To describe the functional and refractive results obtained with the implantation of toric intraocular lens (IOL) in a private clinic, and verify and compare these results with other similar studies.
MethodsRetrospective evaluation of patients implanted with SN60AT toric IOL. Patients undergoing cataract surgery and corneal astigmatism (CA) higher than 0.75 D were included in the study. Preoperative and postoperative uncorrected visual acuity (UCVA), best corrected visual acuity (BCVA), subjective refraction and preoperative keratometry were recorded and analyzed statistically.
ResultsThe study included 68 eyes (52 patients). Thirty eyes were implanted with SN60T3, 11 with SN60T4 and 28 with SN60T5. Mean BCVA gain was of 1.9±1.67 logMAR lines. Comparing the preoperative BCVA versus postoperative UCVA, the improvement was of 0.89±2 logMAR lines. The postoperative refractive astigmatism was −0.37±0.37 D; 75.5% of the eyes had a refractive astigmatism lower than 0.50 D and 98.6% lower than 1.00 D. The expected cylinder supplied by the manufacturer showed a good agreement with the postoperative subjective results (−0.03±0.47 D).
ConclusionsThe implantation of SN60T toric IOL in patients with CA higher than 0.75 D is a safe, predictable and effective way of reducing refractive astigmatism in patients undergoing cataract surgery.
Describir los resultados funcionales y refractivos obtenidos con el implante de una lente intraocular tórica (LIO) en una clínica privada y verificar y comparar estos resultados con otros estudios similares.
MétodosEvaluación retrospectiva de pacientes con LIO tórica SN60AT implantada. En el estudio se incluyeron pacientes sometidos a cirugía de cataratas y con un astigmatismo corneal (AC) superior a 0,75 D. Se registraron y analizaron estadísticamente, preoperatoria y posoperatoriamente, la agudeza visual sin corrección (AVSC), la agudeza visual mejor corregida (AVMC), la refracción subjetiva y la queratometría preoperatoria.
ResultadosEn el estudio se incluyeron 68 ojos (52 pacientes). En 30 ojos se implantó la SN60T3, en 11 la SN60T4 y en 28 la SN60T5. La mejoría media de AVMC fue de 1,90±1,67 líneas de logMAR. Comparando la AVMC preoperatoria con la AVSC posoperatoria, la mejoría fue de 0,89±2,00 líneas de logMAR. El astigmatismo refractivo posoperatorio fue de −0,37±0,37 D. El 75,5% de los ojos tenía un astigmatismo refractivo inferior a 0,50 D y el 98,6% tenía uno inferior a 1,00 D. El cilindro previsto proporcionado por el fabricante mostró buena concordancia con los resultados subjetivos posoperatorios (−0,03±0,47 D).
ConclusiónEl implante de la LIO tórica SN60T en pacientes con AC superior a 0,75 D es un método seguro, previsible y eficaz para reducir el astigmatismo refractivo en pacientes sometidos a cirugía de cataratas.
Astigmatism is one of the most common causes of dependence on corrective lenses for distance vision in patients after cataract surgery. It has been estimated that 15% to 29% of cataract patients have more than 1.50 dioptres (D) of refractive astigmatism1,2 due to corneal astigmatism (CA). The reduction of this pre-existing astigmatism can improve the visual outcome and the spectacle independence after cataract surgery. Traditionally this astigmatism has been reduced during the cataract procedure by incisive relaxation techniques3 or by corneal ablative refractive surgery later on. The advent of toric intraocular lenses (IOL) helps us correcting preexisting corneal astigmatism by implanting a toric IOL.4
The rotation of the toric IOL after implantation was the main problem associated with these lenses4 in the initial designs, but nowadays the rotational stability has been proved in several studies.5,6 For every 1° of axis rotation, approximately 3.3%7,8 of the lens cylinder power may be lost. At 30° of rotation, the power of the IOL cylinder is totally lost and the resulting refraction can be astigmatism of undesirable power and orientation.
The Alcon Acrysoft Natural SN60T toric IOL is a one-piece acrylic hydrophobic lens with a 6 mm optic and 13 mm total diameter. The anterior surface is spherical and the posterior toric, with three cylindrical powers: 1.5 D (T3), 2.25 D (T4), and 3 D (T5), which correct approximately 1 D, 1.5 D, and 2 D at the corneal plane, respectively. This lens was approved by the US Food and Drug Administration (FDA) at the end of 2005 and have showed a better stability and appear to be the preferred IOL for the astigmatism correction when cataract surgery is needed.9,10
This retrospective study has two principal objectives. In one hand we will describe the functional and refractive results obtained in a private clinic with the implantation of the T3, T4 and T5 Alcon Acrysof Natural SN60T toric IOL in a series o consecutive cataract surgery. On the other hand we want to verify and to compare our refractive results with other similar studies.
