The aim of this study was to characterize the quality of primary care referrals of patients to ophthalmology at the Virgen Macarena Hospital in Seville. This will enable us to optimize ophthalmologic resources and to evaluate the role of the optometrist in improving referrals.
MethodsWe performed a retrospective cross-sectional review of 220 ophthalmology consultations referred from primary care to the hospital from March to May 2022.
The following data were extracted: age, sex, reason for consultation, diagnosis, priority level, whether it was an initial consultation or a follow-up visit, whether there was a secondary referral and whether the referral was appropriate. Excel (version 2312) was used for the data analysis.
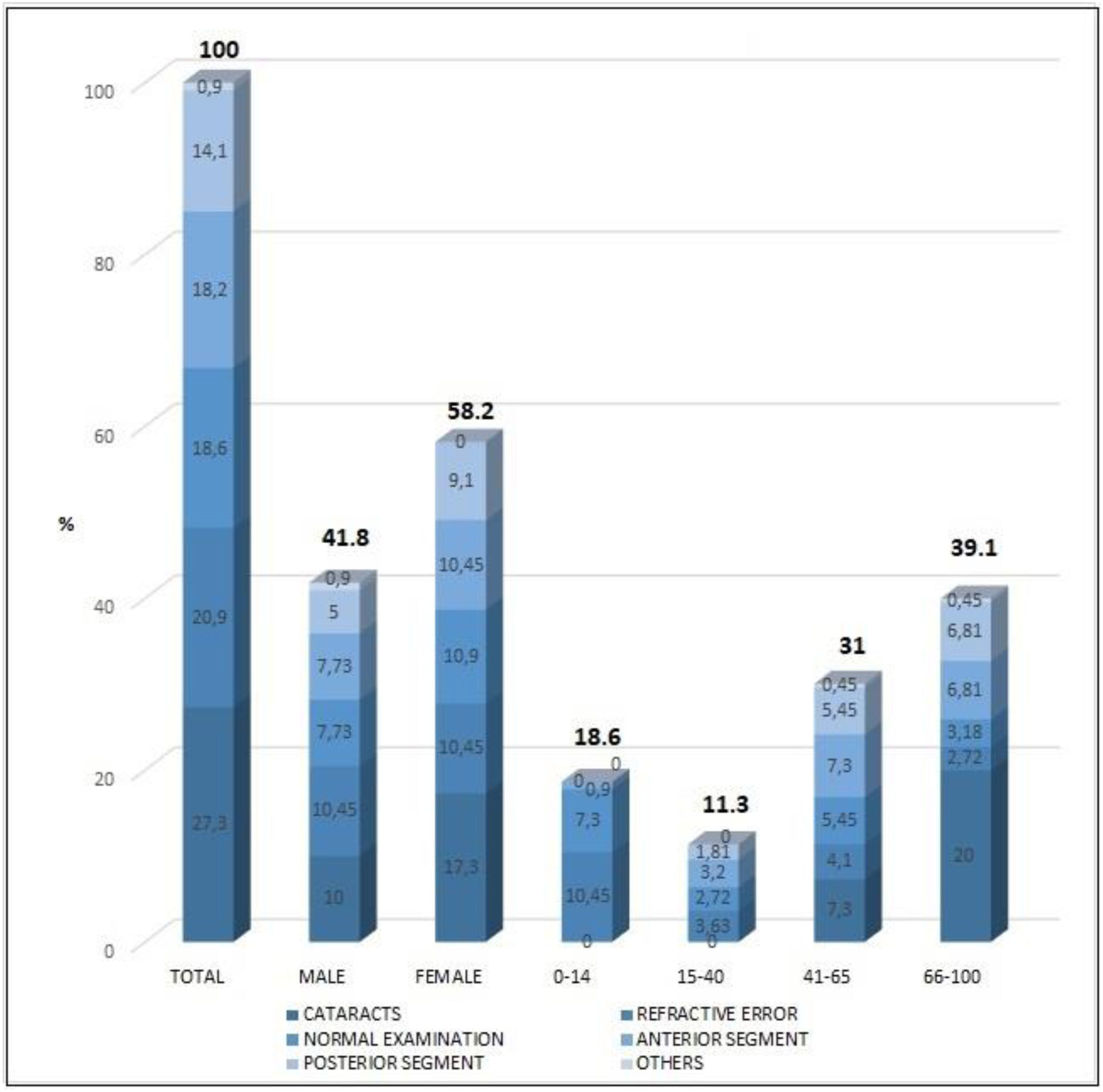
ResultsThe age range of the patients was from 3 years to 91 years. The patients were 41.8 % male and 58.2 % female. The conditions found were grouped as follows: cataracts (27.27 %), refractive errors (20.9 %), anterior segment disease (18.8 %), posterior segment disease (14.07 %), normal examination (18.63 %) and others (0.9 %). The most common reason for consultation was blurred vision or loss of vision (43.63 %). In total, 41.36 % of the consultations were considered inappropriate. The age group requiring the highest number of consultations was over 65 years (38.64 %).
