Specialised Independent Prescribing (IP) community optometrists provided acute eye care during the COVID-19 crisis ensuring that over-stretched hospital emergency eye care was supported, therefore local overall urgent eye care provision was not affected.
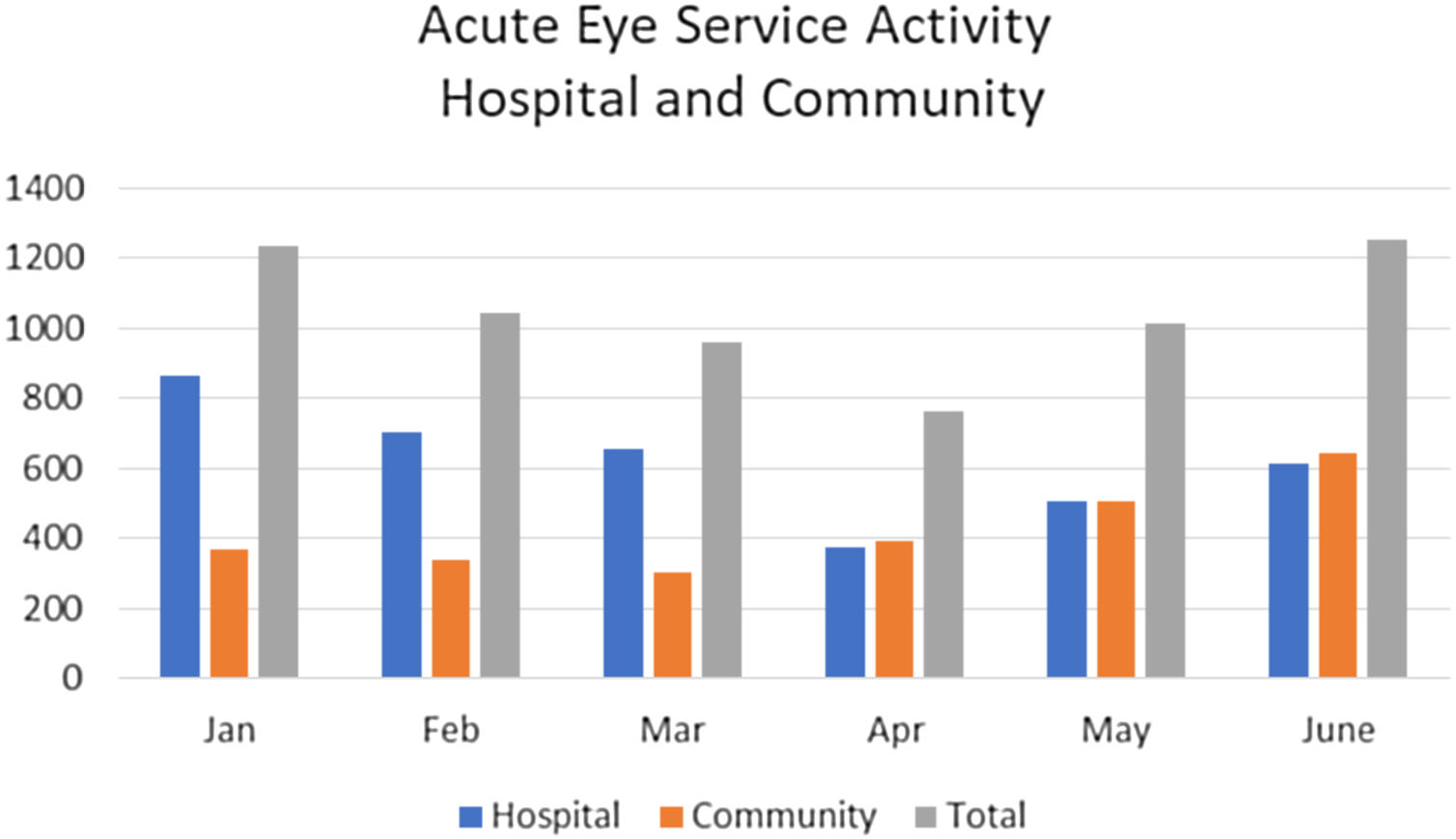
Subjects/methodsNumber of cases seen by hospital Rapid Access Clinic (RAC) between January 2020 and June 2020 were compared to number of cases seen by IP optometrists in community Acute Primary Care Ophthalmology Service (APCOS) during the same time period. Specifically, comparisons were made between the number of cases seen in RAC and the number of cases seen by APCOS during the period before COVID-19 emergency (January–March 2020) and for a similar timeframe thereafter (April–June 2020). Numbers treated by APCOS alone and those referred to RAC were also determined. The change in case numbers between the different healthcare settings was also studied.