MethodsThis is a retrospective evaluation patients implanted with Alcon Acrysoft Natural SN60T toric IOLs in a private clinic (Oftalmo+, Barcelona, Spain) between March 2008 and June 2009.
Inclusion criteria were patients with more than 0,75 D of CA, without other ocular pathologies (different from cataract), and that no postoperative complications. Pre-operating standard explorations included best-corrected visual acuity —BCVA—, biomicroscopy, intraocular pressure, fundus examination and IOLmaster non-contact biometry (Carl Zeiss) and a per protocol systemic work up. The study adhered to the tenets of the Declaration of Helsinki and all patients signed the standard cataract surgery informed consent.
All surgical actions were performed by the same surgeon (J.C) in the Institut Oftalmològic de Cirugia Avançada de Barcelona (IOCAB) or in the Hospital de Barcelona operating rooms. Preoperative and postoperative follow-ups were made in the “Oftalmoplus” ocular clinic.
The surgery technique, phacoemulsification technique for cataract, was similar to that used to implant in monofocal IOLs, but preoperatively markings were made at 0 degrees and 180 degrees with the patient sitting up to avoid cyclorotation. Before surgery, with the patient lied, these marks were used to determine the desired axis of the IOL orientation, which coincides, with the more curved corneal axis. An anastigmatic incision was performed in this meridian and the rest of the intervention was carried out following the standard non-toric IOL phacoemulsification procedure. Patients were treated with Ketorolac trometamol and Ofloxacin every four hours for two weeks and 3 times/day until one month after the surgery.
We registered age, gender, pre and post surgical BCVA (decimal), subjective refraction, preoperative keratometry with IOLMaster and postoperative uncorrected visual acuity (UCVA) at 1 month after surgery.
Statistical analysis was performed by means of SPSS 17 software using parametric paired t test (Chicago, IL, USA) and a p-value lower than 0.05 was considered statistically significant.
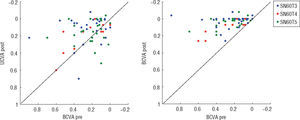
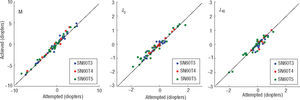
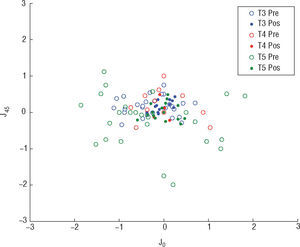
ResultsPreoperative and postoperative visual acuities are represented in figure 1 and shown in table 1. Refractive results are also shown in table 1 and in figures 2 and 3, following vector analysis described by Thibos et al.11
Pre and postoperative visual acuities and refractive astigmatism
| SN60T3 (n=30) | SN60T4 (n=11) | SN60T5 (n=27) | Total (68) | |
| Visual Acuity (logMAR) | ||||
| Pre BCVA | 0.23±0.20 | 0.27±0.21 | 0.23±0.16 | 0.23±0.18 |
| Pos UCVA | 0.11±0.15 | 0.20±0.18 | 0.15±0.14 | 0.14±0.15 |
| Pos BCVA | 0.03±0.08 | 0.09±0.10 | 0.03±0.06 | 0.04±0.07 |
| Astigmatism | ||||
| CA | −1.31±0.20 | −1.68±0.25 | −2.56±0.60 | −1.86±0.71 |
| Pre cyl. | −1.03±0.62 | −1.30±0.63 | −2.33±1.06 | −1.59±1.02 |
| Post cyl. | −0.26±0.32 | −0.27±0.36 | −0.50±0.37 | −0.36±0.36 |
| Exp cyl. | −0.25±0.16 | −0.18±0.16 | −0.56±0.47 | −0.35±0.35 |
| Pre J0 | −0.22±0.49 | −0.11±0.58 | −0.32±1.02 | −0.22±0.75 |
| Post J0 | −0.02±0.14 | −0.01±0.09 | −0.06±0.24 | −0.03±0.18 |
| Exp J0 | 0±0.16 | 0.02±0.09 | −0.05±0.30 | −0.02±0.21 |
| Pre J45 | 0.15±0.25 | 0.20±0.43 | −0.21±0.71 | 0.02±0.54 |
| Post J45 | 0.08±0.13 | 0.06±0.21 | 0.01±0.19 | 0.05±0.17 |
| Exp J45 | −0.01±0.07 | 0.02±0.09 | −0.04±0.19 | 0.05±0.17 |
We evaluated 68 eyes of 52 patients (61,3% females; 38.7% males) of which 28 were right and 40 left. Mean age of the patients was 68 years (range, 49 to 89). The mean spherical equivalent was −0.45±3.02 D (range, −8.25 D to + 4.75 D) and the refractive astigmatism was −1.59±1.02 D (range, −4.00 D to 0.00 D). The preoperative CA was -1.86±0.71 D (range, −3.99 D to −0.93 D).