ConclusionsWith 41.36 percent of referrals deemed unnecessary, it is clear that referrals can be improved. This would reduce strain on the ophthalmology service and improve patient care. The importance of the optometrist in primary care is demonstrated by the fact that 20.9 % of the diagnoses were refractive errors.
Spain's population is aging. According to data from the Spanish Ministry of Health, life expectancy at birth in Spain in 2021 was 83.2 years: 80.3 in men and 86.1 in women1 As a result, access to specialist consultations could be increasingly delayed, due to the increased demand and the reduced number of specialists available in the public health system. According to the Spanish Ministry of Health website, ophthalmology is one of the specialties with the highest number of consultations both in specialized centers and hospitals.2
It is therefore essential to study the efficiency of the healthcare resources available and to explore ways of improving specialized care. Spain has an advanced, world-class public health system, but even so it will not be able to meet the demands of future healthcare needs.3 The National Health System is decentralized to the autonomous communities, each of which is responsible for organizing its regional health system. The healthcare system in the Autonomous Community of Andalusia is divided into primary care and hospital care. Primary care is organized territorially in primary care districts. Each district is organized into basic health zones. These are the territorial units of care. Each zone has one or more primary care centers. There are three types of primary care centers: health centers, local clinics and auxiliary clinics. The second level, hospital care, treats patients requiring specialized care. This comprises outpatient clinics in hospitals and peripheral centers. The Andalusian Health Service has 5 regional hospitals, 10 specialty hospitals, 19 community hospitals and 16 high resolution hospitals.4
This study was carried out at the Virgen Macarena University Hospital (VMUH) in Seville. This hospital is divided into 36 clinical management units. The VMUH ophthalmology clinical management unit has 40 specialist physicians and 8 residents. as well as nurses, assistants and administrative staff and is equipped with the latest ophthalmology technology. In 2017, the unit performed 64,434 ophthalmological consultations and 5914 surgical interventions.5 In 2023, the number of consultations exceeded 92,000, of which approximately 20,000 came from Primary Care.
Few studies have evaluated the cooperation between primary care and ophthalmology.6 Through this study we conducted a descriptive analysis of the referrals from primary care centers to the ophthalmology service of VMUH in the Seville catchment area and an assessment of the quality of these referrals.
Understanding, evaluating and classifying these consultations will allow us to optimize the resources of the ophthalmology service, as well as to design new strategies for patient care in both primary and specialized care. Knowing which are the most common conditions will make it possible to more efficiently allocate the material and human resources available for ophthalmologic care. This will also improve training of personnel, investment in diagnostic and surgical equipment and the incorporation of treatments based on increased demand. In addition, since optician-optometrists are not currently part of the Andalusian public health system, their inclusion could be considered.
MethodologyPatients and methodsA retrospective cross-sectional review of 220 consultation reports was carried out for patients referred from primary care medical centers to the VMUH, a first-level hospital, in Seville, Spain, from March 17, 2022 to May 1, 2022. A simple random sample of patients from all the ophthalmology visits was used as representative of all the ophthalmologists in the service. A total of 2192 ophthalmology consultations were performed during the study period. With a 95 % confidence level, the selected sample size of 220 patients would give a possible error of 0.062 in the estimation of the proportion of referrals deemed inappropriate by the ophthalmologist. No patients were selected on the basis of sex. The sex of the patients was recorded only in order to disaggregate the results. The study authors did not review the consultation records, nor did they have contact with the patients or with those responsible for data collection. Data collection was performed by a licensed ophthalmologist and was anonymous to protect patient privacy. A numerical code was assigned to each patient to ensure that the investigators had no access to the personal data from each consultation. The study complied with the Spanish Data Protection Act and the Declaration of Helsinki. Data were stored in an Excel sheet for later analysis. The authors have no personal or financial interests to declare.
The referring ophthalmologist reviewed the medical records and classified the diagnoses into the following categories: cataracts, refractive error, normal examination, anterior segment diseases, posterior segment diseases and others. Cataracts and refractive error were not grouped due to the high percentage of incidence compared to the rest of the diagnoses. The rest of the diagnoses were very varied and few in number, so they were grouped into anterior segment diseases, posterior segment diseases and others, the latter group including cluster headache and post-surgical visual impairment.
