To evaluate the changes in pupil diameter in women and men after cataract surgery. The correlation of pupillary changes with the variables age and anterior chamber depth will be analyzed.
MethodsThe values of 109 randomized eyes who underwent cataract surgery were obtained and divided into two groups, 71 women and 38 men. Pupil diameter was measured preoperatively and 3-months postoperatively using the pupillometer software of the Topolyzer Vario (Wavelight Laser Technologie AG). Anterior chamber depth was obtained with Pentacam® (Oculus). Differences in pupillary diameters were investigated and correlations with age and anterior chamber depth were analyzed.
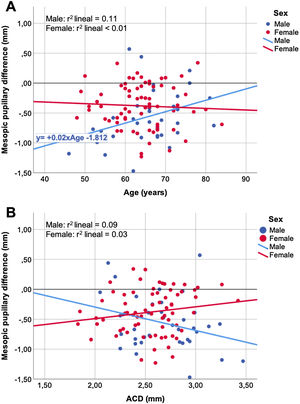
ResultsFor mesopic pupils, the male group had greater reduction in their postoperative pupillary diameter, −0.56 mm (−12.4%), than the female group, −0.38 mm (−8.2%), P = 0.025. Photopic postoperative pupils reduced to a lesser extent, yet more in men than in women (−0.11mm [−4.5%] vs. −0.04 [−1.6%], P = 0.048). Weak significant negative correlation was found between photopic pupillary changes in women with age (r = −0.24, P = 0.041), and positive correlation for mesopic pupillary changes in men with age (r = +0.34, P = 0.039).
ConclusionsPatients experience pupil reduction after cataract surgery in general, but more in men than in women and for both photopic and mesopic lighting conditions. The differences are statistically significant and have moderate clinical relevance. Concerning pupillary changes, weak but opposite sign correlations were found between male/female gender and age.
Trial registration number at ClinicalTrials.gov Identifier: NCT04286646.
Cataract surgery with an intraocular lens (IOL) implant causes a decrease in pupillary diameters and alterations in both their shape and dynamics.1–3 In patients undergoing cataract surgery, the quality of the retinal image will depend not only on the physical characteristics of the implanted IOL but also on their pupillary diameter.4 This postoperative reduction will mitigate the effects of high-order aberrations such as spherical aberration5,6 but on the other hand, it can also limit in practice the benefits of multifocal IOL implants with apodized design. Patients with a large mesopic pupil are more prone to major dysphotopsia problems, affecting more than 42% of patients.7,8 Besides, they present a loss of contrast sensitivity (SC) at high frequencies.7,9
Kanellopoulos et al.10 determined that, after surgery, pupils suffer from a relative reduction of −9.8% in photopic and −9.1% in mesopic conditions. Previous studies have shown that these changes in the pupillary diameter could be related to the increase of the anterior chamber (ACD) depth postoperatively and be more significant with the increase in the patient's age.3 Our clinical experience leads us to conceive the hypothesis that the reduction of pupillary diameters after cataract surgery does not affect the pupils to the same extent in either mesopic or photopic lighting conditions. Furthermore, we have observed that the reduction in the diameter of the postoperative pupils depends on the patient’s gender. So far, the published literature concerning the behavior of the pupil after cataract surgery have analyzed the pupil with various instruments and different lighting conditions and explored possible correlations with variables such as age and ACD.3 However, to the best of our knowledge, they have not considered yet a possible gender-related influence.
The novelty of this study is to describe the behavior of the pupils in two different populations (female and male patients that underwent cataract surgery) by evaluating the pre- and postoperative pupils in two different lighting conditions (photopic and mesopic). We have also studied the correlation of pupillary changes with the ACD and with age.
Material and methodsPatientsThis prospective single-center study included a total of 218 eyes from 109 patients with incipient to moderate cataract who underwent bilateral cataract surgery at Clínica Oftalmológica TACIR, Barcelona, Spain. An over 30-year experienced surgeon (F.C.) operated on all the patients included in the study sample. All implanted lenses were trifocal FineVision (PhysIOL, Liege, Belgium), 26% hydrophilic acrylic with double C-loop haptics. A 2.75 mm angled 45°, bevel up Short-Head Slit Knife (MANI Inc., Utsunomiya, Japan) was used to create a 2.75-mm self-sealing clear corneal incision at 180º (temporal) and about 1 mm anterior to the limbus. One eye per patient was randomly selected for the statistical analysis in this study.
