To assess differences in corneal higher-order aberrations (i.e., HOAs) between six different types of irregular corneas (i.e, keratoconus (KC), keratoglobus (KG), pellucid marginal degeneration (PMD), laser-assisted in situ keratomileusis (LASIK), penetrating keratoplasty (PK), and intrastromal corneal ring segments (ICRS)).
MethodsCorneal aberration data from the 3rd and 4th order together with secondary vertical and horizontal coma, and secondary spherical aberration were retrospectively retrieved from a corneal tomographer and compared between irregular cornea types and for 3-, 5-, and 7-mm pupil diameters.
ResultsSignificant differences were observed in vertical coma, oblique trefoil, secondary oblique astigmatism, primary spherical, and secondary spherical between irregular cornea types across all three pupil sizes (all p≤0.025). Vertical coma consistently exhibited the greatest magnitude of HOA across all irregular cornea types and pupil diameters. For the larger pupil diameters (5 and 7 mm), the 3rd order aberrations (mainly coma-like), the 4th order aberrations (mainly spherical-like), and total HOA RMS were significantly lower in the LASIK group compared to all other irregular cornea types (all p≤0.003). Additionally, at pupil sizes of 5 and 7 mm, the 3rd, 4th, coma-like, spherical-like, and total HOA RMS were significantly lower in KC compared to the ICRS and PK groups (all p≤0.01). Furthermore, the 4th, spherical-like, and total HOA RMS were significantly lower in KC compared to KG at pupil diameters of 3 and 7 mm, 5 and 7 mm, and 7 mm, respectively (all p≤0.03).
ConclusionsVertical coma was the most elevated HOA across all irregular cornea types and pupil diameters. Corneal aberrations were lower in LASIK and KC, and higher in KG and PK.
Irregular corneas are typically characterized by changes in the shape of the cornea, which can cause a significant increase in corneal higher-order aberrations (i.e., HOAs).1–5 In some cases, corneal irregularity occurs as a result of corneal ectasia, such as keratoconus (KC), keratoglobus (KG) or pellucid marginal degeneration (PMD), whereas other types of corneal irregularity might occur secondary to surgical intervention, such as in Laser In-situ Keratomileusis (LASIK), penetrating keratoplasty (PK) or intrastromal corneal ring segments (ICRS). Different types of irregular cornea may not only differ in corneal shape, but also in corneal thickness patterns. Of all corneal ectasias, KC is the most prevalent type of irregular cornea; it is characterized by a bilateral and asymmetric ocular disease that causes progressive thinning and curving of the cornea.1 Corneal thinning typically occurs in the central or paracentral cornea, often in the inferior-temporal corneal quadrant,6 leading to a topographic pattern featuring high central corneal power together with an inferior cornea that is steeper than the superior cornea. KG is a bilateral ectasic disorder characterized by globular protrusion of the cornea associated with diffuse thinning from limbus to limbus, which is commonly maximal at the corneal periphery.7 PMD is a bilateral, peripheral corneal thinning disease characterized by a peripheral crescentic band of thinning, usually in the inferior cornea.2 The ectasic zone, which is normally 1-2 mm from the limbus, lies above the point of the maximum corneal thinning. PMD typically differs from KC in that the corneal protrusion occurs inferiorly, above a narrow band of clear, nonvascularized thinned corneal stroma concentric to the limbus, thus featuring a relatively normal central topographic pattern.2 Although the above three types of corneal ectasia are categorized as corneal thinning disorders, they differ in the location of maximal corneal protrusion, leading to differences in both corneal irregularity and thinning profiles. These differences in corneal thickness and shape are likely to result in different HOA patterns between these corneal ectasia types, potentially leading to distinctively different deteriorations in vision quality. Furthermore, since these three conditions differ in the location of maximal corneal protrusion, HOAs are also likely to change depending on the pupil size at which they are assessed.
Irregular corneas can also occur secondary to ocular surgery, including LASIK, PK and ICRS. LASIK is the most commonly performed laser refractive surgery to correct refractive errors.8–10 This technique initially involves the creation of a partial-thickness corneal flap that is subsequently repositioned in its original position after performing laser ablation of the underlying stromal surface. This induces significant changes in corneal thickness, shape, biomechanics and HOA.8–10 PK, which consists in the removal of the entire thickness of the cornea and replacement with donor tissue, is one of the most commonly used surgical techniques to restore corneal blindness, such as in advanced cases of corneal ectasia, degeneration, dystrophy, opacities and keratitis, although the surgical procedure usually induces irregularity of the front corneal surface.11 ICRS implantation is a surgical procedure, which aims at reducing corneal elevation and irregular astigmatism, by reshaping the cornea in cases of KC, ectasias post-LASIK, ectasias after keratotomy, astigmatism and myopia, with the ultimate goal of improving visual acuity as well as delaying or eliminating the need for lamellar or penetrative PK.12–14 Although the latter technique aims at improving corneal topographic symmetry and reducing HOAs through corneal surface regularization, ICRS implantation normally causes central flattening and peripheral steepening adjacent to the ring insertion site in the cornea, which can also lead to an increase in HOAs, particularly noticeable at larger pupil diameters.15 As with different types of corneal ectasia, these corneal surgery techniques can also lead to different post-surgical corneal shapes and thinning profiles.
Although the HOAs typically found in patients with the above irregular cornea types has been previously reported, to the authors knowledge no previous studies have assessed differences in HOAs between these six different irregular cornea types. As it is well established that irregular corneas differ significantly from normal regular corneas, this study does not aim at assessing differences between normal and irregular corneas; instead, the objective of this study is to evaluate differences in HOAs between six different types of irregular corneas (i.e, KC, KG, PMD, LASIK, PK, and ICRS). Differences in HOAs were assessed for three pupil sizes (i.e., 3, 5 and 7 mm) to evaluate how HOAs might change between different irregular cornea types given the differences in the location of corneal protrusion among the three different types of corneal ectasia as well as the differences in corneal shape induced by the three different surgical procedures. Additionally, as the location of corneal protrusion in corneal ectasias could affect corneal thinning and the different ocular surgery procedures can also affect corneal thickness profiles, differences in the location of the thinnest corneal point between different irregular cornea types were also evaluated.
MethodsA retrospective, descriptive, analytical and transversal study was designed to assess differences in HOAs for different pupil sizes as well as in terms of the location of the thinnest corneal point among six different irregular cornea types (i.e, KC, KG, PMD, LASIK, PK, and ICRS).
Anonymised corneal wavefront aberration and pachymetry data from patients with the above irregular corneas types were retrospectively retrieved from a corneal tomographer (Oculus® Pentacam, Optikgeräte GmbH, Wetzlar, Germany). Given that the objective of the study is to systematically describe and quantify variations in corneal wavefront aberrations across a spectrum of pathological conditions and different pupil diameters, the inclusion of a control group was not deemed necessary. Subsequently, patients’ clinical records were reviewed to confirm they were all diagnosed with corneal ectasia or that they underwent corneal surgery. Data was collected from the Novovision Ophthalmology Clinic and the Optometry Clinic at the Faculty of Optics and Optometry of the Complutense University of Madrid (both in Madrid, Spain). Diagnoses of KC, KG and PMD were performed by an ophthalmologist. Patients with corneal opacities were excluded from the study to ensure that only HOAa affecting the corneal surface were analyzed. As the instrument used (Oculus® Pentacam) does not require consideration of the state of the tear film, this factor was not accounted for during measurements. Multiple corneal wavefront measurements were taken for each patient to ensure accuracy and reliability, and the best-quality measurement was selected for analysis based on the instrument's quality criteria.
