To evaluate the influence of age on visual and refractive results after laser-assisted subepithelial keratomileusis (LASEK) with the adjuvant use of mitomycin C (MMC) for the correction of myopia.
MethodsRetrospective, nonrandomized, cohort study. A total of 1374 eyes treated with LASEK+MMC were included in the study (we compared 1163 eyes of patients aged 18 to 40 years versus 211 eyes of patients over 40 years). Visual and refractive results were evaluated at the 6-month postoperative visit.
ResultsSix months postoperatively, both the uncorrected distance visual acuity and the corrected distance visual acuity were significantly better in the group of young patients (P=0.0001). We found a slight tendency to overcorrection in the group of young patients compared to a slight tendency to undercorrection in the group of patients over 40 years (P=0.002). The efficacy index was significantly better in the group of younger patients (0.91±0.2) than in the older patients (0.86±0.2) (P=0.0001). No significant difference was found in the safety index between groups. 81.5% of eyes in the group of patients aged 18 to 40 years compared to 75.3% of eyes in the group of patients aged >40 years were within±0.5D of emmetropia (P=0.001).
ConclusionsA tendency toward undercorrection and less predictability was found with aging after myopic LASEK with MMC for the correction of myopia.
Evaluar la influencia de la edad sobre los resultados visuales y refractivos tras queratomileusis subepitelial asistida por láser (LASEK) con uso adyuvante de mitomicina C (MMC) para la corrección de la miopía.
MétodosEstudio de cohorte retrospectivo y no aleatorizado. Se incluyó en el estudio a un total de 1.374 ojos tratados con LASEK+MMC (comparamos 1.163 ojos de pacientes de edades comprendidas entre 18 y 40 años, con 211 ojos de pacientes mayores de 40 años). Los resultados visuales y refractivos se evaluaron durante la visita postoperatoria transcurridos 6 meses.
ResultadosA los seis meses de la intervención, tanto la agudeza visual de lejos no corregida como corregida fueron mejores en el grupo de pacientes jóvenes (P=0,0001). Encontramos una ligera tendencia hacia la sobre-corrección en el grupo de pacientes jóvenes, en comparación a una ligera tendencia hacia la infra-corrección en el grupo de pacientes mayores de 40 años (P=0,002). El índice de eficacia fue significativamente mejor en el grupo de pacientes jóvenes (0,91±0,2) que en el de pacientes mayores (0,86±0,2) (P=0,0001). No se encontró diferencia significativa en cuanto al índice de seguridad entre grupos. El 81,5% de los ojos del grupo de pacientes con edades comprendidas entre 18 y 40, en comparación con el 75,3% de los ojos en el grupo de pacientes mayores de >40 años, reflejó un valor±0,5D de emetropía (P=0,001).
ConclusionesSe encontró una tendencia hacia la infra-corrección y menor predecibilidad con la edad tras la realización de LASEK con MMC para la corrección de la miopía.
Excimer laser surface ablation (SA) procedures, such as photorefractive keratectomy (PRK) and Laser-assisted subepithelial keratomileusis (LASEK), have been shown to be safe, effective, and predictable procedures to correct different degrees of myopia.1–5 Despite the disadvantages of SA techniques (i.e. slower visual recovery and higher postoperative discomfort compared to laser in situ keratomileusis [LASIK]), these procedures have become the technique of choice in corneas with inferior steepening on corneal topography without keratoconus, patients with thin central corneal thickness, those at risk of trauma, and those in which epithelial problems are anticipated, such as patients with recurrent erosion syndrome, dry eye, or basement membrane disease.6
Patient age is an important variable that affects the visual outcomes of corneal refractive surgical procedures.7,8 In fact, some studies have reported suboptimal results with LASIK associated with increasing age,8–14 perhaps as a result of a decreased wound-healing response.8 Nevertheless, only three studies have evaluated to date the influence of age on visual results after SA (none of them used mitomycin C -MMC-), showing contradictory results. Hefetz and colleagues15 found no significant differences in the residual refraction among different age groups whereas Loewenstein et al.16 and Rao et al.7 reported a trend to overcorrection with aging. For this reason, and in order to improve the predictability of LASIK and SA, Luger and associates14 proposed laser nomogram adjustments based on age to increase the amount of correction in younger patients. In contrast, older patients might have to be intentionally undercorrected7,8,14 to account for the diminished wound-healing response. However, the percentage of undercorrection in older patients remains unclear.
On the other hand, it is well accepted that the intraoperative use of MMC tends to reduce the corneal wound-healing after laser ablation, causing a tendency to overcorrection that needs to be compensated for with an appropriate adjustment of the laser nomogram.17–22 Nevertheless, we are unaware of previous reports of the predictability of LASEK in different age groups, when intraoperative MMC is used.