The study was conducted following the institution’s Good Clinical Practices, under the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration of 1975, as revised in 1983. Informed consent was obtained from all patients at the time of data collection. The study was performed with approval from the Institutional Reviewer Board of CEIm Grupo Hospitalario Quirónsalud-Catalunya, Barcelona, Spain (ID 47/2018).
Inclusion criteria were patients of age >45 years appointed for bilateral cataract surgery. Exclusion criteria were patients using any medication that could compromise pupil size during cataract surgery. For instance, male patients taking pharmacological treatment of benign prostatic hyperplasia. Patients with pupillary and neurological disorders, diabetes mellitus, glaucoma, corneal diseases, previous corneal, or intraocular surgeries. Active ocular diseases and postoperative complications (e.g., posterior capsular opacity) during the 3-month follow-up were cause for exclusion as well.
MethodPupil diameter was measured preoperatively and 3-months postoperatively using the pupillometer software of the Topolyzer Vario (Wavelight Laser Technologie AG), a system based on the Keratograph 4 (Oculus Optikgeräte GmbH). In addition to corneal topography data, the system provides continuous images of patients’ pupils through an infrared source with central emission at 880 nm and an integrated IR-sensitive CCD camera. Data from one eye are recorded for two minutes. The pupillary response is captured three times with alternating illumination (minimum 0.7 lux and maximum brightness, 44 lux) and the set of measurements averaged by specific software. A single optometrist (E.O.M.) tested all the patients in a test room under dim light. Although the Pentacam provides the diameter of the patient's pupil, we decided to use only the data provided by the Topolyzer Vario because its lighting control system met properly the experimental requirements of the study.
Preoperatively, the ACD, defined as the distance from the corneal endothelium (posterior cornea) to the anterior lens capsule surface, was obtained using Pentacam® HR (Oculus Optikgeräte GmbH, Wetzlar, Germany), an instrument based on Scheimpflug imaging.
Statistical analysis was performed using IBM® SPSS® Statistics software version 26.0 (SPSS Inc., Chicago, Illinois, USA). Descriptive statistical results were presented as mean ± standard deviation. The normal distribution of variables was assessed with Kolmogorov–Smirnov and Shapiro–Wilk tests. The Student t-test and paired Student t-test were performed for all parameter comparisons between women and men groups and intragroup respectively. Cohen’s d was used to assess the magnitude and precision of the effect. The Pearson (r) correlation was used to evaluate in each group the relationship between postoperative pupillary changes with age and ACD in both, photopic and mesopic conditions. Since in some instances, differences in the sign of the correlation coefficients were found between the female and male groups, linear regression analysis was performed to further study the extent of the influence of these signs. All the statistical tests are two-tailed. A P < 0.05 was considered statistically significant.
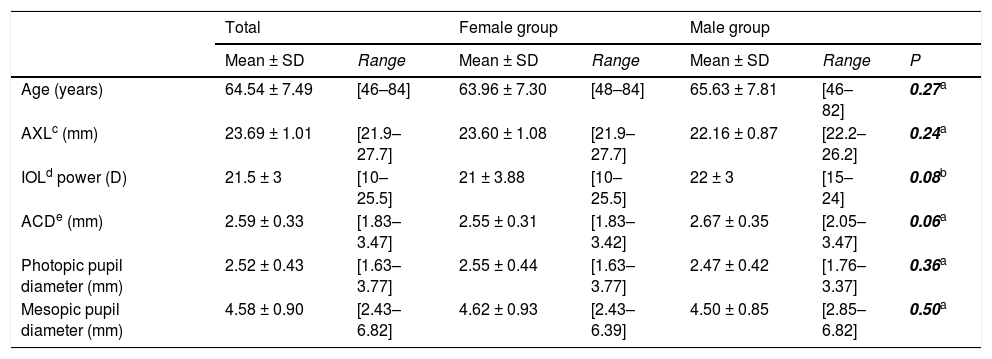
ResultsTable 1 describes the preoperative demographics of our sample. 109 patients (109 randomized eyes) participated in the study: 71 women (65%) and 38 men (29%). No statically significant differences were observed preoperatively in any of the variables between the two groups.