The criteria followed in the clinic for the diagnosis of the different primary corneal ectasias in this study is multifaceted. For KC, evaluation includes assessing the area of minimum pachymetry, its distribution, and the pachymetry progression profile, with a normal progression index usually below 1.20. The assessment of posterior elevation near the area of minimum pachymetry was also accounted for with less than +18 microns being considered normal; +18 to +20 microns suspicious; and more than +20 microns pathological. PMD is diagnosed using biomicroscopic findings and corneal topography, where the curvature map shows flattening and pronounced astigmatism in the vertical meridian resembling a croissant or crab claw. The pachymetric map displays bell-shaped inferior thinning with a prominent protrusion in the anterior elevation. The progression curve typically deviates from the norm, showing an increasing slope before 6 mm and possibly an "inverted curve" in advanced stages. KG features a generalized corneal protrusion with a normal width but significantly thinned stroma, about 1/3 to 1/5 of its thickness, and keratometry readings above 47.00 D. Biomicroscopy may reveal ruptures in Bowman's membrane, with corneal topography providing diagnostic support if the minimum normalized scale value is 44.50 D or higher 7,16–18 For the LASIK group, this study included patients without any ocular pathology in whom the goal was to reduce low-order refractive errors, and all underwent conventional ablation and not wavefront-guided ablation. For the PK group, this study included patients with advanced primary or iatrogenic ectasias who had a medical indication for corneal transplant. For the ICRS group, this study included patients with keratoconus at various stages who did not want or could not adapt to contact lens wear. The study was approved by the Institutional Ethical Committee Review Board of the latter two institutions.
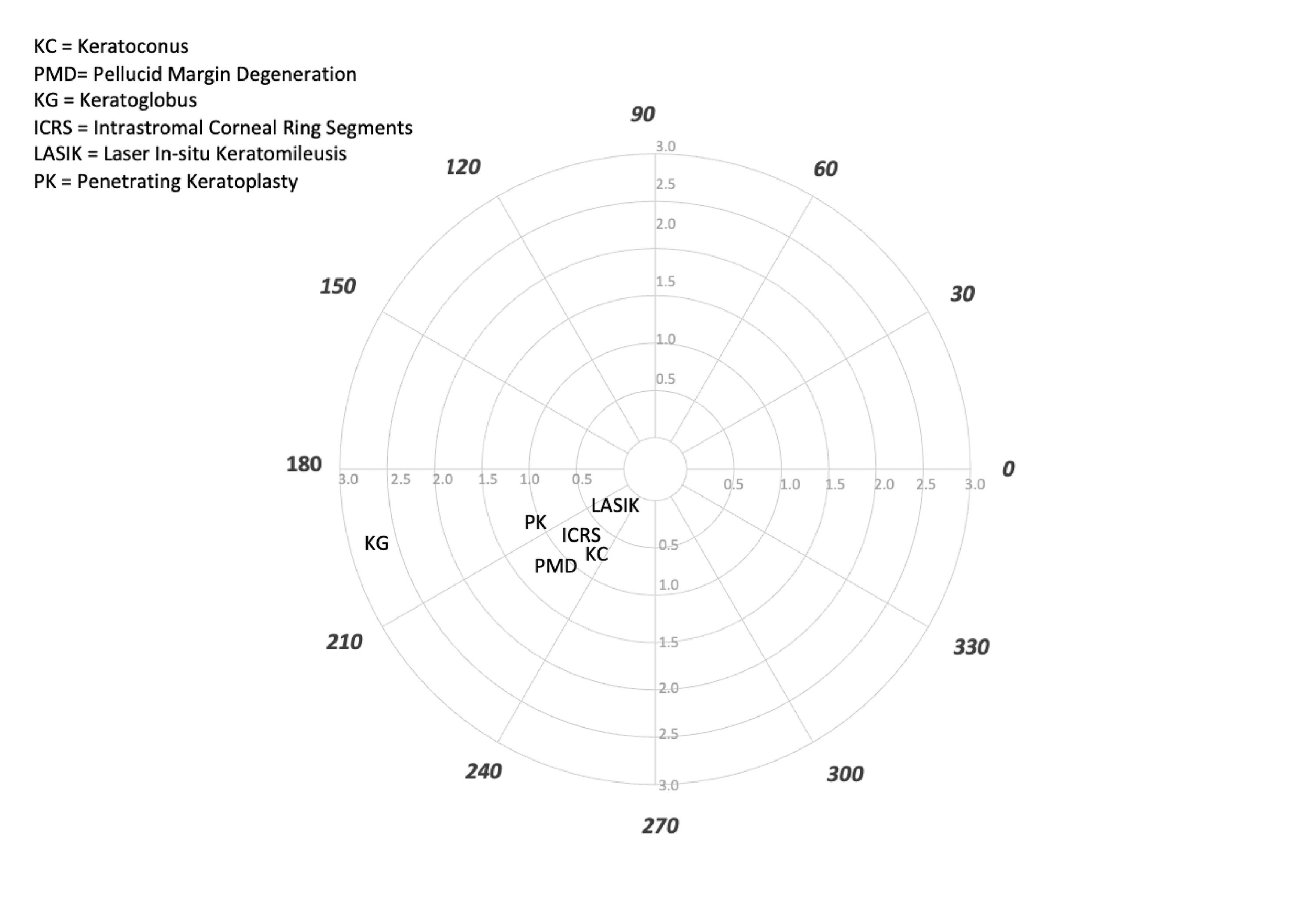
Anterior corneal wavefront aberration data for pupil diameters of 3, 5, and 7 mm were obtained. More specifically, data from the following Zernike coefficients were extracted: 3rd order (vertical trefoil: (Z 3,-3); vertical coma: (Z 3,-1); horizontal coma: (Z 3,1); and oblique trefoil: (Z 3,3)); 4th order (oblique tetrafoil: (Z 4,-4); secondary oblique astigmatism: (Z 4,-2); primary spherical: (Z 4,0); secondary vertical astigmatism: (Z 4,2); and vertical tetrafoil: (Z 4,4)); 5th order (secondary vertical coma: (Z 5,-1); and secondary horizontal coma: (Z 5,1)); and 6th order (secondary spherical: (Z 6,0)). Additionally, the total root mean square (RMS) of the 3rd and 4th orders, coma-like (i.e., (Z 3,1); (Z 3-1); (Z 5,1); and (Z 5,-1)), spherical-like (i.e., (Z 4,0) and (Z 6,0)) and the total HOAs RMS for pupil diameters of 3, 5, and 7 mm were also calculated. Differences in the location of the thinnest point of the cornea between the different types of irregular cornea were also analyzed; these are given by the corneal tomographer in terms of x and y coordinates, which were transformed into vectors and angles to describe the distance and orientation of these locations with regards to the instrument's measurement axis (i.e., the point where the topography map shows the (0,0) coordinate). Superior and inferior, and nasal and temporal corneal locations in right eyes were given positive and negative values, respectively, in relation to the instrument's measurement axis. Data from left eyes have been horizontally inverted so that all data are represented as if for the right eye.
Statistical analysisThe normality distribution of the data was assessed using the Kolmogorov-Smirnov test, resulting in non-parametric data. The Mann-Whitney U and/or Kruskal Wallis tests were used. The Friedman test was used to compare individual HOAs and the RMS within each condition. Differences between groups in gender were assessed using a chi-square test. Parametric and non-parametric data are described as the mean ± standard deviation and median and interquartile range [Q1-Q3], respectively. Statistical analyses were performed using SPSS 27.0 software (SPSS Inc., Chicago, Illinois). The level of statistical significance was taken as 5%.
