To compare improvements in visual acuity (VA) and stereoacuity between active vision therapy (AVT) and conventional patching therapy in children with amblyopia.
MethodsThis study included 65 children aged 5 to 16 years (mean age±SD, 11.00±3.29 years) with unilateral amblyopia. Among them, 31 children underwent active vision therapy (AVT group), and 34 children underwent conventional patching therapy (patching group). AVT group underwent three sequential phases of AVT: Monocular phase (pursuit, saccades, fixation, visuomotor, eye-hand coordination, and central peripheral activities), biocular phase (diplopia awareness, antisuppression, monocular fixation in a binocular field, accommodative activities, bilateral integration, and fine motor activities) and binocular phase (fusion and stereopsis). Patching group patched their fellow eyes as per guidelines by Pediatric Eye Disease Investigator Group. Best-corrected monocular VA and stereoacuity were measured at baseline and after three months of therapy in both groups.
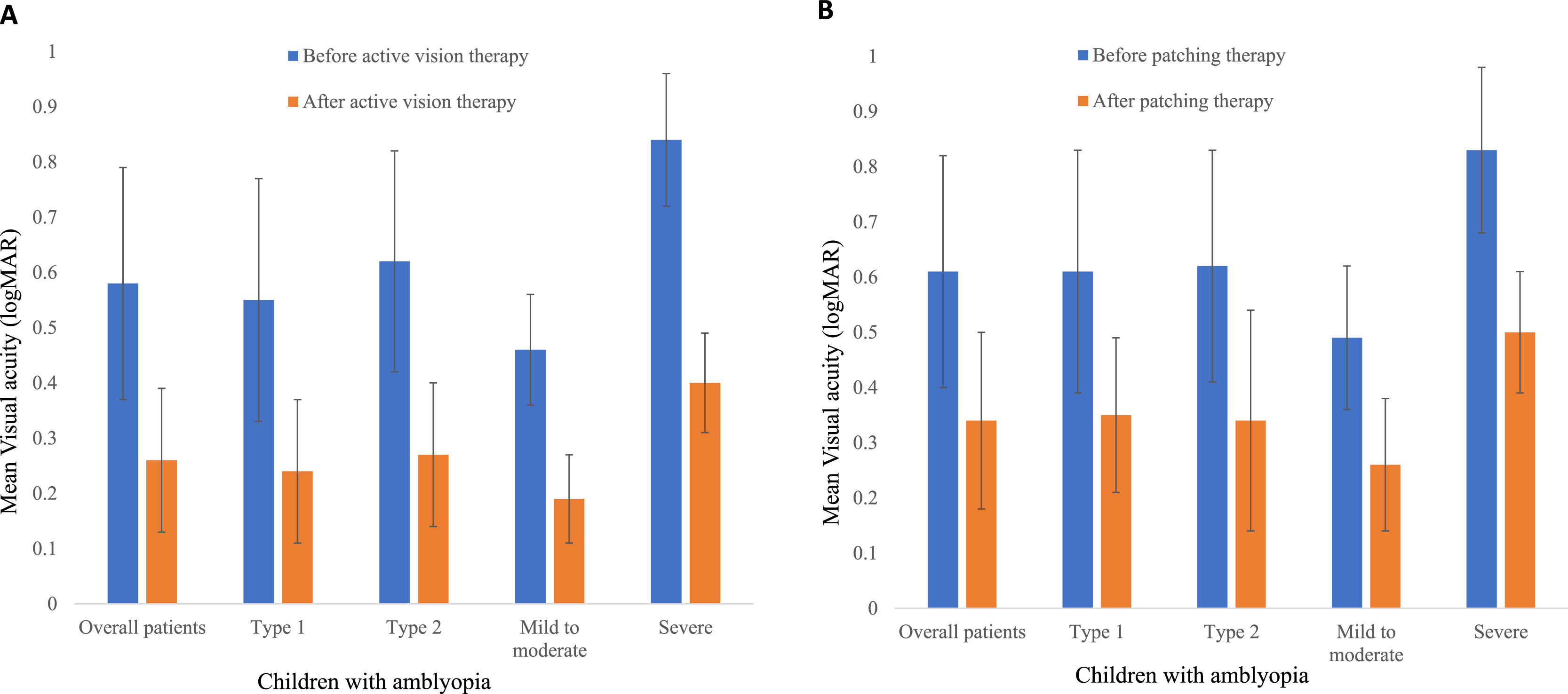
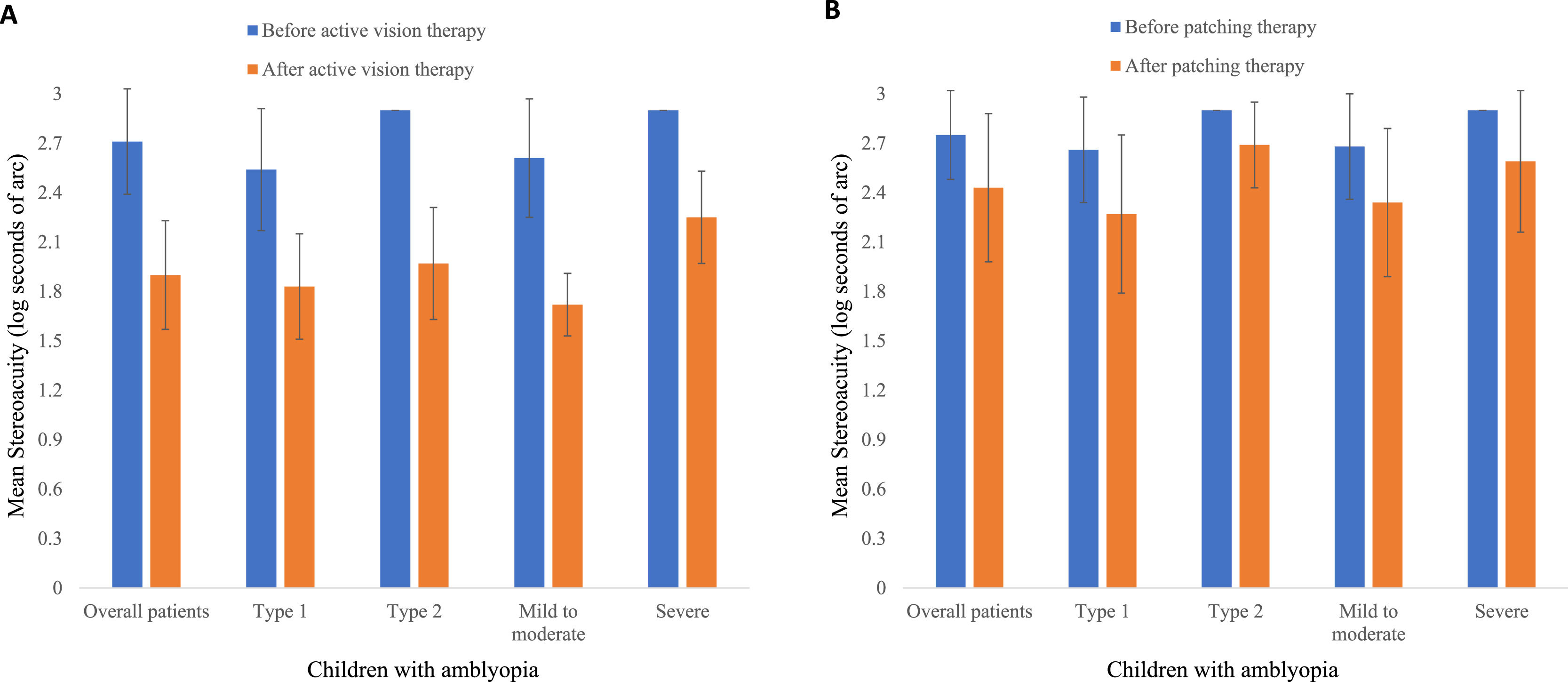
ResultsThere were significant improvements in the mean acuities in amblyopic eye (AE) in both AVT (0.32±0.11 logMAR, p <0.001) and patching groups (0.27±0.19 logMAR, p ˂ 0.001). However, there was no significant difference in mean acuity gains in AE between AVT and patching groups (p = 0.059). Mean gains in stereoacuities (log seconds of arc) were statistically significant in both AVT (0.81±0.34, p < 0.001) and patching groups (0.32±0.34, p < 0.001). The stereoacuity gain in the AVT group was significantly higher compared to patching group (p < 0.001).
ConclusionActive vision therapy had a better impact than conventional patching therapy in terms of improvement of stereoacuity but not in terms of VA when used for treating children with amblyopia.
Amblyopia is a neurodevelopmental disorder impairing unilateral or bilateral best-corrected visual acuity (VA) without any ocular pathology.1 Causes of amblyopia include high refractive error, anisometropia, strabismus, ocular media opacity, or a combination of these conditions. Besides reduction in VA, amblyopia is associated with impairments in stereoacuity,2 pursuit and saccades,3 accommodation,4 dynamic vergence eye movements,5 interocular suppression,6 spatial 7localization,7 visual motor integration,8 and fixation stability.9
The main aim of amblyopia treatment is to improve VA. However, despite good VA after amblyopia treatment, patients may not have normal binocularity.1 Stereoacuity, based on the computation of binocular disparity between the two eyes, is a gold standard technique and a sensitive probe for the quantitative evaluation of foveas regarding the object of interest, however, amblyopes lack this ability.2 Ideas on achieving binocularity in patients with amblyopia are changing as evidence shows that the loss of binocularity of cortical cells could be largely reversible in patients with amblyopia.10
