The purpose of this study was to evaluate the association between the federally mandated Minimum Data Set (MDS) Vision Patterns assessment for nursing home residents in the United States and an assessment of their vision-targeted quality of life as assessed by certified nursing assistants (CNAs).
MethodsParticipants were 371 residents over the age of 55 from 17 nursing homes in the Birmingham, Alabama metropolitan area and the CNAs directly assigned to their care. CNAs assessed the vision-targeted quality of life of residents in their charge using the Nursing Home Vision-Targeted Health-Related Quality of Life (NHVQoL) questionnaire. MDS assessment categories assigned to each resident by the MDS nurse coordinator (“adequate”, “impaired”, “moderately impaired”, “highly impaired”, “severely impaired”) were obtained from the medical record. Visual acuity was measured using logMAR charts by trained research staff.
ResultsCNA-rated NHVQoL subscale scores decreased as the MDS rating indicated more vision impairment (all P's for trend <0.05). Almost all mean scores were in the 80s and 90s for those in the adequate, impaired, and moderately impaired categories. For those with MDS ratings of severely or highly impaired, NHVQoL subscale scores (except ocular symptoms) were dramatically lower (P≤0.001) than those rated as moderately impaired.
ConclusionsRatings by CNAs on the vision-targeted quality of life of nursing home residents under their care is in general agreement with the MDS category assigned by the nurse coordinator. However, CNA ratings are largely homogeneous in the adequate vision to moderately impaired categories.
El objetivo de este estudio era analizar la relación entre el apartado de Visión, perteneciente al cuestionario Conjunto de Datos Mínimo (en inglés, MDS) que las autoridades federales estadounidense obligan a realizar a las personas que viven en residencias de ancianos de los EE. UU., y la evaluación de su calidad de vida en relación con la visión que realizan las asistentes de enfermería (AE) que les atienden en dichas residencias.
MétodosParticiparos 371 residentes mayores de 55 años provenientes de 17 residencias de ancianos distintas situadas en Birmingham, Alabama (EE. UU.). También participaron las AE encargadas de la atención de dichos residentes. Las AE evaluaron la calidad de vida en relación con la visión de los residentes a su cargo, utilizando para ello un cuestionario específico para residencias de ancianos denominado “Calidad de vida y estado de salud en lo que respecta a visión” (o sus siglas en inglés, NHVQoL). Por otro lado, la coordinadora de enfermería del MDS asignó a cada residente, a partir de los datos recabados de su historia médica, una de las siguientes categorías de MDS-Visión: “Aceptable”, “Ligeramente deficiente”, “Moderadamente deficiente”, “Muy deficiente”, “Gravemente deficiente”. La agudeza visual de los participantes la midió personal cualificado utilizando una escala logMAR.
ResultadosLas puntuaciones asignadas a cada participante por las AE en las distintas subsecciones del cuestionario NHVQoL disminuyeron a medida que la categoría de MDS-Visión asignada a ese participante indicaba una mayor deficiencia visual (todos los valores de P relativos a correlación <0,05). Casi todas las puntuaciones promedio obtenidas por los residentes incluidos en la categorías de MDS-Visión “Aceptable”, “Ligeramente deficiente” y “Moderadamente deficiente” estaban comprendidas entre 80 y 99 puntos. Para aquellos incluidos en las categorías de MDS-Visión “Muy deficiente” o “Gravemente deficiente”, las puntuaciones obtenidas en las distintas subsecciones del cuestionario NHVQoL (excluyendo Síntomas Oculares) fueron muchísimo más bajas (P≤0.001) que las obtenidas por aquellos con visión “Moderadamente deficiente”.
ConclusionesLas puntuaciones dadas por las AE a los residentes a su cargo de residencias de ancianos, en lo que respecta a su calidad de vida relacionada con la visión concuerda en general bastante bien con la categoría de MDS-Visión asignada por el coordinador de enfermería. Sin embargo, las puntuaciones dadas por las AE a los integrantes de las categorías de MDS-Visión “Aceptable”, Ligeramente deficiente” y “Moderadamente deficiente” son bastante similares.
