position in the nasal and temporal fields. All values found for GS_cycl and GS_2D were more positive or less negative than those obtained with GS (without cycloplegic or fogging lens). Statistically significant differences across all techniques at different eccentric points were found for hyperopes except at 20° in the temporal field and for emmetropes in the temporal field and 20° in nasal fields (P<0.05, Kruskal-Wallis Test). No statistically significant differences were found across techniques at each of the eccentric points in myopes (P>0.05) although there is a clinically significant trend towards more negative values with GS. Figure 1 graphically illustrates these differences.
Descriptive statistics (mean, SD) of M component for the total sample and for each refractive group under different examination conditions: autorefractor GS, GS_cycl and GS_2D (values are expressed in diopters)
| GS | GS_cycl | GS_2D | P | ||
| Total n=160 | 20 Nas | -0.98 ± 2.40 | -0.71 ± 2.40 | -0.67 ± 2.22 | 0.060b |
| 10 Nas | -1.20 ± 2.34 | -0.95 ± 2.40 | -0.81 ± 2.22 | 0.008b | |
| Center | -1.10 ± 2.22 | -0.85 ± 2.27 | -0.75 ± 2.11 | 0.002b | |
| 10 Tem | -1.16 ± 2.08 | -0.95 ± 2.13 | -0.81 ± 1.95 | 0.017b | |
| 20 Tem | -1.53 ± 1.86 | -1.38 ± 1.90 | -1.16 ± 1.78 | 0.117b | |
| Myopes n=56 | 20 Nas | -3.43 ± 2.57 | -3.24 ± 2.45 | -2.93 ± 2.37 | 0.491b |
| 10 Nas | -3.72 ± 2.35 | -3.58 ± 2.32 | -3.14 ± 2.31 | 0.356b | |
| Center | -3.55 ± 2.15 | -3.42 ± 2.05 | -3.04 ± 2.10 | 0.436b | |
| 10 Tem | -3.46 ± 1.97 | -3.35 ± 1.90 | -2.88 ± 1.98 | 0.279b | |
| 20 Tem | -3.36 ± 1.97 | -3.24 ± 1.96 | -2.80 ± 1.98 | 0.201b | |
| Emmetropes n=52 | 20 Nas | 0.18 ± 0.54 | 0.36 ± 0.51 | 0.31 ± 0.60 | 0.207a |
| 10 Nas | -0.02 ± 0.44 | 0.19 ± 0.42 | 0.19 ± 0.46 | 0.030b | |
| Center | 0.03 ± 0.34 | 0.23 ± 0.34 | 0.24 ± 0.33 | 0.002b | |
| 10 Tem | -0.12 ± 0.39 | 0.04 ± 0.41 | 0.07 ± 0.42 | 0.061b | |
| 20 Tem | -0.78 ± 0.73 | -0.67 ± 0.80 | -0.55 ± 0.79 | 0.296a | |
| Hyperopes n=52 | 20 Nas | 0.51 ± 0.56 | 0.93 ± 0.57 | 0.79 ± 0.46 | <0.001b |
| 10 Nas | 0.33 ± 0.44 | 0.74 ± 0.40 | 0.70 ± 0.39 | <0.001b | |
| Center | 0.40 ± 0.35 | 0.84 ± 0.31 | 0.72 ± 0.25 | <0.001b | |
| 10 Tem | 0.28 ± 0.35 | 0.64 ± 0.37 | 0.54 ± 0.28 | <0.001b | |
| 20 Tem | -0.30 ± 0.55 | -0.08 ± 0.67 | -0.02 ± 0.65 | 0.056a |
n: number of subjects; GS: autorefraction noncycloplegic; GS_2D: autorefraction with fogging lenses +2.00D noncycloplegic; GS_cycl: autorefraction with cycloplegic.
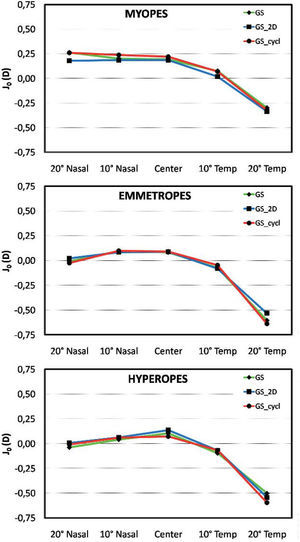
No statistically significant difference was found across techniques neither at the center nor at eccentric locations for the astigmatic components J45 and J0 (P>0.05, Kruskal- Wallis Test), as illustrated in figures 2 and 3.
Table 2 presents the differences corresponding to paired comparisons between techniques for the three refractive groups and at different eccentric locations. This table does not attempt to compare M values between different refractive groups, which of course, are expected to change according to refractive classification of patients. Instead, this table provides information about how the techniques compare to each other regarding refractive status and eccentric location. In this sense, we observe that there are statistically significant differences between those techniques that aim for the relaxation of accommodation (GS_2D and GS_cycl) and GS (P<0.001) but not between GS_2D and GS_cycl, with the exception of the myopic group. Mean differences between methodologies for different eccentric points within each refractive group range from -0.02±0.41 for GS_cycl minus GS_2D in the emetropic group to -0.54±0.50 for GS minus GS_2D in the myopic group. None of the comparisons considering eccentric location as a factor showed statistically significant differences (P>0.05, Kruskal-Wallis Test).