While amblyopia was previously considered a monocular disorder, it is currently considered a cerebral visual impairment and a binocular disorder.1 The treatment of amblyopia involves multiple interventions, including adequate refractive correction, conventional patching, and active vision therapy (AVT). Though conventional patching therapy has been a mainstay of treatment for amblyopia,11 this has many limitations. There is poor compliance with conventional patching, and more than 85% of residual amblyopia has been reported.12 Recurrence of amblyopia has also been revealed in 24% of patients after successfully treating amblyopia with conventional patching.13 Therefore, there is an increased interest in performing AVT to treat amblyopia.1,14 Active vision therapy is a precise, scientific, and sequential regimen for achieving optimum visual function and binocularity by developing visual abilities through a series of oculomotor exercises.14 This AVT consolidates minimal occlusion with a combination of extensive visual motor therapies, thus improving visual function and other aforementioned binocular vision parameters.14,15
A good level of VA contributes to the quality of life; however, it has been suggested that stereopsis is more important than VA.16 In the case of amblyopia, there is no longer a "reserve" eye present and damage to the good eye can have significant impact on quality of life. To enhance stereopsis in amblyopia, one should work on pursuit, saccades, visuomotor, eye-hand coordination, central peripheral activities, antisuppression, bilateral integration, vergence, fusion, accommodation, and other binocular vision parameters.14 To date, limited studies have shown improvements in both VA and stereoacuity with the use of the AVT in its three divided phases (monocular, biocular and binocular).15,17 Considering these paradigms in amblyopia treatment, a sequential approach with monocular, biocular, and binocular phases of AVT was considered.15 The present study is the first to apply all these three sequential phases of AVT in children with amblyopia. This study aimed to compare improvements in distance VA and stereoacuity between AVT versus conventional patching therapy in children with different types and severity of amblyopia.
MethodsStudy design and participantsThis was a longitudinal and interventional study that included 65 children aged 5 to 16 years (mean age±SD, 11.00±3.29 years), who underwent treatment for unilateral amblyopia of different types and severity.