The population of persons aged 85 and older in the United States is expected to more than triple over the next forty years.1 With advanced age being one of the strongest predictors of nursing home placement, the number of nursing home residents in the United States is expected to more than quadruple in just the next twenty years.2 Vision impairment is a common problem among older adult nursing home residents. These residents are 3 to 30 times more likely to have vision impairment than community dwelling older adults.3-5 It has been demonstrated that refractive error correction and cataract surgery can improve visual function and vision-related quality of life, slow functional decline and reduce depressive symptoms among nursing home residents.6-8 However, the number of nursing home residents receiving eye examination is low, despite the high prevalence of vision impairment in this group and the existence of interventions proven to be effective in correcting vision impairment. One issue is that in the United States eye examinations are not federally mandated for nursing home residents,9 and research has suggested that less than 50% of residents ever receive an eye examination after placement.4,10-14
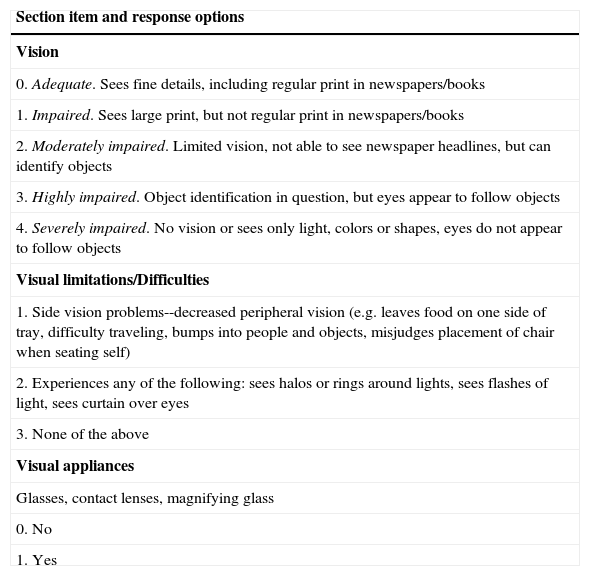
Legislation enacted in 1987 required the implementation of the National Resident Assessment Instrument (RAI) for all nursing homes participating in the federal health care programs Medicare and Medicaid. The RAI is comprised of two parts, the Minimum Data Set (MDS) and Resident Assessment Protocols (RAPs). The MDS is a nearly four hundred item multi-dimensional assessment intended to reflect the resident's status over the previous week. Residents are evaluated using the MDS on admission, quarterly, annually, and whenever there is a significant change in status.15 The MDS is completed by each facility's designated RAI/MDS nurse coordinator and ideally incorporates input from multiple sources, including the resident and other healthcare providers in the nursing home. The MDS assessment together with the triggered RAP (in the case of impairment on the MDS assessment) is intended to guide nursing home staff to the appropriate care that a resident would need.16 In the case of vision this may mean arranging for professional vision examination or making vision-related environmental or care modifications. The currently administered version (namely MDS 2.0) has a section collectively referred to as “Vision Patterns,” which assesses three areas (seeTable 1): 1) quality of vision, 2) visual limitations/difficulties, and 3) use of visual appliances. For this system to function as intended, the MDS must be a valid screening assessment of the visual status of residents. A previous investigation of the validity of the Vision Patterns section of the MDS found that it had questionable validity as a mechanism for triggering comprehensive eye examinations for nursing home residents who have vision impairment.17
Items from the MDS 2.0 Vision Patterns
| Section item and response options |
| Vision |
| 0. Adequate. Sees fine details, including regular print in newspapers/books |
| 1. Impaired. Sees large print, but not regular print in newspapers/books |
| 2. Moderately impaired. Limited vision, not able to see newspaper headlines, but can identify objects |
| 3. Highly impaired. Object identification in question, but eyes appear to follow objects |
| 4. Severely impaired. No vision or sees only light, colors or shapes, eyes do not appear to follow objects |
| Visual limitations/Difficulties |
| 1. Side vision problems--decreased peripheral vision (e.g. leaves food on one side of tray, difficulty traveling, bumps into people and objects, misjudges placement of chair when seating self) |
| 2. Experiences any of the following: sees halos or rings around lights, sees flashes of light, sees curtain over eyes |
| 3. None of the above |
| Visual appliances |
| Glasses, contact lenses, magnifying glass |
| 0. No |
| 1. Yes |
Certified nursing assistants (CNA) provide the bulk of direct care to nursing home residents in the United States. Their duties include assisting with activities of daily living such as feeding, bathing, and toileting, as well as monitoring weight and vital signs such as temperature. In essence, they spend considerable one-on-one time observing and interacting with residents. CNA's training typically consists of a 10 to 12 week didactic program that includes supervised clinical experiences. Given the close direct working relationship CNAs have with residents, one might expect that they would be very familiar with residents’ everyday visual function and with the extent to which they are experiencing difficulties. Governmental guidelines for completing the MDS suggest that the MDS nurse coordinator solicit the CNA's input. The extent to which CNAs participate in formulating the MDS vision assessment is unknown. One previous study reported that CNAs are not regularly a part of the care plan team18 while another found that, in the absence of resident selfreports by the resident for MDS items, CNAs assessments were solicited.19 A question that remains unanswered is to what extent CNAs’ judgments about residents’ vision-targeted quality of life (e.g., visual difficulties) agrees with the MDS rating provided by the nurse coordinator. The purpose of this study was to examine the relationship between the nurse-coordinator-charted MDS 2.0 assessment of Vision Patterns and the CNA rated Nursing Home Vision-Targeted Health-Related Quality of Life Questionnaire (NHVQoL).