The following variables were also collected: age, sex, reason for consultation, whether there was a referral to another specialized ophthalmology unit, whether there was a need for prioritization over other patients, and whether the referral was appropriate. An appropriate referral was understood as the correct referral of a patient from primary care to the specialized ophthalmology service, provided that the referral criteria were met.
Patient age was categorized into age groups for greater significance. From 0 to 14 years, as pediatric patients; 15 to 40 years, a more stable age range in refractions and with less incidence of disease; 41 to 65, as the beginning of presbyopia7 and 66 to 100 years, when diseases such as cataracts, glaucoma and age-related macular degeneration (AMD) become more prominent.8-11 Sex was classified as male or female.12 For the variable reason for consultation, we recorded the patient's complaint as reported by the primary care physician.
To assess the relevance and appropriateness of the referrals, and in the absence of guidelines or reference criteria in Spain, we used the criteria of the Royal Brisbane & Women's Hospital13 and the University Hospital of Wales.14 Two ophthalmologists independently evaluated each case and qualified it as appropriate or inappropriate, and assessed the priority level at referral, indicating whether it was correct. In the event of disagreement, the cases were discussed by both ophthalmologists and a third evaluator.
Statistical analysisData analysis was carried out using Excel (version 2312). The main variables are represented by frequency tables and graphs. The Chi-square test was used to compare the categorical values of the diagnosed disease and whether or not the consultation was appropriate, as well as whether or not the patient was referred for a specialized ophthalmology consultation. It was also used to determine the possible relationship between the diagnosed disease and the age and sex of the patient. The test was considered significant for a p-value < 0.05.
ResultsOf the total number of patients studied, 92 were male (41.8 %) and 128 were female (58.2 %). The percentage of patients in each of the four age groups was 0 to 14 years (18.63 %), 15 to 40 years (11.63 %), 41 to 65 years (31.36 %) and 66 to 100 years (39.54 %).