Amblyopia was defined as an interocular acuity difference of 0.2 logMAR or greater between the amblyopic eye (AE) and fellow eye (FE), and the FE acuity equal to or better than 0.2 logMAR.18 Amblyopia was classified as anisometropic (Type 1) and strabismic or combined mechanism amblyopia (Type 2).18 Anisometropic amblyopia was defined as anisometropia > 1.5 Diopter (D) (spherical or spherical equivalent) or the difference in astigmatism > 1.5 D with no measurable strabismus. Strabismic amblyopia was defined as manifest strabismus (15 to 35 prism dioptres) without refractive error that meets the criteria for anisometropic amblyopia. Combined mechanism amblyopia was defined as the presence of any measurable strabismus (15 to 35 prism dioptres) and hyperopia ≥ 3.50 D, myopia ≥ 3.50 D, anisometropia > 1.5 D (spherical or spherical equivalent), and astigmatism > 1.5 D. Based on the severity of VA, amblyopia was classified as mild to moderate (best-corrected VA from 0.2 logMAR – 0.6 logMAR) and severe (best-corrected VA less than 0.6 logMAR).18
Among 65 children, 31 children underwent active vision therapy (AVT group), and 34 children underwent conventional patching therapy (patching group). In the patching group, children were diagnosed with amblyopia for the first time and had no prior treatment history. In the AVT group, children had a history of wearing glasses, had tried part-time patching therapy in the past for ≥ 3 months, and were non-compliant with patching therapy, which helped to ensure that improvements in VA and stereoacuity would be due to AVT rather than conventional patching therapy, as in the previous study.19 Non-compliance with patching therapy was defined as wearing the patch less than 50% of the prescribed hours or not wearing the patch at all.20 Children in both AVT and patching groups were included if their amblyopia persisted or distance VA in the AE remained unchanged after four weeks of adequate optical correction. Children with eccentric fixation, microstrabismus, nystagmus, history of strabismus surgery, paralytic strabismus, pre-existing visual deficits, neurological problems were excluded from the study. Children who discontinued the assigned AVT or patching therapy between the given time frame were also excluded from the study.
The study was approved by the Ethical Review Board of the Nepal Health Research Council and followed the tenets of the Declaration of Helsinki. Assent was taken from the children, and written informed consent was obtained from the children's legal guardian. Children with unilateral amblyopia who had completed either the sequential AVT or conventional patching therapy were recruited from the Vision Therapy Unit of the Hospital for Children, Eye, ENT and Rehabilitation Services, Nepal. Before children's enrollment, parents were given options to choose either AVT or a patching group for the treatment of amblyopia of their children.
Vision and eye examinationAll children underwent comprehensive eye examination, including anterior segment examination with a slit lamp and posterior segment examination with an indirect ophthalmoscope to determine any associated ocular pathology. Monocular distance VA was tested with Standard Acuity VisuoPrime Diagnostics (Neurapy, India) at three meters in standard room illumination and recorded in logMAR. Dry and wet (cycloplegic) refractions were performed on the first day. Cycloplegic refractions were done using 1% cyclopentolate as used previously.15 Post-cycloplegic refractions were performed after three days to determine the monocular best-corrected distance VA. The presence of diplopia was ruled out with the Worth four-dot test with their subjective acceptance, and then appropriate glasses were prescribed. Four-week adaptation time for the prescribed glasses was allowed before initiating AVT or conventional patching therapy.
Binocular vision assessmentDetailed binocular vision examinations were assessed to rule out any strabismus, including the Worth four-dot test, extraocular motility, and prism bar cover test for both near and distance. The stereoacuity test was performed with a RANDOT stereo test (Stereo Optical, USA) at 40 cm, using the polarized glasses over the habitual glasses, if worn.21 The RANDOT stereo test (graded circles) consists of disparities of 400, 200, 140, 100, 70, 50, 40, 30, 25, and 20 s of arc. A minimum of two correct responses were needed to pass each disparity level, and threshold disparity was recorded. Children unable to detect 400 s of arc were recorded as nil stereopsis. For analysis purposes, seconds of arc were converted to logarithm values (See supplementary data Table A.1). Nil stereo was allocated the next highest log level as 2.90 log seconds of arc with a difference of 0.3 log.
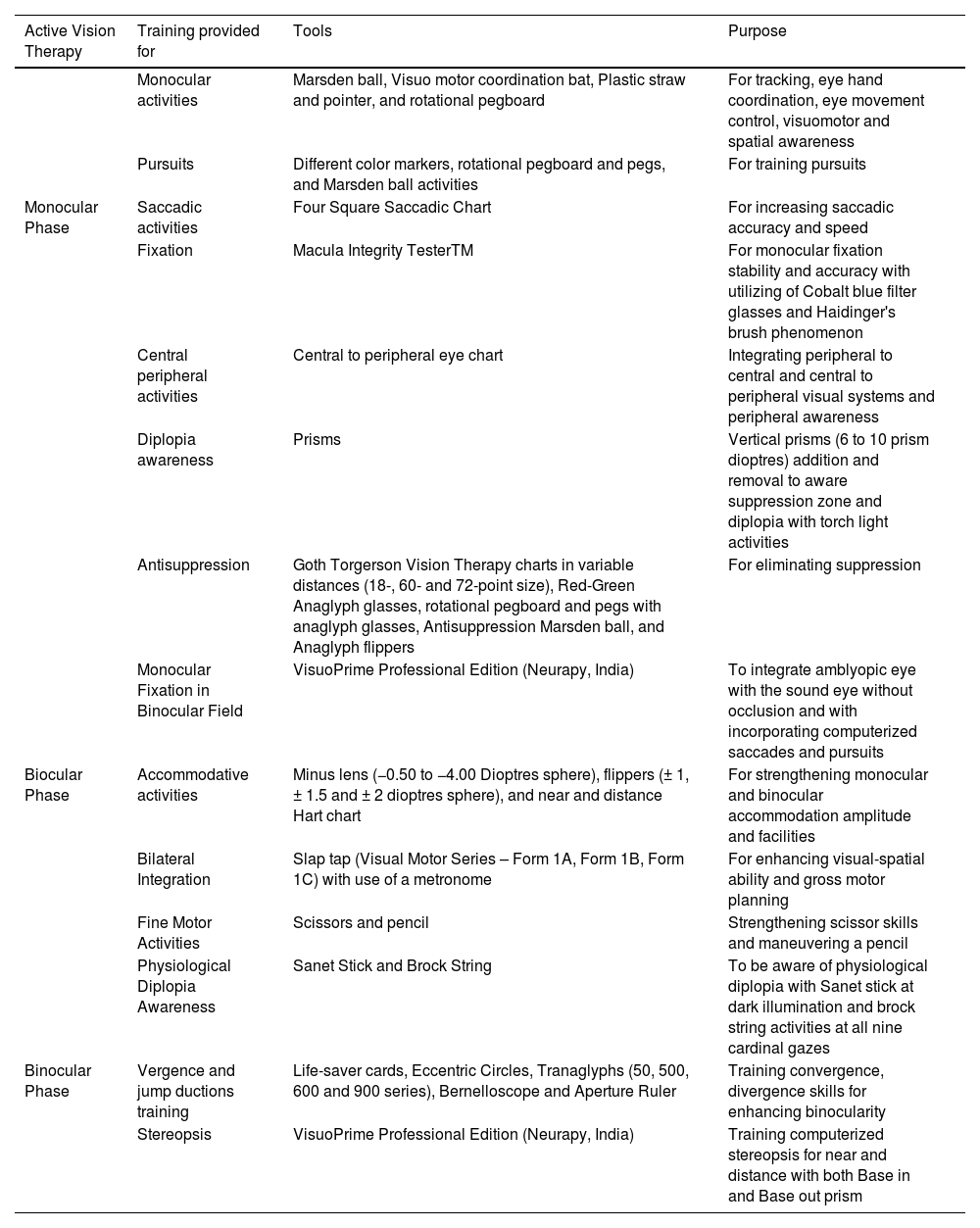
Active vision therapy groupIn this group, all children underwent sequential monocular, biocular and binocular phases of AVT, which incorporated both in-office and home therapies, as given below.