MethodsStudy Design and ParticipantsA detailed description of the study sample and of its primary outcomes has been provided previously.4 Briefly, subjects were 371 residents of 17 nursing homes in the Birmingham Alabama metropolitan area. Potentially eligible residents were identified by the unit charge nurse as persons who would be able to answer questions about health and functioning. In addition, residents had to be at least 55 years of age, English speakers, and have a Mini-Mental State Examination (MMSE)20 score of 13 or above, since aspects of the main study's protocol required participants to follow directions and answer questions. Each nursing home was asked to identify the CNA most closely associated with each individual participating resident. Written informed consent was obtained from both the resident and their sponsor (family member or guardian) after explaining the nature and purpose of the study. This research project was approved by the University of Alabama at Birmingham Institutional Review Board and followed the Tenets of the Declaration of Helsinki.
Data Collection and Variable DefinitionsData was collected through medical chart review and direct assessment or interview. Visual acuity was measured by trained research staff in the resident's room or other area with adequate lighting. Residents wore the habitual prescriptive lenses as routinely used in everyday life; if they had none, they wore none. Distance acuity was measured with the ETDRS chart using the standard protocol with acuity expressed in logMAR (log of the minimum angle of resolution) units.21 Utilizing a back illuminated ETDRS chart minimized differences in residents’ rooms and facilities. Near acuity testing was measured using Lighthouse's Near Visual Acuity Chart with a standardized light source at a distance of 40cm with acuity also expressed in logMAR units.
Assessments made on the Vision Patterns section from the MDS 2.0 completed closest in time to the objective visual function assessment described above, were obtained from the medical record. The Vision Patterns section is comprised of the following three areas: (1) Vision, assessing the resident's ability to see in adequate light with glasses (if used). Possible responses are based on definitions associated with near vision capabilities and range from 0 (adequate) to 4 (severely impaired); (2) Visual limitations/difficulties, assessing the presence of side vision problems/decreased peripheral vision, and whether or not the resident sees halos or rings around lights, flashes of lights, or “curtains” over the eyes; and 3) Visual appliances, assessing whether or not the resident uses specified optical devices; responses are “Yes” or “No”. For the purposes of this study, only the “Vision” item was used due to the small number of participants who were rated as having visual limitations/difficulties. Moreover, for the “Vision” item the levels 3 (“highly impaired) and 4 (“severely impaired”) were collapsed to a single group, again owing to the small number of subjects in these two groups.