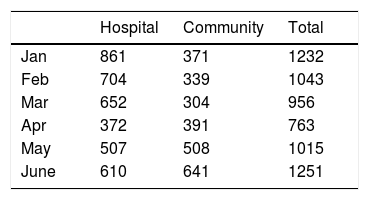
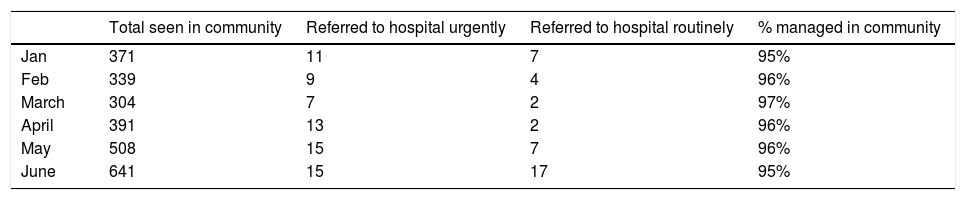
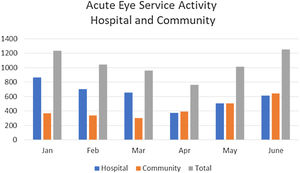
ResultsIncrease in cases seen by APCOS between April (n = 391) and June (n = 641). Number of cases seen by RAC declined from 652 in March to 372 in April, increasing to 610 by June. This was still below maximum number of monthly cases seen by RAC pre-lockdown in January (861). Most of the cases seen by APCOS were managed in the community with 4% referred to RAC.
ConclusionsOphthalmology services delivered by IP specialised optometrists can safely and efficiently treat and manage the vast majority of urgent cases and mitigate the reduced capacity within hospital emergency eye clinics. Our experience provides insights into care pathways for urgent eye cases in the future.
At the start of the COVID-19 emergency, eye departments up and down the country were faced with the challenge of providing safe and high quality eye care in a much higher risk environment. The increased risks posed by the global health threat of COVID-19 are not only to patients, but to healthcare staff, particularly those in ophthalmic units.1
The emphasis was shifted from providing mainly elective services to emergency services. The Rapid Access Clinic (RAC) at Maidstone & Tunbridge Wells NHS Trust delivers emergency eye care to a region that serves a large population of 1.2 million, with diverse demographics.
In our region (West Kent, Medway, Swale, Dartford and Gravesham, Northern Parishes of East Sussex and South East London falling within Kent), the only hospital based full-time emergency eye care service is provided by RAC, based at Maidstone Hospital, i.e. normal office hours and on-call facilities after hours, seven days a week. This department has seen a huge surge in demand over the years, but it became very clear that the traditional ways of providing such a service had to change drastically in light of the COVD-19 pandemic.
Fortunately, the department has forged very strong links with community providers since 2005. Since the inception of the Community Ophthalmology Team (COT), many suitable patients with chronic eye conditions have been repatriated to the community for onward care by specialised and highly trained optometrists and GP. From this service, the Acute Primary Care Ophthalmology Service (APCOS) was developed. This is delivered by the specialist registered therapeutic COT optometrists who hold Independent Prescribing (IP) qualifications.
We describe our experiences of re-organising the emergency eye services for our region. In particular, we discuss the lessons learnt, which have important implications on how such facilities could be delivered in the future and show that increased use of community ophthalmology services can mitigate reduced urgent eye care patient activity in the hospital eye service.
