To evaluate the efficacy of anti-suppression exercises in children with small-angle esotropia in achieving binocular vision.
MethodsA retrospective review of patients aged 3–8 years who underwent anti-suppression exercises for either monocular or alternate suppression between January 2016 and December 2021 was conducted. Patients with esotropia less than 15 prism diopters (PD) and visual acuity ≥ 6/12 were included. Patients with previous intra-ocular surgery or less than three-month follow-up were excluded. Success was defined as the development of binocular single vision (BSV) for distance, near, or both (measured clinically with either the 4 prism base out test or Worth four dot test) and maintained at two consecutive visits. Qualified success was defined as the presence of diplopia response for both distance and near. Additionally, improvement in near stereo acuity was measured using the Stereo Fly test.
ResultsEighteen patients with a mean age of 5.4 ± 1.38 years (range 3–8 years) at the time of initiation of exercises were included in the study. The male female ratio was 10:8. The mean best corrected visual acuity was 0.18 LogMAR unit(s) and the mean spherical equivalent was +3.8 ± 0.14 diopters (D). The etiology of the esotropia was fully accommodative refractive esotropia (8), microtropia (1), post–operative infantile esotropia (4), partially accommodative esotropia (1), and post-operative partially accommodative esotropia (4). Patients received either office-based, home-based, or both modes of treatment for an average duration of 4.8 months (range 3–8). After therapy, BSV was achieved for either distance or near in 66.6 % of patients (95 % CI = 40.03–93.31 %). Binocular single vision for both distance and near was seen in 50 % of children. Qualified success was observed in 38.46% of patients. Persistence of suppression was observed in one patient (5.5 %). Near stereopsis improved to 200 s of arc or more in 60% of the patients. The mean esotropia reduced from 5.7 ± 4.0 PD for distance and 6.2 ± 4.66 PD for near to 2.7 ± 2.4 PD and 3.38 ± 4.7 PD respectively, at the last follow-up (p-value 0.004 and 0.006). Failure of therapy was noticed after six months of follow-up in the child with infantile esotropia.
ConclusionAnti-suppression exercises may be beneficial to improve binocular vision functions in children with small-angle esotropias of variable etiologies. Recurrence of suppression after cessation of therapy is possible, warranting regular follow up.
Suppression is an adaptive mechanism by which there is active central inhibition of disparate and confusing images originating from the retina of the deviated or worse eye. Suppression is strictly limited to the binocular vision wherein the brain simply ignores the poorer eye image while maintaining foveal dominance under monocular viewing. It may be alternating or monocular, depending on the type of fixation used by the patient. Children with the onset of strabismus at an early age are highly susceptible to develop suppression in the non-fixing eye. The critical period for the development of suppression is similar to that of amblyopia, i.e. until 8–9 years of age.1 Similarly, it is at this age wherein anti-suppression exercises may help regain binocular vision and fusion in a child. Though a variety of exercises have been described, there are very few studies showing the effectiveness of these exercises in improving binocular vision in children with small-angle esotropia.
Accommodative esotropia is the most common type of inward deviation seen in children.2 Although full refractive correction reduces the deviation, orthotropia is seldom achieved, and children may continue to have small-angle esotropia (< 15 PD). Children develop strabismic amblyopia in one eye due to delay in presentation and noncompliance with glasses. The vision in such children almost always improves with appropriate patching or penalization of the better eye.3 However, evaluation of the sensory status reveals either suppression of the non-dominant eye or development of anomalous retinal correspondence (ARC). When compared to suppression, ARC is better as it allows some degree of binocular vision.4 Suppression, however, precludes binocularity. anti-suppression exercises will be more effective if instituted early within the premises of the critical period. They would make the child with small angle esodeviation aware of the second retinal image thereby promoting the development of either ARC or normal retinal correspondence (NRC) with diplopia. Children who start appreciating diplopia can then be encouraged for foveal fusion using vergence exercises and prisms.5
There is a scarcity of literature regarding the effect of anti-suppression exercises on improving binocular vision. Li et al.6 conducted a study to evaluate interocular suppression in anisometropic amblyopia. They found that suppression was measured less with rigid gas-permeable contact lenses than with glasses. However, they did not provide their subjects with anti-suppression exercises. In our practice, patients with suppression following strabismus or anisometropia are very common owing to delayed presentation. In our institution, anti-suppression exercises are routinely advised to children with small-angle esotropia. This study aimed to evaluate the success rate of these anti-suppression exercises in such children.