The Nursing Home Vision-Targeted Health-Related Quality of Life Questionnaire (NHVQoL) was completed by the CNA who answered the items in terms of how they applied to the resident for whom they care; it was interviewer-administered by trained research staff. The NHVQoL was specifically designed for the nursing home population.22,23 The item design and question structure is based on the National Eye Institute-Vision Function Questionnaire (NEI-VFQ). The instrument consists of nine subscales focusing on general vision, reading, ocular symptoms, mobility, psychological stress, activities of daily living, activities/hobbies, adaptation/coping and social interaction. Subscale scores were computed by scaling individual items from 0-100 (where 100 represents the highest functional level and 0 the lowest) and then averaging the individual items. Besides these response options, many items had two additional options –“stopped doing this for other reasons or not interested in doing this” and “could do this but not given the opportunity”. If either of these responses was selected, then the item was not used to compute the subscale score. The NHVQoL has shown a reliability and validity equivalent to that seen with other quality of life measures used for nursing home residents.22 It has previously been used in studies as an outcome for evaluating the impact of cataract surgery and refractive error correction among nursing home residents.6,7
Statistical AnalysisAnalysis of variance was used to evaluate the presence of trends in NHVQoL subscale scores across MDS ratings. Ttests were used to compared the NHVQoL scores at a given MDS level of impairment to the next lower impairment level; for example, the NHVQoL scores for the “impaired” group were compared to those obtained for the “adequate” group. Pearson's correlation coefficients were calculated for the relationship between CNA NHVQoL score and the measured distance and near visual acuity (logMAR units) both for the better eye and worse eyes. P-values of 0.05 or less (two-sided) were considered to be statistically significant. Analysis was carried out using SAS version 9.1, (the SAS Institute, Cary, North Carolina, USA).
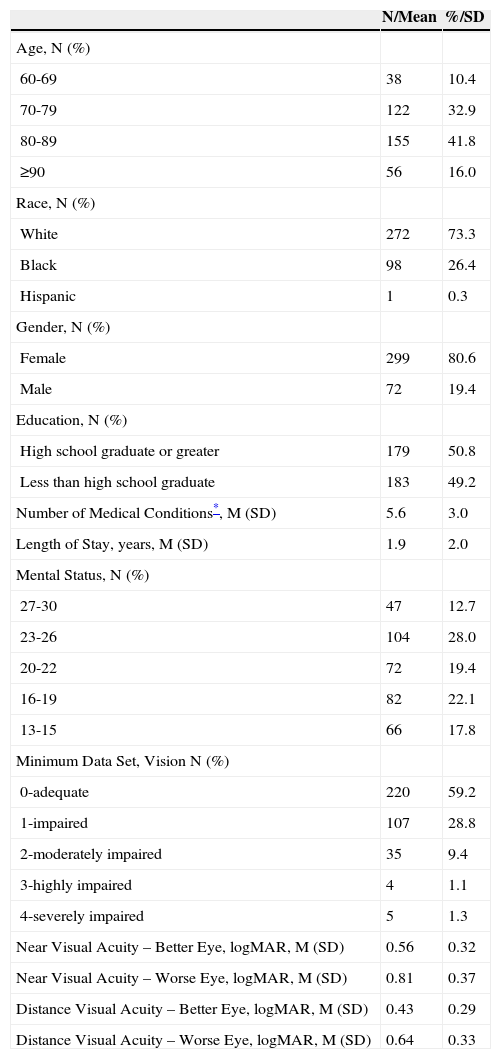
ResultsThe mean age of subjects was 81 years (SD 8.2) with a range going from 60 to 102 (Table 2). Approximately 75% of participants were white, and 81% of the sample were women. Most participants had been residents for at least 1 year with a mean length of stay of 1.9 years (SD 2.0) and a range covering from 0.1 to 12.4 years. Mean MMSE score was 20.9 (SD 4.7). MMSE scores below 24, typically used as a cutoff point for cognitive impairment indicative of dementia, were seen in 66% (247 of 371) of subjects. Participants had a mean of 5.6 chronic medical conditions (ranging from 0 to 15). The MDS rating for quality of vision ranged from 0 to 4 (see Table 1 for the descriptor associated with each category). The majority of residents (59%) were rated as having “adequate” vision, with 29% rated as having “impaired” vision and 9% with “moderately impaired” vision. Together, “highly” and “severely impaired” vision represented about 2% of the sample.
