Phakic intraocular lenses (pIOL) are the main treatment for patients who have either high ametropia or contraindications for laser refractive surgery. The main feature that makes this kind of lenses suitable for its implantation in young adults searching for independence of optical prescription is the conservation of accommodation, since lens extraction is not required. A systematic review has been performed to evaluate the scientific literature on the effect of pIOL implantation on accommodation. Critical assessment of the articles included in the review was achieved using the tool Critical Appraisal Skills Programme in its Spanish form (CASPe). After revising the complete text of 10 articles pre-selected, two quasi-experimental pre-post studies evaluating the outcomes of a specific model of posterior chamber pIOL were included in the systematic review. The CASPe scoring of both studies were 5/11. According to this outcome, the evidence describing the impact of the pIOL implantation on the accommodative function can be defined poor. Some trends are reported as the decrease in the amplitude of accommodation, a decrease positive relative accommodation and improvement of accommodation. However, these results should be confirmed in future controlled studies.
Las lentes intraoculares fáquicas (pIOL) son el tratamiento principal para aquellos pacientes con ametropía o contraindicaciones para la cirugía refractiva con láser. La característica principal que hace que este tipo de lentes sean adecuadas para su implantación en adultos jóvenes, que buscan independencia de la prescripción óptica, es la conservación de la acomodación, ya que la extracción de las lentes no es necesaria. Se ha realizado una revisión sistemática para evaluar la literatura científica relativa al efecto sobre la acomodación de la implantación de pIOL. La valoración crítica de los artículos incluidos en la revisión se consiguió utilizando el Programa Critical Appraisal Skills en su versión española (CASPe). Tras revisar el texto completo de 10 artículos pre-seleccionados, se incluyeron en la revisión sistemática dos estudios cuasi-experimentales pre-post que evaluaban los resultados de un modelo específico para pIOL de cámara posterior. La puntuación CASPe de ambos estudios fue de 5/11. Con arreglo a este resultado, la evidencia que describe el impacto de la implantación de pIOL sobre la función acomodativa puede definirse como débil. Se reportaron algunas tendencias como la disminución de la amplitud de la acomodación, la disminución de la acomodación relativa positiva y la mejora de la acomodación. Sin embargo, estos resultados deberían confirmarse en futuros estudios controlados.
Phakic intraocular lenses (pIOL) are the main treatment for patients who have either high ametropia or contraindications for laser refractive surgery. This sort of surgical procedure has been proved to be safe and effective with a low rate of complications.1–4 Furthermore, this refractive correction option became more important in the last years due to the increase of myopic population. At the same time, it is an important field of research in view of future estimations of prevalence of simple myopia and, above all, severe myopia.5 Aesthetic and optical limitations of traditional ophthalmic lenses, and the trend towards the abuse of contact lenses make pIOLs an appropriate treatment for patients with severe myopia. In addition, the limitations of the laser refractive surgery in these patients, such as the risk of corneal ectasia because of an inadequate postsurgical stroma6 and the increase of high order aberrations (HOAs), which is proportional to the ametropia treated, should be considered.7 Although pIOLs have some advantages in relation to laser refractive surgery (better optical quality in high ametropias, wider range of correction, reversibility, etc.), it should be considered that it is a surgical procedure with normal risks associated with intraocular surgeries, including severe complications such as endophthalmitis.
PIOLs can be classified into two groups depending on where the lens is located: anterior chamber and posterior chamber pIOLS.8,9 Effectiveness and safety of both types are similar when the anterior chamber iris-fixed pIOL and posterior chamber pIOL are compared, though the latter have higher predictability1 and better aesthetics.
The main feature that makes this kind of lenses suitable for its implantation in young adults searching for independence of optical prescription is the conservation of accommodation, since lens extraction is not required. However, scientific literature is limited with regard to the accommodative function after implantation of pIOLs and very few studies analyze it from a clinical point of view. Therefore, the aim of this study is to perform a systematic review on the effect of pIOL implantation on accommodation.