For this reason, and given the importance that this issue could have on refractive results after SA, we decided to evaluate the effect of age on visual and refractive outcomes after LASEK+MMC in a large sample of patients, applying a double nomogram adjustment: an age-based nomogram, and a 10% fixed undercorrection from the intended spherical correction due to the use of MMC.
MethodsWe performed a retrospective study of consecutive eyes that underwent LASEK with intraoperative use of MMC to correct their myopia (with or without astigmatism). In presbyopic patients, when conventional monovision was planned, only the dominant eye (targeted for emmetropia) was included in the study. All the surgeries were performed at the same clinic and by two experienced surgeons from January 2015 till January 2017.
A masked observer performed the same full preoperative examination for all patients that included measurement of the uncorrected distance visual acuity (UDVA), corrected distance visual acuity (CDVA) including the manifest and cycloplegic refractions, corneal keratometry and topography (CSO, Compagnia Instrumenti Oftalmici, Florence, Italy), ultrasound corneal pachymetry (DHG 5100 contact pachymeter; DHG Technology Inc., Exton, PA), mesopic infrared pupillometry (Colvard Pupillometer, Oasis Medical Inc., Glendora, CA), slit-lamp biomicroscopy, Goldmann tonometry (CT-80, Topcon, Tokyo, Japan), and funduscopy.
When evaluated for refractive surgery, we excluded patients with unstable refractions; those who had undergone a previous ocular surgery (refractive or other surgical procedure); keratoconus suspects (defined as any even mild localized steepening seen with Placido corneal topography or slight bowing of the posterior corneal surface detected by corneal tomography); and those with ocular or systemic diseases, such as diabetes mellitus or connective tissue disorders, that could interfere with the wound-healing process.
All patients provided written informed consent, and the Institutional Review Board approval was obtained. The study was performed in accordance with the tenets of the Declaration of Helsinki.
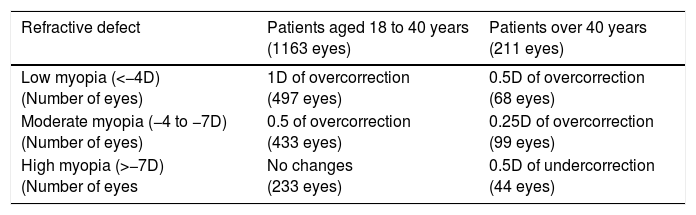
Surgical techniqueTwo experienced surgeons (M.G.-G. and M.A.T.) performed all the procedures. A povidone-iodine solution was applied to the skin and the conjunctiva, and a sterile surgical drape and a rigid eyelid speculum were positioned. All surgeries were performed using topical anesthesia with lidocaine 2%. A 20% alcohol solution diluted in balanced salt solution (BSS) was instilled inside a 7-mm corneal trephine (ASICO, Westmont, Ill) centered on the pupil and left for 40s. A cellulose sponge was used to remove the alcohol, and BSS was copiously instilled to rinse the ocular surface. The edges of the flap were dried with a sponge and the epithelial flap was peeled back with a crescent blade (Alcon Surgical, Orlando, FL), leaving a hinge at the 12 o’clock position. The stromal bed was dried with a sponge and the eye tracker was set in the center of the pupil. The ablation was performed with the Esiris excimer laser (Schwind Eye Tech Solutions, Kleinostheim, Germany) using an age-based PRK nomogram (provided by the manufacturer) as described in Table 1. In addition, and due to the use of MMC, the programmed spherical ablation was 10% less than the intended correction (independently of patient age) in order to avoid overcorrection.
Age-based laser nomogram (provided by the manufacturer) applied in the 1374 eyes that underwent LASEK with Mitomycin C for the correction of myopia. These changes in the nomogram were applied over the intended spherical refraction. The cylinder programmed ablation did not need to be modified.
| Refractive defect | Patients aged 18 to 40 years (1163 eyes) | Patients over 40 years (211 eyes) |
|---|---|---|
| Low myopia (<−4D) (Number of eyes) | 1D of overcorrection (497 eyes) | 0.5D of overcorrection (68 eyes) |
| Moderate myopia (−4 to −7D) (Number of eyes) | 0.5 of overcorrection (433 eyes) | 0.25D of overcorrection (99 eyes) |
| High myopia (>−7D) (Number of eyes | No changes (233 eyes) | 0.5D of undercorrection (44 eyes) |
D=diopters.