Demographic and preoperative data of the total sample (n = 109) and segmented by groups: female group (n = 71) and male group (n = 38).
| Total | Female group | Male group | |||||
|---|---|---|---|---|---|---|---|
| Mean ± SD | Range | Mean ± SD | Range | Mean ± SD | Range | P | |
| Age (years) | 64.54 ± 7.49 | [46–84] | 63.96 ± 7.30 | [48–84] | 65.63 ± 7.81 | [46–82] | 0.27a |
| AXLc (mm) | 23.69 ± 1.01 | [21.9–27.7] | 23.60 ± 1.08 | [21.9–27.7] | 22.16 ± 0.87 | [22.2–26.2] | 0.24a |
| IOLd power (D) | 21.5 ± 3 | [10–25.5] | 21 ± 3.88 | [10–25.5] | 22 ± 3 | [15–24] | 0.08b |
| ACDe (mm) | 2.59 ± 0.33 | [1.83–3.47] | 2.55 ± 0.31 | [1.83–3.42] | 2.67 ± 0.35 | [2.05–3.47] | 0.06a |
| Photopic pupil diameter (mm) | 2.52 ± 0.43 | [1.63–3.77] | 2.55 ± 0.44 | [1.63–3.77] | 2.47 ± 0.42 | [1.76–3.37] | 0.36a |
| Mesopic pupil diameter (mm) | 4.58 ± 0.90 | [2.43–6.82] | 4.62 ± 0.93 | [2.43–6.39] | 4.50 ± 0.85 | [2.85–6.82] | 0.50a |
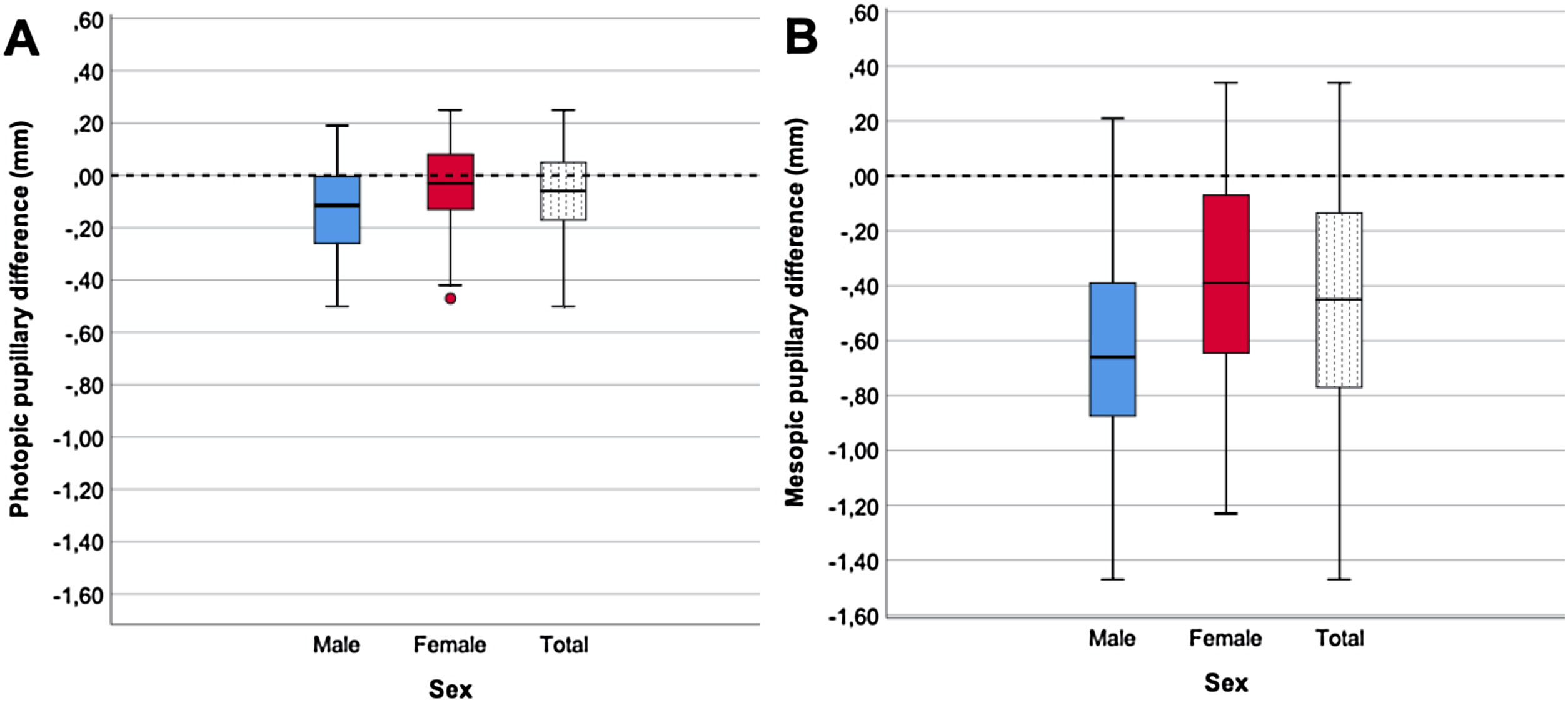
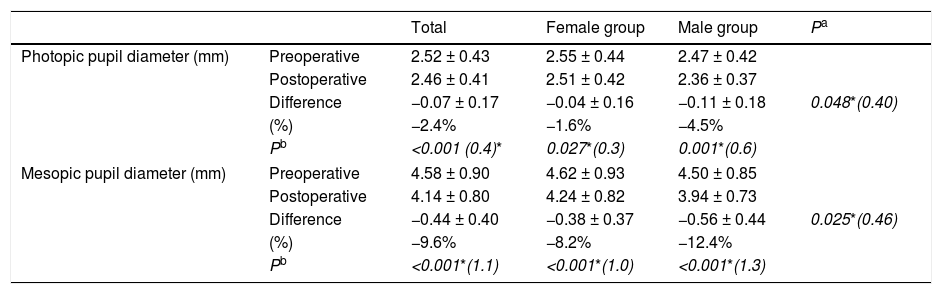
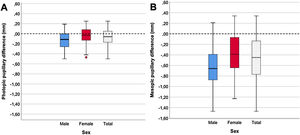
The photopic and mesopic (pre and postoperative) pupil diameters and the resultant pupillary changes are shown in Table 2. Pupillary postoperative changes are shown in Fig. 1. For photopic and mesopic pupils and all the groups (total, women and men), the results show that there was a statically significant reduction of the postoperative pupil diameter.
