High-energy visible (HEV) light has been the subject of considerable debate recently despite its critical role in several physiological functions. High-energy visible light–filtering spectacle lenses, which attenuate transmission of HEV light, are being widely marketed as protective measures for ocular health and interventions to improve visual function and sleep quality. This study reports on the effect of HEV light–filtering spectacle lenses on high and low contrast (10 % and 2.5 %) distance VA.
MethodsHigh and low contrast binocular distance VA was measured in 30 young adults in photopic and mesopic illumination. The VA measurements were taken with four test lenses including three commercially available HEV light–filtering lenses and a control lens. Data were analysed with descriptive and inferential statistics.
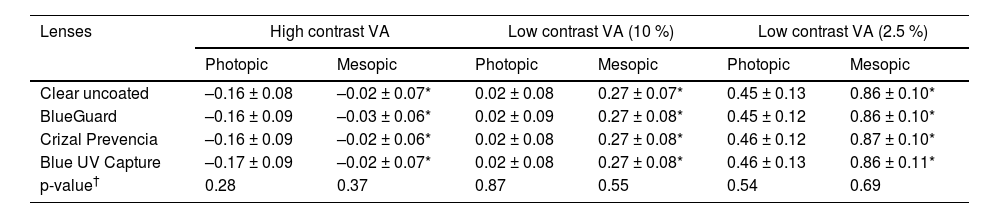
ResultsThere was no significant difference in mean photopic high contrast (F(2.5, 73.5) = 1.30, p = 0.28), low contrast 10 % (F(3, 87) = 0.24, p = 0.87) and 2.5 % (F(3, 87) = 0.72, p = 0.54) VA measurements with the four test lenses. Similarly, in mesopic illumination the mean VA measurements were similar among the four test lenses (high contrast (F(3, 87) = 1.06, p = 0.37), low contrast 10 % (F(3, 87) = 0.70, p = 0.55) and low contrast 2.5 % (F(3, 87 = 0.49, p = 0.69)).
ConclusionThe HEV light–filtering spectacle lenses produced no meaningful changes in VA compared with the control lens in varying illumination. Eye care personnel should consider this information when considering HEV light–filtering spectacle lenses in clinical practice.
High-energy visible (HEV) light corresponds to wavelengths ranging from 380 to 500 nm and is part of the visible spectrum. Although the sun is the greatest source of HEV light,1 changes in technology and behaviours may be increasing daily exposure to HEV light. For instance, light-emitting diode (LED) light bulbs and fluorescent light tubes are increasingly being used for indoor lighting.2 Furthermore, LED backlight displays in digital devices are now being ubiquitously used for various purposes. Although LEDs have better energy efficiency, they emit higher amounts of HEV light2,3 with peak emissions in the 460 to 490 nm range.4 Considering the current widespread presence of LEDs, concerns have been raised about increased exposure to this electromagnetic radiation. These concerns may be related to knowledge that a) short wavelength radiation has higher photon energy5 and b) HEV light is being associated with photochemical retinal damage in preclinical studies.6 Consequently, HEV light has been the subject of considerable debate despite its role in promoting alertness, mood and cognitive function, enhancing blue colour perception and scotopic vision and disrupting the circadian rhythm and sleep-wake cycle.5