Because the ablation depth exceeded 50μm in all cases, a 7mm round cellulose sponge soaked in MMC 0.02% was applied for 30seconds over the ablated stroma, carefully avoiding leakage of the drug to the epithelial flap and the limbus. The stroma was then copiously rinsed with BSS and the epithelial flap was repositioned using the same cannula. A therapeutic soft contact lens (AcuVue; Johnson & Johnson Vision Care Inc, Jacksonville, FL) was carefully placed on the eye and antibiotic drops (ciprofloxacin 3mg/ml) and nonsteroidal anti-inflammatory drops (ketorolac trometamol 5mg/ml) were applied.
Postoperative follow-upThe medications consisted of topical antibiotic (ciprofloxacin 3mg/ml) and steroid (dexamethasone alcohol 1mg/ml) drops four times daily during the first postoperative week. Steroid drops were tapered over the subsequent two months: three times daily the first month, twice daily for the following 15 days, once daily for another 15 days, and then stopped. The therapeutic contact lens was removed one week after surgery.
Postoperative examinations were scheduled for 1 day, 1 week, 1, 3 and 6 months after surgery. Two experienced optometrists refracted the patients at each postoperative visit. All patients were refracted in the same room with the same light adjusted to mesopic conditions. Six months postoperatively, a complete ocular examination including corneal topography was performed in all patients. Indeed, an exhaustive slit-lamp biomicroscopy exam was performed to rule out changes in crystalline lens that could induce some myopic defect that would jeopardize the final refractive outcomes, especially in older patients.
Statistical analysisThe Statview+Graphics software (Abacus Concept Inc., Cupertino, CA) was used for the statistical analyses, using a two-tailed unpaired Student's t-test and linear regression analysis when appropriate. A P value <0.05 was considered significant. The data are expressed as the mean±standard deviation (SD). Although the minimum angle of resolution (logMAR) values of all visual acuity tests were used for the statistical analyses, we converted them to the more conventional Snellen quotation (decimal scale) throughout the text using a visual acuity conversion chart.
To analyze the effect of age on the visual and refractive results, the patients were divided into two groups, according to the age-based nomogram applied. One group included all patients 18 to 40 years, and the other group included all patients over 40 years.
ResultsA total of 1374 eyes treated with LASEK+MMC were included in the study. The mean patient age was 32.5±7.4 years (range, 18 to 65 years). The mean preoperative spherical refraction was −4.33±2.5 diopters (D) (range, −1.00 to −10.00 D). The mean preoperative cylinder was −1.22±1.2 D (range, 0 to −6.50D). The mean preoperative spherical equivalent (SE) was −4.94±2.6D (range, −1.00 to −10.00 D). The mean preoperative CDVA was 1.09±0.19 (range, 0.3 to 1.25). The optical zone of the laser ablation was 6.25±0.5mm (range, 5 to 7.5mm).
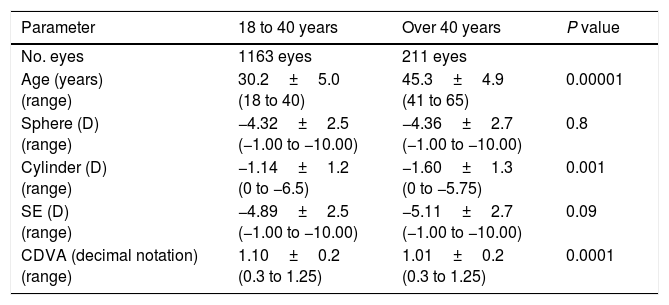
We compared 1163 eyes of patients aged from 18 to 40 years versus 211 eyes of patients over 40 years. The preoperative data from the two age groups are shown in Table 2. Because of the large number of eyes included in the study, the analyses identified significant differences in some of the preoperative data between groups even if these differences were minute and subsequently, not clinically relevant. In fact, in both age groups the mean preoperative CDVA was higher than 1.0 (1.10 in the group of patients aged 18 to 40 versus 1.01 in the group of patients over 40 years) and thus, we believe that a difference in the mean preoperative CDVA of just 0.09 (decimal notation) was probably not clinically relevant even if this difference was statistically significant due to the large sample size analyzed. Moreover, even if the mean preoperative cylinder was significantly lower in the group of younger patients (−1.14D) compared to the group of patients over 40 years (−1.60D), no statistically significant differences were found in the preoperative spherical equivalent, and therefore, we do believe that both groups were comparable in terms of preoperative refraction.