Pre- postoperative pupil diameter change for photopic and mesopic pupils of the total sample (n = 109) and segmented by groups: female group (n = 71) and male group (n = 38).
| Total | Female group | Male group | Pa | ||
|---|---|---|---|---|---|
| Photopic pupil diameter (mm) | Preoperative | 2.52 ± 0.43 | 2.55 ± 0.44 | 2.47 ± 0.42 | |
| Postoperative | 2.46 ± 0.41 | 2.51 ± 0.42 | 2.36 ± 0.37 | ||
| Difference | −0.07 ± 0.17 | −0.04 ± 0.16 | −0.11 ± 0.18 | 0.048*(0.40) | |
| (%) | −2.4% | −1.6% | −4.5% | ||
| Pb | <0.001 (0.4)* | 0.027*(0.3) | 0.001*(0.6) | ||
| Mesopic pupil diameter (mm) | Preoperative | 4.58 ± 0.90 | 4.62 ± 0.93 | 4.50 ± 0.85 | |
| Postoperative | 4.14 ± 0.80 | 4.24 ± 0.82 | 3.94 ± 0.73 | ||
| Difference | −0.44 ± 0.40 | −0.38 ± 0.37 | −0.56 ± 0.44 | 0.025*(0.46) | |
| (%) | −9.6% | −8.2% | −12.4% | ||
| Pb | <0.001*(1.1) | <0.001*(1.0) | <0.001*(1.3) | ||
More in detail, in the case of the photopic pupil, the reduction was slight on average (−0.07 mm, equivalent to −2.4%), even though was relatively larger for men (−0.11 mm, −4.5%, P = 0.001) than for women (−0.04 mm, −1.6%, P = 0.027). When these differences were analyzed between the women and men groups, they showed a statistical significance (P = 0.048), with a size effect Cohen’s d = 0.40.
