The aim of this study is to determine the anterior chamber depth (ACD) in teenagers using two different devices: partial coherence interferometry IOLMaster (Carl Zeiss Meditec) and anterior segment optical coherence tomography (Visante™ OCT, Carl Zeiss Meditec) and to evaluate the degree of agreement between ACD measurements carried out by both instruments.
MethodsIn this prospective study 68 eyes of 34 emmetropic Caucasic patients (18 girls and 16 boys) were analysed. ACD was measured from the anterior corneal surface to anterior surface of the crystalline lens. For each age the ACD size was calculated and the difference between IOLMaster and Visante-OCT measurements was analysed using Bland–Altman plot and paired t-test.
ResultsFor all data the mean (SD) anterior chamber depth was 3.56 (0.19)mm with the IOLMaster and 3.65 (0.21)mm with the Visante-OCT. IOLMaster measurements were an average of 0.10 (0.12)mm less than Visante-OCT (paired t-test, p<0.0001).
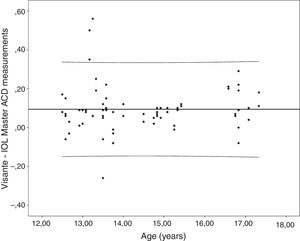
In our study ACD mean differences (SD) by age obtained had been −0.139 (0.163), −0.044 (0.112), −0.082 (0.054) and −0.105 (0.101) for 13, 14, 15 and 17 respectively. The 13-age group showed the larger standard deviation compared to the other groups.
ConclusionsIOLMaster and Visante-OCT are good and useful non-contact methods for measuring ACD in the healthy eyes of teenagers. The measurement differences between two devices were quite small, however, they should take into account in order to calculate the power on intraocular lens. The findings provide more normative date for this age group.
El objetivo de este estudio es determinar la profundidad de la cámara anterior en adolescentes, utilizando dos dispositivos diferentes: la interferometría de coherencia parcial IOLMaster (Carl Zeiss Meditec) y la tomografía de coherencia óptica del segmento anterior (Visante™ OCT, Carl Zeiss Meditec), así como evaluar el grado de concordancia entre las mediciones de la profundidad de la cámara anterior realizadas, utilizando ambos instrumentos.
MétodosEn este estudio prospectivo se analizaron 68 ojos de 34 pacientes caucásicos emetrópicos (18 chicas y 16 chicos). Se midió la profundidad de la cámara anterior desde la superficie anterior de la córnea a la superficie anterior del cristalino. Se calculó el tamaño de la profundidad de la cámara anterior para cada grupo de edad, y se analizó la diferencia entre las mediciones con IOLMaster y Visante-OCT, utilizando el gráfico Bland-Altman y la prueba de t pareada.
ResultadosPara todos los datos, la profundidad de la cámara anterior media (DE) fue de 3,56 (0,19) mm con IOLMaster y de 3,65 (0,21) con Visante-OCT. Las mediciones con IOLMaster fueron de media 0,10 (0,12) mm menores que las realizadas con Visante-OCT (Prueba de t pareada, p<0,0001).
En nuestro estudio, las diferencias medias (DE) de la profundidad de la cámara anterior por edad fueron de -0,139 (0,163), -0,044 (0,112), -0,082 (0,054) y -0,105 (0,101) para los grupos de 13, 14, 15 y 17 años, respectivamente. El grupo de 13 años aporta una desviación estándar superior a la del resto de grupos estudiados.
ConclusionesIOLMaster y Visante-OCT constituyen métodos de no contacto buenos y útiles para la medición de la profundidad de la cámara anterior en los ojos sanos de adolescentes. Las diferencias de medición entre ambos dispositivos fueron bastante peque¿nas, sin embargo, estas diferencias deberían tenerse en cuenta para el cálculo de la lente intraocular. Los hallazgos son interesantes ya que aportan más datos normativos para este grupo de edad.