MethodsA retrospective chart review of patients with small angle esotropia who underwent anti-suppression exercises between January 2016 and December 2021 was performed. Appropriate approval was obtained from the Institutional Review Board and the chart review adhered to the tenets of Helsinki. Children between the ages of three and eight years with esotropia less than 15PD with uniocular or alternate suppression were included. The visual acuity in the worse eye was required to be 6/12 or better at the time of initiation of anti-suppression exercises. Children who had undergone amblyopia treatment in the past and were on maintenance patching (≤ 2 h/day) were included. Those with previous intraocular surgery, trauma, anisometropia (>1.5D Spherical Equivalent (SE)), eccentric fixation, or ARC were excluded. Eccentric fixation was assessed using the visuoscope (HEINE BETA®200, Germany). Abnormal retinal correspondence was considered when the patient saw four lights of the Worth four dot test (WFDT) for either distance or near fixation in the presence of manifest esotropia. Prior strabismus surgery was not an exclusion criteria. Patients with less than three months of follow-up post-anti-suppression therapy or those with incomplete records were excluded.
The presence of suppression was tested using both the 4 prism base out test (objective test) and WFDT (subjective test) for distance and near with patient wearing their best refractive correction. Sensory adaptations were also tested using Bagolini's striated glasses in all patients. However, we found that most children were unable to comprehend this test unlike WFDT which was easy to understand. Stereopsis for near was assessed using the Stereo fly test (Stereo Optical Company, Inc, Chicago IL) in all patients. Distance stereopsis was not measured. The presence of esotropia was detected using the cover test. The angle of deviation was measured using the alternate cover test and prisms.
All the subjects underwent either office-based (OBT) or home-based (HBT) anti-suppression therapies based on standard protocols of our binocular vision therapy clinic. The initial intensive treatment consisted of 10 sessions of OBT or four weeks of HBT. Thereafter, children who developed BSV were advised maintenance phase HBT for three months, and those who could not be continued intensive exercises for three additional months. If there was no improvement in binocular status after four months of well-compliant therapy, the exercises were stopped. The scheme of the treatment schedule is shown in Fig. 1.
Data recorded included age at presentation, age at initiation of anti-suppression therapy, gender, best corrected visual acuity (BCVA), refractive error, the etiology of esotropia, amount of deviation for distance and near, presence of amblyopia if any, details of patch therapy, binocular vision status, and stereopsis. The visual acuity was measured with Allen's pictures in preschool children and Snellen's or LogMar chart in school-going children. It was converted to LogMAR values for analysis. The mode, duration, and compliance with the therapy provided were recorded. Compliance was ascertained at each visit by questioning the parents. If the child had practiced the therapies on 75% of the days, he/she was included in the study. The total duration of follow-up and recurrences if any were documented.
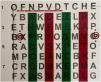
Office-based therapies included ten consecutive sittings, each consisting of 30–45 min of exercise. The exercises comprised of macular massage with auto flashing and chasing exercises on the synoptophore (Fig. 2), red-green HART chart (Fig. 3), and Cheiroscope (Fig. 4). The red-green HART chart (Bernell. Co) consist of a text with alternate vertical bands of red and green color. The child uses anaglyph red and green glasses to read the text through red-green stripes. Thus to read the text in continuity the child needs to use both eyes. The Cheiroscope is an instrument in which the patient looks through two eyepieces which are separated by an oblique mirror septum placed at an angle of 45° and each eyepiece has +7.0 diopter lenses. The better eye sees a pad of paper with a drawing or an object and the suppressed eye draws the same on the other side of the mirror. Based on the principle of haploscopy, this instrument promotes anti-suppression and improves hand-eye coordination.7,8 For HBT, the patients were advised Red-Green HART chart reading, and red-filter exercises like filling letter ‘O’ with red pen and drawing for 30 min every day. The red-filter exercises differ from the red-green HART chart reading. The red filter (the lens that blocks red color light) is worn in front of the suppressed eye as the good eye is occluded while the child uses a red color pencil or pen to do the writing tasks so that the suppressed eye's cone cells dominating fovea is stimulated. During the maintenance phase, only red-filter letter ‘O’ filling exercise was advised for 30 min each, two times a week.
Success was defined as the presence of BSV for either distance or near at two consecutive follow-up visits after initiation of the anti-suppression therapy. Qualified success was the presence of a diplopia response for both distance and near. If the suppression persisted despite four months of intensive therapy, it was considered a failure. Additionally, the presence of near stereo acuity of 200 s of arc or more was considered a good outcome. Recurrence was considered if there was a rebound of suppression at any time after successful treatment. Analysis of results was done using average values and confidence intervals for 95% limits. Descriptive statistics were used for baseline characteristics.
