To evaluate and compare Comfilcon A and Senofilcon A silicone hydrogel contact lenses used as a therapeutic bandage following transepithelial excimer laser photorefractive keratectomy (PRK).
MethodsPatients undergoing transepithelial PRK for myopia were prospectively recruited. Included patients had a Comfilcon A silicone hydrogel lens inserted in one eye, with a Senofilcon A lens in the contralateral eye. Postoperative assessment of subjective pain, epithelial healing and visual recovery was at day 1, 3 and 7. Contact lens factors including centration, movement and deposits were assessed.
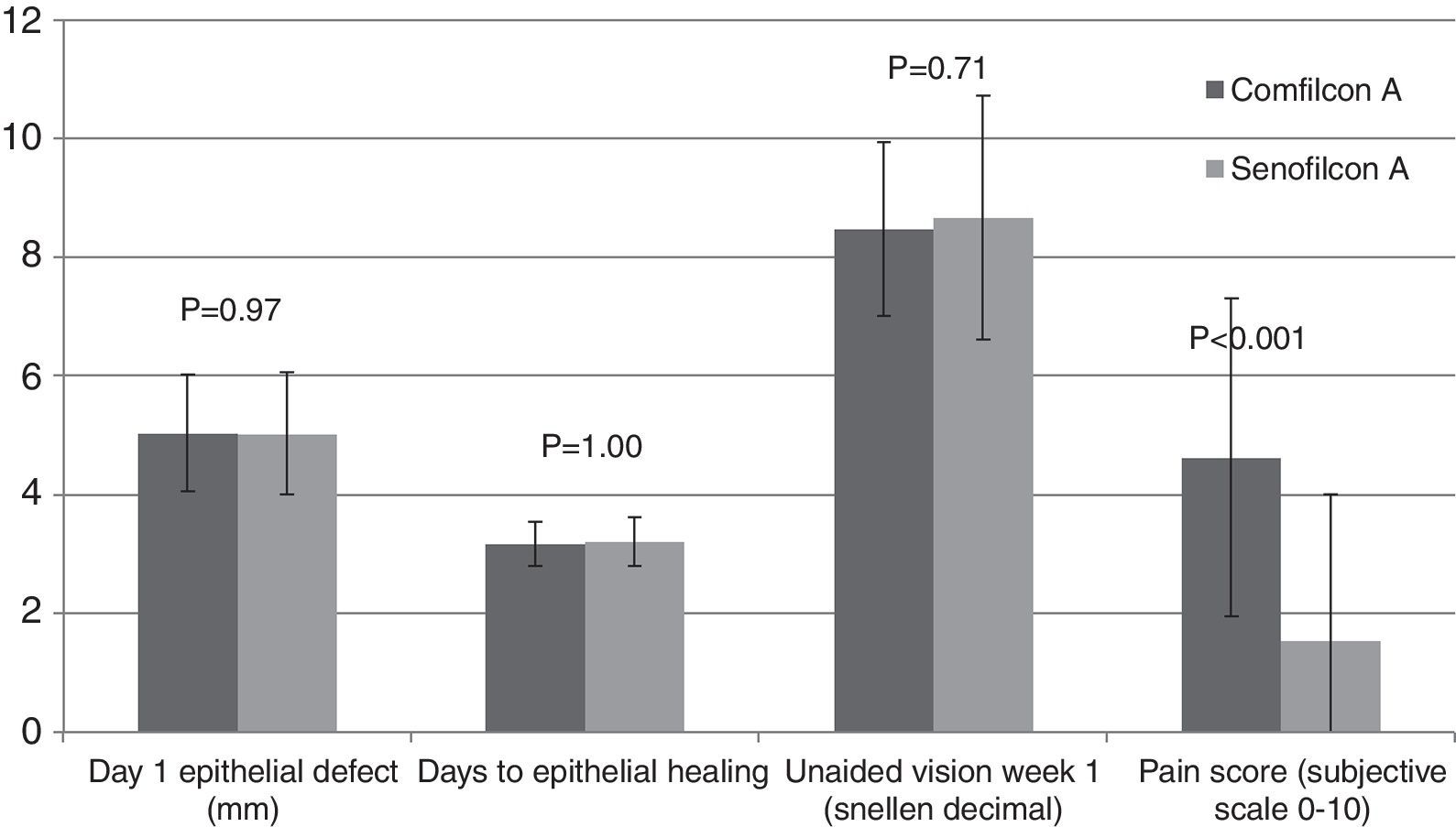
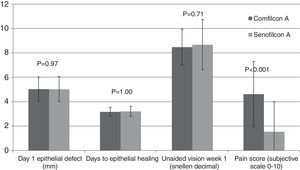
Results48 eyes of 24 patients were included in the study. Mean age was 31 years (SD 11) and mean refractive error −4.5 D (SD 1.8). Mean pain score at day 1 was significantly higher in the Comfilcon group at 4.6 (SD 2.7) vs. 1.5 (SD2.5) in the Senofilcon group (P<0.005). Mean time to healing was 3.17 days (SD 0.37) in the Comfilcon group, and 3.21 days (SD 0.4) in the Senofilcon group, with no difference in defect size. There was a pronounced central raphe in 1 eye in the Comfilcon group vs. 5 eyes in the Senofilcon group (P=0.19). Significantly more eyes demonstrated no lens movement in the Senofilcon group (18 vs. 4, P=0.0001).
ConclusionThe variation in material characteristics and lens geometry of different silicone hydrogel lenses affects their clinical characteristics in therapeutic roles. Other factors than oxygen permeability may affect pain and epithelial healing, with superior pain relief from the less permeable Senofilcon lens in this study.
Evaluar y comparar las lentes de contacto de hidrogel de silicona Comfilcon A y Senofilcon A, utilizadas como apósito terapéutico tras la realización de una queratectomía fotorrefractiva (PRK) mediante láser excimer transepitelial.