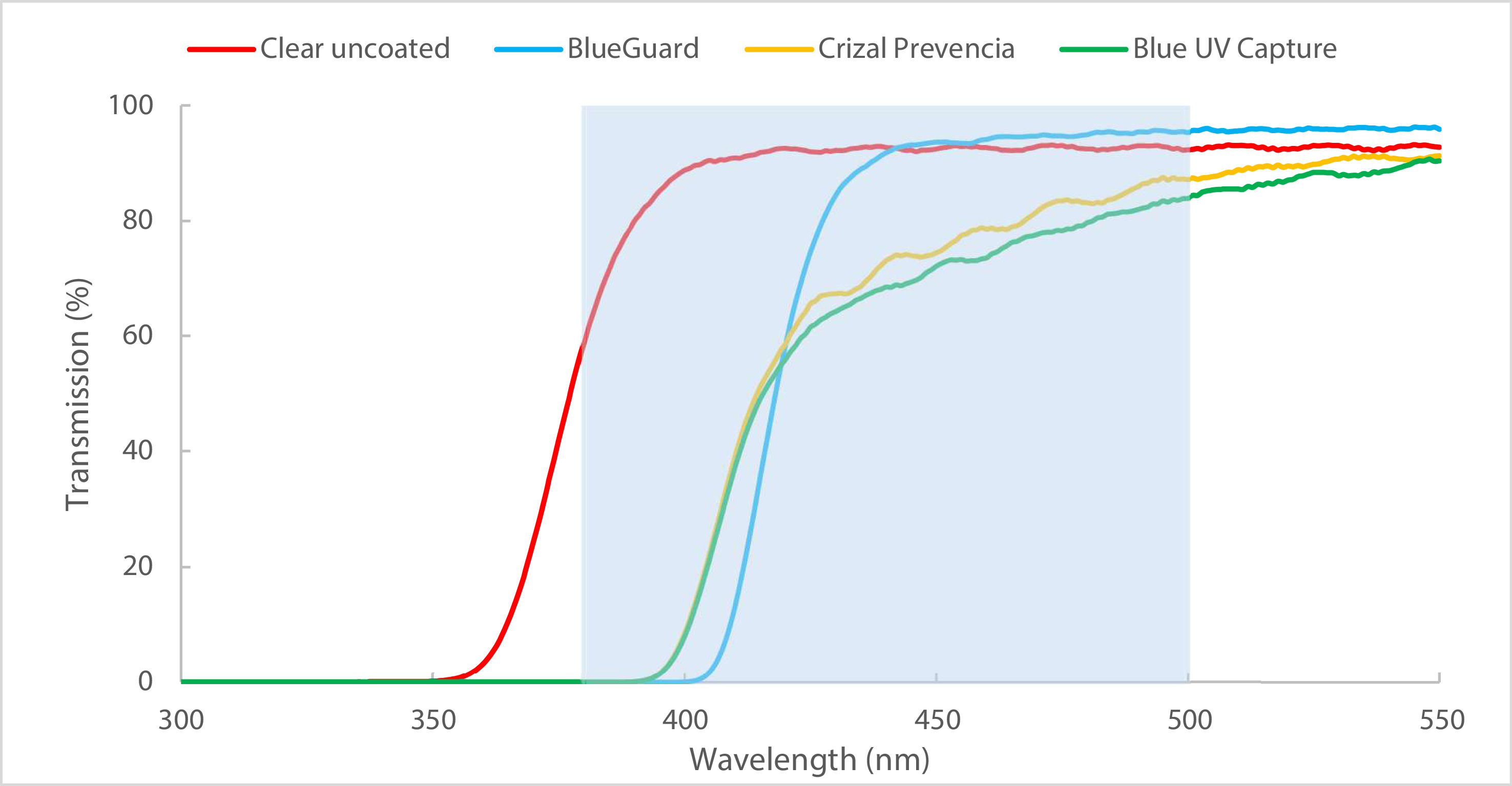
High-energy visible light–filtering, sometimes called light blocking, spectacle lenses are designed to selectively attenuate transmission of short wavelength HEV light.7 This is achieved using reflection or absorption principles by means of chromophores, interference surface coatings or both incorporated into these lenses.4,7 The older generation HEV light–filtering spectacle lenses effectively block HEV light with negligible transmission values (< 1 %) for wavelengths <500 nm and have a visible yellow hue.3,8 This contrasts with the modern generation HEV light–filtering spectacle lenses that show moderate attenuation of HEV light with transmission values between 57 % and 94 % and lack a discernable hue.9,10 Recently, these modern generation HEV light–filtering spectacle lenses are being widely marketed as both protective measures for ocular health and as interventions to improve visual function and sleep quality. However, scientific evidence to support the benefits of using HEV light–filtering spectacle lenses is unclear.1,4 The lack of consensus and high-quality evidence among researchers likely accounts for even popular media materials containing equivocal content about these lenses.11 For example, the Advertising Standards Authority in United Kingdom ruled that an optical chain retailer advertisement was misleading consumers with overstated claims about the harmful effects of HEV light as well as the benefits of using HEV light–filtering spectacle lenses.12
Despite optometrists acknowledging the uncertainty of evidence concerning HEV light–filtering spectacle lenses, they self-reported commonly prescribing these lenses.13,14 As these spectacle lenses are likely being worn for everyday tasks, it is important to understand their influence (if any) on visual performance. Previous studies have reported on the impact of modern generation HEV light–filtering spectacle lenses on colour discrimination,10,15 contrast sensitivity15,16 and photostress recovery times17 with limited attention to visual acuity (VA). Given that good VA is essential for tasks such as driving, reading etc., it is important to understand the influence of HEV light–filtering spectacle lenses on VA. Such information would be useful to optometrists and patients to better understand the consequences of wearing these lenses (if any). Therefore, the aim of this study was to determine the effect of HEV light–filtering spectacle lenses on high and low contrast distance VA.