Preoperative data of 1374 eyes that underwent LASEK with Mitomycin C divided into two age groups based on the age-related nomogram applied. Data are expressed as the mean±standard deviation.
| Parameter | 18 to 40 years | Over 40 years | P value |
|---|---|---|---|
| No. eyes | 1163 eyes | 211 eyes | |
| Age (years) (range) | 30.2±5.0 (18 to 40) | 45.3±4.9 (41 to 65) | 0.00001 |
| Sphere (D) (range) | −4.32±2.5 (−1.00 to −10.00) | −4.36±2.7 (−1.00 to −10.00) | 0.8 |
| Cylinder (D) (range) | −1.14±1.2 (0 to −6.5) | −1.60±1.3 (0 to −5.75) | 0.001 |
| SE (D) (range) | −4.89±2.5 (−1.00 to −10.00) | −5.11±2.7 (−1.00 to −10.00) | 0.09 |
| CDVA (decimal notation) (range) | 1.10±0.2 (0.3 to 1.25) | 1.01±0.2 (0.3 to 1.25) | 0.0001 |
D=diopters; SE=spherical equivalent; CDVA=corrected-distance visual acuity; NS=not significant.
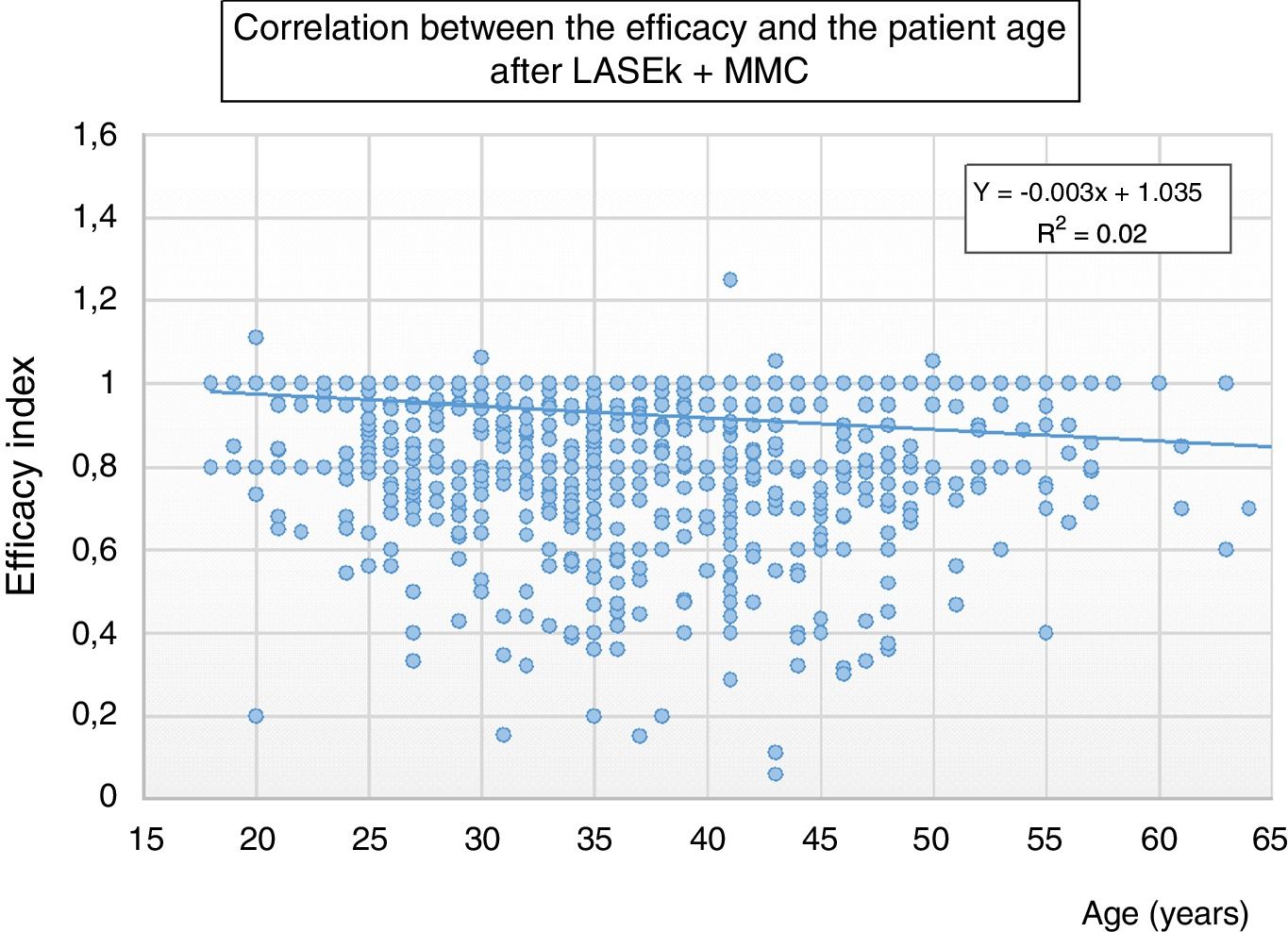
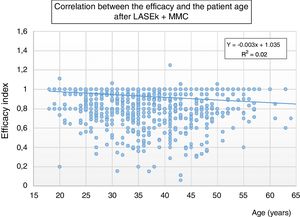
Six months postoperatively, linear regression analysis showed a significant correlation between age and the efficacy index (P=0.0001, r2=0.01); i.e., LASEK+MMC tended to provide less efficacy with aging (Fig. 1). No significant correlation was found between age and the postoperative SE (P=0.1), neither between age and the safety index (P=0.8).