MétodosSe incluyó prospectivamente a pacientes sometidos a PRK transepitelial para corrección de miopía. Los pacientes incluídos en el estudio utilizaban una lente de hidrogel de silicona Comfilcon A en un ojo, y una lente Senofilcon A en el ojo contralateral. La evaluación postoperatoria del dolor subjetivo, reepitelización y recuperación visual se realizó los días 1, 3 y 7. Se evaluaron factores sobre lentes de contacto tales como centrado, movimiento y depósitos.
ResultadosEl estudio se completó incluyendo 48 ojos de 24 pacientes. La edad media fue de 31 años (DE 11) y el error refractivo medio de -4,5 D (DE 1,8). El índice medio de dolor en el día 1 fue considerablemente superior en el grupo de Comfilcon, con un valor de 4,6 (DE 2,7), frente a 1,5 (DE 2,5) en el grupo de Senofilcon (P<0,005). El tiempo medio de reepitelización fue de 3,17 días (DE 0,37) en el grupo de Comfilcon, y de 3,21 días (DE 0,4) en el grupo de Senofilcon, sin diferencia en cuanto a tamaño de defecto. Se produjo erosión central pronunciadaenen un ojo del grupo de Comfilcon, frente a cinco ojos en el grupo de Senofilcon (P=0,19). Los ojos del grupo de Senofilcon reflejaron una considerable diferencia en cuanto a ausencia de movimiento de la lente (18 frente a 4, P=0,0001).
ConclusiónLa variación en cuanto a características del material y geometría de las distintas lentes de hidrogel de silicona afecta a sus características clínicas de función terapéutica. En este estudio, otros factores diferentes a la permeabilidad del oxígeno pueden afectar al dolor y a la curación epitelial, con un alivio superior del dolor en el grupo de las lentes Senofilcon, que son menos permeables.