ResultsThe retrospective review identified eighteen children who fulfilled the inclusion criteria. The mean age at presentation was 5 years (range 3–7 years) and that at the time of initiation of anti-suppression exercises was 5.4 ± 1.38 years (range 3–8 years). The male: female ratio was 10:8. The etiology of esodeviation was fully accommodative refractive esotropia in eight patients, partially accommodative esotropia in one patient, post-operative infantile esotropia in four patients, postoperative partially accommodative esotropia in four patients, and microtropia in one patient. Ten subjects had unilateral amblyopia and were treated using appropriateocclusion therapy prior to the initiation of anti-suppression exercises. The mean BCVA at the time of initiation of exercises was 0.22 LogMar (range 0–0.3 LogMar) in the worse eye. The mean SE was 3.8 ± 0.14 D of hyperopia.
Seventeen patients had monocular suppression with fixation preference for one eye and one patient had alternate suppression. The average pre-therapy esotropia for distance was 5.7 ± 4.0 prism diopters (PD) (range 0–12 PD) and for near was 6.2 ± 4.66 PD (range 0–14PD). Near stereopsis was absent in ten subjects. The remaining eight subjects demonstrated low stereopsis levels ranging from 400 to 3000 s of arc for near.
Six children underwent OBT for the first ten days followed by home exercises, and eight children performed the HBT alone. Four patients started with HBT but were later supplemented with OBT for 10 sessions due to poor compliance with HBT. The average duration of exercises done was 4.5 ± 1.97 months (range 3–10 months). The mean duration of follow-up was 12 ± 8.63 months (range 3–34 months).
Binocular single vision was achieved for either distance or near fixation in 12 patients (66.6% (95% CI = 40.03–93.31%)). A successful outcome was seen as early as three weeks after initiation of the therapy to as late as four months. Binocular single vision for both distance and near was achieved in 9 patients (50%). Binocular single vision for distance was seen in 11 patients and for near was seen in 10 patients. Diplopia response for both distance and near was present in 5 patients (38.46%). It was observed in six patients for distance and in seven patients for near. None of these children complained of subjective diplopia. Persistence of suppression was observed in only one patient (5.5%). Table 1 shows the various combinations of the results of anti-suppression exercises. Those children who had developed diplopia response on sensory evaluation were started on therapies to stimulate bifoveal fusion with vergence exercises with or without prisms.
Summary of the results of the sensory tests after anti-suppression therapies in the eighteen patients.
| Result of anti-suppression therapy in the patients | |
|---|---|
| Suppression | 1 |
| Combination of BSV & diplopia | 3 |
| Diplopia for both D & N | 5 |
| BSV for both D & N | 9 |
D = distance, N = near, BSV = binocular single vision.
The mean esotropia reduced to 2.7 ± 2.4 PD for distance and 3.38 ± 4.7 PD at the last follow-up (p.). The status of retinal correspondence was determined based on the response to WFDT testing and the presence of esophoria/esotropia/orthophoria. A normal retinal correspondence (NRC) was present in 13 patients for distance fixation. Among them eight patients had BSV and five patients appreciated diplopia on WFDT. For near fixation NRC was achieved in 14 patients, among whom six patients had a diplopia response on WFDT and eight patients gave a BSV response. Anomalous retinal correspondence for distance fixation was seen in four patients and for near fixation in three patients.
Near stereopsis improved in all subjects except one patient with operated infantile esotropia. The average post-therapy near stereopsis was 223.33 ± 151.11 s of arc (range 0–400 s of arc). A near stereopsis of 200 s of arc or more was observed in 55.55 % of the patients. Recurrence of suppression was seen in three subjects of accommodative esotropia. Table 2 provides detailed data on the individual patients.
Results of anti-suppression exercises in patients with small angle esotropia.
BCVA, best corrected visual acuity; PD, prism diopters; HBT, home-based therapy; OBT, office-based therapy; RE, right eye; AE, fully accommodative esotropia; PAET, partially accommodative esotropia; s/p sx, status post strabismus surgery; IE, infantile esotropia; BSV, binocular single vision; ET, esotropia; EP, esophoria; ARC, anomalous retinal correspondence; NRC, normal retinal correspondence; f/b, followed by.