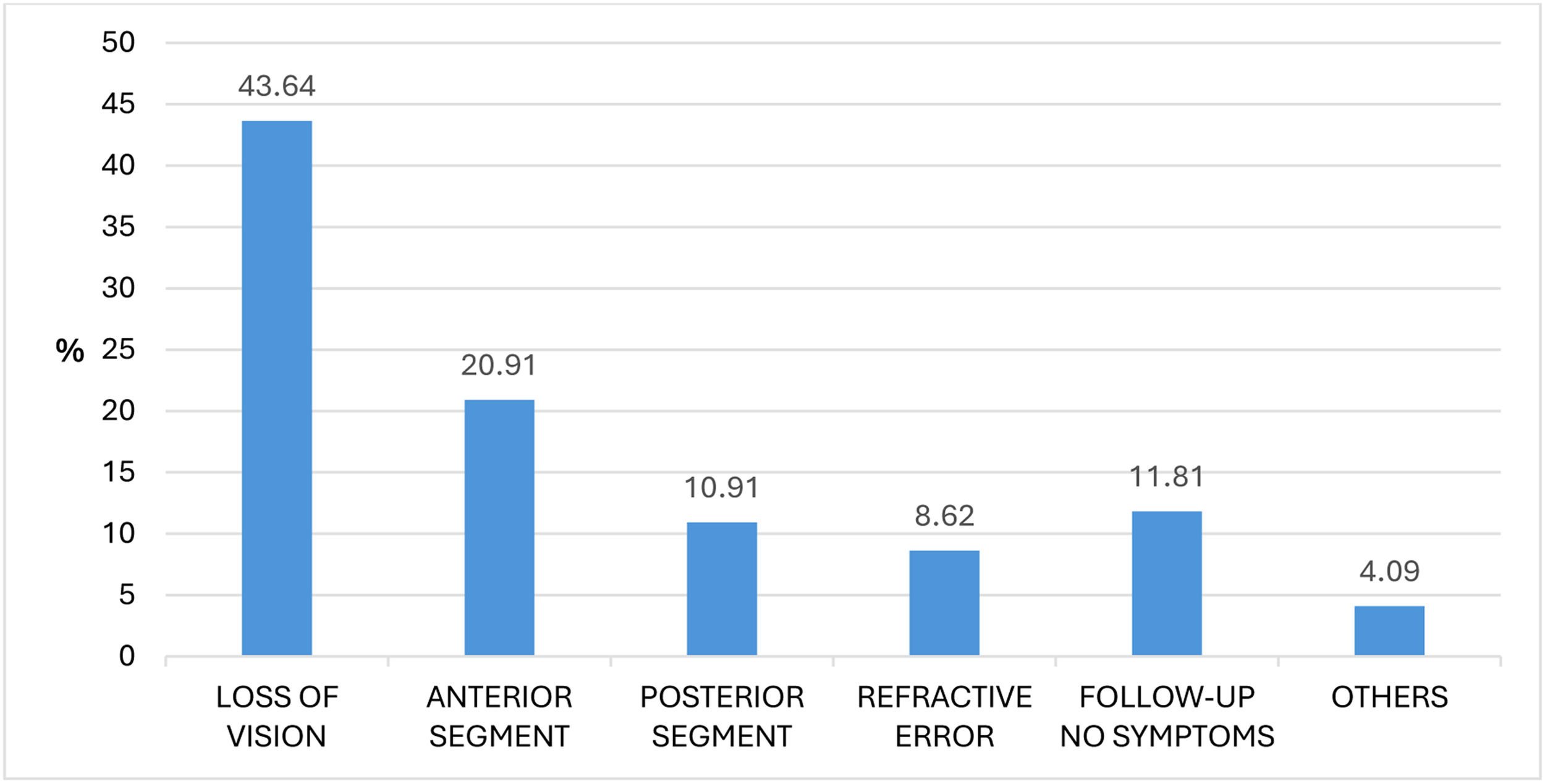
The reasons for which patients sought medical attention and were referred to the ophthalmology service were grouped according to the part of the eye affected: blurred vision or loss of vision (43.64 %), anterior segment (20.91 %), posterior segment
(10.91 %), refractive error (8.62 %), follow-up with no symptoms (11.81 %) and others (4.09 %). The main complaint was blurred vision or loss of vision.
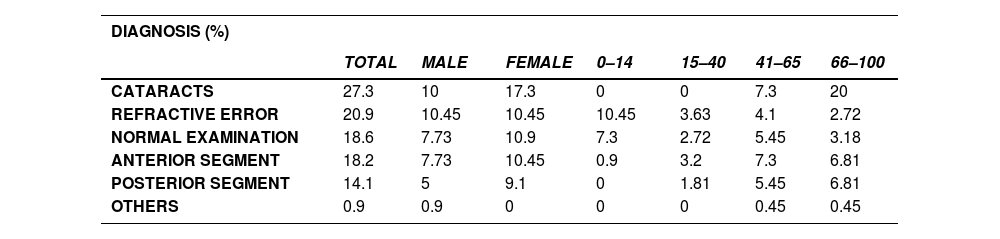
The percentages of each group of conditions were calculated according to sex and age.
Table 1 shows the percentage of each diagnosis group. The first column shows the percentage of the total sample in each group. The following columns show the percentage of the total for each diagnosis according to sex and age. The most frequent disease in the referrals was cataracts with 27.3 %. This was more common in females than in males and in the age group 66 years and older. Refractive error referrals were the second most frequent category. There were no differences between sexes, and more patients were referred for this reason in the age range 0–14 years. Normal examination accounted for 18.6 % of the total sample and was more common in females and in the age group 0–14 years. Anterior segment diseases were more common in females and in the age groups 41–65 and 66–100 years. Posterior segment diseases, similar to those of the anterior segment, were more common in the female population and in the 41–65 and 65–100 age groups. There were no cases in those under 40 years of age.
Grouped diagnoses. Total sample, by sex and by age. (%).
Fig. 2 illustrates the percentages of each diagnosis category in the total sample, by sex and by age group.
The number of patients who should have been prioritized by the primary care physician to ophthalmology services due to the severity of their ocular condition was also recorded. It was found that 9.09 % of the patients who were referred should have been prioritized versus 90.9 % who should not have been. These patients should have been seen before the rest.