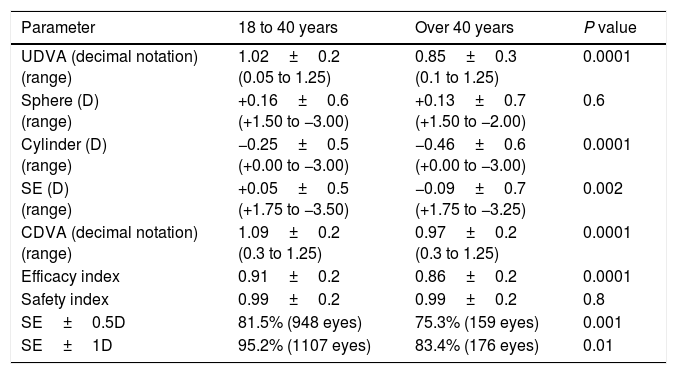
Table 3 shows the postoperative data and the comparison of the different parameters between the group of patients aged from 18 to 40 years and the group of patients over 40 years.
Visual and refractive results 3 months after LASEK with Mitomycin C for the correction of myopia in both age groups. Data are expressed as the mean±standard deviation.
| Parameter | 18 to 40 years | Over 40 years | P value |
|---|---|---|---|
| UDVA (decimal notation) (range) | 1.02±0.2 (0.05 to 1.25) | 0.85±0.3 (0.1 to 1.25) | 0.0001 |
| Sphere (D) (range) | +0.16±0.6 (+1.50 to −3.00) | +0.13±0.7 (+1.50 to −2.00) | 0.6 |
| Cylinder (D) (range) | −0.25±0.5 (+0.00 to −3.00) | −0.46±0.6 (+0.00 to −3.00) | 0.0001 |
| SE (D) (range) | +0.05±0.5 (+1.75 to −3.50) | −0.09±0.7 (+1.75 to −3.25) | 0.002 |
| CDVA (decimal notation) (range) | 1.09±0.2 (0.3 to 1.25) | 0.97±0.2 (0.3 to 1.25) | 0.0001 |
| Efficacy index | 0.91±0.2 | 0.86±0.2 | 0.0001 |
| Safety index | 0.99±0.2 | 0.99±0.2 | 0.8 |
| SE±0.5D | 81.5% (948 eyes) | 75.3% (159 eyes) | 0.001 |
| SE±1D | 95.2% (1107 eyes) | 83.4% (176 eyes) | 0.01 |