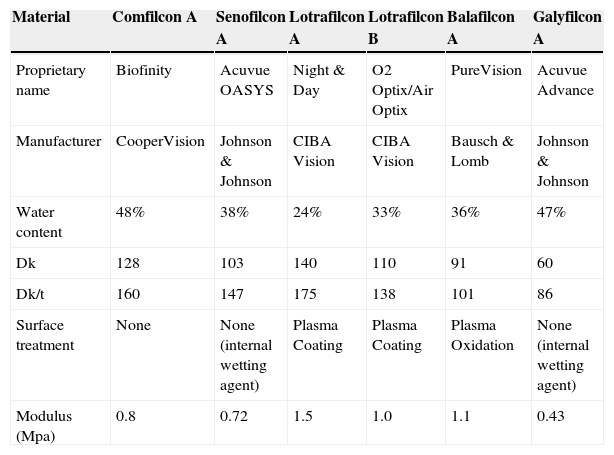
Photorefractive keratectomy (PRK) is an established procedure for the excimer laser correction of refractive errors.1 One of the major limitations of PRK is the postoperative pain and delay of visual recovery while epithelial healing takes place. Soft hydrogel contact lenses have been widely used as a bandage to reduce pain and optimise the epithelial healing process, both in PRK and subsequently LASEK.2 In this situation, the bandage contact lens is typically inserted at the time of surgery and used on a continuous extended wear basis for 2–7 days. The most commonly used type of lens for this indication has been conventional hydrogel material. However these lenses are not intended for extended wear, and do not provide adequate corneal oxygenation, which may inhibit the healing process.3–6 Following the introduction of silicone hydrogel lenses, there is a superior option to maintain oxygenation during epithelial regeneration. Existing studies support this notion, with faster re-epithelisation and reduced discomfort using silicone hydrogel lenses compared to conventional hydrogel lenses.3,4,7–10 Different silicone hydrogel lenses vary considerably with respect to a number of characteristics in addition to oxygen permeability alone (Table 1). These include water content, material stiffness (Young's modulus), thickness, edge profile, surface smoothness, surface treatments, hydrophobicity, size and base curve. The effect of these characteristics individually on pain and epithelial healing is not well elucidated; nevertheless there may be considerable variation in the performance of different silicone lenses. In the current study we determined the relative merits of two silicone hydrogel lenses when used as a bandage following transepithelial photorefractive keratectomy.
Characteristics of Silicone hydrogel lenses used in study and comparison with other commonly available Silicone hydrogel lenses.
| Material | Comfilcon A | Senofilcon A | Lotrafilcon A | Lotrafilcon B | Balafilcon A | Galyfilcon A |
|---|---|---|---|---|---|---|
| Proprietary name | Biofinity | Acuvue OASYS | Night & Day | O2 Optix/Air Optix | PureVision | Acuvue Advance |
| Manufacturer | CooperVision | Johnson & Johnson | CIBA Vision | CIBA Vision | Bausch & Lomb | Johnson & Johnson |
| Water content | 48% | 38% | 24% | 33% | 36% | 47% |
| Dk | 128 | 103 | 140 | 110 | 91 | 60 |
| Dk/t | 160 | 147 | 175 | 138 | 101 | 86 |
| Surface treatment | None | None (internal wetting agent) | Plasma Coating | Plasma Coating | Plasma Oxidation | None (internal wetting agent) |
| Modulus (Mpa) | 0.8 | 0.72 | 1.5 | 1.0 | 1.1 | 0.43 |
Dk: Oxygen permeability (×10−11); Dk/t: oxygen transmissibility (×10−9).
This was a prospective double masked contralateral eye study carried out at a refractive surgical centre in Heraklion, Greece. After undergoing transepithelial PRK for myopia, a Comfilcon A (Biofinity, Coopervision, Fairport, NY) silicone hydrogel lens was inserted in one eye, with a Senofilcon A (Acuvue Oasys, Johnson & Johnson, Jacksonville, FL) lens in the contralateral eye. Patients were included subject to informed consent, and prior ethical approval was obtained from the institutional review board. The research conformed to the tenets of the Declaration of Helsinki. Patients were excluded in the presence of any ocular or systemic condition which might affect epithelial healing or pain perception. In particular patients with significant dry eye or any corneal epithelial abnormality were excluded.