Material and methodsEthical approval was obtained from the Biomedical Research Ethics Committee of the University of KwaZulu-Natal (reference number BREC/00004362/2022) and the study adhered to the tenets of the Declaration of Helsinki. Written informed consent was obtained from all participants prior to participation. The study used a quantitative research design and participants were recruited using convenience sampling. A priori sample size estimation showed that 27 participants were needed to detect a standardised effect size of 1.40, based on results from previous studies,18,19 with 90 % power and 5 % significance level.20 To account for incomplete data, the sample was increased by 10 % yielding a minimum sample size of 30.20 Anderson and Vingrys21 asserted that small samples are suitable for studies that evaluate whether a perceptual effect is present or absent. Consequently, the study was considered appropriately powered to detect whether or not HEV light–filtering spectacle lenses had any effect on high and low contrast distance VA rather than attempting to determine the magnitude of the effect in a particular population or attempting to compare the effect among different populations.21
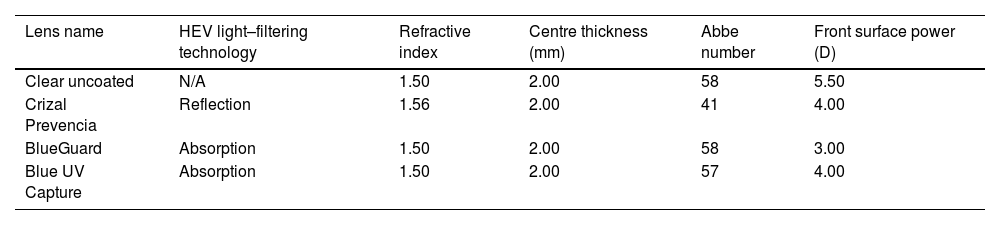
Table 1 shows the characteristics of the four test lenses included in the study. These lenses were obtained directly from two ophthalmic lens companies. The four test lenses were afocal plastic polished stock lenses with similar refractive indices and same centre thickness (Table 1). A clear uncoated lens served as the control. The three HEV light–filtering lenses use either reflection (Crizal Prevencia) or absorption (BlueGuard and Blue UV Capture) technologies to attenuate HEV light (Table 1). The test lenses were cut and mounted into full-aperture trial lens holders for ease of use. The spectral transmission curves of the four test lenses are shown in Fig. 1.
Characteristics of the four test lenses.
N/A: not applicable; HEV: high-energy visible; mm: millimetres; D: dioptres; UV: ultraviolet.
The sample consisted of healthy adults aged between 18 and 35 years to minimise the effect of ocular diseases on the distance VA measurements. All participants were screened for eligibility by assessing case history, Snellen distance VA, non-cycloplegic refraction (objective and subjective) and ocular health evaluation using white light assessment and ophthalmoscopy. Participants were included if they had unaided VA of 6/6 or better in each eye, emmetropia (spherical equivalent refraction ≤0.50 D in absolute value with maximum refractive astigmatism of 0.75 D),22 no history of ocular conditions, surgery or trauma and no ocular or systemic conditions.