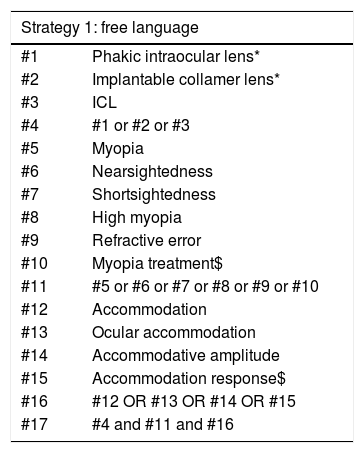
MethodThree searching strategies were used (Table 1) in four different databases: PubMed, Web of Science, Scopus and ProQuest. For that purpose, there were neither temporal restriction nor source of information or type of article during the search. Next, the following inclusion criteria were applied in the article selection:
- •
Original articles aimed at evaluating the accommodative function in patients who underwent refractive surgery with pIOL
- •
Any type of study
- •
Articles in English or Spanish
- •
Any type of population
Search strategies used in our systematic review.
| Strategy 1: free language | |
|---|---|
| #1 | Phakic intraocular lens* |
| #2 | Implantable collamer lens* |
| #3 | ICL |
| #4 | #1 or #2 or #3 |
| #5 | Myopia |
| #6 | Nearsightedness |
| #7 | Shortsightedness |
| #8 | High myopia |
| #9 | Refractive error |
| #10 | Myopia treatment$ |
| #11 | #5 or #6 or #7 or #8 or #9 or #10 |
| #12 | Accommodation |
| #13 | Ocular accommodation |
| #14 | Accommodative amplitude |
| #15 | Accommodation response$ |
| #16 | #12 OR #13 OR #14 OR #15 |
| #17 | #4 and #11 and #16 |
| Strategy 2: controlled vocabulary (MeSH terms) | |
|---|---|
| #1 | "Phakic Intraocular Lenses"[Mesh] |
| #2 | "Myopia"[Mesh] |
| #3 | "Refractive Errors"[Mesh] |
| #4 | "Accommodation, Ocular"[Mesh] |
| #5 | #1 and #2 and #3 and #4 |
| Strategy 3: free language search used in Scopus | |
|---|---|
| #1 | “Phakic intraocular lens” |
| #2 | “Implantable collamer lens” |
| #3 | ICL |
| #4 | #1 or #2 or #3 |
| #5 | Myopia |
| #6 | Nearsightedness |
| #7 | Shortsightedness |
| #8 | “High myopia” |
| #9 | “Refractive error” |
| #10 | “Myopia treatment” |
| #11 | #5 or #6 or #7 or #8 or #9 or #10 |
| #12 | Accommodation |
| #13 | “Ocular accommodation” |
| #14 | “Accommodative amplitude” |
| #15 | “Accommodation response” |
| #16 | #12 or #13 or #14 or #15 |
| #17 | #4 and #11 and #16 |
Article selection was carried out in some steps. First, titles and abstracts were reviewed for excluding those which were not relevant for this study; next, duplicates were excluded too. Second, complete texts were downloaded for their review, selecting only those documents which comply with inclusion criteria and answer the research question. Third, manual search was done to obtain references that might have not appeared during the first step.
Finally, a critical assessment of the included articles was achieved using the tool Critical Appraisal Skills Programme in its Spanish form (CASPe) for evaluating the quality of the studies and their risk of bias.10 It should be pointed out that there were only two quasi-experimental pre-post studies after revising all the peer-reviewed literature. CASPe did not have a specific tool for evaluation of this type of studies and we decided to use the clinical trial instrument as recommended but for the quasi-experimental pre-post studies obtained.
First documentary search was carried out on 24 January 2018, and databases were reviewed again on 11 July 2018 applying the same method, not finding any new article.