Surgical techniquePreoperative topical anaesthesia was with 0.5% preservative free proxymetacaine. All treatments were carried out with single step transepithelial PRK using the Schwind Amaris 750 excimer laser platform. This excimer laser platform uses a 750Hz flying spot laser of 0.54mm super Gaussian profile, with 6-axis eye tracking. In the transepithelial treatment, excimer ablation of the epithelium and refractive ablation of the stroma are carried out in one continuous ablation profile. In contrast to mechanical or alcohol assisted epithelial removal during conventional PRK, laser epithelial removal in tPRK results in an epithelial defect of consistent size, with a regular smooth edge matching the stromal ablated area. This predictable regular defect avoids the inherent variability of epithelial defects present in conventional PRK, and thus provides a better experimental context for the evaluation of postoperative recovery than conventional PRK. A Comfilcon A silicone hydrogel lens (base curve 8.6mm, diameter 14.0mm, power −0.50D) was inserted in one eye, with a Senofilcon A lens (base curve 8.4mm, diameter 14.0mm, power −0.50D) in the contralateral eye. The laterality of insertion was determined from a custom randomisation table.
Clinical assessmentPreoperative history, refraction, vision and absence of corneal and ocular surface pathology were noted. Although patients were aware from the consent process that different contact lenses would be used in either eye, no information as to the nature of the specific lenses was provided. The operating surgeon was also not aware of the random lens choice selected by the assistant at the time of the procedure. The assessing doctor postoperatively was not aware of the laterality of lens used. Postoperative study assessment was at day 1, 3 and 7 with an additional visit at 5 days if epithelisation was incomplete at day 3. Postoperative assessment at each visit was carried out by the same experienced practitioners, and included vision and slitlamp biomicroscopy. Subjective pain perception was assessed using a 0–10 numeric pain rating scale administered verbally, with 0 representing no discomfort and 10 representing severe pain. The epithelial defect was quantified by measuring the horizontal and vertical size at the slitlamp using the scale provided with a narrow slit beam. The area was calculated using the major and minor radii of the ellipse thus obtained. Contact lens centration was noted and degree of movement of the lens on blinking classified into none, minimal moderate or large. Contact lens deposits were noted, and graded according to the scheme of Gil-Cazorla et al.3
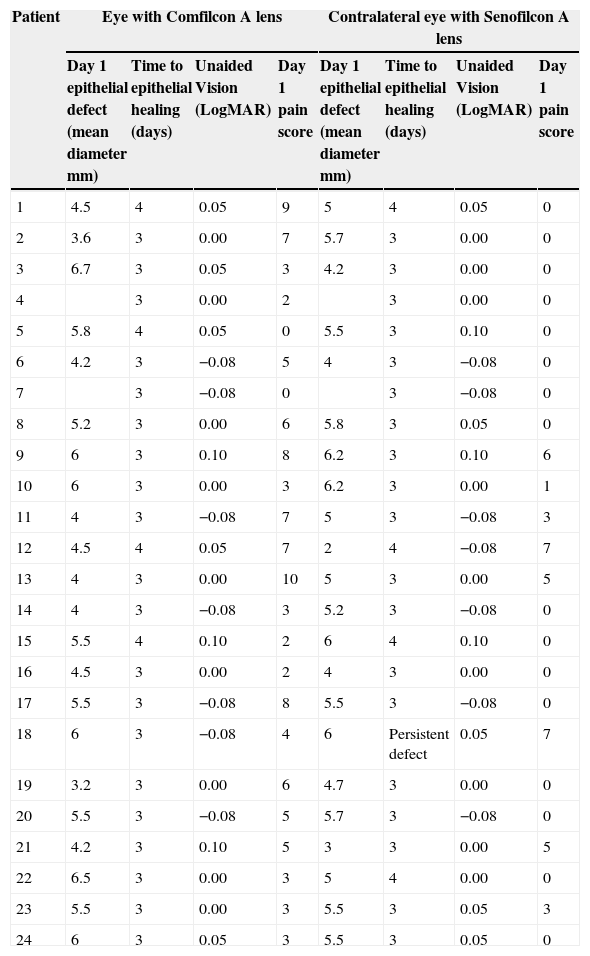
ResultsThe study population consisted of 50 eyes of 25 patients. One patient was excluded due to inadequate follow-up, leaving 48 eyes for analysis. The mean age was 31 years (SD 11: 22–41). Mean spherical equivalent error was −4.5D (SD 1.8: −8 to −1.5). Baseline comparison of Comfilcon and Senofilcon groups demonstrated no significant difference in spherical equivalent (−4.5D vs. −4.5D), astigmatism (−0.7D vs. −0.8D) or preoperative vision (0.00 vs. 0.00 LogMAR), with P<0.001 for all variables. All other factors were constant due to the contralateral eye design, and in all cases utilising Mitomycin C this was in both eyes. Raw clinical data for each patient are provided as Appendix 1 to this paper.