UDVA=uncorrected distance visual acuity; D=diopters; SE=spherical equivalent; CDVA=corrected-distance visual acuity.
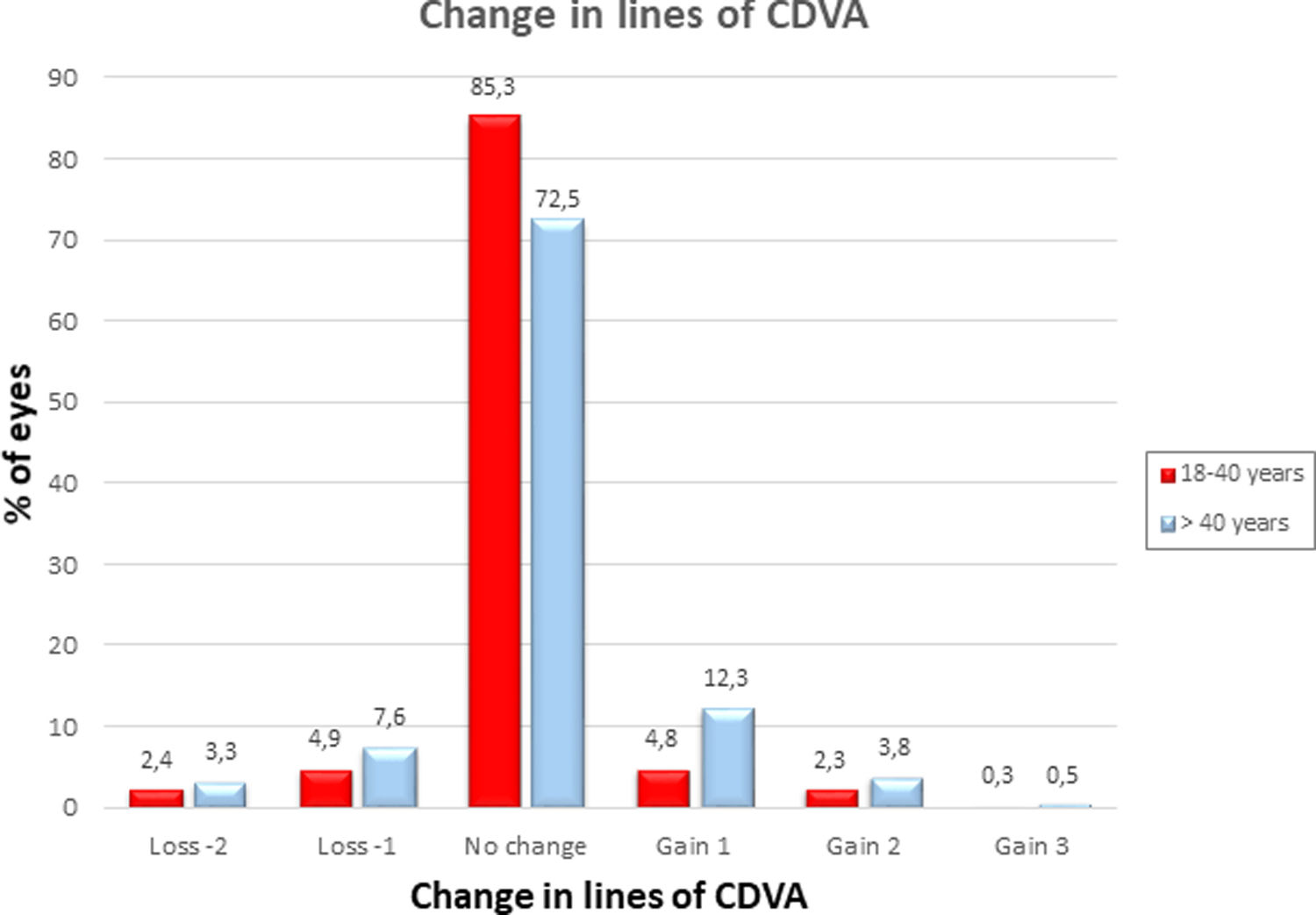
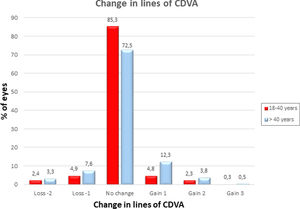
Both the UDVA and the CDVA were significantly better in the group of young patients (P=0.0001). Regarding the postoperative SE refraction, we found a slight tendency to overcorrection in the group of young patients (the mean postoperative SE was +0.05±0.5D) compared to a slight tendency to undercorrection in the group of patients over 40 years (the mean postoperative SE was −0.09±0.7D) (P=0.002). The efficacy index was significantly better in the group of younger patients (0.91±0.2) than in the older patients (0.86±0.2) (P=0.0001). No significant difference was found in the safety index between groups. 86 eyes (7.4%) in the group of patients aged 18 to 40 years compared to 35 eyes (16.6%) in the group of patients over 40 years gained 1 or more lines of CDVA, whereas 85 eyes (7.3%) versus 23 eyes (10.9%) lost 1 or more lines of CDVA in the groups of patients aged 18–40 years and >40 years, respectively. Changes in lines of CDVA in both age groups are shown in Fig. 2.