Anterior chamber depth (ACD) measurement is very useful to provide valuable information in different fields of ophthalmology. Recently, this parameter has become increasingly important because it is essential for the new theoretical biometric formulas used to calculate the power on intraocular lenses (IOLs), as well as in surgical planning of IOL implantation and also it is used as a screening risk factor for glaucoma.1–5
Different methods for measuring the ACD are available, based in ultrasonic, optical and photographic techniques.6,7 The most common method for ACD measuring has been ultrasound (US) biometry. This method requires corneal contact and corneal applanation could be possible, which may lead to false results due to indentation of the cornea, and the exact axial placement of the probe relative to the centre of the cornea.8–12
Like all contact methods, it may be uncomfortable for the patient or even lead to damage of the corneal epithelium. Thus, non-contact methods are preferred for the ACD measurement.13,14
The optical systems to measure ACD, such as IOLMaster and Visante-OCT, were made commercially available several years ago. These devices have potential advantages, provide non-contact measurements and their use is reported to require minimal training.15–17
Previous reports5,7,11,17 have studied the agreements between ACD measurements obtained with these devices with different study population, for example: different pathologies and refractive errors, sex, ethnicity, and so on, in order to establish possible influence factors that could affect the clinical diagnostic.
Most of these studies5,11,17 have been carried out with adult populations, being less frequently among children and teenager population.
The aim of this study was to determinate the ACD in healthy emmetropes teenagers and to assess the agreements obtained using two methods of noninvasive ACD measurements, the IOLMaster and Visante-OCT, and to describe the potential advantages and disadvantages of each method, in order to verify the adequacy of both instruments to characterise the eyes of this population group.
Materials and methodsThis prospective study enrolled 34 healthy Caucasic emmetropic teenagers, with no anterior eye segment pathology on slitlamp examination, no previous intraocular surgery, no glaucoma of any type, and no wearer contact lenses. Emmetropia was defined as a spherical equivalent of ±0.25 D. The study was performed in compliance with the tenets of the Declaration of Helsinki. Informed consent was obtained in writing from a parent for each subject prior to their participation.
The same experienced examiner performed all measurements with two devices. The examiner was masked to the results obtained with each device.
Measurements of ACD from the corneal epithelium to the anterior surface of the crystalline lens were obtained using different devices, IOLMaster (Carl Zeiss Meditec, Dublin, CA) and Visante-OCT (Visante™, Carl Zeiss Meditec, Dublin, CA).
Each patient was evaluated on the same day. IOLMaster and Visante-OCT measurements were taken under identical physical environments and half the subjects were measured first using the IOLMaster and then using the Visante-OCT and the other half, vice versa, with approximate intervals of 15min between measurements to allow for relaxation of the patients and restoration of ocular tear film.
Subjects were seated in front of the device, in a typical position, using chinrest. All of them were instructed to keep both eyes open and fixate on a fixation target.
IOLMaster imaging techniqueThe IOLMaster uses the partial coherence interferometry principle to measure the axial length. The anterior chamber depth is determined by calculating the distance along the visual axis from the corneal epithelium to the anterior crystalline lens.17,18
Carl Zeiss, Meditec, Inc. Software Version 5.2.1 was used.
First, a valid keratometer measurement was performed prior to ACD measurement by the system automatically, because the IOLMaster system requires the input of the corneal radius.
The device took five ACD measurements in rapid succession; the mean of these readings was employed to the database.
Anterior segment optical coherence tomography techniqueThe Visante-OCT is a non-contact, high resolution tomographic and biomicroscopic device, that provides cross-sectional images of the anterior segment of the eye. This technique uses infrared (1310nm) radiation to provide real-time images of the anterior segment.19,20
Scans were centred on the pupil and taken along the horizontal meridian. The scan was optimally aligned when the optically produced corneal reflex was visible as a vertical white line along the centre of the cornea.
The images obtained were processed using analysis version 3.0.1.8 software of Enhanced Anterior Segment Single optical coherence tomography.
In the current study the Visante-OCT was used to obtain central corneal thickness and ACD. Visante-OCT measured ACD from the posterior surface of the cornea (endothelium), whereas IOLMaster from the anterior corneal surface (epithelium). Therefore, to compare ACD measurements between two instruments, we added to the ACD measurements results of the Visante-OCT the central corneal thickness value.
Statistical analysisStatistical analysis was performed using SPSS (Version 19.0 for Windows, SPSS Inc., Chicago, IL).
Kolmogorov–Smirnov test was used to test the data with respect to normality distribution, and difference in measurements between two methods was assessed using the paired t test. A value of p<0.05 was considered significant.