Thirty eyes were implanted with SN60T3, 11 with SN60T4 and 27 with SN60T5.
Functional resultsThe functional results are shown in figure 1 and table 1. Note that all the functional results are expressed in logMAR visual acuities units.
Patients experienced a mean BCVA gain of 1.9±1.67 lines (95% confidence interval −CI−, 1.49;2.3; p<0.001) after the surgery respect preBCVA. Comparing the preBCVA versus posUCVA, the improvement was of 0.89±2 lines (95% CI, 0.4;1.37; p<0.001).
The group of patients implanted with SN60T3 improved their BCVA in 1.97±2.01 (95% CI, 1.22;2.72; p<0.001) lines. Comparing preBCVA versus posUCVA the improvement was of 1.16±2.21 lines (95% CI, 0.34;1.99; p=0.007).
In the group of the SN60T4 IOL, the BCVA improved in 1.85±1.46 lines (95% CI, 0.87;2.84; p=0.02). While the posUCVA was 0.72±1.32 lines (95% CI, −0.16;1.61; p=0.097).
The analysis of the group implanted with SN60T5 showed an improvement of 1.82±1.36 lines (95% CI, 1.29;2.37; p<0.001) and the comparison preBCVA versus posUCVA resulted in an improvement of 0.65±2.01 lines (95% CI, −0.15;1.44; p=0.105).
Refractive resultsThe refractive results are resumed in table 1.
Mean postoperative spherical equivalent was −0.13±0.44 D; 82.4% of the patients were between±0.50 D and 95.6% between±±1.00 D.
The postoperative mean refractive astigmatism value was −0.36±0.36 D. In this case 73.5% of the eyes had a refractive astigmatism equal or lower than 0.50 D and 98.5% equal or lower than 1.00 D.
Mean change in total refractive astigmatism was a decrease of −1.24 D (−1.24±0.99 D; 95% CI, −1.47;−1.00; p<0.001) and the total power of the expected cylinder supplied by the manufacturer showed a good agreement with postoperative subjective results (−0.03±0.41 D; 95% CI, −0.10; + 0.10; p=0.948). An analysis using power vectors is showed in figures 2 and 3 and in table 1.
Statistical analysis in the group of patients implanted with SN60T3 showed a decrease in the refractive astigmatism of −0.78±0.62 D (95% CI, −1.01;−0.54; p<0.001). In this group the approximation of expected and postoperative-refractive cylinder also showed a good accordance (0.01−0.31 D; 95% CI, −0.11; + 0.13; p=0.871). In this group all the eyes were within±0.50 D in J0 and J45.
Patients implanted with the SN60T4 IOL reduced the refractive astigmatism in −1.02±0.84 D (95% CI, −1.59;− 0.46; p=0.002), while the agreement between expected and postoperative-refractive cylinder was 0.09±0.43 D (95% CI, −0.19; + 0.38; p=0.501). In this group, vector analysis of the astigmatism showed that all the eyes were within±0.50 D in J0 and J45 components.
The group of patients implanted with the SN60T5 showed a mean reduction of astigmatism of −1.83±1.09 D (95% CI, −2.26;−1.40; p<0.001), and the accordance between the expected and postoperative-refractive cylinder was −0.11±0.61 D (95% CI, −0.34; + 0.13; p=0.348). In this case, vector analysis showed that all the eyes were within±0.50 D in the J45 component. In the J0 component, all the eyes were within±1.00 D and all except one were within±0.50 (96.3%).
Discussion and conclusionsThis study corroborates other studies results (see table 2) and shows that the implantation of Acrysof Natural SN60T toric IOL is a safe and effective procedure for reducing refractive astigmatism in cataractous eyes.