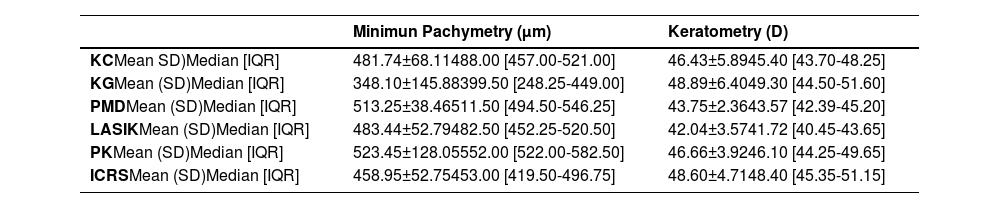
ResultsSubjects’ demographicsA total of 720 eyes with irregular corneas were analyzed (KC =455; KG =10; PMD=16; LASIK=108; PK =33; and ICRS=98). Participants’ mean age was 41.2±13.1 years and the majority were males (67.3%). Significant differences in mean age were found between irregular cornea types (KC: 39.3±12.2 years; KG: 43.8±18.3 years; PMD: 45.2±6.4 years; LASIK: 49.6±5.5 years; PK: 47.3±14.6 years; and ICRS: 41.2±14.8 years) (p=0.026). No significant differences in gender were found between irregular cornea types (p>0.05). Table 1 shows the pachymetry and keratometry values for each of the corneal conditions.
Pachymetry and keratometry values for the 6 types of irregular cornea
μm, micron; D, diopters; SD, standard deviation; IQR, interquartile range [Q1-Q3]; KC, keratoconus; KG, keratoglobus; PMD, pellucid marginal degeneration; LASIK, laser in-situ keratomileusis; PK, penetrating keratoplasty; ICRS, intrastromal ring segments.
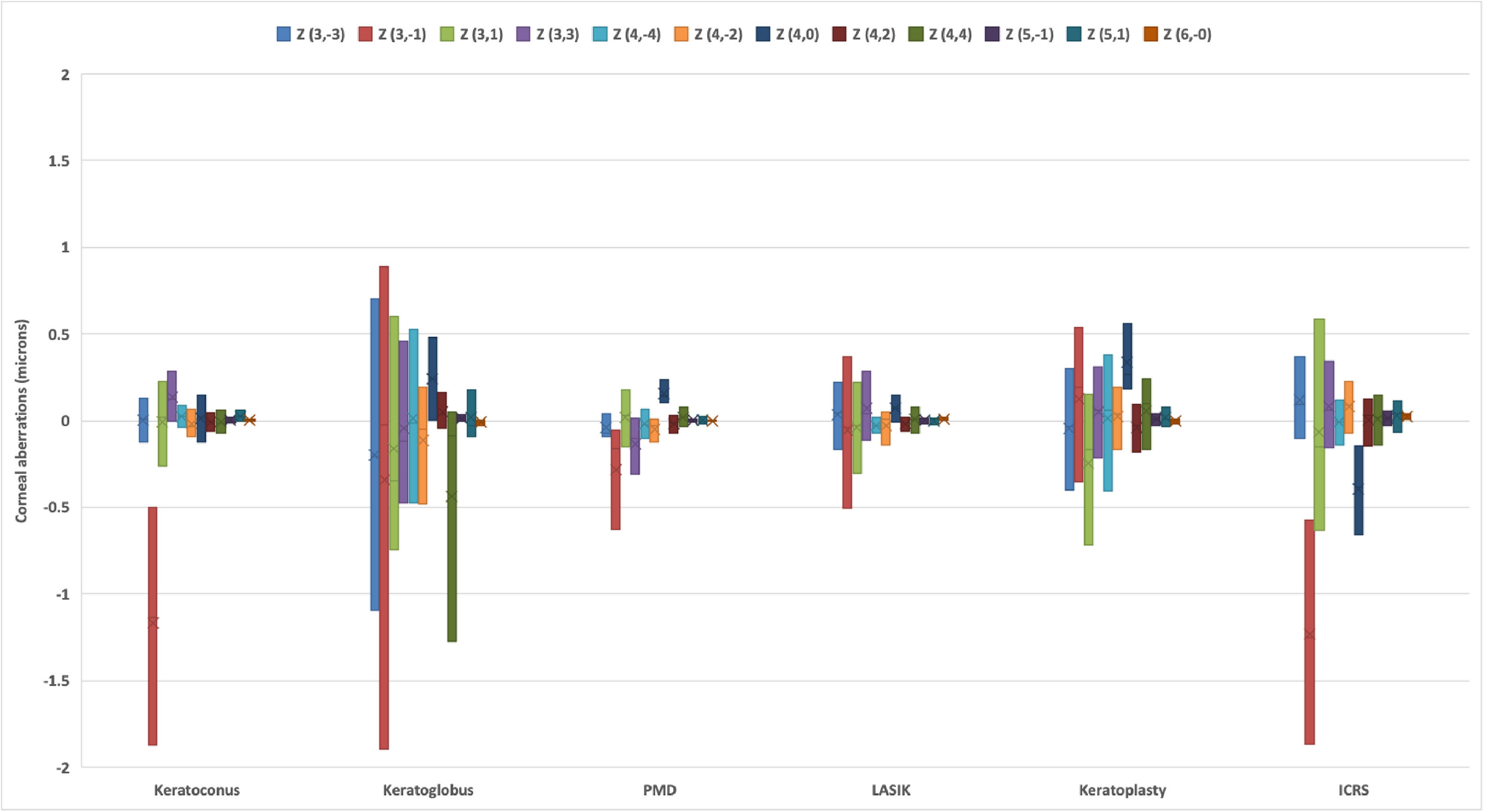
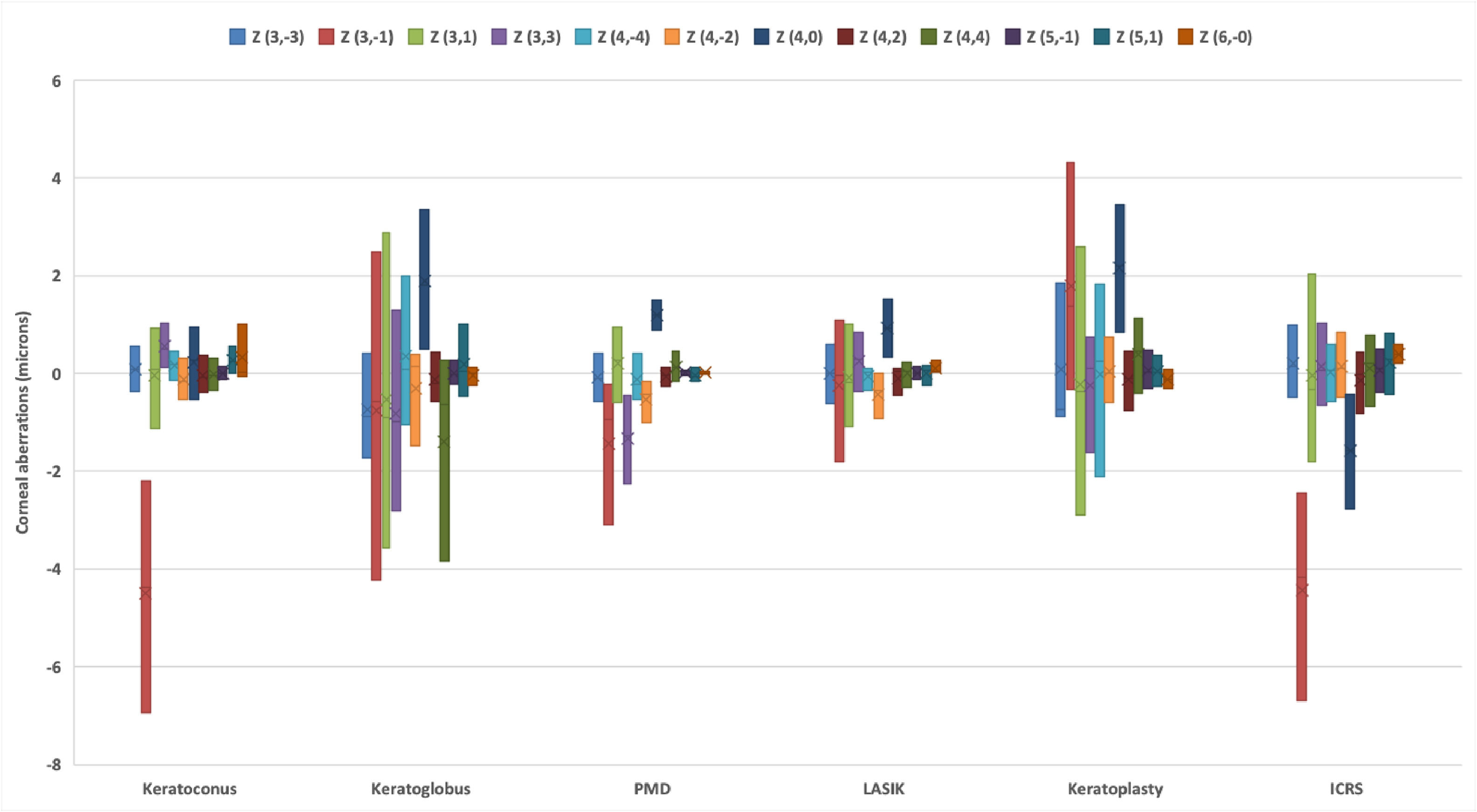
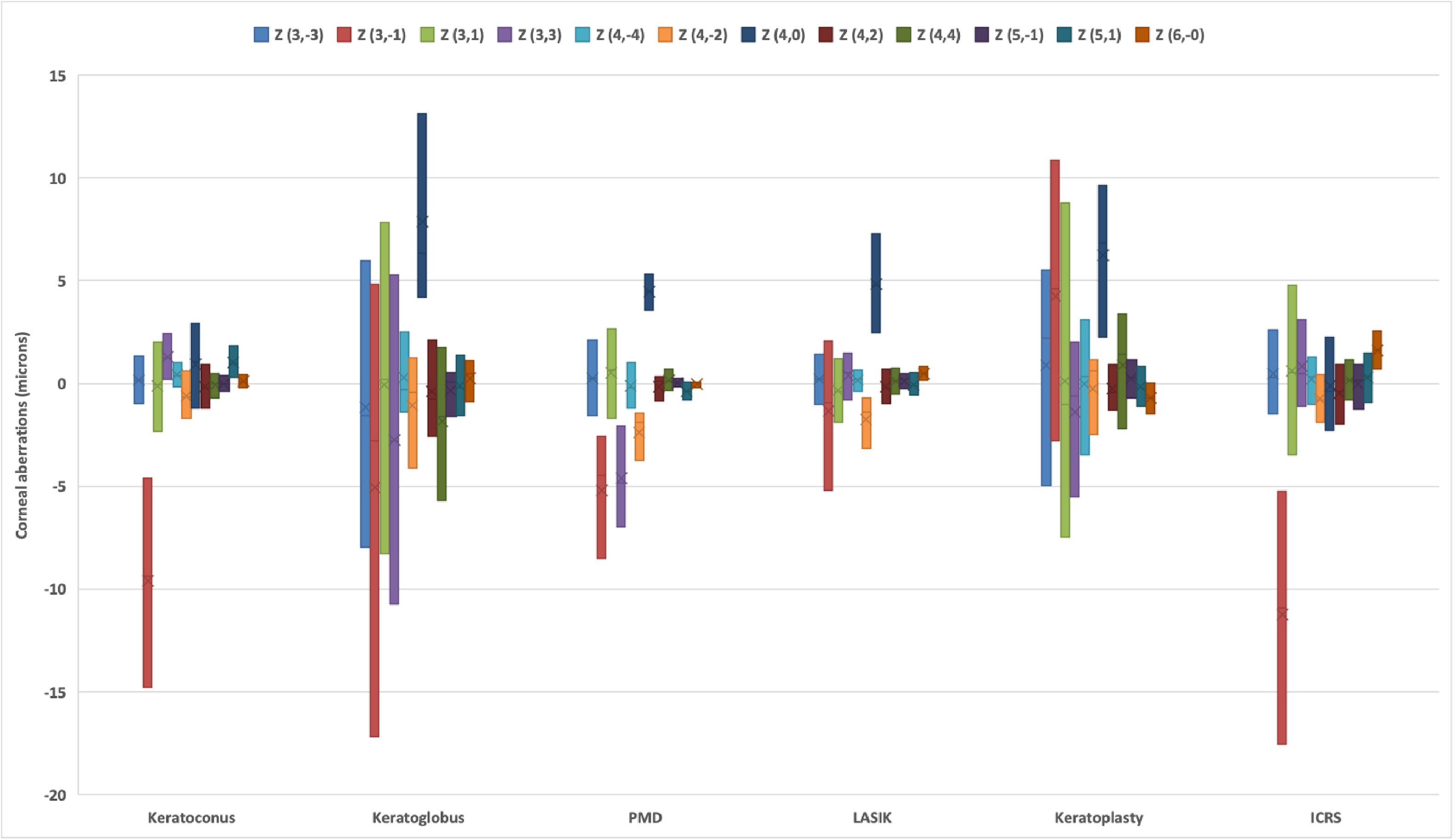
Overall, for all six types of irregular corneas, (Z 3,-1), (Z 3,1), (Z 4,0), (Z 4,2) and (Z 6,0) changed significantly with increasing pupil size (all p<0.05) (Figs. 1 to 3). In KC, as pupil size changes so do so (Z 3,-1), (Z 4,2), (Z 5,-1), and (Z 6,0) (all p<0.05), with (Z 3,-1) and (Z 