Eligible participants proceeded to data collection wherein high and low contrast distance VA measurements were assessed using the Low Vision Resource Centre (LVRC) paper charts that conform with the Bailey-Lovie design principles.23 Such charts are considered the gold standard for quantifying VA and addressing the limitations of the Snellen chart.23 The VA measurements were taken binocularly, resembling habitual viewing, at a four meter testing distance. Low contrast VA was measured at two contrast levels namely 10 % and 2.5 % while high contrast VA was measured at ∼97 % contrast level. The high and low contrast distance VA measurements were taken in both photopic and mesopic lighting conditions. Participants wore mesopic filters (Good-Lite, USA) to simulate mesopic lighting as done in a previous study.24 The mesopic filters produce a uniform reduced lighting level of 3 cd/m2 that is within the stipulated mesopic light intensity level.24 The order of the lighting condition (starting with photopic or mesopic lighting) was counterbalanced to minimise any order effects and the VA measurements began after an adaptation period of 15 min in the lighting condition as done in a previous study.25 This time period was considered sufficient to prevent any effects from the previous lighting condition as more stable measurements of visual function have been noted after an adaptation period of 15 min.26 When adapting to mesopic lighting, participants wore the trial frame with the mesopic filters, and when adapting to photopic lighting, they wore the trial frame only.
After adapting to the lighting condition, the distance VA measurements were taken with the four test lenses. The order of the VA tests (high contrast, low contrast 10 % and low contrast 2.5 %) was randomised to minimise any learning effects as done in a previous study.27 Participants adapted to each test lens (with/without the mesopic filters for either photopic or mesopic lighting) for at least two minutes prior to measuring the VA. This time period was considered sufficient to prevent any effects of the previous test lens and is consistent with the lens adaptation period used previously.10,16,27 The order of presentation for the test lenses (control lens and the three HEV light–filtering lenses) was randomised to minimise any order effects. Participants were instructed to read aloud the letters in a vertical row from the top of the chart proceeding downwards. The threshold VA was determined using letter-by-letter scoring and participants were encouraged to read the optotypes but no feedback was provided on whether the optotype was correctly identified. The VA was recorded in logarithm of the minimum angle of resolution (logMAR) notation.23 Two versions of the high contrast LVRC chart (letters and numbers) were used to minimise learning effects. As there was only one version of the low contrast 10 % and 2.5 % charts, care was taken to minimise memorisation of the letter optotypes. This included using different vertical rows of letters when participants read from the top of the chart and randomly pointing to optotypes when determining the threshold VA.
For standardisation, a pilot study was performed and only one researcher performed all data collection tests in the same room with lighting provided by cool white fluorescent light tubes that remained unchanged. All room windows were covered with black roller blockout blinds to prevent stray light and the room illumination was 519 lx noted as the average of five measurements using a light meter (Digital Light Meter MT940, Voltex, Major TECH, Durban, South Africa). Participants were masked to the identity of the four test lenses to minimise any performance bias.
Data were captured and analysed using the Statistical Package for Social Sciences with results summarised using means, standard deviations, frequency counts, percentages and ranges. Normality of the VA measurements was assessed using the Shapiro-Wilk test and skewness and kurtosis statistics. The paired sample t-test was used to assess differences in mean VA measurements for the same test lens in photopic and mesopic lighting conditions. The one-way repeated measures analysis of variance (ANOVA) test was used to evaluate differences in mean VA measurements among the four test lenses in the same lighting condition. Mauchly’s test of sphericity tested for the assumption of sphericity and whenever this was violated, the appropriate correction was applied to modify the degrees of freedom. A probability (p) value of <0.05 was considered statistically significant.
ResultsThe sample consisted of 30 adults with more females (n = 26) than males (n = 4) with a mean age of 21.20 ± 1.40 years (range, 18 to 24). The mean spherical equivalent refraction was +0.04 ± 0.21 D (range, +0.50 to –0.25 D) and +0.05 ± 0.25 (range, 0.50 to –0.50 D) for the right and left eyes respectively. An equal proportion started with photopic (n = 15) and mesopic (n = 15) lighting. When all four test lenses were considered, the mean high contrast VA in photopic and mesopic lighting conditions was –0.17 ± 0.08 logMAR (range, 0.00 to –0.30) and –0.02 ± 0.07 logMAR (range, 0.14 to –0.18), respectively. The mean low contrast 10 % VA for the four test lenses in photopic and mesopic conditions was 0.02 ± 0.08 logMAR (range, 0.24 to –0.14) and 0.27 ± 0.08 logMAR (range, 0.50 to 0.10) respectively. For the low contrast 2.5 % VA measurement, the mean photopic VA was 0.45 ± 0.12 logMAR (range, 0.74 to 0.16) while the mean mesopic VA was 0.86 ± 0.10 logMAR (range, 1.00 to 0.64).