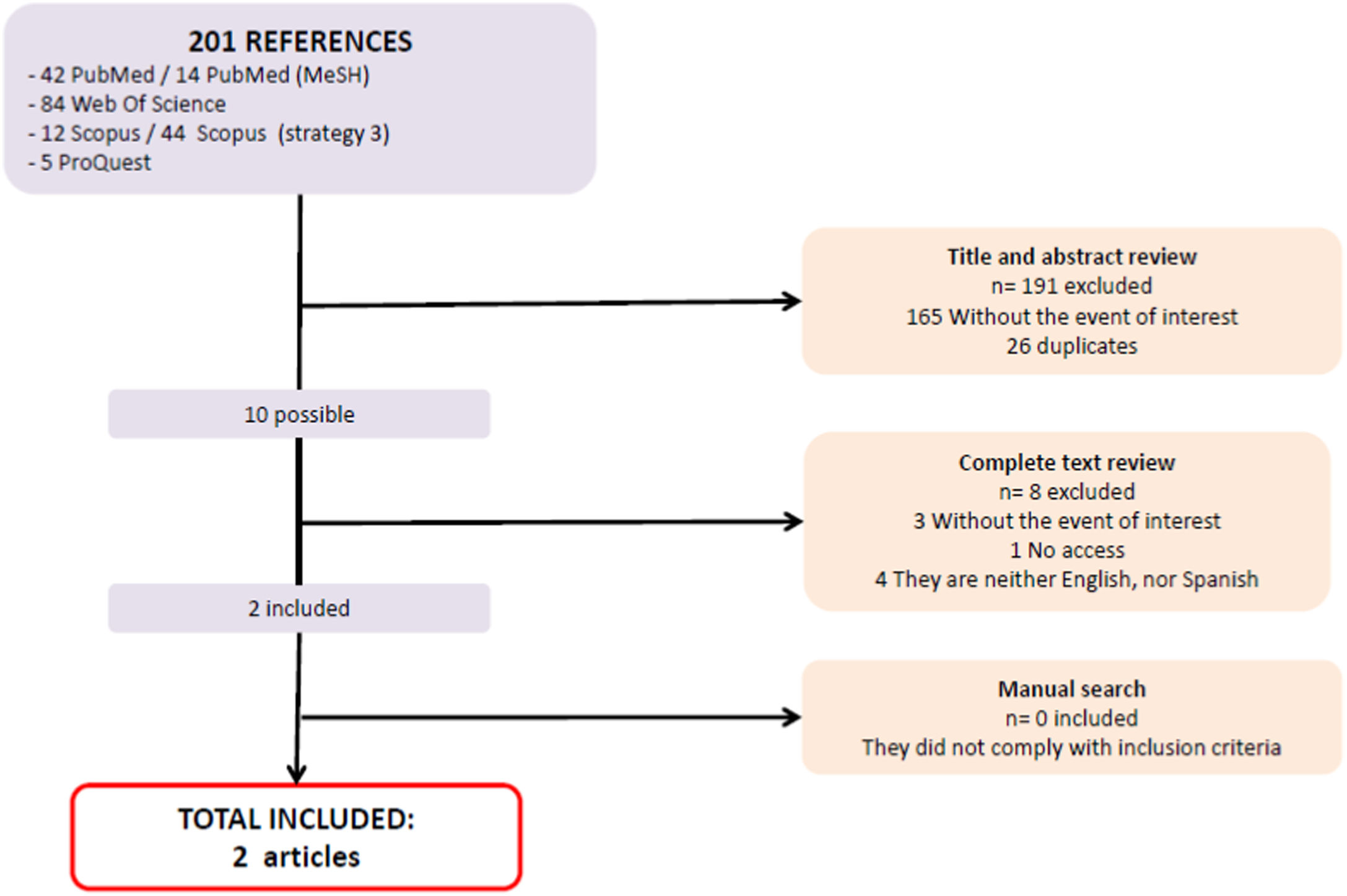
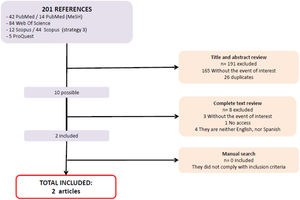
ResultsSearch resultsIn the search, 201 documents were obtained. After reviewing titles, abstract and dismissing duplicates, only 10 articles were included for complete text reading.11–20 A total of 8 out of 10 of those articles were excluded because they did not meet the inclusion criteria. Finally, two remaining articles were included, and an additional manual search was carried out, but no more references were found (Fig. 1). The two articles selected evaluate changes in the accommodative function after implantation of the posterior chamber pIOL Implantable Collamer Lens (ICL, Staar Surgical, Monrovia, CA, USA).