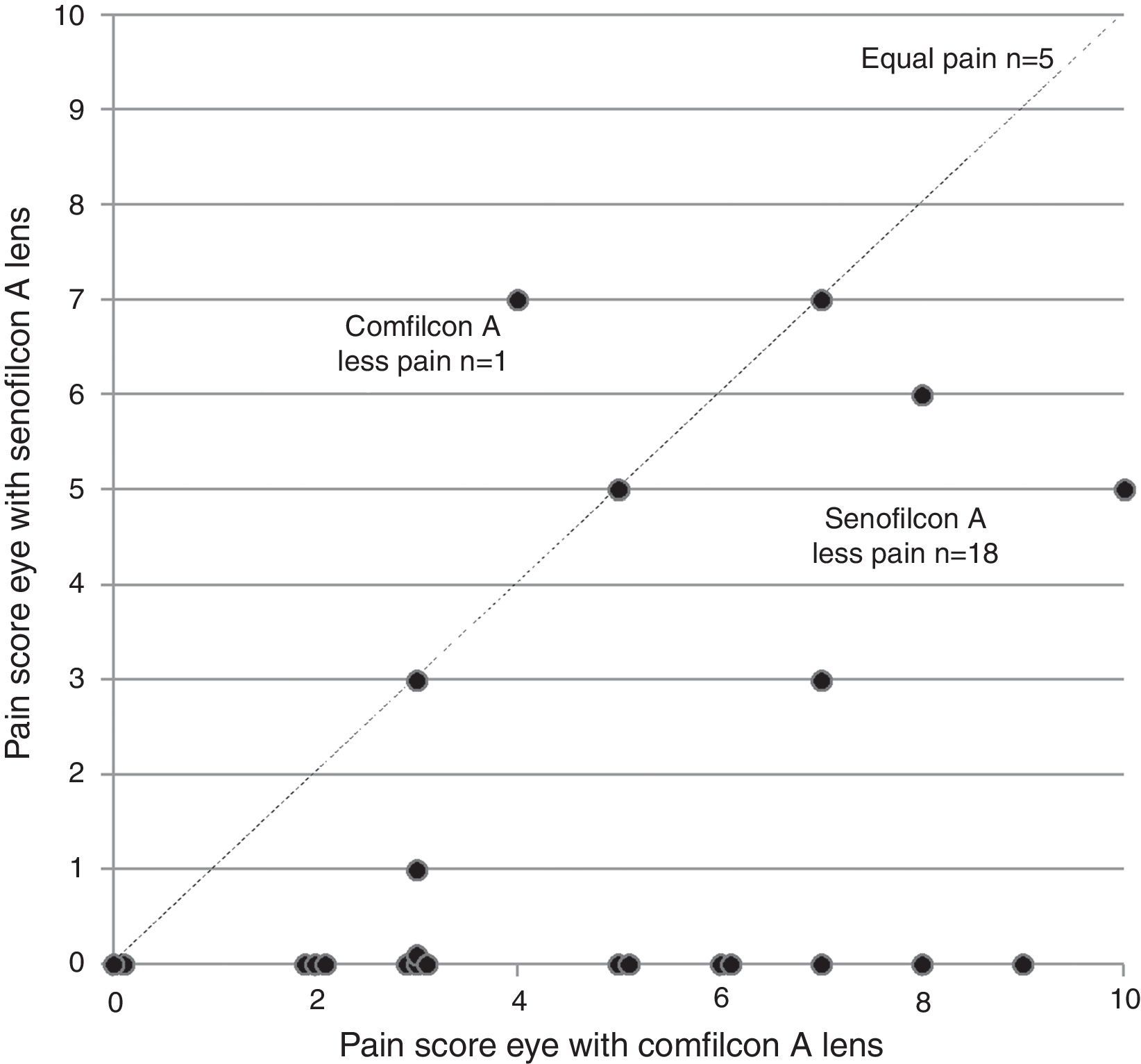
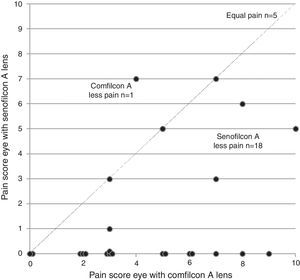
PainMean pain score at day 1 was 4.6 (SD 2.7: range 0–10) in the Comfilcon group, and 1.5 (SD 2.5: range 0–7) in the Senofilcon group (Fig. 1). The pain scores in the Comfilcon group were statistically significantly greater (P<0.005 paired 2 tailed T-test). For each patient, the pain score was greater in the eye with Comfilcon lens in 18 (75%), equal in both eyes in 5 (21%) and greater in the eye with Senofilcon lens in 1 (4%), with significantly more patients finding the Comfilcon lens more painful (P=0.01 Sign test) (Fig. 2).
Inter-eye comparison of subjective pain scores between a second (Senofilcon A) and third generation (Comfilcon A) silicone hydrogel bandage contact lens in contralateral eyes after transepithelial photorefractive keratectomy. Each point represents one patient, with points below the dashed line indicating that pain was lesser in the eye with a Senofilcon A lens.
Mean epithelial defect size at day 1 was 20.8mm2 (SD 7.7: range 8.0–35.3) in the Comfilcon group, and 20.7 mm2 (SD 7.1: range 3.1–30.2) in the Senofilcon group. For each patient, epithelial defect size was larger in the Comfilcon eye in 8 (36%), larger in the Senofilcon eye in 11 (50%) and equal in the remainder. In two patients the epithelial defect could not be characterised accurately. There was