Demographic and Medical Characteristics (N=371)
| N/Mean | %/SD | |
| Age, N (%) | ||
| 60-69 | 38 | 10.4 |
| 70-79 | 122 | 32.9 |
| 80-89 | 155 | 41.8 |
| ≥90 | 56 | 16.0 |
| Race, N (%) | ||
| White | 272 | 73.3 |
| Black | 98 | 26.4 |
| Hispanic | 1 | 0.3 |
| Gender, N (%) | ||
| Female | 299 | 80.6 |
| Male | 72 | 19.4 |
| Education, N (%) | ||
| High school graduate or greater | 179 | 50.8 |
| Less than high school graduate | 183 | 49.2 |
| Number of Medical Conditions*, M (SD) | 5.6 | 3.0 |
| Length of Stay, years, M (SD) | 1.9 | 2.0 |
| Mental Status, N (%) | ||
| 27-30 | 47 | 12.7 |
| 23-26 | 104 | 28.0 |
| 20-22 | 72 | 19.4 |
| 16-19 | 82 | 22.1 |
| 13-15 | 66 | 17.8 |
| Minimum Data Set, Vision N (%) | ||
| 0-adequate | 220 | 59.2 |
| 1-impaired | 107 | 28.8 |
| 2-moderately impaired | 35 | 9.4 |
| 3-highly impaired | 4 | 1.1 |
| 4-severely impaired | 5 | 1.3 |
| Near Visual Acuity – Better Eye, logMAR, M (SD) | 0.56 | 0.32 |
| Near Visual Acuity – Worse Eye, logMAR, M (SD) | 0.81 | 0.37 |
| Distance Visual Acuity – Better Eye, logMAR, M (SD) | 0.43 | 0.29 |
| Distance Visual Acuity – Worse Eye, logMAR, M (SD) | 0.64 | 0.33 |
Mean distance acuity in each participant's better eye was 0.43 logMAR with a range going from -0.06 to 1.1 logMAR. Distance acuity in the worse eye ranged from 0.02 to 1.2 log-MAR. Using the United States definition of statutory blindness (20/200 or less in the better eye), 6.2% of subjects were legally blind. Distance acuity in the better eye worse than 20/40 (Snellen chart) is a frequently used criterion in the United States for defining visual impairment. Using this criterion 211 of 369 subjects (57.1%) were visually impaired. Mean near acuity in the better eye was 0.57 logMAR with a range going from -0.04 to 1.4 logMAR. Mean near acuity in the worse eye was 0.81 logMAR ranging from 0 to 1.4 logMAR.
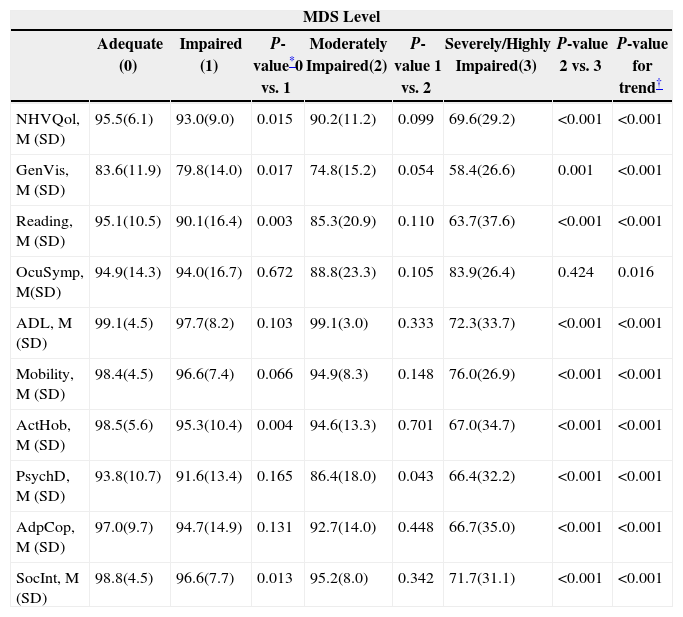
Regarding the scores on each of the NHVQoL subscales, as the MDS rating indicated worse visual function, the corresponding mean NHVQoL score decreased (Table 3). At the Adequate and Impaired MDS levels, all mean NHVQoL scores were in the 90s except for the “General Vision”. subscale. Several mean scores of those participants belonging to the Moderately-impaired category are also in the 90s with a few in the 80s and one in the 70s (General Vision). In the combined Severely/Highly-impaired category, NHVQoL scores are appreciably lower.
