Several previous clinical research studies1–6 have found the pattern visual-evoked potential (VEP) to be useful in detecting a wide range of visual-field defects objectively. In a previous study completed in our laboratory,6 circular, annular, hemi-field, and quadrant absolute visual-field defects were simulated and assessed objectively for detection and discrimination using the pattern VEP method. The results were clear and consistent, and thus encouraging. The group mean VEP amplitude exhibited a linear increase (y=0.805x+2; R=0.986) with increase in central circular field diameter. In comparison, the group mean amplitude decreased linearly (y=−0.769x+16.22; R=0.987) with increase in central blank field diameter for the annular stimuli. Lastly, VEP responses were able to differentiate between hemi- and quad-defects. No significant change in latency was found with any stimulus configuration. All of the aforementioned categories of simulated visual-field defects were detected with excellent repeatability. Thus, these findings suggested that the VEP could be used as an objective technique to detect different types of visual field defects rapidly and reliably. However, none of the previous studies further simulated and tested visual-field defects smaller than quadrants.1–6 Therefore, in the current study, our checkerboard pattern test field was further divided into eight horizontally oriented, rectangular stimulus regions (i.e., octants).
Thus, the purpose of the present study was to assess quantitatively the effect of simulated octant, absolute visual field defects on VEP responsivity in a visually normal adult population. This avenue was pursued to assess potential detectability of even smaller, simulated absolute visual-field defects than in previous investigations.
MethodsFive visually normal adults (ages 19–70 years) comprised of students and faculty at the college participated in the investigation. Each subject had a visual acuity of 20/20 monocularly and binocularly both at distance and near. None had any binocular dysfunction. Four subjects were emmetropic, and one was myopic with a spherical refractive correction of −2.50 diopters in each eye. The DIOPSYS™ NOVA-TR system (Diopsys, Inc., Pine Brook, New Jersey, USA) was used to generate the checkerboard pattern stimuli and to analyze the VEP data6. All testing was performed binocularly with full refraction in place. Details have been provided elsewhere.6
There were three stimulus patterns:
- 1.
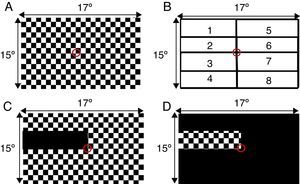
Full-field central stimulus – A standard central 64×64 (17H°×15V°), checkerboard pattern (20min arc check size at 1 meter, 90s test duration) was used as the baseline comparison stimulus, as well as to assess for normality of responses (Fig. 1A).
Figure 1.VEP visual field stimulus configurations. (A) Standard full-field checkerboard pattern stimulus with a small central fixation target. (B) Schematic of horizontal octant visual-field numerical designations. (C) Example of a 1/8th non-patterned (blank) visual field stimulus. (D) Example of a 1/8th patterned (non-blank) visual field stimulus. All not drawn to scale.
- 2.
1/8th non-patterned octant stimulus – 1 of the 8 regions of the checkerboard pattern was now non-patterned (i.e., blank), while the other 7 patterned octants were present (Fig. 1B and C).
- 3.
1/8th patterned octant stimulus – 1 of the 8 regions of the checkerboard pattern was patterned (i.e., the checkerboard was present), while the other 7 octants were non-patterned, or blank (Fig. 1D).
The study was approved by the Institutional Review Board (IRB) at the SUNY, State College of Optometry. Written informed consent was obtained from all subjects.
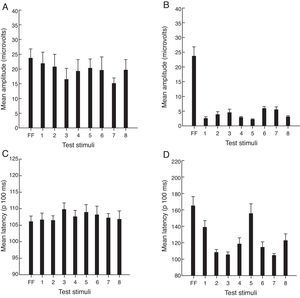
ResultsFig. 2 presents the group results for mean amplitude and latency (P100ms). Fig. 2A presents the mean amplitude for the full-field patterned and the 1/8th non-patterned octant stimulus configurations. A repeated-measures, one-way ANOVA for the factor of stimulus configuration was significant (p=0.0025). The post hoc Tukey test revealed the following significant (p=0.05) comparisons as related to the full-field value: octants 3 and 7. Fig. 2B presents the mean amplitude for the full-field patterned and the 1/8th patterned octant stimulus configurations. A repeated-measures, one-way ANOVA for the factor of stimulus configuration was significant (p=0.0001). The post hoc Tukey test revealed the following significant (p<0.05) comparisons as related to the full-field value: octants 1–8. Fig. 2C presents the mean latency for the full-field patterned and the 1/8th non-patterned octant stimulus configurations. A repeated-measures, one-way ANOVA for the factor of stimulus configuration was not significant (p=0.10). Fig. 2D presents the mean latency for the full-field patterned and the 1/8th patterned octant visual field stimulus configurations. A repeated-measures, one-way ANOVA for the factor of stimulus configuration was significant (p=0.0001). The post hoc Tukey test revealed the following significant (p<0.05) comparisons as related to the full-field value: octants 1–8.