The treatment of suppression through anti-suppression exercises remains controversial. Anti-suppression exercises aim to make the sensory system aware of the second image arising from the deviated eye. In our study, 66% of the children with small-angle esotropia who were treated with anti-suppression exercises showed the presence of BSV after the therapy. There was an improvement in the near stereo acuity of all the patients. Arguments against these therapies are based on the possibility of the development of bothersome diplopia if the child is made aware of both images. In our study, eight esotropic children (44%) between 4 and 8 years of age, when treated with anti-suppression therapies showed NRC with five lights response in the WFDT for at least one of the fixation distances. None of these patients complained of subjective double vision in free space. Seven out of these eight patients also demonstrated the presence of near stereo acuity ranging from 100 to 400 s of arc. Children who showed diplopia response on the Worth 4 dot test were prescribed fusional vergence exercises with or without prisms to promote sensory and motor fusion. The results following the vergence therapy are not a part of the current study.
The WFDT is a relatively more dissociative test for sensory fusion.9 Though the WFDT tends to overestimate suppression, this should not affect the results of our study as the same test was used for both pre-and post-intervention assessments. We attempted Bagolini glasses testing on our patients, however, the children failed to comprehend the test accurately.
In our series, it was found that the esotropia was also reduced after the anti-suppression therapy. Ten children achieved orthophoria or esophoria at both distance and near fixation. Raveendran et al. showed that in strabismic amblyopes with small angle deviation, a reduction in the interocular suppression by reducing the contrast of the better eye improved the fixation stability.10 The fixational stability also improved with haploscopic alignment providing bifoveal images. This fixation stability was transient in their study and recurred when the contrast of the better eye returned to normal. We believe that the decrease in esotropia in our patients post-anti-suppression therapy occurred via the same mechanism. Two of the anti-suppression therapies employed in the current study were based on the haploscopic principle; the synoptophore and the cheiroscope. In both techniques, the fovea of the deviated eye was stimulated. The fixation stability was long-lasting in the patients in the current study since they did not have significant amblyopia. This is supported by the research findings of Gonzalez et al. which showed that the eye position stability is reduced in amblyopes in both monocular and binocular viewing conditions compared to normal patients.11
There were eight patients in which small angle esotropia persisted at the last follow-up visit. Five out of them showed the presence of a BSV response on WFDT for either of the fixation distances. These patients would have developed ARC following the anti-suppression therapy. The development of NRC with BSV is considered to be the best sensory outcome following treatment for strabismus. Anomalous retinal correspondence is nonetheless better than suppression, especially in microtropia.4 It enables a heterotropic patient to achieve the binocular single vision, diplopia-free vision and moderate stereo acuity. Whether fusional divergence exercises to reduce the esodeviation should have preceded the anti-suppression exercises to reduce or prevent the incidence of ARC is a matter of future research.
The results of our study should be interpreted in light of its retrospective design. The decision between the office or home-based therapies was based on patients’ convenience. Hence, this study cannot determine which type of therapy is better. Also compliance was ascertained by verbal feedback from parents so it may lead to bias. Around 16 children were undergoing maintenance patch therapy during the therapy period. Although it was ascertained that the visual acuity had stabilized for three months before the exercises were started, we cannot conclude definitively that patch therapy did not influence the results. The increase in visual acuity from the point of initiation of therapies and the last follow-up visit was noted. On average the vision in the worse eye improved by six letters and in the better eye by three letters. This could be partly attributed to the normal improvement in vision with growing age as around 50% of the subjects were below five years of age at the time of initiation of exercises. Thus, the most important limitation is probably the absence of a control group comprising of children who are on maintenance patch therapy only and their binocular status is analyzed.
Despite its limitations, this study explores the effect of anti-suppression exercises in small angle esotropia in children between ages 3 and 8 years. The study shows that children with acquired eso deviations retain their binocular potential and can be trained to utilize it. The risk of intractable diplopia remains low. Whether this active orthoptic therapy achieves better functional results than passive treatment such as monocular or alternating occlusion or no treatment at all is a matter of further research.
Financial disclosureNone of the author have any financial disclosure.
Source of fundingNone.
Previous presentationNone.
CRediT authorship contribution statementPreeti Sharma: Conceptualization, Data curation, Formal analysis, Writing – original draft, Writing – review & editing. Shailja Tibrewal: Conceptualization, Formal analysis, Writing – original draft, Writing – review & editing. Prem Kumar Singh: Conceptualization, Writing – original draft. Suma Ganesh: Conceptualization, Writing – review & editing.