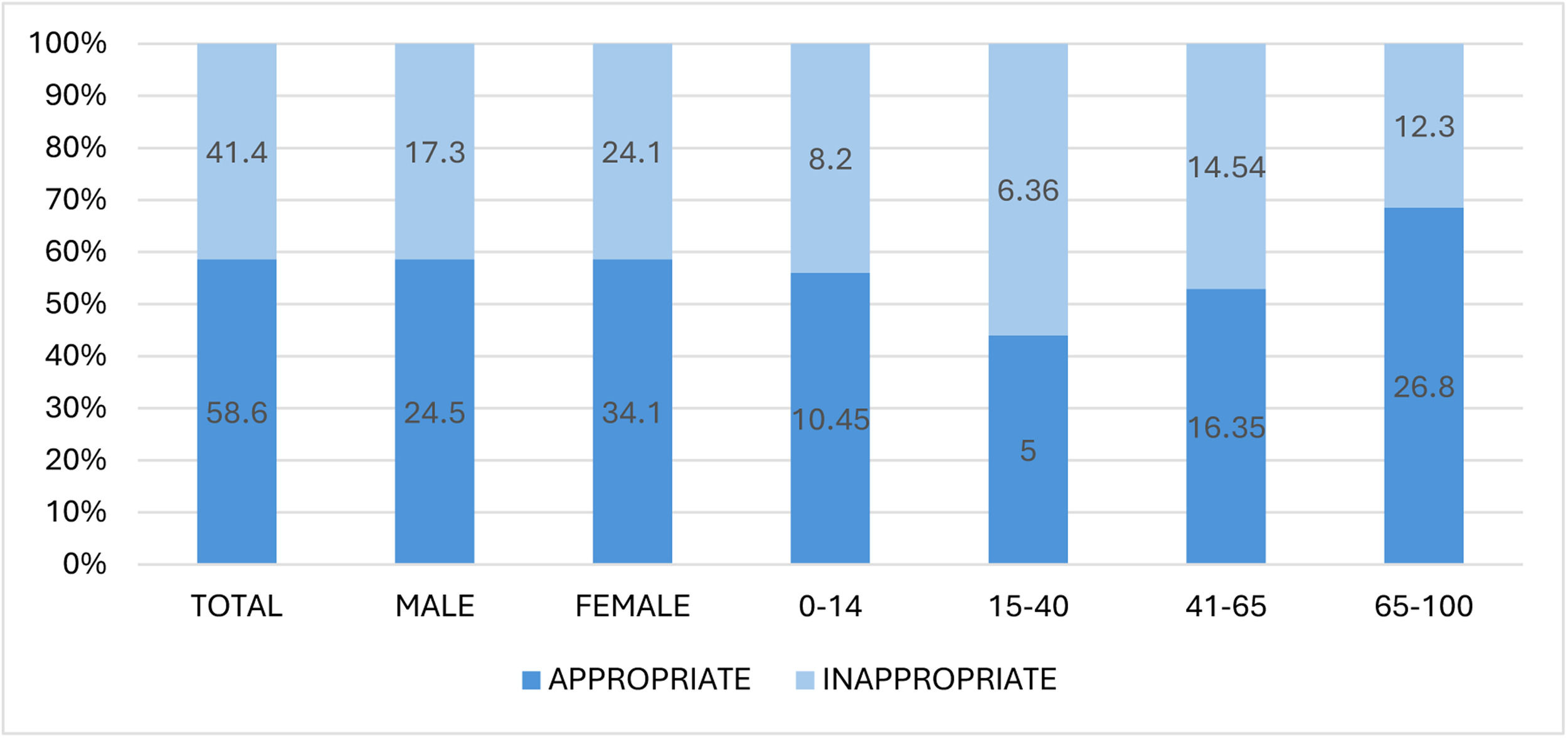
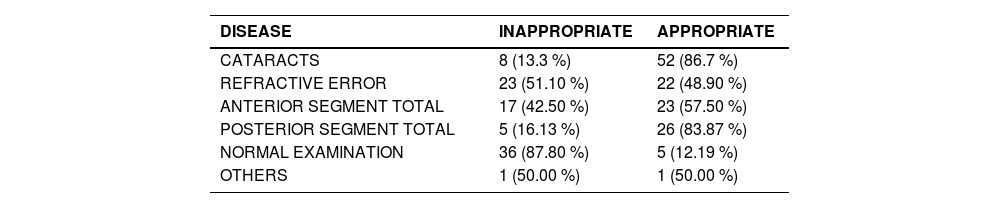
According to the criteria used by the referral ophthalmologist, 41.4 % of all referrals were inappropriate while 58.6 % were appropriate. Clearly, there is considerable room for improvement in ophthalmologic referrals. A comprehensive study of the subject is warranted.
Fig. 3 illustrates the percentages of appropriate and inappropriate consultations in the total sample and in each sex and age group. The same proportion of appropriate and inappropriate referrals is observed both in the total sample and in the categories sex (p-value = 0.899) and age (p-value = 0.145), except in the 15–40 and 65–100 age groups although the contrast is not significant. We can conclude that age and sex do not influence the appropriateness of the consultation.