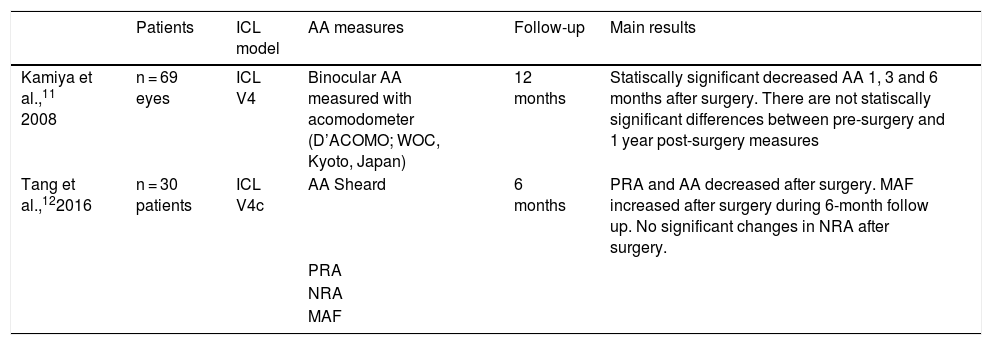
Included studiesMain aspects of the two studies selected are summarized in Table 2.
Articles included in the current systematic review.
| Patients | ICL model | AA measures | Follow-up | Main results | |
|---|---|---|---|---|---|
| Kamiya et al.,11 2008 | n = 69 eyes | ICL V4 | Binocular AA measured with acomodometer (D’ACOMO; WOC, Kyoto, Japan) | 12 months | Statiscally significant decreased AA 1, 3 and 6 months after surgery. There are not statiscally significant differences between pre-surgery and 1 year post-surgery measures |
| Tang et al.,122016 | n = 30 patients | ICL V4c | AA Sheard | 6 months | PRA and AA decreased after surgery. MAF increased after surgery during 6-month follow up. No significant changes in NRA after surgery. |
| PRA | |||||
| NRA | |||||
| MAF |
AA = amplitude of accommodation.
PRA = positive relative accommodation.
NRA = negative relative accommodation.
MAF = monocular accommodation facility.
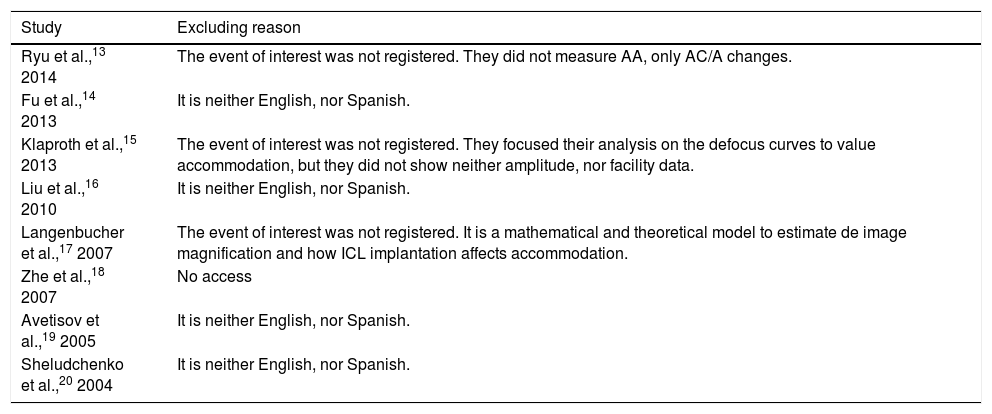
A total of 8 articles were excluded after the complete text review. Excluding reasons are described in Table 3.