6,0) increasing in magnitude, although the former became more negative whereas the latter more positive. Vertical coma became more negative, increasing in magnitude, with increasing pupil diameter (p<0.001). In KG, (Z 4,0) increased with increasing pupil size from 3mm to 7mm (p=0.004). In PMD, (Z 3,-3), (Z 4,0) and (Z 4,2) increased along with pupil size (all p≤0.008). In LASIK, as pupil size increases so do so in magnitude (Z 3,-1)) and (Z 4,0) (both p≤0.01), although (Z 3,-1) became more negative, whereas (Z 4,0) became more positive. In PK, (Z 4,0) and (Z 6,0) increased in magnitude along with pupil size (all p≤0.005), although the former became more positive whereas the latter more negative. In ICRS, (Z 3,-1), (Z 4,0) and (Z 6,0) increased in magnitude with increasing pupil size, although the former two in the negative direction, whereas the latter one in the positive direction (all p<0.05). In contrast, (Z 4,2) changed from positive to negative with increasing pupil diameter (p=0.003).
Corneal aberrations for a 3-mm pupil diameter in each irregular cornea type. The upper and lower part of each of the vertical bars represent the upper and lower quartiles, respectively. The cross (X) and horizontal line (—) within each of the bars represent the mean and median, respectively. PMD, pellucid marginal degeneration; LASIK, laser-assisted in situ keratomileusis; ICRS, intracorneal ring segments.