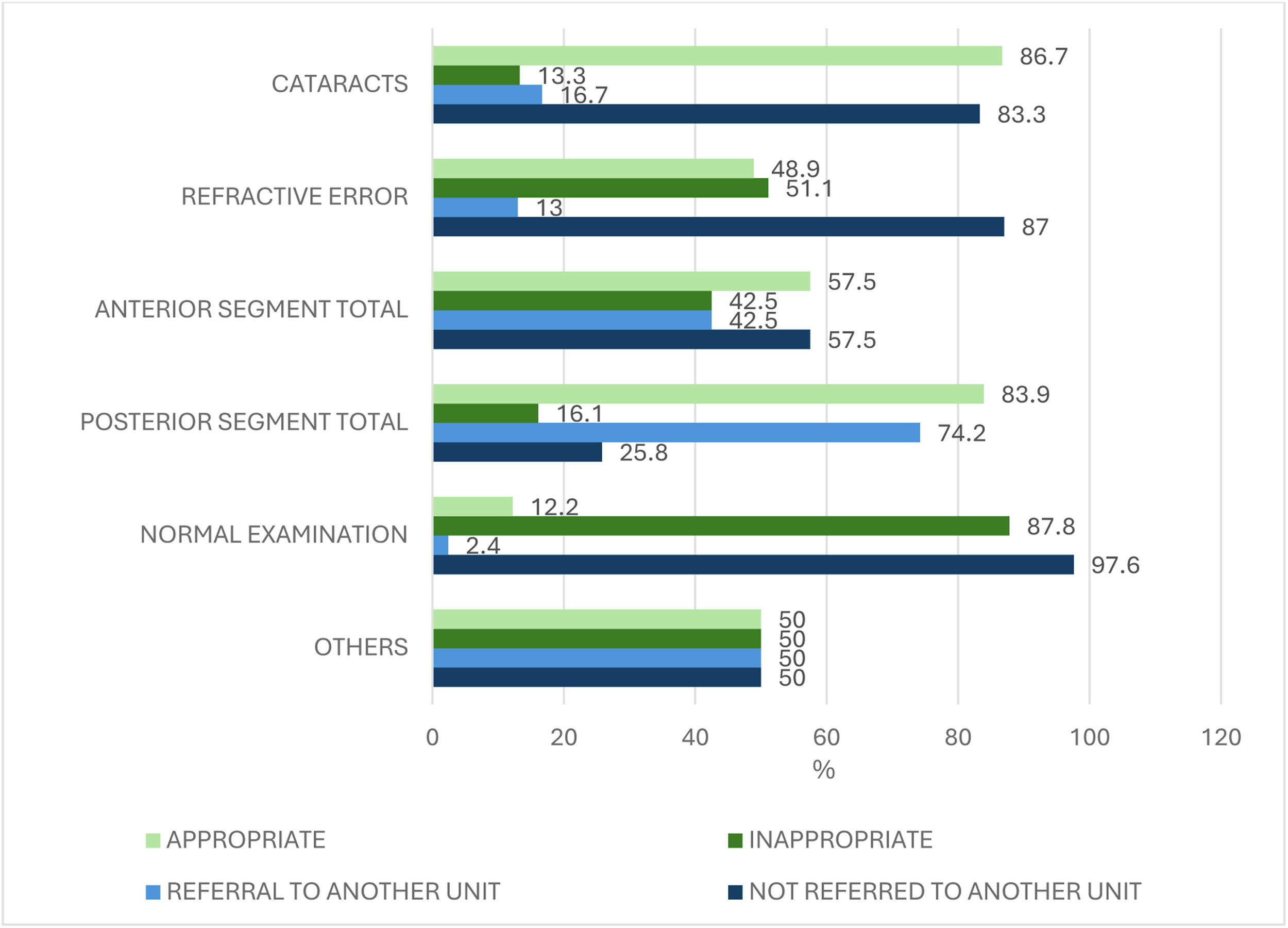
Table 2 shows for each group of conditions whether the consultation was appropriate or not. The criteria followed by the referral ophthalmologist indicate whether the patient should have remained in primary care or, conversely, should have been referred to the ophthalmology department. We observed a dependence between the percentage of consultations that were considered to be appropriate or not and the disease (p-value < 0.001), with a higher percentage of consultations considered inappropriate in normal examination and in refractive error.
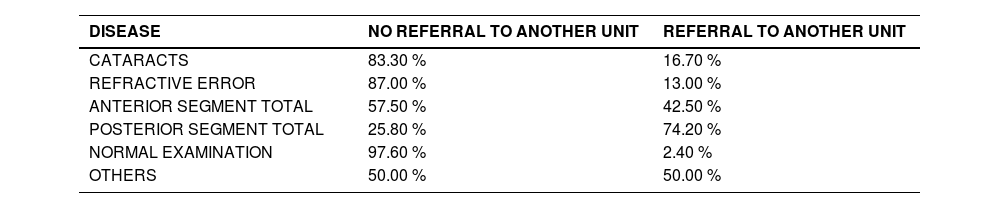
Table 3 shows for each group of conditions the percentage of patients who were referred to a specialized ophthalmology unit for treatment, termed secondary referral. The ophthalmology service is divided into specialized units. The general ophthalmologist either resolves the consultation at the first visit or refers the patient to a specialized ophthalmology unit for medical or surgical treatment of the disease. An association was found between the percentage of consultations that were not referred and those that were referred to a different unit and the disease. (p-value < 0.001), with a higher percentage of consultations referred to another unit in the posterior segment category. Pathologies of the posterior ocular pole are, in general, more serious, requiring more specific complementary tests and follow-up by a retina specialist. Hence, it is the diagnostic category that produces the most secondary referrals.