Group data (n=5). (A) Mean amplitude for full-field (FF) patterned and individual octant 1/8th non-patterned visual field stimuli. (B) Mean amplitude for full-field (FF) patterned and individual octant 1/8th patterned visual field stimuli. (C) Mean latency (P100ms) for full-field (FF) patterned and individual octant 1/8th non-patterned visual field stimuli. (D) Mean latency (P100ms) for full-field (FF) and individual octant 1/8th patterned visual field stimuli. Plotted is the mean +1 SEM.
In addition, the same analyses were performed individually with regard to the amplitude data in each subject. Similar significant results were found in each subject, with excellent repeatability using the coefficient of variability metric.
DiscussionSeveral studies have used the VEP technique to assess central, hemifield, and quadrant visual field defects (see Yadav et al.,6 for details of these earlier studies). However, this is the first study to demonstrate that the pattern VEP technique could be used to detect and assess reliably small octant-sized, simulated, absolute visual-field defects. It serves as an extension to our previous investigation,6 in which simulated quadrant-sized, absolute visual-field defects were the smallest regions that were detected and quantitatively assessed. Therefore, the results of our current and past study provide additional, and mutually supportive, evidence that the patterned VEP method can be used to detect in a laboratory setting a range of simulated absolute visual-field defects, even smaller than a quadrant. This could be accomplished using the parameter of response amplitude for the isolated stimulus configuration (Fig. 1D); the related latency information proved to be too variable for the proposed assessment. These concepts and techniques should now be extended and tested in the clinical setting with appropriate patients (e.g., hemianopes).
The topics of clinical strategy and test time are critical. In the clinical domain, we suggest that only the amplitude-based information for the 1/8th isolated patterned condition should be employed. Thus, octant clinical testing of the potential visual-field loss would now be “targeted”. That is, based on the patient's symptoms and related clinical findings, including conventional visual-fields, OCT, etc., only a small region of the field would be assessed. For example, if the symptoms and clinical signs suggested a suspected problem in the upper right quadrant, then only octants 5 and 6 would be tested, with a total set-up and test time of approximately 10min. This is not especially long, including a short rest period between each octant assessment to minimize fatigue and maximize attention.
These findings, and the related suggested technique and protocol, should prove helpful to the clinician. The pattern VEP can now be extended even further and be used as a relatively rapid and simple objective technique to assess small absolute visual-field defects, especially in special populations (e.g., young children and those cognitively impaired), who may not be capable of responding reliably to traditional visual-field testing. Furthermore, the pattern VEP technique does not require subjective determination or any type of physical response (e.g., depressing a switch) by the patient. The proposed VEP test stimulus and protocol provides valuable information, which is relatively easily elicited, from individuals who have had stroke, victims of auto accidents who have suffered coup-contrecoup injuries to the brain, and essentially anyone who cannot respond reliably to traditional visual-field testing.6 This area deserves future detailed clinical investigation with larger sample sizes and a range of diagnostic conditions, e.g., glaucoma. We are currently testing adult stroke patients with hemianopia, and the preliminary findings are promising. The VEP is an important adjunct tool for the clinician in the detection and diagnosis of visual-field defects, and if found, then demonstrating them to the patient in a confirmatory manner in conjunction with the other related clinical findings.
The study and data accumulation were carried out with the approval from the SUNY, State College of Optometry, Institutional Review Board (IRB). Written informed consent was obtained from all subjects. We thank DIOPSYS™ Inc., Pine Brook, New Jersey, USA for providing the VEP system for the study.