no significant difference between groups with respect to mean defect size or assignment of greater defect to either lens. The mean time for epithelial healing was 3.17 days (SD 0.37: range 3–4) in the Comfilcon group, while 3.21 days (SD 0.4: range 3–4) in the Senofilcon group. The majority of eyes had healed epithelium at day 3, with 4 (17%) in the Comfilcon and 5 (21%) in the Senofilcon groups taking longer than 3 days to heal. Of these 4 eyes in the Comfilcon group all healed by day 4, while of the 5 eyes in the Senofilcon group, 4 eyes healed by day 4, but one eye developed a persistent defect requiring epithelial debridement which resulted in subsequent late healing. The assessment of quality of central epithelium at the time of contact lens removal revealed a pronounced central raphe in 1 eye in the Comfilcon whereas 5 eyes had a pronounced raphe in the Senofilcon group, although this difference was not significant (P=0.19).
VisionMean LogMAR equivalent early uncorrected visual acuity at day 5 in the Comfilcon group was 0.08 (SD 0.08: range 0.0–0.3), 0.07 (SD 0.1: range −0.08 to 0.3) in the Senofilcon group (P=0.7). At 1 month postoperatively, the uncorrected acuity was 0.00 (SD 0.06: range −0.08 to 0.1) in Comfilcon and 0.00 (SD 0.06: range −0.08 to 0.1) in the Senofilcon group (P=1.0). There was no statistical difference between groups in this regard.