Fig. 4 shows for each group of conditions whether the consultation was appropriate or inappropriate and whether the problem was resolved in the first consultation or whether the patient was referred to another unit. The relationship between the number of consultations and secondary referrals can be seen in all the categories except in the anterior segment, where there is a greater disparity. This gives us an idea of the degree of accuracy of the primary care physician's criteria and which group of diseases should be targeted to improve referrals.
DiscussionStatistical data on referrals from primary care for diagnosed diseases, the reasons for consultation or the efficacy of referrals are scarce. The purpose of this study was to show the importance of obtaining these data. The Health Observatory in Asturias published a report in 2012 on primary care referrals, which revealed that ophthalmology was the most requested specialty. In this report, diagnoses related to visual acuity account for 50 % of referrals. This report provides data that mixes disease diagnoses with reasons for consultation and is therefore not fully comparable to our study.15
This study shows that, at least in our setting, many primary care referrals are inaccurate and others are unnecessary. Nevertheless, the sample should be expanded to improve the results. Having good statistics on referrals and diagnoses would improve the efficiency of ophthalmology service resources. Knowing which conditions are most frequently diagnosed would help to optimize personnel, their training, the necessary diagnostic equipment and investments, and the management of operating rooms and beds.
Ophthalmology specialty care is overcrowded due to excessive referrals from primary care. This may be due to the difficulty of the eye examination, lack of knowledge and measurement equipment. Primary care physicians do not have the necessary diagnostic equipment to diagnose eye diseases. Collaboration with an optometrist could be key in such a mission and unnecessary referrals could be better filtered. As indicated in Table 1, refractive errors accounted for 20.9 % of the cases in the sample studied. Additionally, as shown in Table 3, 51.1 % were consultations considered inappropriate by the referral ophthalmologist. In Spain, according to Law 44/2003, of November 21, 2003, on the Regulation of Health Professions, opticians-optometrists carry out activities related to the detection of refractive errors of the eye, by means of instrumental measurements, the use of re-education, prevention and visual hygiene techniques, and the adaptation, verification and control of optical aids. Accordingly, opticians-optometrists are qualified professionals who can benefit the public system in this task. Training primary care physicians in anterior segment diseases would also reduce the number of referrals. The equipment needed for this examination is not very sophisticated or expensive. The optician-optometrist is trained in the use of equipment such as the slit lamp that can help the primary care physician to detect and filter these anterior segment diseases.
Alabbasi et al.16 analyzed urgent ophthalmologic referrals to a reference hospital and concluded that most cases could be referred to outpatient care and treated by primary care physicians. This would improve the management of ophthalmologic emergencies.
We found several similar studies. However, they all focus on ophthalmologic emergencies. Domínguez-Serrano et al.17 studied ophthalmologic emergency visits in two tertiary hospitals in 2014 and 2015, in which 73.42 % of the visits were classified as non-urgent. The most frequent conditions were conjunctivitis (17.28 %), keratitis (15.31 %) and posterior vitreous detachment (5.37 %). The study by Schlenker et al.18 compared ophthalmologic referrals to the emergency department before and after the pandemic. The most diagnosed diseases were classified differently: anterior segment (44 %), posterior segment (23 %), neuro-ophthalmology (11 %), normal examination (8 %), oculoplasty/orbit (7 %), uveitis (5 %) and glaucoma (2 %). They do not specify which diseases are grouped in each category and, since they are emergency cases, the results cannot be extrapolated to those of our study.
Docherty et al.19 also studied emergency referrals and concluded that the most frequent diagnoses were posterior vitreous detachment (12.2 %), corneal abrasion (7.4 %) and retinal detachment (5.3 %). Alangh et al.20 determined that the five highest volume emergency diagnoses in descending order were posterior vitreous detachment/vitreous syneresis, corneal abrasion, keratitis, anterior uveitis and retinal tear/detachment.
In their 2019 study, Olthof et al.21 concluded that continuity of care for patients in primary care decreases referral rates. They stress that improvements in primary care reduce referrals. This reaffirms the idea that improving primary care conditions by collaborating with optometrists, or by providing training and equipment to physicians, can reduce referrals and improve their quality.