For mesopic pupils, the results showed, on average, larger reduction of the postoperative pupil diameter (−0.44 mm, equivalent to −9.6%) than in the photopic condition. The reduction appeared both in the women group (−0.38 mm, −8.2%, P < 0.001) as well as in the men group (−0.56 mm, −12.4%, P < 0.001). Notice that again, the largest reduction occurred in the men group, and in this pupil condition, the differences between the two groups reached clear statistical significance (P = 0.025, Cohen’s d = 0.46).
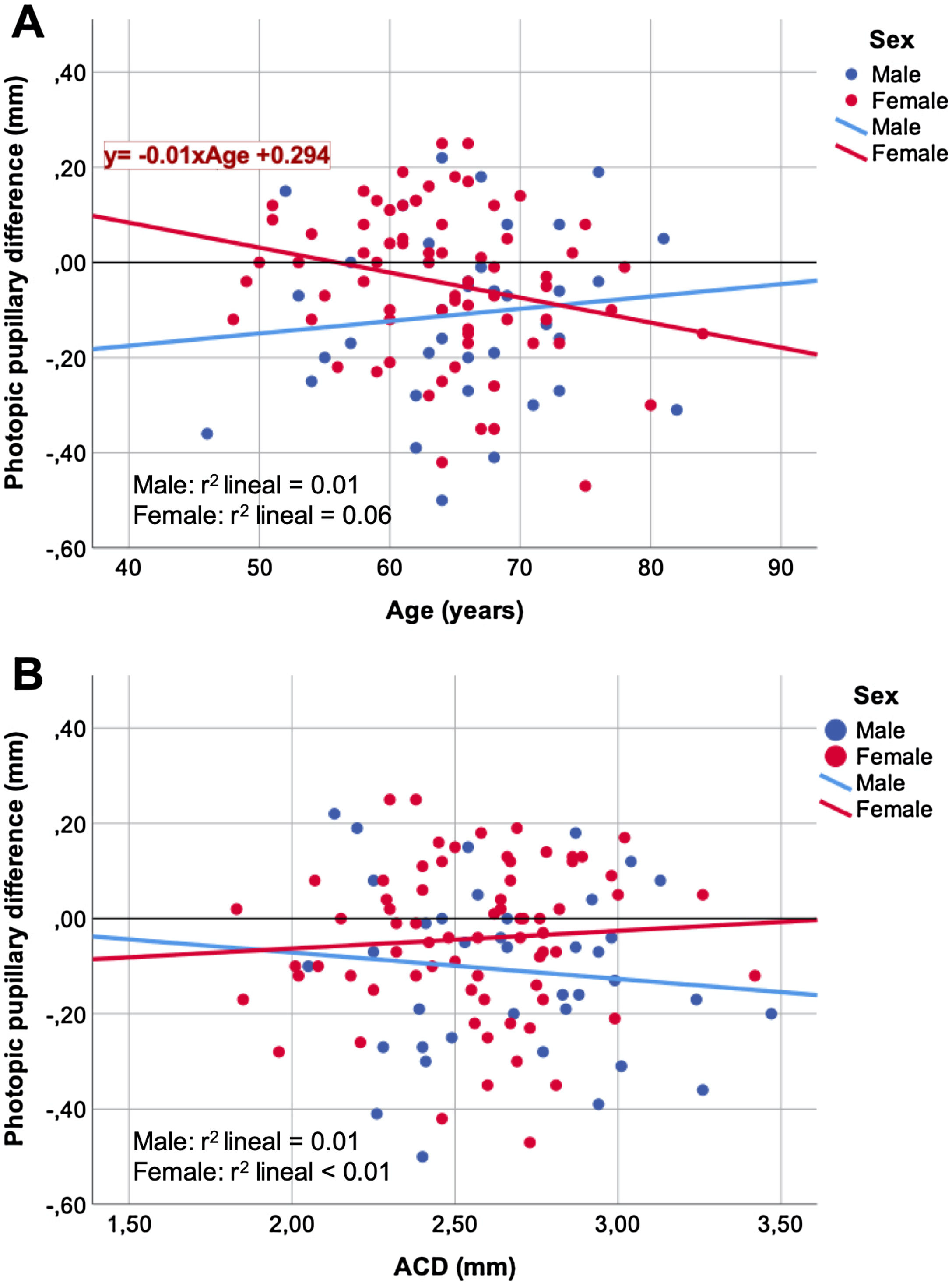
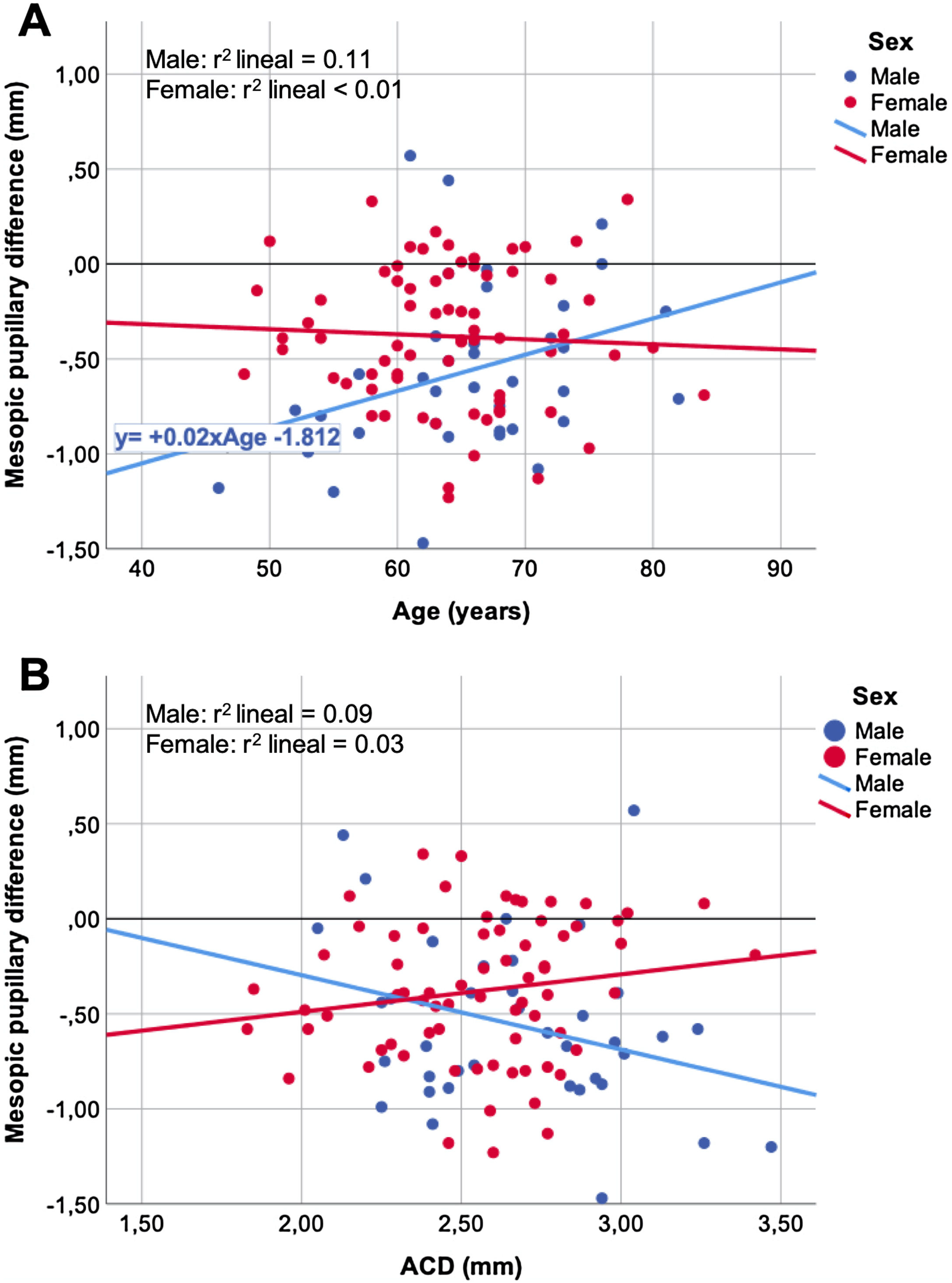
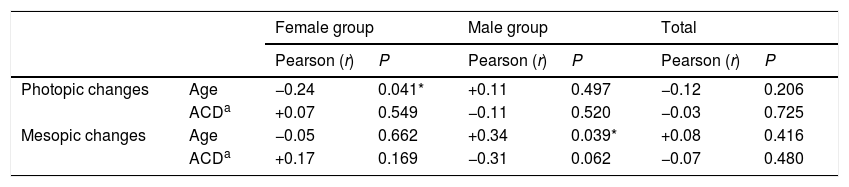
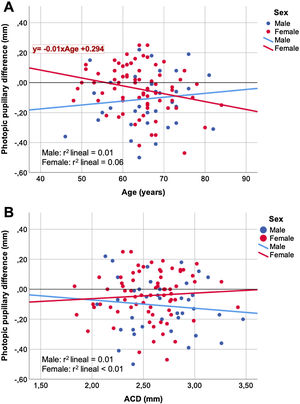
Table 3shows the correlation between pupillary changes after cataract surgery and the variables age and ACD. Again, gender-related differences appeared: a weak significant negative correlation was found between photopic pupillary changes in women with age (r = −0.24, P = 0.041, r2 = 0.06) and a positive correlation for mesopic pupillary changes in men with age (r = +0.34, P = 0.039, r2 = 0.11).
Pearson's correlation between photopic and mesopic pupillary changes with variables age and ACD of the total sample (n = 109) and segmented by groups: female group (n = 71) and male group (n = 38).