Nursing Home Vision Related Quality of Life and MDS Level
| MDS Level | ||||||||
| Adequate (0) | Impaired (1) | P-value*0 vs. 1 | Moderately Impaired(2) | P-value 1 vs. 2 | Severely/Highly Impaired(3) | P-value 2 vs. 3 | P-value for trend† | |
| NHVQol, M (SD) | 95.5(6.1) | 93.0(9.0) | 0.015 | 90.2(11.2) | 0.099 | 69.6(29.2) | <0.001 | <0.001 |
| GenVis, M (SD) | 83.6(11.9) | 79.8(14.0) | 0.017 | 74.8(15.2) | 0.054 | 58.4(26.6) | 0.001 | <0.001 |
| Reading, M (SD) | 95.1(10.5) | 90.1(16.4) | 0.003 | 85.3(20.9) | 0.110 | 63.7(37.6) | <0.001 | <0.001 |
| OcuSymp, M(SD) | 94.9(14.3) | 94.0(16.7) | 0.672 | 88.8(23.3) | 0.105 | 83.9(26.4) | 0.424 | 0.016 |
| ADL, M (SD) | 99.1(4.5) | 97.7(8.2) | 0.103 | 99.1(3.0) | 0.333 | 72.3(33.7) | <0.001 | <0.001 |
| Mobility, M (SD) | 98.4(4.5) | 96.6(7.4) | 0.066 | 94.9(8.3) | 0.148 | 76.0(26.9) | <0.001 | <0.001 |
| ActHob, M (SD) | 98.5(5.6) | 95.3(10.4) | 0.004 | 94.6(13.3) | 0.701 | 67.0(34.7) | <0.001 | <0.001 |
| PsychD, M (SD) | 93.8(10.7) | 91.6(13.4) | 0.165 | 86.4(18.0) | 0.043 | 66.4(32.2) | <0.001 | <0.001 |
| AdpCop, M (SD) | 97.0(9.7) | 94.7(14.9) | 0.131 | 92.7(14.0) | 0.448 | 66.7(35.0) | <0.001 | <0.001 |
| SocInt, M (SD) | 98.8(4.5) | 96.6(7.7) | 0.013 | 95.2(8.0) | 0.342 | 71.7(31.1) | <0.001 | <0.001 |
P-values for ANOVA comparing visual function at higher MDS level and next lower level (e.g. 0 vs.1, 1 vs. 2, 2 vs. 3). Categories 3 and 4 were combined for analysis.
P-values for ANOVA of MDS level and mean score. NHVQoL-composite score, GenVis-general vision subscale, Reading-reading subscale, OcSymp-Ocular symptoms subscale, ADL-activities of daily living subscale, Mobility- mobility subscale, ActHob- activities/hobbies subscale, PsychD-psychological stress subscale, AdpCop- adaptation and coping subscale, SocInt- social interaction subscale.
No significant differences were seen in NHVQoL scores when comparing those with “Adequate” MDS vision rating and “Mild Impaired” for the subscales of Ocular Symptoms, Activities of Daily Living, Mobility, Psychological Stress and Adaptation/Coping. Only the NHVQoL subscale scores for Psychological Stress and General Vision showed statistically significant differences between those in the “Mild” and “Moderate” impairment categories. All subscale scores of the NHVQoL, except for Ocular Symptoms, were statistically significant between “Moderate” and “Highly” impaired MDS levels. When comparing a two-step change in the MDS; e.g. from the “Adequate” to the “Moderately impaired” category, most NHVQoL scores (except those for ADL and Adaptation/Coping) were statistically significant. When looking at the extremes of the MDS vision rating scale; i.e., comparing “Adequate” vision and “Highly impaired” vision, all subscale scores were significantly different between the two rating groups, including Ocular Symptoms.