In-office therapiesThe in-office AVT for each child consisted of a total of 36 sessions with a therapy of one hour per day on alternate days for three months (three days a week for four weeks, i.e., approximately one month in each phase of therapy). The in-office AVT was executed in sequential three different phases, as used previously (Table 1).14,15 Monocular phase was for pursuit, saccades, fixation, visuomotor, eye-hand coordination, and central peripheral activities. The biocular phase was for diplopia awareness, antisuppression, monocular fixation in a binocular field, accommodative activities, bilateral integration, and fine motor activities. Finally, the binocular phase consisted of therapies for fusion and stereopsis.
Phases, tools and purposes of monocular, biocular and binocular phases of active vision therapy.
The in-office exercises were accompanied by daily one-hour home exercises. Monocular exercises with patching their fellow eye were line and letter tracing, video games, reading books, puzzle activities, and near and distance monocular activities with a hart chart for the first two months of AVT. After two months, brock string activities were given for the binocular exercise. On every visit to AVT, patients or their parents were asked if they performed home therapies to ensure proper compliance.
Patching groupAs per Pediatric Eye Disease Investigator Group (PEDIG) guidelines, children with mild to moderate amblyopia were advised to patch their FE for two hours/day with at least one hour near activities,22 and children with severe amblyopia were advised to patch their FE for six hours/day with a minimum of one hour near activities.12 Near activities were line and letter tracing, video games, reading books, puzzle activities, and near and distance monocular activities with a hart chart. To ensure patching compliance, a monthly reminder call was made to the parents of children and they were advised to keep a personalized calendar to follow up after three months.
Best-corrected monocular distance VA and stereoacuity were tested again after three months in both the AVT and patching groups, similar to how they were tested at the baseline.
Statistical analysisData analyses were carried out using SPSS (version 23.0, IBM, Armonk, NY, USA), and the significance level was set at a p-value < 0.05. The mean changes in VA and stereoacuity before and after therapy in both AVT and patching groups were compared using the student's paired t-test and Wilcoxon signed-rank test, respectively. The differences between the mean changes in VA and stereoacuity outcome between the AVT and patching groups were explored using the independent t-test and Mann-Whitney U test, respectively. Chi-square test was used to compare categorical values between the AVT and patching groups, including gender distribution.
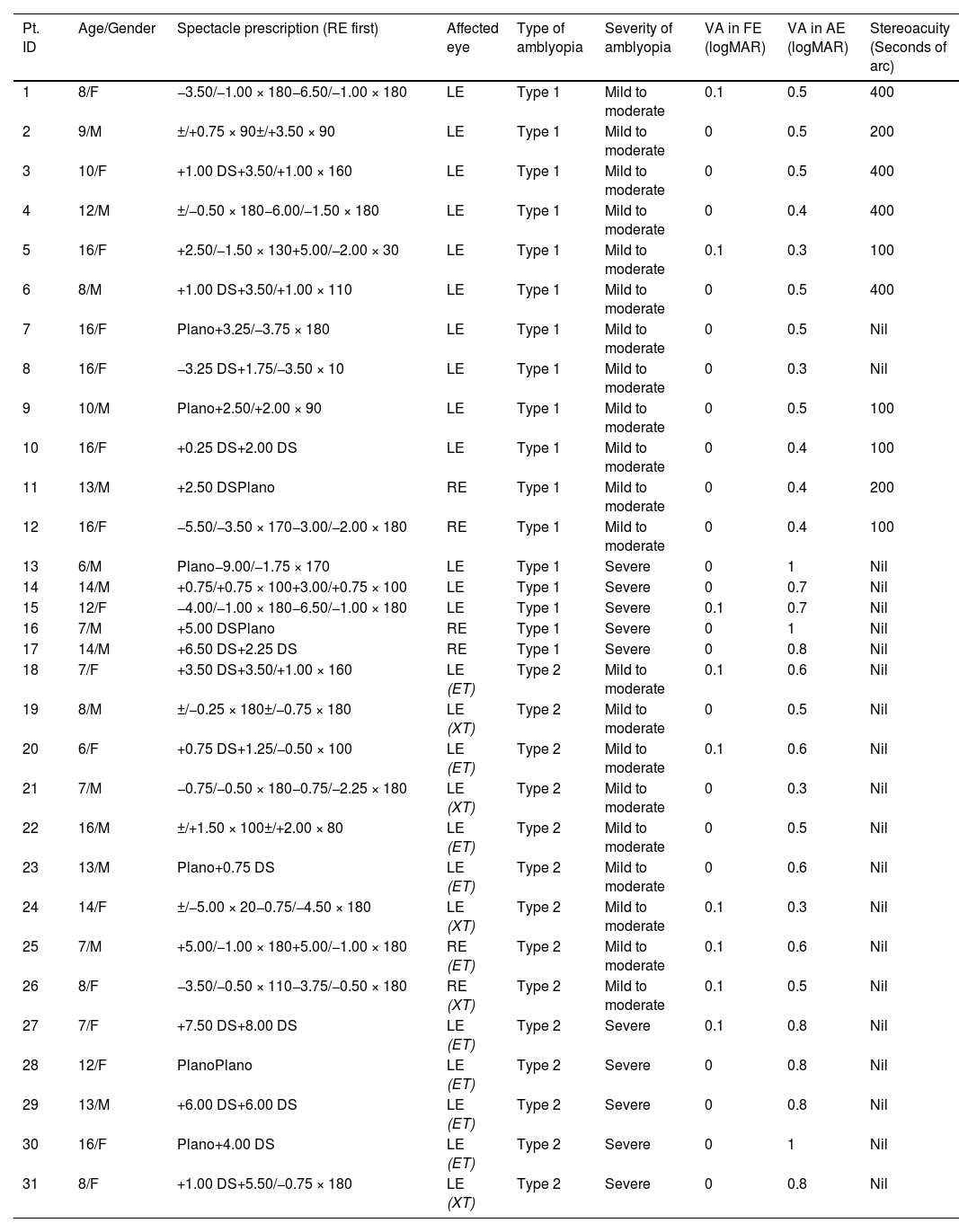
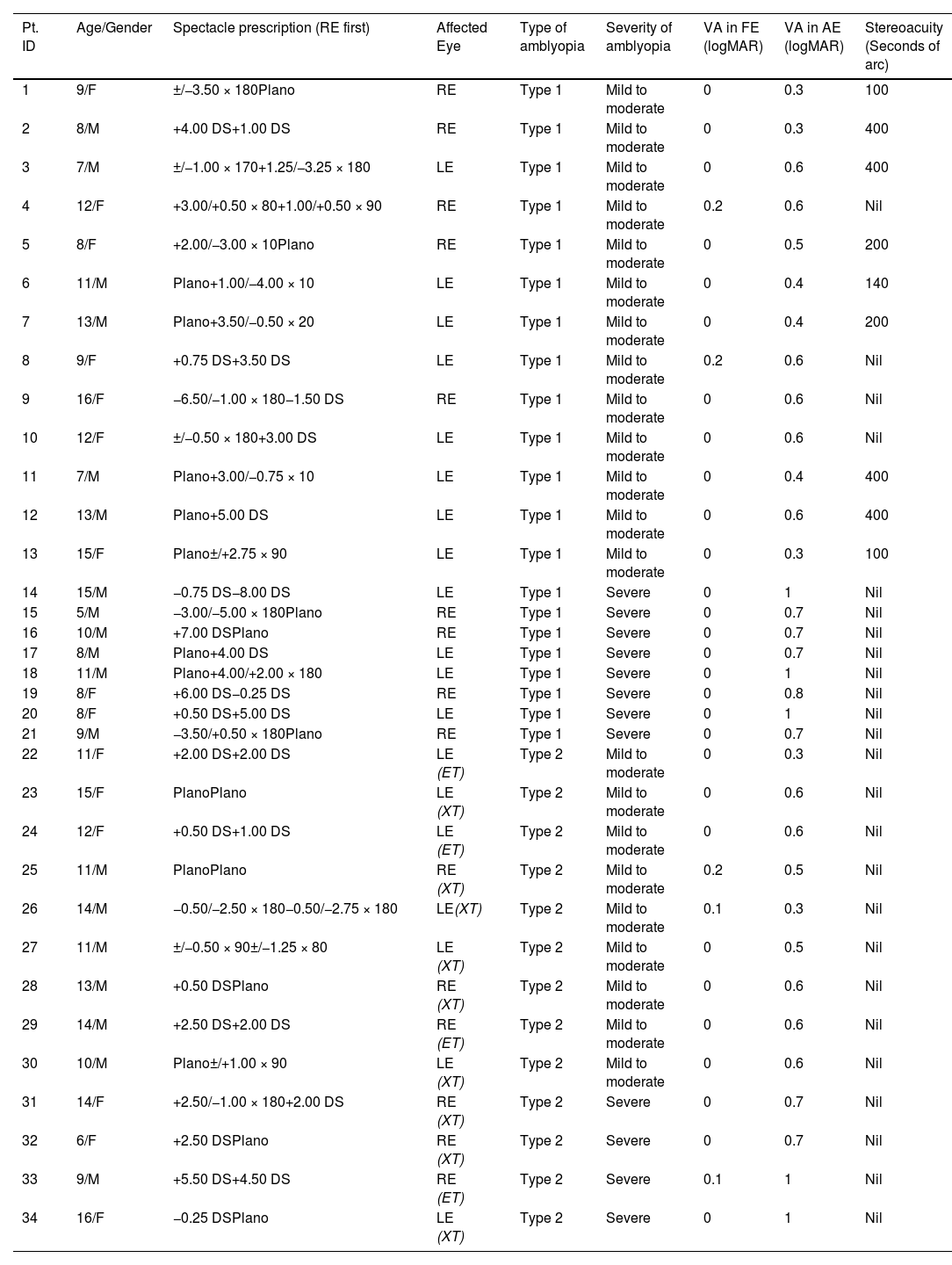
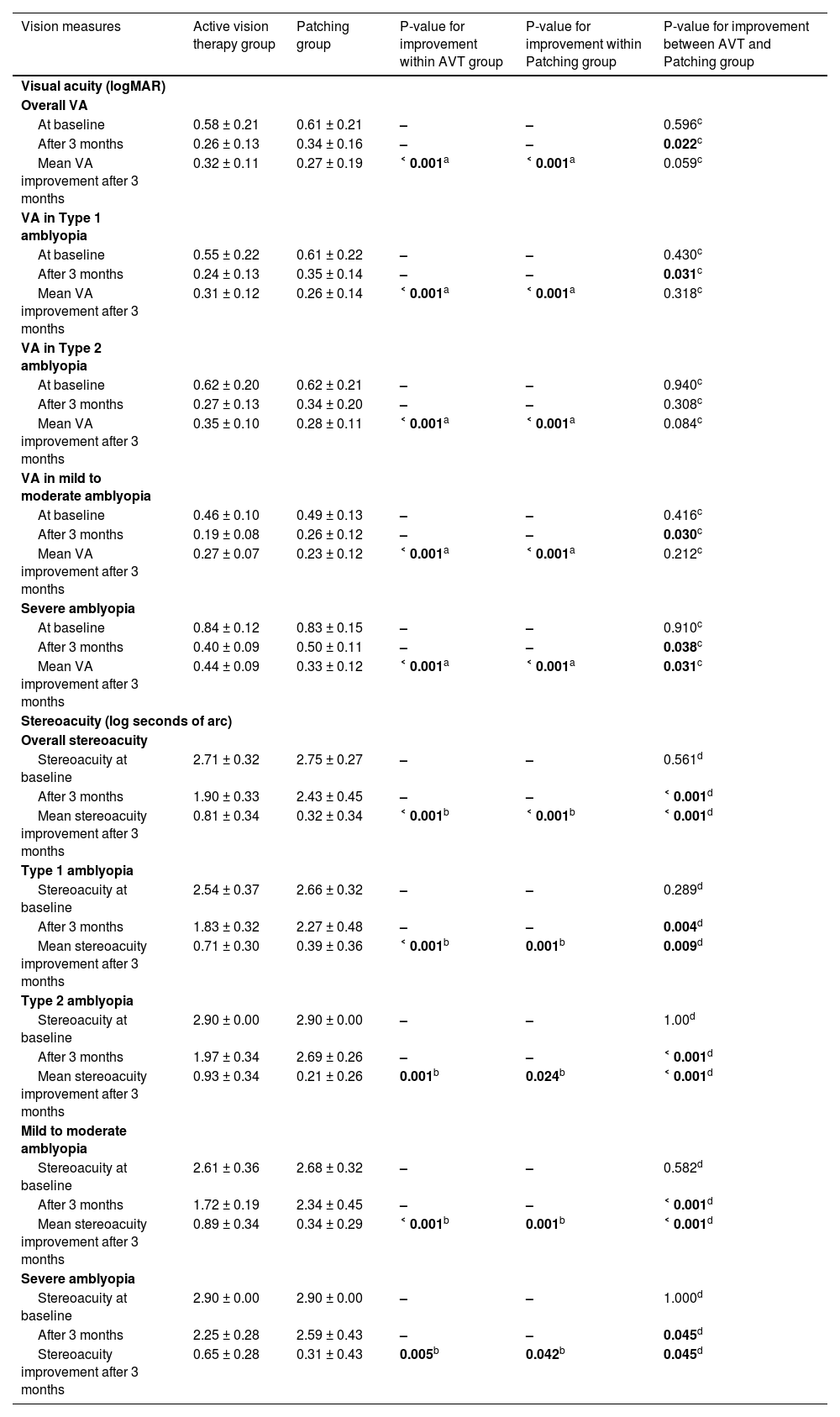