Figs. 2 and 3 show the correlation between the changes in the photopic (Fig. 2) and mesopic (Fig. 3) pupils that occurred after cataract surgery with the variables age (Figs. 2A, 3A) and ACD (Figs. 2B, 3B). In the scatter plots, the straight lines obtained by a linear regression fit tended to have opposite behavior between the women and men groups.
The literature published so far has not considered a possible sex-related difference in the pupil change after cataract surgery. As shown in Table 1, the sample studied was sorted into two groups segmented by sex. Both groups were quite homogeneous in terms of age, ACD, and preoperative photopic and mesopic pupillary diameter, without finding statistically significant differences.
When the results of the total group (i.e. men and women) are analyzed, our findings are consistent with many other studies that have reported a decrease in pupil diameter after cataract surgery.1–3,10–16 In particular, we have found that the average photopic pupil suffered a slight reduction of −0.07 mm (−2.4%) and the average mesopic pupil a larger reduction of −0.44 mm (−9.6%) (Table 2). The effect size reached by the mesopic pupils (Cohen's d = 1.1) is interpreted as a substantial clinical change. However, the effect size of the changes in the photopic pupil diameter, although statistically significant, involves a medium-low clinical change (Cohen's d = 0.4).17,18
These changes in the pupil size have been explained from the increased depth and volume of the anterior chamber caused by the natural lens removal and replacement by a thinner IOL. As a matter of fact, the natural crystalline is approximately 4.4 mm thick and an IOL approximately 1 mm.19 A thin IOL allows greater space and freedom of movement to the iris constrictor muscles, which would be able to reduce further the pupil size. Furthermore, after cataract surgery, it has been reported that the ipRGC retinal ganglion cells responsible for the pupillary reflex react more efficiently due to increased stimulus area and retinal intensity, which could cause the pupil to respond more effectively.20–22
So, it is generally accepted that after cataract surgery there is a decrease in pupillary diameters in different lighting conditions, but there are discrepancies between the values reported by different studies. The variability in the results obtained when comparing different studies could be explained from the different instruments and technology used in the measurement of the pupils, which not always are very precise.3 These differences could increase the variability observed in the pupil reduction (shrinking). For example, Koch et al.,12 who used a photographic system, suggested that these changes were approximately −0.5 mm in five lighting situations whereas Kanellopoulos et al.,10 using a more precise measuring instrument, the Topolyzer Vario, determined that the photopic pupil was reduced −0.28 ± 0.14 mm (−9.8%) and the mesopic −0.43 ± 0.25 mm (−9.1%).