Contact lens assessmentMean lens movement score was higher at 1.1 (SD 0.6: range 0–2) in the Comfilcon compared to 0.17 (SD 0.4: range 0–1) in the Senofilcon group (P=0.0008). Significantly more eyes also demonstrated no movement (grade 0) in the Senofilcon group than the Comfilcon group (18 vs. 4, P=0.0001). 4 eyes demonstrated mild (grade 1–2) clinically observable contact lens deposits in the Senofilcon group, with 1 (grade 1) in the Comfilcon group (P=0.35). No association between pain or epithelial healing and lens movement or deposits was identified.
DiscussionThe use of silicone hydrogel lenses following surface excimer refractive surgical procedures has become recognised to offer benefits with regard to epithelial healing.3,4,6,8 There has been a progressive development of desirable features of such lenses. First generation silicone hydrogel lenses require hydrophilic surface treatments, and have relatively high modulus and low water content. Second generation lenses have higher water content due to internal wetting agents. Third generation lenses have lower modulus, while maintaining higher water content without internal wetting agents.6
In this study we evaluated two silicone hydrogel lenses used as therapeutic bandages following PRK surgery. One lens, the Acuvue Oasys, is composed of Senofilcon A, a second generation silicone hydrogel material. This material differs from earlier first generation materials in having an internally incorporated wetting agent (polyvinyl pyrrolidone), rather than depending on surface treatments to maintain wetting. As a result the material has a moderately high water content (38%) and is relatively low in stiffness (modulus 0.73MPa).3,11–13 By comparison the Biofinity lens is composed of the third generation material, Comfilcon A. This is an inherently wettable polymer, which, like Senofilcon requires no surface treatment for wettability. As a result the Comfilcon material has both a higher water content (48%) and higher oxygen transmissibility (Dk 128 units) compared to Senofilcon, while maintaining a low stiffness modulus of 0.75MPa.6,13,14 Surface characteristics also differ, and the Comfilcon and Senofilcon lens surfaces have been shown to differ by atomic force microscopy, with some evidence of a smoother surface in Comfilcon lenses.13,14
Given these differences of Comfilcon to Senofilcon in these various parameters, it might be expected to offer some advantage as a bandage lens. In this study, however, we found no difference in the speed of epithelial healing between the two lenses. The subjective assessment of epithelial healing quality did favour the Comfilcon lens, with a smoother epithelial surface as evidenced by a lower proportion of eyes with a visible central raphe, but this difference was not statistically significant, and appeared to be of little clinical relevance. There was also no difference in early visual recovery following healing.
The main finding of this study was of superior pain control following PRK with the Senofilcon compared to the Comfilcon lens, with significantly lower pain scores. This is consistent with the findings of other previous studies. Razmjoo et al. compared a Senofilcon A to lotrafilcon A lens for PRK and found better pain and discomfort control with Senofilcon.11 Qu et al. compared a Galyfilcon A lens to Balafilcon A for LASEK and found better pain control with Galyfilcon.7 This is notable because Galyfilcon is a precursor to the development of Senofilcon, and both share many chemical characteristics. Grentzelos et al. compared lotrafilcon A and lotrafilcon B for PRK and found no difference in pain.15 Plaka et al. compared Asmofilcon A to Lotrafilcon B following PRK, but did not assess subjective pain.16
The mechanism of pain relief by contact lenses is not well elucidated. Although the Comfilcon lens appears equivalent or superior in a range of material characteristics, there may be other factors involved in pain relief. It is notable that the Senofilcon lens in this study demonstrated significantly reduced movement compared to the Comfilcon lens. The potential benefits of tight fit for bandage use has been suggested by some authors.15,17 In this study, a base curve of 8.4 was used for the Senofilcon A lens, while the Comfilcon A lens was of base curve 8.6. It is thus possible that a tighter fit with reduced mobility of the Senofilcon lens accounts for the greater relief of pain, by preventing blink effects on the exposed nerve endings or friable nascent epithelium.6
ConclusionThe expected performance of various silicone hydrogel lenses when used in a therapeutic role for pain or epithelial healing depends on a number of factors, and may not easily be predicted on the basis of material or geometry characteristics. Thus, clinical evaluation of lens types is valuable to determine the optimal lens choice in this setting.