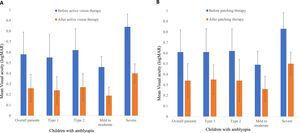
ResultsThis study included 31 children (15 males and 16 females) in the AVT group (mean age±SD, 11.13±3.64 years) and 34 children (19 males and 15 females) in the patching group (10.88±2.99 years). Tables 2 and 3 summarize the demographic and baseline characteristics of the AVT and patching groups, respectively. Overall, as well as according to the types and severity of amblyopia, there were significant improvements in the best corrected VAs in AEs and stereoacuities after 3-months of therapies for both AVT and patching groups (Figs. 1 and 2) (Table 4). Table 4 shows the mean improvements in the best corrected distance VA in AEs and stereoacuity between AVT and patching groups across all patients, and separately according to types and severity of amblyopia.
Demographic and baseline characteristics of the active vision therapy group.
Pt. ID: Patient Identity Document; M: Male; F: Female; RE: Right Eye; LE: Left Eye; DS: Dioptres sphere; FE: Fellow Eye; AE: Amblyopic Eye; logMAR: Logarithm of the Minimum Angle of Resolution; ET: Esotropia; XT: Exotropia; Participants who were unable to detect even 400 s of arc were recorded as nil stereopsis.
Demographic and baseline characteristics of the patching group.
Pt. ID: Patient Identity Document; M: Male; F: Female; RE: Right Eye; LE: Left Eye; DS: Dioptres sphere; FE: Fellow Eye; AE: Amblyopic Eye; logMAR: Logarithm of the Minimum Angle of Resolution; ET: Esotropia; XT: Exotropia; Participants who were unable to detect even 400 s of arc were recorded as nil stereopsis.
Comparison of best-corrected distance visual acuity of amblyopic eye and stereoacuity outcome between active vision therapy and patching group. Values are mean±SD.
| Vision measures | Active vision therapy group | Patching group | P-value for improvement within AVT group | P-value for improvement within Patching group | P-value for improvement between AVT and Patching group |
|---|---|---|---|---|---|
| Visual acuity (logMAR) | |||||
| Overall VA | |||||
| At baseline | 0.58 ± 0.21 | 0.61 ± 0.21 | – | – | 0.596c |
| After 3 months | 0.26 ± 0.13 | 0.34 ± 0.16 | – | – | 0.022c |
| Mean VA improvement after 3 months | 0.32 ± 0.11 | 0.27 ± 0.19 | ˂ 0.001a | ˂ 0.001a | 0.059c |
| VA in Type 1 amblyopia | |||||
| At baseline | 0.55 ± 0.22 | 0.61 ± 0.22 | – | – | 0.430c |
| After 3 months | 0.24 ± 0.13 | 0.35 ± 0.14 | – | – | 0.031c |
| Mean VA improvement after 3 months | 0.31 ± 0.12 | 0.26 ± 0.14 | ˂ 0.001a | ˂ 0.001a | 0.318c |
| VA in Type 2 amblyopia | |||||
| At baseline | 0.62 ± 0.20 | 0.62 ± 0.21 | – | – | 0.940c |
| After 3 months | 0.27 ± 0.13 | 0.34 ± 0.20 | – | – | 0.308c |
| Mean VA improvement after 3 months | 0.35 ± 0.10 | 0.28 ± 0.11 | ˂ 0.001a | ˂ 0.001a | 0.084c |
| VA in mild to moderate amblyopia | |||||
| At baseline | 0.46 ± 0.10 | 0.49 ± 0.13 | – | – | 0.416c |
| After 3 months | 0.19 ± 0.08 | 0.26 ± 0.12 | – | – | 0.030c |