Similarly, significant differences were found in the 3rd, 4th , coma-like and spherical-like RMS orders for the different pupil diameters (all p<0.001). However, no significant differences were found in some RMS orders for certain pairs of pupil diameters. In KC, no significant differences were found in 3rd and coma-like order RMS between the 3- and 5-mm pupil diameters (p>0.05). Likewise, in KG, no significant differences were found in 3rd and coma-like RMS neither between 3- and 5-mm nor between 5- and 7-mm pupil sizes (all p>0.05). In PMD, no significant differences were found in 3rd, 4th, coma-like and spherical-like RMS neither between 3- and 5-mm nor in 3rd and 4th RMS between 5- and 7-mm pupil diameters (all p>0.05). In LASIK, no significant differences were found in any of the orders assessed between 3- and 5- mm pupil diameters nor between 3- and 7-mm pupil diameters in the 3rd and 4th RMS (all p>0.05). In PK and ICRS, no significant differences were found in coma-like and spherical-like RMS orders between 3 and 5 mm pupil diameters (all p>0.05).
Differences in HOAs between different types of irregular corneaSignificant differences in HOAs were found between irregular cornea types for each of the three pupil diameters (Figs. 1, 2 and 3).
Corneal aberrations for a 5-mm pupil diameter in each irregular cornea type. The upper and lower part of each of the vertical bars represent the upper and lower quartiles, respectively. The cross (X) and horizontal line (—) within each of the bars represent the mean and median, respectively. PMD, pellucid marginal degeneration; LASIK, laser-assisted in situ keratomileusis; ICRS, intracorneal ring segments.
Corneal aberrations for a 7-mm pupil diameter in each irregular cornea type. The upper and lower part of each of the vertical bars represent the upper and lower quartiles, respectively. The cross (X) and horizontal line (—) within each of the bars represent the mean and median, respectively. PMD, pellucid marginal degeneration; LASIK, laser-assisted in situ keratomileusis; ICRS, intracorneal ring segments.
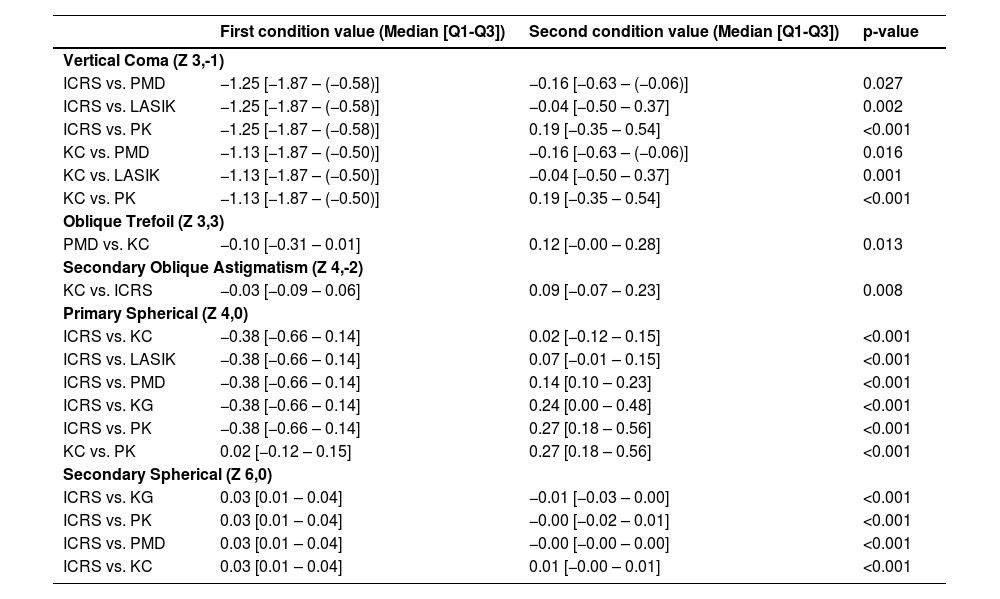
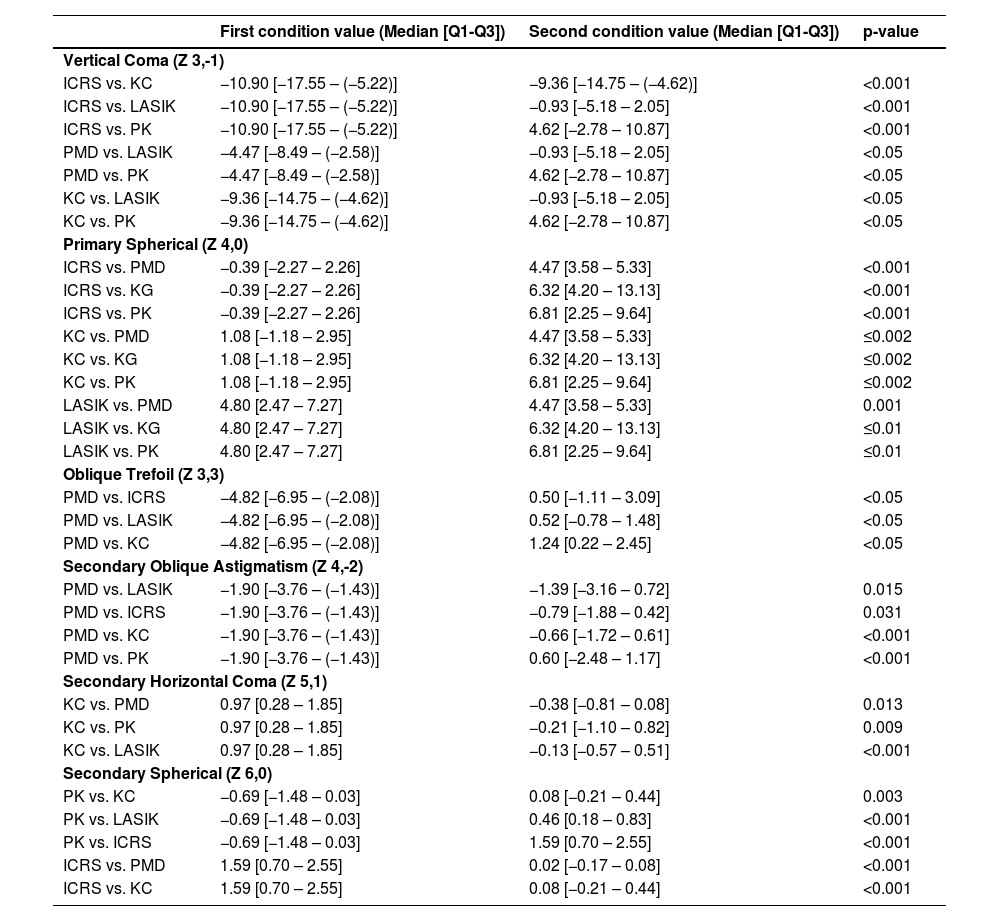
For a 3-mm pupil diameter, significant differences were found in (Z 3,-1), (Z 3,3), (Z 4,-2), (Z 4,0), and (Z 6,0) (all p≤0.01). Table 2 shows the comparison between the different conditions.
Changes in HOAs for a 3-mm pupil diameter.