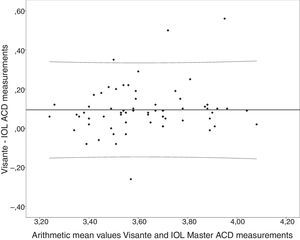
The ACD measurements by the two devices employed were graphically displayed in Bland–Altman plot, in order to obtain information of relationship between difference and averages, to identify any system bias and possible outliers. The 95% limits of agreements were determined using this method.21,22
ResultsSixty-eight eyes of 34 subjects were examined. Their mean (SD) age was 14.45 (1.51) years, range 13–17. There was no marked offset between ACD results of right and left eyes.
For all data the mean anterior chamber depth was 3.56 (0.19)mm with the IOLMaster and 3.65 (0.21)mm with the Visante-OCT (Table 1). Considering all data IOLMaster measurements were an average of 0.10 (0.12)mm less than Visante-OCT (paired t-test, p<0.0001) (Table 2).
Table 3 shows for each age the mean ACD measured with two devices, demographic properties of subjects and the differences between the two devices.
Demographic properties of subjects and mean differences in anterior chamber depth measurements.
| Age, (years) | n | IOLMaster (SD) (mm) | Visante-OCT (SD) (mm) | Mean difference (SD) (95% CI) | p-Value |
| 13 | 20 | 3.59 (0.19) | 3.73 (0.23) | −0.14 (0.16) (−0.22 to 0.06) | 0.0012* |
| 14 | 16 | 3.50 (0.16) | 3.55 (0.19) | −0.04 (0.11) (−0.10 to 0.02) | 0.1348 |
| 15 | 20 | 3.62 (0.22) | 3.69 (0.21) | −0.08 (0.05) (−0.11 to −0.06) | <0.0001* |
| 17 | 12 | 3.49 (0.16) | 3.59 (0.17) | −0.11 (0.10) (−0.17 to −0.04) | 0.0041* |
ACD, anterior chamber depth; SD, standard deviation; CI, confidence interval.
Bland–Altman plot is shown in the Fig. 1. The vertical axis represents the difference between Visante-OCT and IOLMaster measurements, and the horizontal axis shows the arithmetic mean values for ACD. The bold line represents the mean difference between ACD measurements with two devices. The simple lines represent the 95% limits of agreement. Fig. 2 shows the differences between Visante and IOLMaster measurements as a function of the patient's age.
There are several methods available for measuring the biometric parameters of anterior segment, such as anterior chamber depth. These methods use different techniques, and each has its own advantages and disadvantages. The accuracy of measuring instruments is an essential factor when selecting a device for clinical purpose.
According to Barret et al.6,7 these techniques can be classified as ultrasonic, optical and photographic. Ultrasound ACD measurements have been widely used in ophthalmology and optometry for a long time, so this technique has been considered as the gold standard.
Previous studies18,23–25 have shown that the ultrasound technique may not be very repeatable and studies comparing ultrasound with other optical instruments agree that ultrasonic ACD measurements are less repeatable and more variable. Perhaps, it may be due to the influence of different factors related with the techniques employed.
The values measured with contact US devices can be distorted, apart by indentation of the cornea, by other factors such as the experience of the operator, measurement, the differences in probe tip handling, and the different settings of US velocity. Indentation of the cornea during contact measurements can be eliminated with the immersion technique but it can be uncomfortable for subjects additionally this technique requires experience and knowledge of the ideal pattern of ultrasonic spikes,26,27 so in our study we used noncontact methods, because they are more comfortable and faster.
The optical systems to measure ACD, such as IOLMaster and Visante-OCT, are commercially available for several years now. These devices have potential advantages, provide non-contact measurements and their use is reported to require minimal training. The current study was restricted to the assessment of agreement. Given that high repeatability and reproducibility have already been shown in previous studies,26,28 we did not evaluate this to avoid unnecessary examinations of the participants.
The accuracy of a measuring instrument is an essential factor when selecting a device for clinical purpose, so the study of the interchangeably of the results obtained of different optical systems is relevant.
In this study, we measured the ACD in 68 emmetropic healthy eyes with two different non-contact optical devices. We found a good agreement between measurements obtained. In our study we report ACD values in a teenager population. We have not found a direct size progression between ACD values and age. Dispersion of ACD measurements (difference between maximum and minimum ACD values) is higher for the 13-age group maybe poorer collaboration.