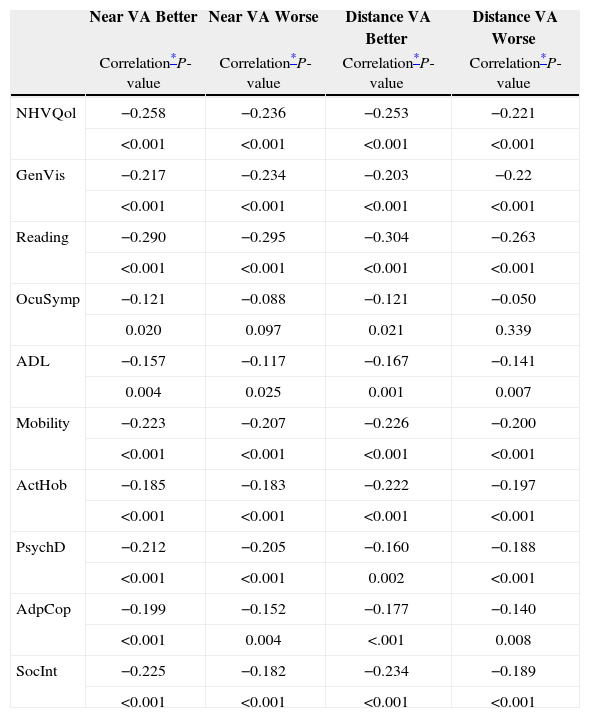
Correlations between all acuity measures and the NHVQoL subscale scores were statistically significant (all P<0.025) except for that between the ocular symptoms subscale and worse eye's distance and near acuity (seeTable 4). All correlation coefficients between logMAR visual acuity measures and NHVQoL scores were negative, indicating that better acuity (lower logMAR scores) was associated with higher NHVQoL scores. The highest correlations were found between both distance and near acuity measures and the Reading subscale score.
Correlation Coefficients for NHVQoL and Visual Acuity Measures
| Near VA Better | Near VA Worse | Distance VA Better | Distance VA Worse | |
| Correlation*P-value | Correlation*P-value | Correlation*P-value | Correlation*P-value | |
| NHVQol | −0.258 | −0.236 | −0.253 | −0.221 |
| <0.001 | <0.001 | <0.001 | <0.001 | |
| GenVis | −0.217 | −0.234 | −0.203 | −0.22 |
| <0.001 | <0.001 | <0.001 | <0.001 | |
| Reading | −0.290 | −0.295 | −0.304 | −0.263 |
| <0.001 | <0.001 | <0.001 | <0.001 | |
| OcuSymp | −0.121 | −0.088 | −0.121 | −0.050 |
| 0.020 | 0.097 | 0.021 | 0.339 | |
| ADL | −0.157 | −0.117 | −0.167 | −0.141 |
| 0.004 | 0.025 | 0.001 | 0.007 | |
| Mobility | −0.223 | −0.207 | −0.226 | −0.200 |
| <0.001 | <0.001 | <0.001 | <0.001 | |
| ActHob | −0.185 | −0.183 | −0.222 | −0.197 |
| <0.001 | <0.001 | <0.001 | <0.001 | |
| PsychD | −0.212 | −0.205 | −0.160 | −0.188 |
| <0.001 | <0.001 | 0.002 | <0.001 | |
| AdpCop | −0.199 | −0.152 | −0.177 | −0.140 |
| <0.001 | 0.004 | <.001 | 0.008 | |
| SocInt | −0.225 | −0.182 | −0.234 | −0.189 |
| <0.001 | <0.001 | <0.001 | <0.001 |
Pearson's correlation coefficient Near VA Better- LogMAR acuity at near better seeing eye Near VA Worse LogMAR acuity at near worse seeing eye Distance VA Better- LogMAR acuity at distance better seeing eye Distance VA Worse LogMAR acuity at distance worse seeing eye NHVQoL-composite score, GenVis-general vision subscale, Reading-reading subscale, OcSymp-Ocular symptoms subscale, ADL-activities of daily living subscale, Mobility- mobility subscale, ActHob- activities/hobbies subscale, PsychD-psychological stress subscale, AdpCop- adaptation and coping subscale, SocInt- social interaction subscale.
Our results show that as a nursing home resident's vision is rated as more impaired by the nurse coordinator on the MDS, the CNA's judgment of vision-targeted health-related quality of life is also likely to produce lower scores. Thus, there appears to be a general agreement between the MDS ratings as provided by the nurse coordinator/care team and the CNA's ratings of vision-targeted quality of life. Only the NHVQoL's Ocular Symptom subscale turned out to be unrelated to MDS levels, regardless of which categories were compared. It is important to point out that while the CNA's scores on the NHVQoL were lower as the MDS ratings moved toward greater impairment levels, the decreases in scores across MDS categories ranging from Adequate to Moderately Impaired are modest, even though statistically significant, and in some cases there are no decreases, depending on the specific subscale under analysis. This suggests that from the CNA's perspective (based on extensive everyday observation and interaction with the resident), visual functional differences in residents placed in the first two to three MDS categories (adequate, impaired, moderately impaired) are not readily differentiated based on the everyday behavior of residents and/or their interactions with the CNA.