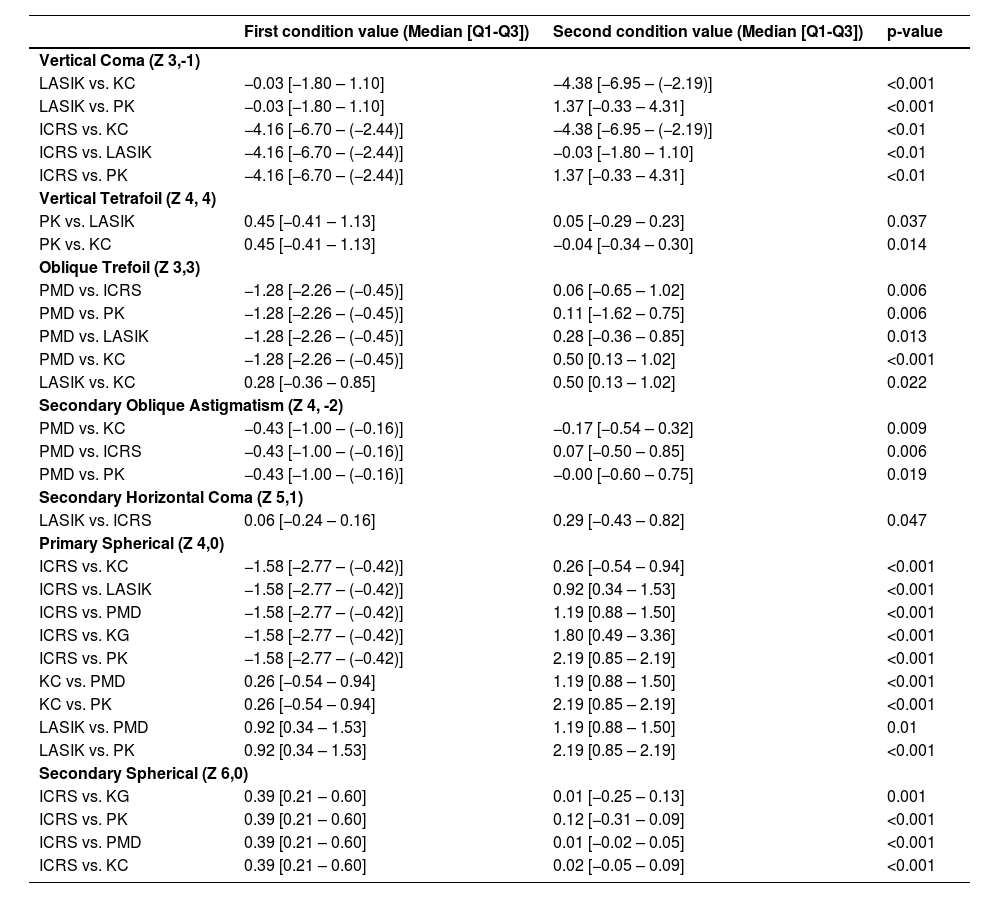
For a 5-mm pupil diameter, significant differences were found in (Z 3,-1), (Z 3,3), (Z 4,-2), (Z 4,0), (Z 4,4), (Z 5,1), and (Z 6,0) (all p≤0.025). Table 3 shows the comparison between the different conditions.
Changes in HOAs for a 5-mm pupil diameter.
For a 7-mm pupil diameter, significant differences were found in (Z 3,-1), (Z 3,3), (Z 4,-2), (Z 4,0), (Z 5,1), and (Z 6,0) (all p<0.001). Table 4 shows the comparison between the different conditions.
Changes in HOAs for a 7-mm pupil diameter.
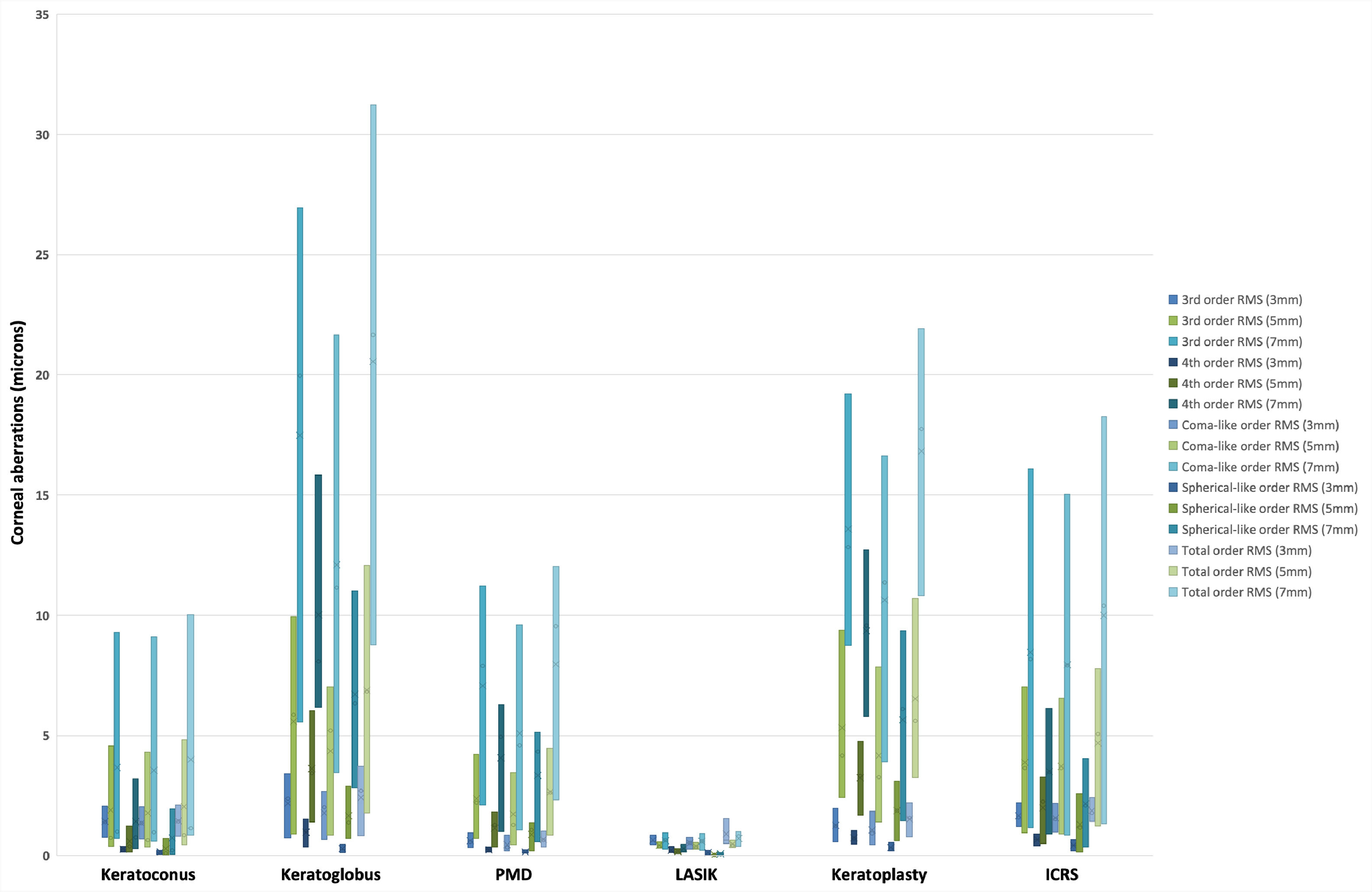
Significant differences were also found in the 3rd, 4th, coma-like and spherical-like and total HOA RMS between the different types of irregular cornea (Fig. 4).
Root mean square (RMS) corneal aberrations for the different irregular cornea types and pupil diameters. The cross (X) and horizontal line (—) within each of the bars represent the mean and median, respectively. PMD, pellucid marginal degeneration; LASIK, laser-assisted in situ keratomileusis; ICRS, intracorneal ring segments.