Paired comparison for the differences between techniques, M component (values are expressed in diopters)
| GS – GS_cycl | P | GS – GS_2D | P | GS_cycl – GS_2D | P | ||
| Myopes | 20 N | -0.19 ± 0.21 | <0.001a | -0.50 ± 0.47 | <0.001a | -0.31 ± 0.40 | <0.001a |
| 10 N | -0.13 ± 0.21 | <0.001a | -0.58 ± 0.53 | <0.001a | -0.44 ± 0.51 | <0.001a | |
| C | -0.13 ± 0.20 | <0.001a | -0.50 ± 0.58 | <0.001a | -0.37 ± 0.56 | <0.001a | |
| 10 T | -0.10 ± 0.17 | <0.001a | -0.57 ± 0.55 | <0.001a | -0.47 ± 0.54 | <0.001a | |
| 20 T | -0.12 ± 0.24 | <0.001a | -0.56 ± 0.37 | <0.001a | -0.44 ± 0.39 | <0.001a | |
| Emmetropes | 20 N | -0.19 ± 0.27 | <0.001b | -0.13 ± 0.44 | 0.033b | 0.06 ± 0.53 | 0.449b |
| 10 N | -0.21 ± 0.24 | <0.001a | -0.21 ± 0.35 | <0.001a | 0.00 ± 0.40 | 0.825a | |
| C | -0.20 ± 0.23 | <0.001a | -0.22 ± 0.26 | <0.001a | -0.01 ± 0.28 | 0.647a | |
| 10 T | -0.16 ± 0.30 | <0.001b | -0.19 ± 0.30 | <0.001a | -0.03 ± 0.33 | 0.216a | |
| 20 T | -0.11 ± 0.40 | 0.055b | -0.24 ± 0.40 | <0.001b | -0.13 ± 0.45 | 0.046b | |
| Hyperopes | 20 N | -0.43 ± 0.34 | <0.001b | -0.28 ± 0.34 | <0.001a | 0.15 ± 0.39 | 0.021a |
| 10 N | -0.41 ± 0.34 | <0.001a | -0.37 ± 0.32 | <0.001b | 0.05 ± 0.29 | 0.302a | |
| C | -0.44 ± 0.33 | <0.001a | -0.32 ± 0.26 | <0.001a | 0.12 ± 0.29 | 0.011a | |
| 10 T | -0.37 ± 0.34 | <0.001a | -0.26 ± 0.29 | <0.001a | 0.10 ± 0.30 | 0.023a | |
| 20 T | -0.22 ± 0.43 | <0.001b | -0.28 ± 0.32 | <0.001b | -0.06 ± 0.48 | 0.379b |
GS: autorefraction noncycloplegic; GS_2D: autorefraction with fogging lenses +2.00D; noncycloplegic; GS_cycl: autorefraction with cycloplegic.
With the results of the present study we have showed that relaxation of accommodation can be attained using fogging spectacle lenses, when peripheral measurements are carried out with an open-field autorefractor. In a previous study we had already shown that the same could be achieved for central measurements,27 so in this sense, the present results could be expected. However, after that study, we asked ourselves if prismatic effects or oblique incidence of light could be a source of error when peripheral measurements were to be obtained through the fogging lens. Nevertheless, the present study also showed that the influence of oblique incidence of light, with potential effects on astigmatism or prismatic effects, is negligible when using this methodology. This is supported by the absence of differences in peripheral refraction (particularly regarding the J0 and J45 components) when using the fogging lenses, as compared with the use of cycloplegic agent alone. The study further showed that this effect can be achieved in emmetropes and hyperopic young adults where the accommodative system is very active.
Even though this work aimed to analyze peripheral refraction under several measuring conditions using a sole instrument for different refractive groups, when conducting a first analysis of the results obtained, we verified that the differences across techniques found in peripheral refraction are similar to those observed for the central measurements. As expected, this study also showed that peripheral refraction is more astigmatic than central refraction and is asymmetric, in the sense that the astigmatism is more accentuated on the temporal retina than on the nasal retina. This horizontal asymmetry is higher for hyperopes and emmetropes than for myopes, which is in agreement with previous studies.4,19,21,22
When analyzing the various refractive components individually, the component M demonstrated that peripheral refraction on hyperopes and emmetropes was more myopic in the temporal retina. Meanwhile, at the same point, for myopes, peripheral refraction presented slightly less myopic or more hyperopic values than those found for central refraction. At the nasal retina, and for all refractive groups, the values obtained were more hyperopic or more positive than those found in the central region. This trend was also verified by Atchison et al. when analyzing the influence of age on peripheral refraction using the same measuring technique (GS). In a group of young adults (24±3 years), for the point 20° in the temporal retina, they found more myopic values, in approximately -0.70D for emmetropes and similar values for an adult population of hyperopes by -0.80D (age 59 ± 3 years). They also found that there were small variations between the nasal and the central region of the retina, with smaller differences being observed in the myopic group, which is in good agreement with our results.19 In another study conducted by Seidemann et al. using a different autorefractor the results were slightly different, as all refractive groups showed a trend towards more myopic values in the periphery.