| Mean VA improvement after 3 months | 0.27 ± 0.07 | 0.23 ± 0.12 | ˂ 0.001a | ˂ 0.001a | 0.212c |
| Severe amblyopia | |||||
| At baseline | 0.84 ± 0.12 | 0.83 ± 0.15 | – | – | 0.910c |
| After 3 months | 0.40 ± 0.09 | 0.50 ± 0.11 | – | – | 0.038c |
| Mean VA improvement after 3 months | 0.44 ± 0.09 | 0.33 ± 0.12 | ˂ 0.001a | ˂ 0.001a | 0.031c |
| Stereoacuity (log seconds of arc) | |||||
| Overall stereoacuity | |||||
| Stereoacuity at baseline | 2.71 ± 0.32 | 2.75 ± 0.27 | – | – | 0.561d |
| After 3 months | 1.90 ± 0.33 | 2.43 ± 0.45 | – | – | ˂ 0.001d |
| Mean stereoacuity improvement after 3 months | 0.81 ± 0.34 | 0.32 ± 0.34 | ˂ 0.001b | ˂ 0.001b | ˂ 0.001d |
| Type 1 amblyopia | |||||
| Stereoacuity at baseline | 2.54 ± 0.37 | 2.66 ± 0.32 | – | – | 0.289d |
| After 3 months | 1.83 ± 0.32 | 2.27 ± 0.48 | – | – | 0.004d |
| Mean stereoacuity improvement after 3 months | 0.71 ± 0.30 | 0.39 ± 0.36 | ˂ 0.001b | 0.001b | 0.009d |
| Type 2 amblyopia | |||||
| Stereoacuity at baseline | 2.90 ± 0.00 | 2.90 ± 0.00 | – | – | 1.00d |
| After 3 months | 1.97 ± 0.34 | 2.69 ± 0.26 | – | – | ˂ 0.001d |
| Mean stereoacuity improvement after 3 months | 0.93 ± 0.34 | 0.21 ± 0.26 | 0.001b | 0.024b | ˂ 0.001d |
| Mild to moderate amblyopia | |||||
| Stereoacuity at baseline | 2.61 ± 0.36 | 2.68 ± 0.32 | – | – | 0.582d |
| After 3 months | 1.72 ± 0.19 | 2.34 ± 0.45 | – | – | ˂ 0.001d |
| Mean stereoacuity improvement after 3 months | 0.89 ± 0.34 | 0.34 ± 0.29 | ˂ 0.001b | 0.001b | ˂ 0.001d |
| Severe amblyopia | |||||
| Stereoacuity at baseline | 2.90 ± 0.00 | 2.90 ± 0.00 | – | – | 1.000d |
| After 3 months | 2.25 ± 0.28 | 2.59 ± 0.43 | – | – | 0.045d |
| Stereoacuity improvement after 3 months | 0.65 ± 0.28 | 0.31 ± 0.43 | 0.005b | 0.042b | 0.045d |
Note: Improvements in VA and stereoacuity were calculated by subtracting respective values at 3 months from the baseline values.
There was no significant difference in age between the AVT and patching groups (χ2=15.09, df=11, p = 0.178). There was also no significant difference in gender between the AVT and patching groups (χ2=0.365, df=2, p = 0.546). There were also no significant differences between the AVT and patching groups for baseline VA (p = 0.596) and stereoacuity in (p = 0.561) AEs (Table 4) across all participants. While the mean gain in VA, across all participants, in AE was higher in the AVT group (0.32 ± 0.11 logMAR) compared to the patching group (0.27 ± 0.19 logMAR), the difference in the mean gain in VA between the two groups only approached significance (p = 0.059). However, in severe amblyopia, the mean gain in VA in AE was significantly higher (p = 0.031) in the AVT group than in the patching group (Table 4). Unlike VA, the mean overall stereoacuity gain across all participants was significantly higher (p ˂ 0.001) in the AVT group (0.81 ± 0.34 log seconds of arc) compared to the patching group (0.32 ± 0.34 log seconds of arc). There were also higher gains in stereoacuities in the AVT group compared to patching group, according to types and severity of amblyopia (Table 4).