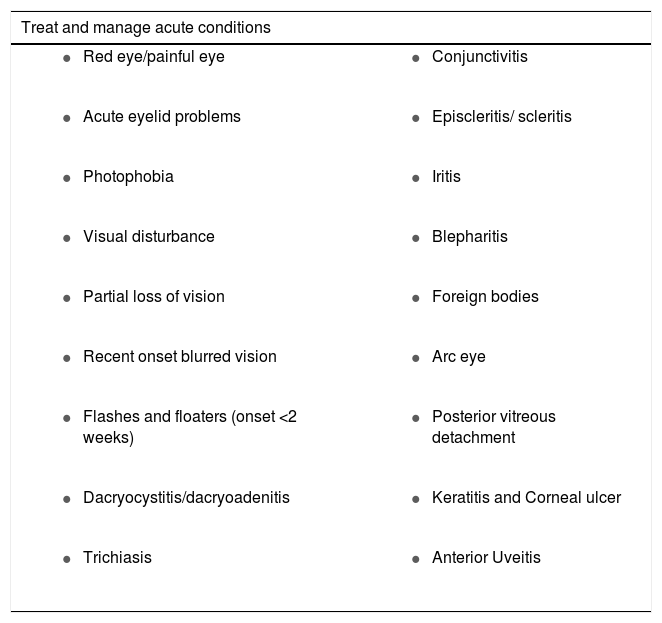
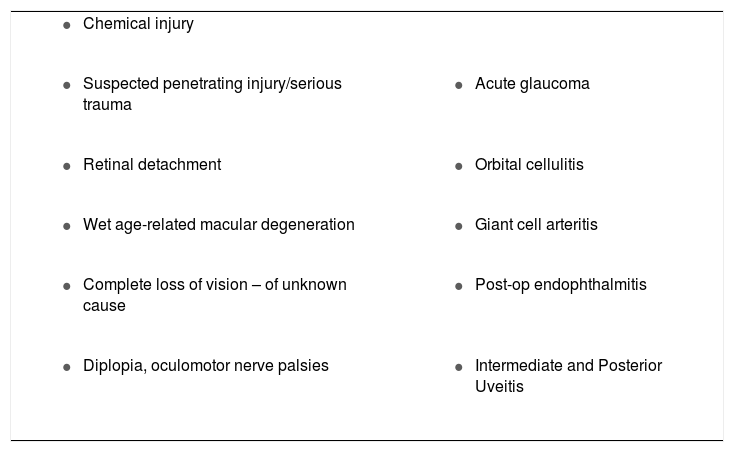
MethodsAnonymised data were collected by APCOS providers and by RAC on numbers of cases attending the service every month in the periods January–March, pre lockdown, and April–June 2020, lockdown, both inclusive. Additional data included the number of cases seen treated and discharged by APCOS and the number referred to HES (hospital eye service). The diagnosis of these cases was also recorded (Tables1 and 2). APCOS and RAC used the same diagnostic criteria.
Cases managed by APCOS.
| Treat and manage acute conditions | |
|---|---|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Cases to be referred on triage directly to RAC.
| |
|
|
|
|
|
|
|
|
|
|
RAC data was collected for the number of cases seen in the period April–June 2020 inclusive. For comparison, the same data was collected for the period January–March 2020 inclusive. These data are readily available from RAC appointment diary, paper notes and electronic notes (“e-notes”).
A dedicated e-mail receives referrals from optometrists, NHS 111, A & E, RAC and GPs. These are triaged immediately on a rota by APCOS team members and booked by a dedicated primary care booking service to the most local APCOS provider to the patient. Case types (Tables 1 and 2) not suitable for APCOS are forwarded directly to the RAC by e-mail. The APCOS triage e-mail is checked at least hourly Monday–Friday. Referrals are seen the same day, and up to 36 h to allow for Sundays off.
During the pandemic crisis, the case appointments directly attending the hospital were reviewed by a consultant ophthalmologist. These were sub-divided into phone/ video consultations and face to face consultations. The face to face consultation were limited within the hospital eye service and an increasing case load was directed towards community providers. A fast-track system is in place in the event that a case seen by APCOS is subsequently deemed to require HES assessment. The fast-track system ensures same day review in RAC for such cases.
ResultsThere was a steady increase in the number of cases seen by APCOS during the study period. This was matched by a decline in the number of cases seen by RAC. The numbers seen in RAC steadily rose in May and June, but not to the maximum pre-lockdown levels of January (Table 3). The numbers seen in the community also rose during this period of time.