Table 2 shows the means and standard deviations for the high and low contrast VA measurements taken in photopic and mesopic conditions with the test lenses. The table shows that the higher the contrast level, the better the mean logMAR VA measurements and the smaller the difference between the mean photopic and mesopic VA measurements. For all test lenses, the mean photopic VA measurements were significantly better than the mean mesopic VA measurements for high contrast (t ≥ −11.80, p < 0.001), low contrast 10 % (t ≥ −15.17, p < 0.001) and low contrast 2.5 % (t ≥ −17.85, p < 0.001). The difference between the mean photopic and mesopic VA measurements was ∼0.14, ∼0.25 and ∼0.41 logMAR for the high, low 10 % and low 2.5 % contrast VA, respectively (Table 2). Mauchly’s test of sphericity showed the assumption of sphericity was violated only for high contrast photopic VA measurements as the variances of the differences were significantly different (x2(5) = 13.95, p = 0.02). Therefore, the degrees of freedom were corrected using the Huynh-Feldt estimate of sphericity (ε = 0.84) for high contrast photopic VA measurements. The results of the ANOVA analysis showed no significant difference in mean high contrast VA measurements in photopic conditions among the test lenses (F(2.5, 73.5) = 1.30, p = 0.28). Furthermore, the low contrast 10 % (F(3, 87) = 0.24, p = 0.87) and 2.5 % (F(3, 87) = 0.72, p = 0.54) VA measurements in photopic conditions were not significantly different among the test lenses (Table 2). Similarly, in mesopic conditions there was no significant difference in the mean VA measurements for high contrast (F(3, 87) = 1.06, p = 0.37), low contrast 10 % (F(3, 87) = 0.70, p = 0.55) and low contrast 2.5 % (F(3, 87 = 0.49, p = 0.69) among the test lenses (Table 2).
High and low contrast (10 % and 2.5 %) logMAR VA measurements (means ± standard deviations) for the test lenses in photopic and mesopic conditions.
| Lenses | High contrast VA | Low contrast VA (10 %) | Low contrast VA (2.5 %) | |||
|---|---|---|---|---|---|---|
| Photopic | Mesopic | Photopic | Mesopic | Photopic | Mesopic | |
| Clear uncoated | –0.16 ± 0.08 | –0.02 ± 0.07* | 0.02 ± 0.08 | 0.27 ± 0.07* | 0.45 ± 0.13 | 0.86 ± 0.10* |
| BlueGuard | –0.16 ± 0.09 | –0.03 ± 0.06* | 0.02 ± 0.09 | 0.27 ± 0.08* | 0.45 ± 0.12 | 0.86 ± 0.10* |
| Crizal Prevencia | –0.16 ± 0.09 | –0.02 ± 0.06* | 0.02 ± 0.08 | 0.27 ± 0.08* | 0.46 ± 0.12 | 0.87 ± 0.10* |
| Blue UV Capture | –0.17 ± 0.09 | –0.02 ± 0.07* | 0.02 ± 0.08 | 0.27 ± 0.08* | 0.46 ± 0.13 | 0.86 ± 0.11* |
| p-value† | 0.28 | 0.37 | 0.87 | 0.55 | 0.54 | 0.69 |
This study evaluated the effect of HEV light–filtering spectacle lenses on high and low contrast distance VA. Such information would be important as HEV light–filtering technologies are being incorporated into spectacle lenses and commonly prescribed despite limited knowledge of its effect on visual function.7,28 As there are currently no clinical practice or prescribing guidelines for HEV light–filtering spectacle lenses,7,15 there is a need for improved understanding of the effect of these spectacle lenses on visual function (if any). Such information would facilitate evidence-based discussions between eye care personnel and patients for more informed decisions when considering HEV light–filtering spectacle lenses in clinical practice.