Comparison of toric SN60T studies
| Astigmatism | ||||||
| Study/year | FU (monts) | Eyes (n) | Preoperative (D±SD) | Postoperative (D±SD) | Postoperative lower than 0.50 D | Postoperative lower than 1.00 D |
| Present/2010 | 1 | 68 | −1.59±1.02 | −0.36±0.36 | 82.6% | 95.7% |
| J0 −0.22±0.75 | J0 −0.03±0.18 | J0 98.5% | J0 100% | |||
| J45 −0.02±0.54 | J45 −0.05±0.17 | J45 100% | J45 100% | |||
| Tsinopoulos13/2010 | 6 | 29 | 2.38±0.91 | 0.64±0.61 | NA | NA |
| Ahmed12/2010 | 6 | 234 | −1.7±0.4a | 0.4±0.4 | 70.7% | 90.2% |
| Mendicute10/2009 | 3 | 20 | −1.75±0.71 | −0.62±0.46 | J0 95% | J0 100% |
| J45 90% | J45 100% | |||||
| Bauer5/2008 | 4.5 | 43 | −2.21±1.10 | 91%<1.0 | 74% (±0.75 D) | 91% |
| Mendicute9/2008 | 3 | 30 | −2.34±1.28 | −0.72±0.43 | J0 80% | J0 100% |
| J45 93% | J45 100% | |||||
| Zuberbuhler6/2008 | 3 | 44 | 1.0 to 5.0b | NA | 81% | 90% |
| Chang14/2008 | 1 | 100 | 2.5 | 0.5 | NA | NA |
NA: not available.
All patients maintained or improved their BCVA after surgery, that was expected because they were cataract patients, and no complications were observed in the sample. The spherical equivalent results shows that the calculation of the spherical component of the toric IOLs can be made by the standard procedures usually used to calculate the power of monofocal lenses. There is a good agreement between the expected cylinder and the post refractive cylinder at one month, which is better for low astigmatic IOLs (SN60T3). It is logical, because the same decentration, tilt or rotation of the IOL in lower cylinders will have minor repercussions that with high cylinders. Although they are very similar, our postoperative subjective refractive astigmatism results are slightly better than other similar studies (table 2, right columns).
Despite we did not evaluate the precise postoperative orientation of the IOL, but the agreement between postoperative refractive and the expected cylinder was excellent. Under our point of view the dilation of the patient in the postoperative follow-ups is not necessary for refractive reasons if the refraction does not show an important unexpected degree and axis of astigmatism. We based our study in refractive prescription better than in axis rotation.
There are other studies that show a good stabilization of the SN60T IOL with longer follow ups (table 2). Zuberbuhler et al.6 found a mean of axis rotation between the one week and three months follow-up after the surgery of 2.2±2.2° and the rotations were independent of the clockwise rotation (clockwise 36%; anti-clockwise 36%; no rotation 28%); Ahmed et al12 made a 6 month follow up of their patients assessing the IOL axis orientation one day after the surgery, and at 1, 3 and 6 months obtaining a mean deviation between 2±2° and 2±4° and Tsinopoulos et al13 measured the IOL rotation at on month postoperation (2.2±1.5°) and six month postoperation (2.7±1.5°) and found that the later rotation occurred between the one and six months was found to be more than one degree (1.1°) only in one eye (of 29 in the sample). These studies suggest us that a week after the surgery the refractive stability of the implanted eyes can be acceptable. Under our point of view, the changes in spherical and cylindrical refraction after the first week of the surgery may be due mainly to displacement and tilts of the IOL rather than to rotations.
The simple method used for the proper alignment of the IOL is valid and avoids errors due to natural cyclotorsion that occurs when the patient is placed supine.
It is convenient to perform the incision at the more curved meridian, in this way the IOL is practically on the desired axis when is deployed in the capsular bag and proper alignment is easier.
Anyway further studies may be needed to assess the refractive stability with longer follow-ups, the incidence of posterior capsular opacification, and the effect of YAG-capsulotomy on the rotational stability of the IOL.
One of the limitations of the study is the relatively short follow-up time and its retrospective design, which precluded collection of relevant data, such as intraocular cylinder stabilization after surgery and postoperative corneal astigmatism.
We conclude that the implantation of SN60T toric IOL in patients with CA higher than 0.75 D is a predictable way of reducing refractive astigmatism.
Conflict of interests
Authors declare that they don’t have any conflict of interests.
The authors thank Prof. M.S. Millán from Universitat Politècnica de Catalunya, for fruitful discussion. One of the authors (F. Alba-Bueno) acknowledges a PhD scholarship from UPC and thanks the Spanish Ministerio de Educación y Ciencia and FEDER for financial support under project DPI2009-08879.