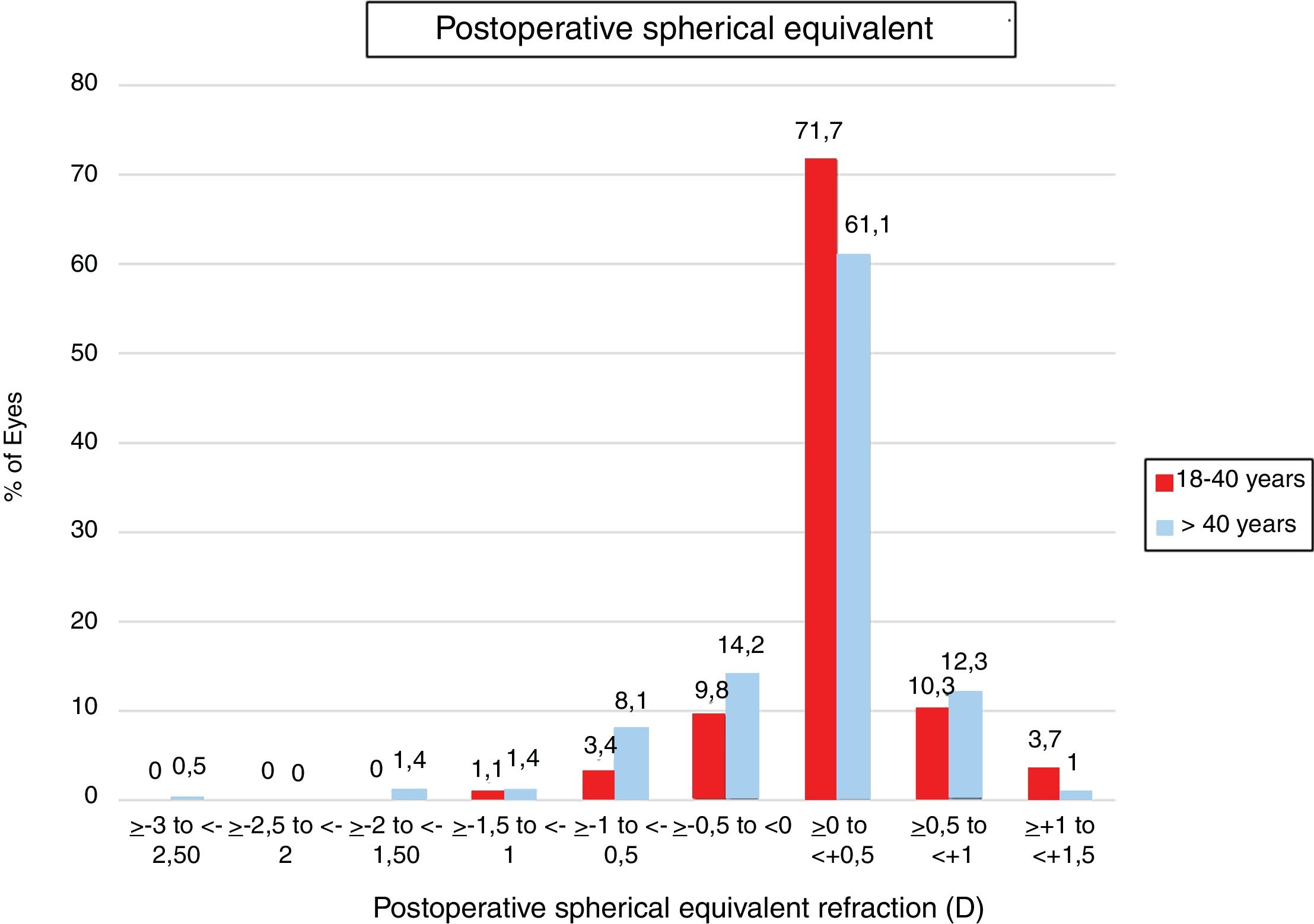
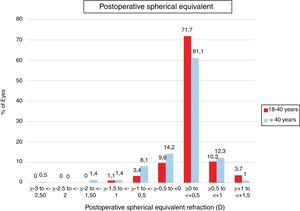
Regarding predictability, LASEK+MMC provided significantly better results in the group of patients aged 18 to 40 years. In fact, 81.5% of eyes in the group of patients aged 18 to 40 years compared to 75.3% of eyes in the group of patients aged >40 years were within ±0.5D of emmetropia (P=0.001). Predictability of LASEK+MMC in both age groups is shown in Fig. 3.
No intraoperative or early postoperative complications and no problems with epithelial healing were detected. No case of haze of more than grade 1 (mild, not affecting visual acuity or refraction) was registered during any postoperative visit.
DiscussionIn the current study, LASEK with intraoperative use of MMC showed to be a safe, effective, and predictable procedure for the treatment of myopia in different age groups. However, when using an age-based excimer laser nomogram, a slight tendency toward undercorrection and less efficacy and predictability were found with increasing age.
Patient age has been considered as an important variable that affects the visual outcomes of corneal refractive surgical procedures.8–14,23 In fact, some studies have reported suboptimal visual results with LASIK associated with increasing age,8–14 such as higher retreatment rates,8–11 decreased patient satisfaction12 and increased night vision complaints.13 In contrast, only three studies have evaluated to date the influence of age on visual outcomes of SA procedures7,15,16 (none of them used MMC), showing contradictory results.
Hefetz and associates15 reported the results of PRK to correct myopia from -2D to −10.25D in 599 eyes. The authors found no significant differences in postoperative refraction and corneal haze in the three age groups evaluated (<30 years, 30 to 39 years, ≥40 years) at 3, 6 and 12 months postoperatively.
Loewenstein and associates16 reported the results of PRK performed in 72 patients. For the analysis, they divided the patients in two age groups: one group included 39 patients aged from 18 to 26 years, and the other group included 33 patients aged from 35 to 54 years. Unlike the study of Hefetz,15 Loewenstein et al.16 found a trend toward overcorrection in the group of older patients, especially in cases of moderate to high myopia.