Visual acuity tests evaluate the spatial resolution aspect of vision and are widely used to assess visual function.29 Physiologically, VA involves optical and neutral processing and may be affected by both optical and neural factors.29,30 Traditionally, distance VA is often measured under optimal photopic lighting using charts with maximum optotype contrast. Although high contrast photopic distance VA measures are routinely used, it is a poor indicator of everyday functional vision possibly as the testing environment and/or chart used are not always representative of real-world conditions.31 Furthermore, the photopic high contrast VA measurement may be insensitive to functional vision changes in early stages of certain ocular diseases and do not always correlate with patient symptoms.30 Also, the photopic high contrast VA measurement is only one aspect of visual function and may not accurately predict functional vision for everyday tasks.30,31 This is as everyday tasks usually occur in visually cluttered environments with varying illumination involving objects of varying contrast levels. Consequently, the traditional photopic high contrast VA test may be less informative of functional vision in environments with reduced lighting such as adverse weather conditions and at night.24 Therefore, evaluation of VA under low luminance conditions24 and/or using charts with different contrast levels30 may provide a better estimate of visual function in real-world conditions. For this reason, distance VA was evaluated using charts with different contrast levels and under two lighting conditions in this study.
The effect of the HEV light–filtering spectacle lenses on VA was determined by evaluating the differences in logMAR VA measurements among the four test lenses in the same lighting condition. The results showed no significant difference in mean high and low contrast (10 % and 2.5 %) VA measurements among the four lenses in both photopic and mesopic lighting conditions. This implies that the HEV light–filtering spectacle lenses produced no meaningful changes in high and low contrast distance VA measurements in either photopic or mesopic lighting compared with the control lens. These results align with previous studies32,33 that also showed no differences in mean VA measurements in normal individuals with and without spectacle lenses designed to reduce transmission of HEV light. For example, Hammond32 noted comparable VA measurements with HEV light–filtering clip-on spectacle lenses (0.051 ± 0.105 logMAR) and non-HEV light–filtering clip-on spectacle lenses (0.049 ± 0.099 logMAR) in a sample of 155 pseudophakes. Two recent systematic reviews concluded HEV light–filtering spectacle lenses33 and intraocular lenses34 have no effect on best-corrected VA. The negligible impact on VA in this study is likely explained by the modest attenuation of HEV produced by these modern generation HEV light–filtering spectacle lenses. It is well-known that intraocular scattering is higher with shorter wavelength visible light18 and such scattering reduces contrast sensitivity and consequently, VA. Thus, the reduced transmission of HEV light and consequently intraocular scattering produced by HEV light–filtering lenses should improve optical quality and visual function. However, it seems that effects on visual function depend on the transmission profile of the filters blocking HEV light and the optical media of participants. For instance, other researchers19,35 reported that filters blocking HEV light, which blocked higher amounts of HEV light with a discernible yellow hue, improved VA in individuals with dry eye (n = 22)19 and in a preliminary study involving two elderly participants (≥ 70 years). It is also likely that the characteristics of the ocular media with ageing and in dry eye disease may have made the reduction in intraocular scattering more considerable further accounting for the improved optical quality and consequently VA noted previously.19,35
In this study, the lack of differences in VA measurements between the control lens and the HEV light–filtering lenses may be explained by various factors. Firstly, the modern generation HEV light–filtering lenses included in this study show relatively low attenuation of HEV light and the sample consisted of healthy adults. The reported effect of HEV light–filtering lenses on visual function depends on the test used8. The lack of differences in VA measurements suggests that either the VA tests could not detect the small changes or that the HEV light–filtering spectacle lenses resulted in changes that were lower than the recognition threshold of participants. Even the characteristics of the stimuli in the test are likely to impact the results as achromatic stimuli may be affected to a lesser extent than chromatic stimuli particularly if the colour corresponds to the wavelength of light being selectively attenuated by the lens.16 As the optotypes in the high and low contrast distance VA tests were achromatic, future studies should investigate VA measurements using chromatic, particularly blue coloured, targets to see if there are any differences. Alternately, the results imply that objective changes in distance VA measurements may not be noticeable with short term use of HEV light–filtering spectacle lenses. Therefore, patients’ subjective functional vison reports when using these spectacle lenses should also be considered.