As a limitation of the study, it should be noted that given the high number of referrals received by the Ophthalmology Service of the Hospital Virgen Macarena, it would be of interest to further expand the sample.
ConclusionsThe sex of the patients was not a determining factor in the number of ophthalmology consultations, as it only varied by 10.45 % between the sexes, with the female population having the highest number of visits. The age group with the highest number of consultations was the over 65 years age group (38.64 %), followed by those between 40 and 65 years (31.36 %). The third most important age group was 0–14 years (18.98 %), with the highest number of referrals for refractive errors. The age group 15 to 40 years had the lowest number of visits (11.36 %). Furthermore, we can conclude that age and sex do not influence the appropriateness or inappropriateness of the consultation (see Fig. 3).
The most common diagnoses in the referrals were cataracts, followed by refractive error and normal examination (see Table 1).
We examined the appropriateness of ophthalmology consultation or referral to an ophthalmologist in each group of diseases. Our referral ophthalmologists determined whether the referral of patients from the primary care physician to the ophthalmology consultation was appropriate or inappropriate. Of the total cases reviewed, 41.36 % of the consultations were inappropriate according to the reference ophthalmologists. These cases should have been resolved in primary care.
Regarding the referrals for anterior segment diseases, 42.5 % were inappropriate (see Table 3). Examples include dry eye, blepharitis, stye and pinguecula. Of the posterior segment cases, 25.8 % were resolved in the first ophthalmologic consultation and 74.2 % required referral to a specialized unit (see Fig. 4). Anterior segment diseases should be better prioritized and primary care physicians could diagnose and treat more patients.
For refractive error referrals, only those of patients younger than 13 years of age were considered appropriate. Only 13 % of these cases were referred to another specialized unit and 87 % were resolved in the first consultation (see Fig. 4). At this point, collaboration with optometrists becomes more important as many referrals could be avoided. Opticians and optometrists are qualified professionals who can be of benefit to the public system in this role. In addition, they are trained in the use of diagnostic equipment that can assist the primary care physician in making certain diagnoses. This collaboration could prove important in the filtering of normal examinations, anterior segment diseases and incipient cataracts.
Another strategy would be to establish teleophthalmology systems with optometrists between primary care centers and specialized care centers. These systems are being successfully implemented in countries such as Australia, Denmark, Scotland and England.22-28
Concerning the cases of cataracts, only 13.3 % were inappropriate and only 16.7 % were not referred for surgery (see Fig. 4). Most cases came from primary care sufficiently advanced to undergo surgery. There appears to be good filtering in primary care.
Among the cases of patients with posterior segment diseases, we detected very few cases of AMD coming from primary care (2.72 % of the total sample). Of these, 100 % were referred to a specialized ophthalmology unit. This is a small number for the average age of the population, as Klein et al. reported that the prevalence of AMD is 9.8 percent in individuals over the age of 65.29 Very few cases of glaucoma were referred (1.26 %), a figure lower than the prevalence of the disease, which, according to Jonas et al. Tham et al. is approximately 3.5 % in people over 40 years of age.30-31 Regarding diabetic retinopathy, very few cases come from primary care. In Andalusia a telemedicine system is in place for the monitoring of diabetic patients by endocrinology specialists.
The number of new cases of posterior segment diseases is low, but these patients require many follow-up visits, such as for glaucoma, diabetic retinopathy and AMD. Referrals were appropriate in most cases.
The most common reason for consultation was blurred vision or loss of vision, comprising 43.63 % of the cases (see Fig. 1), followed by requests for refraction, strabismus testing and routine check-ups in the absence of symptoms, accounting for 62.25 % of the referrals from primary care.
It is also striking that anterior segment-related reasons represented 20.90 % of the visits, and that in 42.50 % of the anterior segment diseases diagnosed, referrals were inappropriate (see Table 3). Many anterior segment conditions are easily diagnosed because they are located in the most external and visible part of the eye and have characteristic symptoms. In addition, only basic ophthalmologic equipment is needed to diagnose many of them.
A total of 9.09 % of referrals should have been prioritized over the rest, shortening the normal time frame for care. These patients were not seen quickly enough according to their condition. Improvements are needed in primary care to identify the most urgent conditions.
Postal addresses: Department of Biochemistry and Molecular Biology, Faculty of Pharmacy, Universidad de Sevilla, España: C/ Profesor García González, n° 2, 41012 Sevilla, España.
Virgen Macarena University Hospital, Seville, Spain: Av. Dr. Fedriani, 3, 41009 Seville
Department of Economics, Quantitative Methods and Economic History, Pablo de Olavide University, Spain: Pablo de Olavide Building N°3, Conde de Floridablanca, Utrera Highway, km.1 41013 – Seville, Spain.