For a 3-mm pupil diameter, the 3rd order RMS was significantly lower in PMD (0.58 [0.33 – 0.95]) in comparison with KC (1.40 [0.77 – 2.07], p=0.009), ICRS (1.58 [1.20 – 2.21], p<0.001) and KG (2.37 [0.74 – 3.42], p=0.007), as well as lower in LASIK (0.60 [0.45 – 0.86]) in comparison with ICRS (p=0.001) and KG (p=0.034). For a 5-mm pupil diameter, it was significantly lower in LASIK (0.39 [0.30 – 0.58]) in comparison with all other irregular cornea types (KC (0.74 [0.39 – 4.56]); PMD (2.20 [0.72 – 4.21]); ICRS (3.65 [0.95 – 7.03]); PK (4.17 [2.41 – 9.39]); and KG (5.85 [0.92 – 9.94]) (all p<0.001)). It was also lower in KC in comparison with ICRS and PK (both p<0.001). For a 7-mm pupil diameter, it was significantly lower in LASIK (0.65 [0.27 – 0.94]) in comparison with the other irregular cornea types (KC (1.00 [0.71 – 9.29]); PMD (7.89 [2.11 – 11.22]); ICRS (8.17 [1.17 – 16.08]), PK (12.84 [8.74 – 19.21]); and KG (19.97 [5.55 – 26.94]) (all p<0.001)). It was also significantly lower in KC in comparison with ICRS and PK (both p<0.001).
Fourth-order RMSFor a 3-mm pupil diameter, the 4th order RMS was significantly lower in PMD (0.27 [0.14 – 0.36]) in comparison with ICRS (0.66 [0.41 – 0.91], p<0.001), PK (0.71 [0.47 – 1.04], p<0.001) and KG (1.02 [0.36– 1.52], p=0.016). It was also lower in LASIK (0.18 [0.13 – 0.38]) in comparison with ICRS, PK and KG (all p≤0.017). Likewise, it was lower in KC (0.24 [0.15 – 0.39]) in comparison with ICRS, PK and KG (all p≤0.003). For a 5-mm pupil diameter, it was significantly lower in LASIK (0.15 [0.08 – 0.29]) in comparison with KC (0.39 [0.16 – 1.25]), PMD (1.28 [0.35 – 1.82], p=0.001), ICRS (2.24 [0.51 – 3.25]), PK (3.32 [1.67 – 4.75]) and KG (3.44 [1.40 – 6.02]) (all p<0.001). For a 7-mm pupil diameter, it was significantly lower in LASIK (0.25 [0.14 – 0.47]) in comparison with all other irregular cornea types (KC (0.77 [0.28 – 3.20]); ICRS (3.48 [0.90 – 6.13]); PMD (4.94 [0.99 – 6.30]); KG (8.09 [6.16 – 15.82]); and PK (9.56 [5.79 – 12.71]) (all p<0.001)). It was also lower in KC in comparison with ICRS, PMD and KG (all p<0.001).
Coma-like RMSFor a 3-mm pupil diameter, the coma-like RMS was significantly lower in PMD (0.35 [0.20 – 0.85]) in comparison with KC (1.35 [0.70 – 2.03]), ICRS (1.51 [0.97 – 2.19]), and KG (2.00 [0.65 – 2.66] (all p≤0.010). It was also lower in LASIK (0.54 [0.27 – 0.76]) in comparison with KC, ICRS, and KG (all p≤0.025). For a 5-mm pupil diameter, it was significantly lower in LASIK (0.37 [0.26 – 0.54]) in comparison with KC (0.65 [0.35 – 4.31]), PMD (1.28 [0.45 – 3.44]), ICRS (3.65 [0.91 – 6.55]) and KG (5.21 [0.85 – 7.01]) (all p≤0.010). It was also lower in KC in comparison ICRS and PK (3.26 [1.41 – 7.85]) (both p<0.001). For a 7-mm pupil diameter, it was significantly lower in LASIK (0.59 [0.23 – 0.94]) in comparison with KC (0.97 [0.59 – 9.01]), PMD (4.58 [1.07 – 9.60]), ICRS (7.92 [0.84 – 15.03]), KG (11.16 [3.45 – 21.65]), and PK (11.36 [3.90 – 16.63]) (all p≤0.001). It was also lower in KC in comparison ICRS and PK (both p<0.001).
Spherical-like RMSFor a 3-mm pupil diameter, the spherical-like RMS was significantly lower in LASIK (0.11 [0.03 – 0.22]) in comparison with PK (0.29 [0.19 – 0.56]) and ICRS (0.42 [0.20 – 0.66]) (both p≤0.008). It was also lower in KC (0.14 [0.06 – 0.22]) in comparison with PK and ICRS (both p<0.001). It was lower in PMD (0.14 [0.10 – 0.23]) in comparison with ICRS (p=0.019). For a 5-mm pupil diameter, it was significantly lower in LASIK (0.03 [0.01 – 0.06]) in comparison with KC (0.11 [0.03 – 0.71]), PMD (1.08 [0.19 – 1.35]), ICRS (1.17 [0.15 – 2.58]), KG (1.38 [0.72 – 2.90]) and PK (1.86 [0.62 – 3.10]) (all p<0.001). It was also lower in KC in comparison with ICRS, KG and PK (all p≤0.028). For a 7-mm pupil diameter, it was significantly lower in LASIK (0.06 [0.03 – 0.11]) in comparison with KC (0.22 [0.06 – 1.94]), ICRS (2.09 [0.35 – 4.04]), PMD (4.34 [0.58 – 5.12]), PK (6.11 [1.45 – 9.37]), and KG (6.34 [2.81 – 11.02]) (all p<0.001). It was also lower in KC in comparison ICRS, PMD, PK, and KG (all p≤0.019).
Total HOAs RMSFor a 3-mm pupil diameter, the total RMS was significantly lower in PMD (0.64 [0.37 – 1.02]) in comparison with KC (1.42 [0.81 – 2.11]), PK (1.55 [0.80 – 2.19]), ICRS (1.77 [1.42 – 2.41]) and KG (2.69 [0.84 – 3.71]) (all p≤0.014). It was lower in LASIK (0.64 [0.50 – 1.55]) in comparison with ICRS and KG; and lower in KC in comparison with ICRS (all p≤0.035). For a 5-mm pupil diameter, it was significantly lower in LASIK (0.44 [0.34 – 0.63]) in comparison with all other irregular cornea types (KC (0.86 [0.45 – 4.82]); PMD (2.62 [0.85 – 4.48]); ICRS (5.06 [1.22 – 7.76]); PK (5.61 [3.23 – 10.69]); and KG (6.83 [1.77 – 12.07]) (all p≤0.003). Similarly, it was also lower in KC in comparison with ICRS, PK, and KG (all p≤0.035). For a 7-mm pupil diameter, it was significantly lower in LASIK (0.80 [0.38 – 0.99]) in comparison with all other irregular cornea types (KC (1.15 [0.85 – 10.03]); PMD (9.56 [2.32– 12.03]); ICRS (10.38 [1.33 – 18.25]); PK (17.75 [10.82 – 21.92]); and KG (21.67 [8.78 – 31.22]) (all p<0.001)). It was also lower in KC in comparison with ICRS, PK and KG (all p≤0.027).
Location of the thinnest corneal pointSignificant differences were found in the position of the thinnest corneal point between the different types of irregular corneas (p<0.001), with this point being significantly closer to the geometric centre of the cornea in LASIK (r: 0.49 [0.42]) compared with KC (r: 0.84 [0.45], p<0.001), PMD (1.24 [1.06], p<0.001), PK (1.19 [2.09], p<0.001), ICRS (0.74 [0.43], p<0.001), and KG (2.62 [1.56], p<0.001) (Fig. 5). It was also significantly closer to the geometric center of the cornea in ICRS in comparison with KG (p<0.001).