Although there was a dip in the total (APCOS + RAC) cases seen in April at the start of the lockdown period, this normalised in May and June by which time pre-lockdown total case numbers were observed (Table 3; Fig. 1).
Before the lockdown period, there was a disparity between the numbers seen in RAC and in APCOS, with the majority of cases being seen in RAC. From April to June, this disparity was no longer evident with similar numbers being seen in both care settings (Fig. 1).
Between January and June, the percentage of cases managed fully in the community ranged from 95-97%. Critically, during the lockdown phase, between 95–96% were managed to resolution in the community (Table 4).
DiscussionFrom an early stage during the response to the COVD-19 pandemic, the Ophthalmology department had to maximise patient safety measures in line with Trust and national guidance.2 The particular susceptibility of ophthalmologists3,4 and of their mostly elderly patients, to infection, alerted us to augment safety measures, which included reducing the flow of people through the department. Even in the pre-COVID era, secondary hospital based settings were known to be sources of healthcare associated infections.5 Primary eye care services have robust infection control procedures in place.6,7 It was clear that a safer option to see urgent cases would be to utilise the community eye services, thereby reducing footfall in the acute hospital setting.
The Acute Primary Care Ophthalmology Service (APCOS) provided an efficient and effective means of assessing and treating urgent ophthalmology referrals outside the hospital eye service (HES). The reduced number of cases seen in HES in the wake of the COVID-19 crisis was mitigated by the increased number of cases seen in the community, i.e. the existing capacity in APCOS had margin to accommodate the extra numbers.
In comparison to the pre-lockdown period before March 23rd 2020, there was only a slight decrease in total number of cases (APCOS + HES) seen in March and April, building up to pre-lockdown levels by May. Other ophthalmology units8 and other specialities (A&E Attendances and Emergency Admissions April 2020 Statistical Commentary, NHS England) have seen patients delaying seeking emergency care. Our local service has not had this experience because of increasing acute eye care capacity in a pre-existing community ophthalmology service.
Community Ophthalmology services delivered by IP qualified therapeutic optometrists provide urgent eye care in the community following nationally agreed frameworks (Clinical Council for Eye Care Health Commissioning, November 2018). The use of specialist registered therapeutic IP optometrists within community ophthalmology services sits apart from entry level primary eye care services such as Minor Eye Care Services (MECS) or COVID-19 Urgent Eyecare Service (CUES) by empowering the IP optometrist to medically treat and manage. This allowed more urgent cases to be diverted to the community where the vast majority were seen and treated by APCOS; only 4% of cases were referred back to HES (Table 4) with all other cases manged to resolution. The performance of IP therapeutic optometrists in assessing higher risk cases has been validated previously.9
Other authors have shown that direct referrals by non-specialist optometrists into emergency ophthalmology services have poor referral efficiency.10 Our experience is that if community ophthalmology services delivered by IP specialist registered therapeutic optometrists are engaged appropriately, they can safely and efficiently treat and manage the vast majority of urgent ophthalmology cases and mitigate the reduced capacity within emergency eye clinics in hospital eye departments. This became particularly pertinent during a crisis situation that necessitated the restriction of patient traffic through the acute hospital setting.
In conclusion, previous studies have indicated that direct referrals by non-specialist optometrists into emergency ophthalmology services have poor referral efficiency. IP optometrists who have higher qualifications and the ability to prescribe, can potentially see a wider range of cases autonomously, including higher risk ones, and the performance of IP optometrists in assessing higher risk cases has been validated previously. What this study adds is that specialised IP optometrists were able to provide increased capacity for urgent eye conditions in the community, allowing HES to engage stricter safety measures in the acute hospital setting. Most acute cases seen by specialist registered IP optometrists were managed to resolution, with very few being referred onto HES; furthermore, all cases seen were unique, i.e. no patients returned with the same presentation after being treated and discharged by APCOS. This not only provided an invaluable service during the COVID-19 crisis, but also helped plan enhanced care pathways for acute cases beyond the lockdown phase.
Our experience demonstrated that extra capacity could be freed up for urgent cases in the community in a crisis situation. It also implied that this extra capacity could be utilised for the foreseeable future to direct more cases to the community setting beyond the lockdown period.
FundingThis study did not receive any funding.
Conflicts of interestThe authors have no conflict of interest to declare.
The APCOS team for providing community data.