High contrast photopic VA measurements represent functioning of the cone photoreceptors in the central retina.24 During photopic illumination, cones are the primary photoreceptor for vision and visual perception contributing to high spatial acuity and colour perception. During mesopic illumination, both cones and rods are functioning contributing to visual perception although the exact nature of their interactions and physiology are unclear.36 As expected, the mean VA measurement, when the four test lenses were considered, deteriorated and was poorer under mesopic than photopic conditions (–0.02 ± 0.07 versus –0.17 ± 0.08 logMAR). This trend of reduced VA when luminance decreased has been noted previously.25,37–39 These results could be explained by the increased pupil size and consequent impact on depth of field, decrease in retinal illuminance40 and that both rod and cone photoreceptors are stimulated in mesopic conditions.24 Comparable VA measurements were reported by Garcia-Rojo et al.37 for photopic (–0.09 ± 0.01 logMAR) and mesopic (–0.06 ± 0.06 logMAR) VA. In contrast, Hiraoka et al.38 reported photopic and mesopic VA of –0.11 ± 0.08 logMAR and 0.39 ± 0.12 logMAR, respectively implying that the mesopic VA was almost four lines worse. This could be attributed to the lower mesopic illuminance used (0.1 ± 0.01 cd/m2) and that data from only the right eye was considered by Hiraoka et al.38 In this study, the high contrast VA in mesopic lighting conditions was reduced but still relatively good (–0.02 LogMAR or ∼6/6). This may be as the mesopic luminance was 3cd/m2 and more significant changes in mesopic VA are noted only with mesopic luminance <1.0 cd/m2.24 Furthermore, the difference between the mean photopic and mesopic VA measurements was ∼0.14 logMAR or ∼7 letters in this study. Wood et al.24 recommended that further clinical investigation is needed when this difference is greater than 13 letters. Despite this, the reduced VA measurements in mesopic conditions necessitates that eye care personnel continue to advise patients of reduced visual capabilities in environments with reduced lighting.
Strengths of this study include use of commercially available HEV light–filtering spectacle lenses, a control lens with similar characteristics and that participants were masked to the lens being tested. Furthermore, VA measurements were taken in two lighting conditions that were counterbalanced. Limitations include that the VA measurements were taken at one point in time and not monitored continuously. Consequently, the influence of these HEV light–filtering spectacle lenses over a longer duration particularly in reduced lighting remains unknown. Also, these results may not be generalised to older individuals and those with ocular diseases. Therefore, future studies should investigate the effect of HEV light–filtering lenses on VA in older individuals and those with disorders of the ocular media. Furthermore, participants were not screened for non-strabismic binocular vision anomalies, such as divergence insufficiency basic exophoria, basic esophoria and accommodative excess, that may cause intermittent blur and diplopia at distance and this should be considered in future research. The study was not designed to provide reference values for VA measurements with HEV light–filtering spectacle lenses and that could be investigated in future studies with larger samples. Although the HEV light–filtering lenses had no effect on high and low contrast VA, they may provide other advantages such as reducing glare and light scattering. However, these were not evaluated in the present study and should be considered in future studies. Lastly, these results are limited to the three commercially available HEV light–filtering lenses used and it is possible that other lenses may show different VA measurements.
ConclusionThis study showed no meaningful differences in mean VA measurements among the four test lenses. These results provide a baseline for future work on the effect of HEV light–filtering spectacle lenses on visual performance. Furthermore, these results may provide useful information concerning distance VA for eye care personnel who prescribe HEV light–filtering spectacle lenses in clinical practice.
Data availability statement: Data generated for the study is available on request from the corresponding author.
Ethics approval statementEthical approval for the study was obtained from the University of KwaZulu-Natal Biomedical Research Ethics Committee (BREC/00,004,362/2022).
FundingThis work is based on the research supported by the National Research Foundation of South Africa (Grant Number 138247).
None.
The authors thank Dr Z Dessie for assistance with the statistical analysis.