On the other hand, the CNA's assessment of vision-related quality of life is dramatically worse (e.g., 20 points lower) for those residents in the combined MDS category of highly/severely impaired, as compared to those in the moderate impairment category. The MDS descriptors for highly and severely impaired levels correspond to very serious vision impairment or no light perception. The step between moderate impairment and the combined highly/severely impaired category appears to be large enough to allow both the MDS nurse coordinator and the CNAs (as revealed on the NHVQoL) to distinguish between these groups. Thus, the CNAs seem to be readily aware of serious visual disabilities through caring for residents and interacting with them. In general, our results show that the CNAs’ responses on the NHVQoL have construct validity with respect to visual acuity, in that CNAs indicated that persons with worse visual acuity for near or distance vision had more difficulties in the visual activities of daily living including reading.
This is one of very few studies to evaluate CNAs’ assessments of the quality of life as related to the MDS and the first to specifically focus on their assessment as related to the MDS vision pattern section. Most studies directly relating CNAs’ assessments and the quality of nursing home care in the United States have concentrated on the effects of staffing and turnover.24 Higher levels of CNA staffing and increased direct CNA contact hours have been associated with some positive nursing home outcomes including reduced levels of hospitalization and lower levels of pressure sore development.25,26 In other studies CNAs have been able to assess the pain level of residents with some degree of accuracy compared to clinical assessment.27,28 One study has suggested that CNA pain assessment more closely matches analgesic use than does the MDS pain assessment.19 In the current study, there was also significant associations between CNAs estimate of vision-targeted quality of life and resident's visual acuity.
The strengths of this study include its large sample size recrited across a large number of nursing homes and the use of a validated and nursing home vision-specific quality of life measure. We do recognize that despite its large sample size, the number of residents with severely impaired vision was low. Additionally, this study evaluated the association of two proxy assessments of visual status by facility staff within nursing homes (i.e. MDS nurse coordinators and CNAs). Proxy assessment of health related quality of life has been shown to be subject to both over and under estimation bias28 with the NHVQoL not being specifically designed with proxy observer use in mind.
Overall, the results of this study suggest that MDS nurse coordinators and CNAs at the nursing homes participating in this study were in general good agreement as to the visual status of their residents as measured through the MDS Visual Patterns section and the NHVQoL respectively. This is a positive finding in that CNAs ratings of residents’ vision-targeted quality of life were correlated with residents’ objective visual acuities. Although it is unknown if CNAs at the participating nursing homes were a part of the care plan team, the results of this study provide evidence that CNAs assessments should be solicited for completion of the MDS Visual Patterns section. In the absence of a federal mandate in the U.S. for routine vision examination for nursing home residents by an optometrist or ophthalmologist, the MDS Vision Patterns evaluation is a key component in assuring that nursing home residents in the United States receive appropriate referral for eye care services. Incorporating CNA assessments as a part of this process may increase the number of residents who are appropriately referred for eye care services. However, it should be cautioned that while CNAs appear to be able to differentiate those residents with severe vision problems from those who do not have severe vision problems, the NHVQoL scores for those belonging to the MDS categories Adequate, Impaired, And Moderately Impaired were very similar. This may be attributable to a number of factors, including problems with how the MDS rating criteria are defined,30 the MDS nurse coordinators not experiencing enough close contact with each resident to understand their daily visual difficulties, inadequate validity of the MDS with visual acuity,17 or the CNA's inability to detect more subtle visual difficulties through the resident's behavior. Future research should be directed at clarifying the validity of the MDS and how it should be implemented if it is to be used to trigger eye care services for nursing home residents in the U.S.
This research was supported by the Retirement Research Foundation, the EyeSight Foundation of Alabama, National Institutes of Health grant R21-EY14071, the Alfreda J. Schueler Trust, Pearle Vision Foundation, and Research to Prevent Blindness, Inc.
Financial disclosure: None of the authors has financial conflict of interests to report. None of the supporting institutions provided input into the preparation of this manuscript.