Similarly to our work, in that study smaller changes were found in the nasal retina for all refractive groups.4 Similar values were also reported by Calver et al. and by Atchison et al., who presented results for myopes and emmetropes only.4,21,22
Peripheral refraction studies usually reveal higher values of astigmatism on the peripheral retina than in the center, reaching its highest values in the temporal retina. When analyzing the astigmatism J0 separately, we also observed an asymmetry between the temporal field and the central retina, being most negative at the temporal side by -0.63D for hyperopes, -0.68D for emmetropes and -0.47D for myopes. Concerning the nasal retina, the refractive alteration, as compared to the center, was less accentuated than for the temporal retina (-0.14D for hyperopes, -0.09D for emmetropes and +0.09D for myopes). These results are in agreement with Atchison et al. for the three refractive groups.19 Calver et al. presented a curve and values very similar to the ones found in the present study for the astigmatic component J0.22 Similar results were also described by Atchison et al. for the emmetropic group, and mainly for a myopic group having refractive characteristics similar to those of the present study. Concerning the results for the 20° region, they also observed that the nasal retina presented a dispersion of values in relation to the adjusted curve and more positive values of J0, compared to the center.21
Astigmatism J45 varies in an almost linear way between the nasal and the temporal retina, but with a smaller amplitude for emmetropes (J45_20°nasal – J45_20°temporal = +0.05D). Values of this magnitude were also found by Atchison et al., even if their tendency was the opposite. A higher magnitude was found for the hyperopic and myopic group (+0.15D). Regarding myopes, Atchison et al. found amplitudes of approximately -0.25D, while Calver et al. found higher values, of about 0.60D.21,22
Beyond the agreement with previous studies analyzing similar eccentric areas of the visual field, the present results showed that the same difference observed for the central refraction between methods attempting to control the accommodative response is maintained in the periphery, across the horizontal meridian up to 20°. Regarding the particular case of direct comparison between pharmacological and optical relaxation of the accommodative response during refraction, no statistically significant differences were found for the three refractive groups between GS_cycl and GS_2D at all eccentric locations along the horizontal meridian, with the only exception of myopes, for whom the fogging lenses seem to render higher accommodative control than cycloplegia. At present we do not have an explanation for this different behavior. In clinical terms, the fact that both accommodative control strategies behave in an effective and similar way in emmetropes and hyperopes is important, as a shift towards myopia due to accommodation could misclassify a subject as myopic or less hyperopic.33,34
One limitation of the study is the fact that using the same power for the fogging lens, irrespective of the patient's ammetropia, could result in a slightly different accommodation control. This seems to be particularly important in myopes, where higher differences between cycloplegic and fogging lens scenarios seem to be present. However, using the same lens allows us to keep the experimental conditions constant across all refractive groups. In this study, we attempted to proof that fogging lenses can be successfully used to perform peripheral refraction, in the same manner it was to measure central refraction,27 and this goal seems to be achievable with no apparent influence on peripheral astigmatism when compared with the no-fogging-lens situation.
Therefore, the measurement of central and peripheral refraction using fogging lenses to replace the use of cycloplegic is valid in young adults, particularly in emmetropes or hyperopes. Surprisingly, the use of fogging lenses doesn’t have a significant impact on peripheral astigmatism because of the oblique incidence of light on the fogging lens. This is somewhat expected if we bear in mind that the light passes through the lens perpendicularly, since only the eye is turned. The potential impact of oblique incidence of light on peripheral astigmatism could be more important if the instrument were displaced or the head itself turned,35 as opposed to the approach commonly used, where the subject only turns their eyes. This could be at least in part attributed to the small entrance pupil of this instrument.36 We cannot ensure that the same results would be obtained when using other instruments.
ConclusionThe use of fogging lenses seems to provide an accommodative relaxation comparable to that obtained with cycloplegic in young-adults, without any measurable effect on peripheral refraction related to oblique incidence or prismatic effects. These results are valid for the Grand Seiko open-field autorefractor when used to assess eccentric locations up to 20° in the nasal and temporal fields. The present results have potential application in mass field studies involving population where accommodative control is more critical and cycloplegic administration less desirable, such as in children screening, and particularly when conducted by non-medical staff. However, cycloplegia has the additional advantage of achieve pupil dilatation, thus allowing more peripheral data to be obtained.
We thank J. A. Díaz-Rey for his contributions in the preliminary ophthalmological examination of patients and administration of cycloplegic agent. None of the authors has a commercial or financial interest in the instruments presented here.