DiscussionThis study assessed differences in corneal aberrations between different irregular cornea types and for different pupil diameters. That there were significant differences in the number of subjects found within each of the irregular cornea types in this retrospective, descriptive study is attributed to the prevalence of the different primary ectasias (i.e, KC, KG, and PMD) and the popularity of the different corneal surgery types assessed (i.e, LASIK, PK, and ICRS). It also reflects on the types of patients with irregular cornea typically coming to an ophthalmology clinic in downtown Madrid and to the Optometry Clinic at the Faculty of Optics and Optometry of the Complutense University of Madrid. Overall, for all six types of irregular corneas, (Z 3,-1), (Z 3,1), (Z 4,0), (Z 4,2) and (Z 6,0) changed significantly with increasing pupil size, particularly (Z 3,-1) and (Z 4,0) (Figs. 1 to 3). Vertical coma was the HOA of greatest magnitude across all irregular cornea types and pupil diameters. Significantly larger increases in (Z 3,-1), (Z 3,3) and (Z 4,-2) were found in PMD at the 7- vs 3-mm pupil diameters in comparison with the other irregular cornea types. Although HOAs usually increase in magnitude with increasing pupil size,19,20 this study was able to detect differences in the pattern of HOAs between different types of irregular corneas for different pupil diameters given the marked differences in corneal irregularity profiles among these conditions. Most notably, (Z 3,-1) was greater in magnitude in ICRS in comparison with LASIK and PK for all three pupil diameters, and it was also greater in magnitude in comparison with KC for the 5- and 7-mm pupil sizes. It was also lower in magnitude in LASIK in comparison with KC for all three pupil diameters. Oblique trefoil (Z 3,3) was significantly greater in magnitude in PMD in comparison with LASIK, ICRS and KC at the 5- and 7-mm pupil sizes. Secondary oblique astigmatism (Z 4,-2) was significantly greater in magnitude in PMD in comparison with KC, ICRS and PK for the 5- and 7-mm pupil sizes. Primary spherical (Z 4,0) was significantly more negative in ICRS in comparison with all other irregular corneal types for the 3- and 5-mm pupil diameters, and it was also significantly more negative in comparison with PK, PMD and KG for the 7-mm pupil size. Likewise, primary spherical (Z 4,0) was significantly lower in KC in comparison with PK for all three pupil diameters as well as lower in comparison with PMD for the 5- and 7-mm pupil diameters. Secondary spherical (Z 6,0) was greater in magnitude in ICRS in comparison with KC, KG, PMD and PK for the 3- and 5-mm pupil sizes. Significant differences were also found in the 3rd, 4th, coma-like, spherical-like and total RMS between the different irregular cornea types, with HOAs also typically increasing with increasing pupil diameter (Fig. 4). Across all three pupil diameters, 3rd, 4th, coma-like, spherical-like and total RMS were typically lower in LASIK and KC, and higher in KG and PK; these results largely agree with previous studies.2,3 Whist KC showed lower HOAs particularly in comparison with ICRS and PK, LASIK showed lower RMS aberrations in comparison with all other irregular corneas types, particularly at larger pupil sizes. The 3rd, 4th, coma-like and total RMS were significantly lower in PMD in comparison to most of the other irregular cornea types for the 3-mm pupil diameter, but not for the other two diameters.
Higher-order aberrations, including coma-like, spherical-like, and total HOA RMS are increased in patients with KC.21–23 That KC and PMD demonstrated a relatively similar corneal aberration profile largely agrees with a previous study that compared ocular aberrations between these two types of corneal ectasia.2 Of interest is to notice that the significantly larger HOAs found in PMD at the 7-mm pupil diameter in comparison to most of the other irregular cornea types is attributed to the corneal shape pattern typically observed in this condition, in which the location of maximal corneal thinning and steepening is normally seen near the limbus in the far inferior corneal periphery,24,25 but the central corneal surface is relatively symmetric thus bearing relatively low and high HOAs in the central and peripheral cornea, respectively.2 That KG was found to have higher HOAs compared with the other two types of corneal ectasia was expected as KG is characterized by global corneal protrusion with diffuse thinning from limbus to limbus,7 leading to greater levels of corneal irregularity and HOAs. Although there were some differences in individual HOAs between the irregular corneas secondary to ocular surgery (Figs. 1 to 3), LASIK showed a lower magnitude of HOAs in comparison with PK and ICRS at all pupil diameters (Fig. 4). Despite HOAs change significantly post- vs pre-LASIK intervention,10 LASIK is used for correcting refractive error in eyes with relatively normal corneas, with some LASIK procedures incorporating wavefront-guided and aspheric techniques to control for increases in aberrations,26 which might explain the overall lower magnitude of HOAs found with LASIK in comparison with the other irregular cornea types. Although ICRS is typically used for improving corneal topographic symmetry and reducing HOAs,4,15,27 a greater total HOAs RMS was found in ICRS in comparison with most of the other irregular cornea types (Fig. 4). A previous study reported a decrease in primary coma and coma-like aberrations, but an increase in primary spherical corneal aberrations post-operatively following ICRS implantation in eyes with early to moderate ectatic disease.28 Another study found that ICRS implantation in KC decreased coma and tilt, but increased trefoil, tetrafoil, secondary astigmatism and primary spherical ocular aberrations.15 The greater magnitude of corneal aberrations found in PK was somehow expected as this surgical technique is likely to result in increased corneal irregularity and, in turn, greater HOAs in comparison to the other cornea types.29
All six irregular corneal types had the thinnest point of the cornea located in the infero-temporal corneal quadrant, albeit within less than 1.5µm from the geometrical center of the cornea, with LASIK showing the thinnest point closer and KG farthest from the geometric center of the cornea (Fig. 5). These results agree with those of a previous study, which reported such point also to be located in the infero-temporal corneal quadrant in KC.6 That all types of irregular corneal types evaluated had the thinnest point of the cornea in the infero-temporal corneal quadrant might reflect on the normal thickness profile of the cornea, with such point being independently located in this part of the cornea regardless of whether cornea irregularity results from a ectasia or secondary to surgical intervention.30,31
A limitation of this study is that the number of eyes examined and the mean age of subjects varied among the six irregular cornea types. Another limitation includes that no the degree of severity of the three ectatic conditions assessed were available. As such, it was not possible to control whether similar number of eyes with similar mean ages and degrees of severity were included within each of the study groups. Likewise, neither pre-surgical ocular details nor the indications for receiving corneal surgery were available from eyes which received LASIK, PK and ICRS. Furthermore, pupil size was not directly measured in our sample. It would be interesting to demonstrate if alterations of aberrations at the largest pupil sizes (7 mm) may have a real impact on the visual quality of the patients assessed in this study. However, the objective of this study was to assess differences in HOAs between different types of irregular corneas and not to compare the outcomes of corneal surgery. Despite the abovementioned limitations, a major strength of this study is the relatively large number of eyes assessed with different types of irregular cornea and for three pupil diameters.
In conclusion, differences in HOAs and the location of the thinnest point of the cornea were found between different irregular cornea types. Overall, (Z 3,-1) was the HOA of greatest magnitude across all irregular cornea types and pupil diameters. Corneal aberrations were lower in LASIK and KC, and higher in KG and PK. The thinnest point of the cornea was located in the infero-temporal corneal quadrant across all irregular cornea types.