In the AVT group, the gain in stereoacuity was neither correlated with the mean initial acuity level (r = 0.21, p = 0.25) nor the mean improvement of acuity (r = 0.06, p = 0.73). In the patching group, the gain in stereoacuity was not significantly correlated with the mean initial acuity level (r = 0.09, p = 0.60) but was significantly correlated with the mean improvement of acuity (r = 0.34, p = 0.047).
DiscussionBoth AVT and conventional patching therapy were demonstrated to be beneficial in treating children with unilateral amblyopia. Our findings showed that improvements in distance VA and stereoacuity with three sequential phases of AVT combined with planned home therapies were higher than conventional patching therapy alone, regardless of the types and severity of amblyopia in children. However, the gain in the mean distance VA was not significantly different between the AVT and patching group, except in children with severe amblyopia, where there was a significantly higher mean gain in distance VA in AE in the AVT group than in the patching group. On the contrary, the gain in the mean stereoacuity in the AVT group was significantly higher than in the patching group. Therefore, this study suggests that sequential monocular, biocular, and binocular phases of AVT could be a promising treatment for amblyopia.
Successful outcomes of AVT for amblyopia have been reported in the past.23 In this study, improvements in distance VA and stereoacuity were greater than in the previous study that performed balanced binocular viewing therapy.18 However, with the planned AVT, this study reported similar mean acuity gain to one study19 but lower than another study.20 Further, there was a higher mean stereoacuity gain compared to a study that performed AVT in children with anisometropic amblyopia.19 These inconsistent findings could be due to discrepancies in study methods, such as duration and regimen of AVT. These findings suggest the lack of stringent criteria for AVT, suggesting the need for homogeneity in the therapy protocols, duration, and frequency of AVT sessions.
Management of amblyopia needs to target remarkable binocular recovery restoring higher-level functions (e.g., in spatial or object vision).1 Children with amblyopia are significantly influenced by deficits in eye-hand coordination or visuomotor.8 Recovery of binocularity confers increasing benefits for visuomotor, eye-hand coordination, speed and accuracy.8 Moreover, fixation instability and the associated poor stereoacuity in amblyopic patients result from decorrelated binocular experience.9 The ability of steady fixation is a fundamental aspect of good visual function. Hence, we have included exercises for eye-hand coordination, visuomotor, spatial awareness, pursuit, saccades and fixation in the first monocular phase of our AVT.