The Topolyzer Vario is an instrument that measures corneal topography and pupillary reflex. Salah-Mabed et al.23 studied the instrument's reliability, showing excellent repeatability when measuring the pupil's dynamic parameters obtaining an ICC (intraclass correlation coefficient) value greater than 0.9. Despite having used the same instrument as Kanellopoulos,10 our outcomes are partially concordant. Both studies agree that the size of the mesopic pupil experiences a relative reduction of approximately −9% on average. However, for the photopic pupils, they obtained a −9.8% in contrast to our results −2.4%.
When the results are analyzed by sorting out the patient sample according to sex (Table 2 and Fig. 1), it was observed that, with a photopic pupil, the female group suffered a little decrease in the diameter of −0.04 mm (−1.6%) while in the male group the reduction was greater in absolute and percentage terms (−0.11 mm, −4.5%). The pupil size change in the male group was almost three times bigger than in the female group, and this change was statistically significant with P = 0.048 and a side effect Cohen’s d = 0.40. With the mesopic pupil, the pupils of men also experienced a greater reduction in their pupil diameter −0.56 mm (−12.4%) compared to that of the women group −0.38 mm (−8.2%), P = 0.025. Even though such a difference was statistically significant, the effect size of these changes is moderate (Cohen's d = 0.46).
Although the nervous system (regulator of pupillary size) is independent of the endocrine, they often work together to help the body function properly. We know that the endocrine system is different in men and women. Therefore, different hormonal changes (menopause/andropause) existing between the sexes, could justify the difference found between the groups.
Looking at the dot plots of the post-surgery pupillary changes versus age (Figs. 2A, 3A) and ACD (Figs. 2B, 3B) variables, the trend of linear adjustment between women and men tend to have opposite sign slopes. Although there is no strong relationship (low r2 coefficients), the different trends of the linear adjustment slopes could explain the variability between the results obtained by different studies, which will be dependent not only on the women-men ratio but also influenced by the age of the sample.
According to the results in Table 3, the age of the patients is the only variable significantly related to the change in the diameter of the pupils after surgery. However, since the ACD in the male and female groups was close to statistical significance (P = 0.06 in Table 1), we prudently ponder the tendencies shown by the results obtained concerning ACD and recommend further study in the future concerning this biometric parameter.
Our study demonstrates a weak negative correlation between changes in women photopic pupils with age r = −0.24 (Table 3). It means that the older the patient, the greater the expected photopic pupillary change after surgery (Fig. 2A). Although we have not found statistical significance, the trend for changes in men's photopic pupils appears to be the opposite, that is, the older the patient, the smaller the expected pupil photopic change. Apart from that, we have found a weak degree of a positive correlation between men mesopic pupillary changes and age, r = 0.34. It seems that the older the patient, the lesser the pupillary change expected after surgery (Fig. 3A).
Regarding the methodology used in this study, it would have been advisable to include age and gender control groups. For example, adequate pupillary data could have been obtained three months apart in a control cohort of cataract patients who had not undergone eye surgery during that period. This fact would have reinforced the findings found. Another limitation of this study is that there is no ideal 1:1 relationship between the groups because the sample was recruited through a continuous series of patients. To mitigate the potential effect of this fact on the results, we applied an additional statistic (Cohen's d), which points beyond the statistical significance of the P-value,18 minimizes the difference between the proportions of the group and shows the effect size (that is, the magnitude of the difference between groups).17,24
This study's findings open new lines for future research, particularly on their clinical implications (e.g., the influence of detected pupillary changes on the visual acuity and dysphotopsia phenomena).
In conclusion, the results of this study derived from our clinical experience, show that men have a greater reduction in pupil diameter than women after cataract surgery in both photopic and mesopic conditions. Changes in the diameter of the men pupils are up to three times as much as that of the women pupils. And these differences are not only statistically significant but have moderate clinical relevance. Furthermore, changes in the photopic pupillary diameter of women and mesopic pupillary changes of men are weakly correlated with the age of the patients.
FundingThis work was supported by the Spanish Ministerio de Economía y Competitividad and FEDERfunds under project Ref. DPI2016-76019-R.
Conflicts of interestThe authors have no conflicts of interest to declare.