Ethical approvalThe study was performed with informed consent and approval by the Local Ethics Committee. Research adhered to the tenets of the Declaration of Helsinki.
FundingNo financial support was received for this submission.
Conflict of interestNone of the authors have conflict of interest with the submission. No author has any financial interest in the subject matter.
| Patient | Eye with Comfilcon A lens | Contralateral eye with Senofilcon A lens | ||||||
|---|---|---|---|---|---|---|---|---|
| Day 1 epithelial defect (mean diameter mm) | Time to epithelial healing (days) | Unaided Vision (LogMAR) | Day 1 pain score | Day 1 epithelial defect (mean diameter mm) | Time to epithelial healing (days) | Unaided Vision (LogMAR) | Day 1 pain score | |
| 1 | 4.5 | 4 | 0.05 | 9 | 5 | 4 | 0.05 | 0 |
| 2 | 3.6 | 3 | 0.00 | 7 | 5.7 | 3 | 0.00 | 0 |
| 3 | 6.7 | 3 | 0.05 | 3 | 4.2 | 3 | 0.00 | 0 |
| 4 | 3 | 0.00 | 2 | 3 | 0.00 | 0 | ||
| 5 | 5.8 | 4 | 0.05 | 0 | 5.5 | 3 | 0.10 | 0 |
| 6 | 4.2 | 3 | −0.08 | 5 | 4 | 3 | −0.08 | 0 |
| 7 | 3 | −0.08 | 0 | 3 | −0.08 | 0 | ||
| 8 | 5.2 | 3 | 0.00 | 6 | 5.8 | 3 | 0.05 | 0 |
| 9 | 6 | 3 | 0.10 | 8 | 6.2 | 3 | 0.10 | 6 |
| 10 | 6 | 3 | 0.00 | 3 | 6.2 | 3 | 0.00 | 1 |
| 11 | 4 | 3 | −0.08 | 7 | 5 | 3 | −0.08 | 3 |
| 12 | 4.5 | 4 | 0.05 | 7 | 2 | 4 | −0.08 | 7 |
| 13 | 4 | 3 | 0.00 | 10 | 5 | 3 | 0.00 | 5 |
| 14 | 4 | 3 | −0.08 | 3 | 5.2 | 3 | −0.08 | 0 |
| 15 | 5.5 | 4 | 0.10 | 2 | 6 | 4 | 0.10 | 0 |
| 16 | 4.5 | 3 | 0.00 | 2 | 4 | 3 | 0.00 | 0 |
| 17 | 5.5 | 3 | −0.08 | 8 | 5.5 | 3 | −0.08 | 0 |
| 18 | 6 | 3 | −0.08 | 4 | 6 | Persistent defect | 0.05 | 7 |
| 19 | 3.2 | 3 | 0.00 | 6 | 4.7 | 3 | 0.00 | 0 |
| 20 | 5.5 | 3 | −0.08 | 5 | 5.7 | 3 | −0.08 | 0 |
| 21 | 4.2 | 3 | 0.10 | 5 | 3 | 3 | 0.00 | 5 |
| 22 | 6.5 | 3 | 0.00 | 3 | 5 | 4 | 0.00 | 0 |
| 23 | 5.5 | 3 | 0.00 | 3 | 5.5 | 3 | 0.05 | 3 |
| 24 | 6 | 3 | 0.05 | 3 | 5.5 | 3 | 0.05 | 0 |