Evidence demonstrates that binocular dysfunction is primary, and monocular VA loss is secondary in amblyopia.1 This indicates that binocular treatments incorporating exercises for fusion and stereopsis are much more effective in improving VA and stereoacuity for the management of amblyopia.19 Thus, as in the previous study, we have included the third phase, including exercises for fusion and stereopsis.19 In our study, only ten children (32.26%) in the AVT group had measurable stereoacuity before therapy. Interestingly, all patients in the AVT group showed improvements in stereoacuity after AVT. In contrast, in a previous study, only patients with measurable poor stereoacuity showed improvement in stereoacuity after binocular treatment.18 Therefore, sequential three phases of AVT could be more successful in treating amblyopia than previous binocular treatment.18
Different binocular difficulty includes suppression, increased refractive error, and deviation in the amblyopic eye.14 The ideal outcome in the treatment of amblyopia is achieved when there is 20/20 visual acuity in both eyes, along with fine stereopsis, good eye movements, and have normal range of other binocular vision parameters. Good acuity in both eyes is not enough, and good acuity doesn't necessarily mean having good stereopsis.1 There is a phenomenon called ‘interocular suppression’, which can occur in normal vision as well as in amblyopic vision that prevents binocular function24; i.e., the seemingly expected normal monocular functions in treated amblyopia is not necessarily to be normal in day-to-day functions when both eyes are open, and interact with each other. In this study, all children in the AVT group were aware of physiological diplopia at all nine cardinal gazes with brock string at the last visit of AVT, which indicates all the children in AVT groups had lost the interocular suppression. In contrast, it is unclear if conventional patching therapy could recover interocular suppression in children with amblyopia; that could be because there was no change in stereoacuity in 14 (41.17%) children after undergoing conventional patching therapy, and therefore, a future study is required to explore if patching therapy can recover interocular suppression.
Binocular treatment enhance binocular summation and potentially involves neural plasticity in different brain regions for maintaining binocular vision, like the parietal cortex.1 The scientific group is embracing the notion that active treatments and rehabilitation can alter brain reorganization and functional recovery in motor, sensory and cognitive impairments.10 AVT strengthens synaptic connections and induces cortical reorganization for maximizing visual efficiency, and these neuroplastic changes take place throughout different aforementioned three phases of AVT.25
As per PEDIG guidelines, children with mild to moderate amblyopia are advised to patch FE for two hours/day,22 and children with severe amblyopia are advised to patch for six hours/day.12 Patching therapy needs between 178 and 276 h to gain 0.2 logMAR in children.26 This study reported that 180 h of patching in mild to moderate amblyopia and 540 h of patching in severe amblyopia, are needed in three months to improve 2.7 logMAR lines. On the contrary, lesser time, only 126 h of AVT (36 h of AVT and 90 h of home therapies), is needed to improve 3.2 logMAR lines in three months.
There is a stronger interocular suppression in strabismic amblyopia than in anisometropic amblyopia,27 and it is challenging to overcome suppression in strabismic amblyopia. This study showed a higher mean VA and stereoacuity gain in strabismic amblyopia than in anisometropic amblyopia in the AVT group. On the contrary, the mean stereoacuity gain was higher in anisometropic amblyopia than strabismic amblyopia in the patching group. Therefore, our findings indicate that these three phases of AVT could be more effective in the treatment of strabismic amblyopia. This supports the evidence-based practice upon a view of behavioural optometrists that strabismus needs to be managed by surgery only as a last resort.14 However, future studies quantifying the deviation before and after AVT in strabismic amblyopia could strengthen the study if AVT can successfully decrease the deviation with improvement in stereoacuity. Moreover, the mean acuity gain was higher in severe amblyopia than in mild to moderate amblyopia, and the mean stereoacuity gain was higher in mild to moderate amblyopia than in severe amblyopia in both AVT and patching groups. We postulate that these findings are due to higher interocular suppression in severe amblyopia than in mild to moderate amblyopia, and severe amblyopia has a higher range for improvement in VA from the baseline VA.27
There have been rapid developments in video game therapies in treating amblyopia, used as an effective adjunct treatment, achieving similar results compared to patching therapy in a short duration.28-30 Video game therapies are designed to reduce suppressive interactions in the visual cortex by rebalancing visual stimuli between the two eyes and thus promoting binocular vision. .28 VA outcome with AVT was higher in this study than in the dichoptic digital therapy.28 Stereoacuity outcome with sequential three phases of AVT in this study was higher than the action video game.29 Further, dichoptic stimulation in treating strabismic amblyopia was ineffective compared to anisometropic amblyopia.30 In contrast, our model of AVT was more effective in strabismic amblyopia.
The strengths and limitations of this study should also be considered. In this study, the best approach was made to ensure that improvements in VA and stereoacuity in the AVT group was not just occasional. First, there were no significant differences in age, gender and all baseline characteristics (VA and stereoacuity) between the AVT and patching groups. Second, the duration of the therapy was similar in both groups, i.e., for three months. Third, all children in the AVT group received the therapy with the same principles. The limitations of this study included the lack of assessment of contrast sensitivity, saccades, pursuits, accommodation, vergence, and other motor entities that might be impaired in patients with amblyopia. Furthermore, while refractive adaptation could take longer up to three months, this was only four weeks due to time constraint and to minimize the potential loss of follow-up, and therefore, future study with longer refractive adaptation is needed. In addition, quantifying improvement skills like oculomotor, accommodation, vergence and visual-motor integration with AVT would further strengthen the study. In this study, the difference in the mean gain in VA between the AVT and patching groups approached a significance level of p = 0.059 (which might be due to small sample size), which is very close to a significant difference. Expanding the study with a larger sample would be useful if AVT can be superior in terms of improving VA and any amblyopia recurrence in long-term follow-up with AVT. There is a need for randomized clinical trials for the creditability of good optometry practice for scientific evidence in the treatment of amblyopia. It is also important to note that high cost may be required for undergoing vision therapy. Therefore, the evaluation of the cost associated with vision therapy and its affordability could be future research.
ConclusionThe findings of this study indicated that sequential monocular, biocular, and binocular phases of AVT were superior to patching therapy in terms of improving stereoacuity but not for VA improvement, when used for treating children with amblyopia. Importantly, AVT is a promising technique for treating amblyopia in children, regardless of the type and severity of amblyopia.