Rao and associates7 evaluated the influence of age on the visual results of PRK in a group of 197 eyes. For this purpose, patients were divided into four age groups: <30 years; 31 to 40 years; 41 to 50 years; >50 years. As reported by Loewenstein et al.,16 Rao and colleagues7 also found a tendency to overcorrection in the group of oldest patients. Moreover, the predictability of PRK tended to decrease with age.
Therefore, and to the best of our knowledge, the current study is the largest study of a myopic population specifically designed to evaluate the influence of age on the refractive outcomes after LASEK, using in all cases intraoperative MMC, and applying an age-based nomogram in order to improve the predictability of the procedure. We are conscious that one limitation of the current study is that it was retrospective and not controlled. Thus, a better study design would have been a prospective study randomizing all cases in two refractive-matched groups, one applying the age-based nomogram and the other without applying it. However, we want to remark that the main purpose of our study was to evaluate, in a high sample of eyes, the predictability of LASEK with mitomycin C in different age groups when the same age-based nomogram (provided and recommended by the excimer laser manufacturer) was applied in all cases. For this reason, we do believe that the design of the study (nonrandomized but including a large sample size) is adequate for the purpose of the current study. Another limitation of our study is the different number of participants in the two comparison groups (1163 versus 211 eyes). Two reasons would explain the lower number of eyes included in the older age group: first, in presbyopic patients, when conventional monovision was planned, only the dominant eye (targeted for emmetropia) was included in the study; second, several patients with myopia and presbyopia were better candidates for a refractive lens extraction than for a corneal refractive procedure. Nevertheless, the relatively high number of patients in both groups guarantees that the current study has enough statistical power to detect differences between groups. On the other hand, we are conscious that several surgeons worldwide perform PRK instead of LASEK, but given the fact that it is well accepted that both procedures provide similar visual and refractive results,24 we believe that our results can be useful for those surgeons that perform PRK.
It is well known that one factor that undermines the predictability and stability of a refractive surgical procedure is the corneal wound-healing properties. Younger patients tend to have a more aggressive healing response, which may contribute to some regression of the treatment effect.7 For this reason, nomogram adjustments have been suggested based on age14 to increase the amount of correction in younger patients. In contrast, older patients may have to be intentionally undercorrected7,8,14 to account for the diminished wound-healing response. Nevertheless, when an age-based nomogram was applied in the current study, we found that LASEK+MMC continued to be more predictable in young patients, and a trend to undercorrection of the myopia was found with increasing age (although the correlation was very weak, r2=0.02). For this reason, and based on our results, an overcorrection from the intended spherical correction seems to be adequate in young patients, in which this residual refractive overcorrection might not affect the efficacy index and the postoperative UDVA as a result of their preserved accommodative response. Moreover, a slight overcorrection might be desirable in very young patients in order to compensate a possible late myopic regression. In contrast, given the slight undercorrection found with increasing age, it might be reasonable to reduce the percentage of undercorrection (or even to not apply any undercorrection) when LASEK+MMC is performed in patients over 40 years. Therefore, it would be helpful to analyze our results in different age subgroups (patients <25 years, 25 to 40 years, 41 to 50 years, 51 to 65 years, >65 years) and to compare them with a control group (i.e., an age, sex and refraction matched group without applying an age-based nomogram) in order to improve the predictability of myopic LASEK.
On the other hand, it is well accepted that the intraoperative use of MMC tends to reduce the corneal wound-healing after laser ablation, causing a tendency to overcorrection that needs to be compensated for with an appropriate adjustment of the laser nomogram. Therefore, some authors have proposed to perform an undercorrection of 10%21 to 20%22 of the preoperative spherical refraction when MMC is used. Usually the cylinder programmed ablation does not need to be modified. Moreover, if we consider that older patients might have a diminished wound-healing behavior, the use of MMC would suppose an additional reduction in the corneal wound-healing response. However, only Lacayo and associates20 mentioned in their review that they applied an undercorrection of 8–15% in the sphere component depending on patient age and preoperative spherical defect, when they used MMC. Unfortunately, the authors did not indicate neither the percentage of undercorrection applied in each age group nor the final refractive outcomes. In the current study, because of the use of MMC, the programmed ablation was 10% less than the intended correction in all cases irrespective of patient age, and based on the high predictability achieved, we believe that this percentage of undercorrection seems to be adequate.
In conclusion, according to our results, a tendency toward undercorrection and less efficacy and predictability was found with aging after myopic LASEK with the intraoperative use of MMC. Further comparative studies are needed to better clarify the nomogram that might be applied in patients over 40 years in order to improve the predictability of LASEK in this older population.
Conflicts of interestThe authors have no conflicts of interest to declare.