Fig. 1 shows there was a tendency towards higher readings with Visante-OCT when compared with IOLMaster readings. Comparison of the ACD measurements showed a systematic difference between the two methods, with a mean difference of 0.097mm.
Our findings appear to be consistent with other studies.28,29 In a previous study involving adults, Lavanya et al.29 found good agreement between three different non-contact methods, IOLMaster, AS-OCT and Scanning Peripheral Anterior Chamber (SPAC), although there were small but significant differences in the measurements.
Possible factors could influence in this differences related, mainly, with the accommodation and the pupil size.29,30 In our study, accommodation was minimised by adjusting the fixation target, whereas the IOLMaster does not have a non-accommodative fixation target. The anterior chamber depth of the human eye also depends on the accommodative state of the eye, so with IOL Master device, subjects were directed to focus on the internal measurement target within the instrument head and were asked not to look outside the machine. This likely introduced a degree of accommodation which may have contributed to the difference in ACD measurements between the 2 instruments. Related with pupil size, IOLMaster can give inaccurate measurements in subjects with small pupils. In addition, the use an infrared light source in the Visante-OCT may keep the pupil size unaltered, thereby presumably giving a more accurate ACD value. Other explanations for the differences between readings with different devices could be related with physical principles of each device, although it should not alter the readings.
In this work, cyclopegic agents were not used, but the non-accommodative fixation target was used in Visante-OCT. In the techniques employed in our study, the correct alignment of the beam is important because only a minor deviation of the correct direction affects the results of the ACD measurements. So, an important source of error that can arise during ACD evaluation is off-axis measurement.
Utine et al.17 evaluated measurements in myopic subjects in order to correlate values with the refractive error. They demonstrated that there was not any significant relationship between ACD and refractive error, although the difference in the ACD measurements obtained with IOLMaster and Orbscan seemed to rise slightly with increasing refractive error.
Tong et al.24 examined the agreement in anterior chamber length in children (aged between 6 and 12 years) using A-Scan ultrasonography and Scheimpflug photography. The authors found differences in readings obtained using these two devices, and these differences do not appear to be consistent with other studies involving adults. It can be concluded that findings in the above studies may arise from methodological differences as well as different subjects. In our study, we did not find significant differences found in other studies involving adults.
The ACD in clinically normal eyes of teenagers is measured differently by IOLMaster and Visante-OCT. The 95% limits of agreement were narrowest, suggesting that these two instruments have good agreement. Rosa et al.31 measured the ACD with IOLMaster and Orbscan II. They found a good agreement between the two devices before and after photorefractive keractectomy (PRK) and suggested that the differences were not clinically significant. Contrarily, Nemeth et al.26 obtained significantly deeper ACD values with anterior segment OCT than with immersion A-Scan so they did not consider interchangeable measurements with both devices in spite of the high correlation with each other. O’Donnel et al.32 recently compared central corneal thickness (CCT) and ACD measurements using three techniques. The results showed an acceptable agreement between the Pentacam and LenStar and poorer between the Visante and LenStar and between the Visante and Pentacam, so they suggested that the CCT and ACD measures from these instruments should not be used interchangeably.
According to Nemeth et al.26 and O’Donnel et al.32 we consider measurements with IOLMaster and Visante-OCT should not be interchangeable in this population studied. From our point of view we think Visante measurements are more accurate, because the accommodation is controlled by a fixation point. On the other hand, IOLMaster might be underestimated ACD measurements because it uses different fixation target, so the role of accommodation might be a source of bias.
In conclusion, small but significant differences exist between the Visante AS-OCT and the IOLMaster. Hence, the clinician should take the different modalities into consideration during ACD assessment using various devices.
This study adds to our previous knowledge of ACD measurement difference with various devices available. The two instruments employed may produce statistically different values in teenager; however, although the absolute differences are quite small they should take into account in order to calculate the power on intraocular lens. The findings are interesting, as they provide more normative date for this age group. However, a more extensive study will be necessary to obtain a global standard ACD values for teenager population with these instruments.
FundingNone.
Conflicts of interestThe authors have no conflicts of interest to declare.