Articles excluded in the current systematic revew.
| Study | Excluding reason |
|---|---|
| Ryu et al.,13 2014 | The event of interest was not registered. They did not measure AA, only AC/A changes. |
| Fu et al.,14 2013 | It is neither English, nor Spanish. |
| Klaproth et al.,15 2013 | The event of interest was not registered. They focused their analysis on the defocus curves to value accommodation, but they did not show neither amplitude, nor facility data. |
| Liu et al.,16 2010 | It is neither English, nor Spanish. |
| Langenbucher et al.,17 2007 | The event of interest was not registered. It is a mathematical and theoretical model to estimate de image magnification and how ICL implantation affects accommodation. |
| Zhe et al.,18 2007 | No access |
| Avetisov et al.,19 2005 | It is neither English, nor Spanish. |
| Sheludchenko et al.,20 2004 | It is neither English, nor Spanish. |
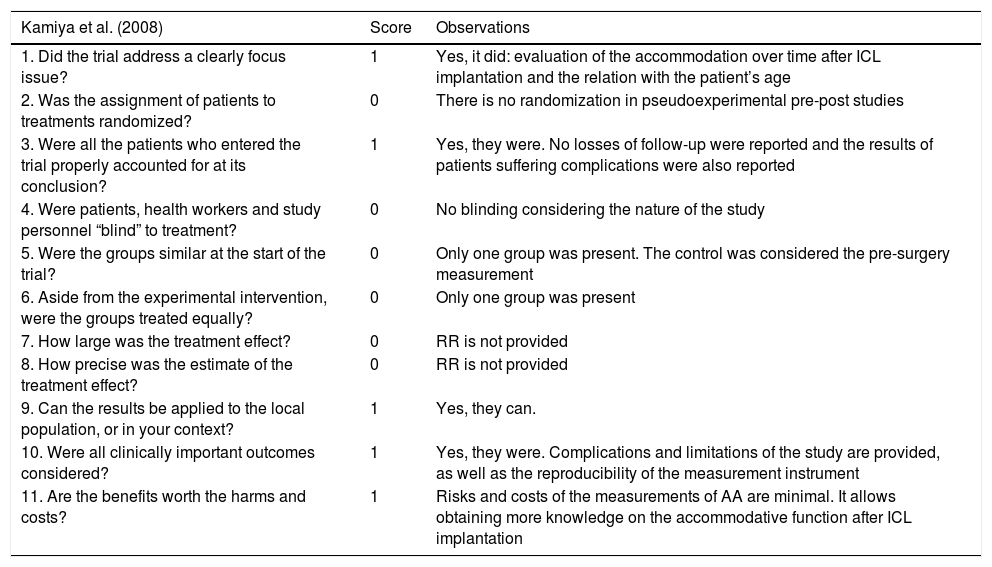
It cannot be calculated since no randomized clinical trials describing the event of interest were found. Likewise, articles analyzing the relative risk were not found either. Concerning the scoring of CASPe analysis, a value of 5/11 was obtained for the two articles included in the review (Tables 4 and 5).
Evaluation of the quality of the study «Time course of accommodation after implantable collamer lens implantation» (Kamiya, 2008) with the CASPe tool.
| Kamiya et al. (2008) | Score | Observations |
|---|---|---|
| 1. Did the trial address a clearly focus issue? | 1 | Yes, it did: evaluation of the accommodation over time after ICL implantation and the relation with the patient’s age |
| 2. Was the assignment of patients to treatments randomized? | 0 | There is no randomization in pseudoexperimental pre-post studies |
| 3. Were all the patients who entered the trial properly accounted for at its conclusion? | 1 | Yes, they were. No losses of follow-up were reported and the results of patients suffering complications were also reported |
| 4. Were patients, health workers and study personnel “blind” to treatment? | 0 | No blinding considering the nature of the study |
| 5. Were the groups similar at the start of the trial? | 0 | Only one group was present. The control was considered the pre-surgery measurement |
| 6. Aside from the experimental intervention, were the groups treated equally? | 0 | Only one group was present |
| 7. How large was the treatment effect? | 0 | RR is not provided |
| 8. How precise was the estimate of the treatment effect? | 0 | RR is not provided |
| 9. Can the results be applied to the local population, or in your context? | 1 | Yes, they can. |
| 10. Were all clinically important outcomes considered? | 1 | Yes, they were. Complications and limitations of the study are provided, as well as the reproducibility of the measurement instrument |
| 11. Are the benefits worth the harms and costs? | 1 | Risks and costs of the measurements of AA are minimal. It allows obtaining more knowledge on the accommodative function after ICL implantation |
CASPe scoring: 5/11.
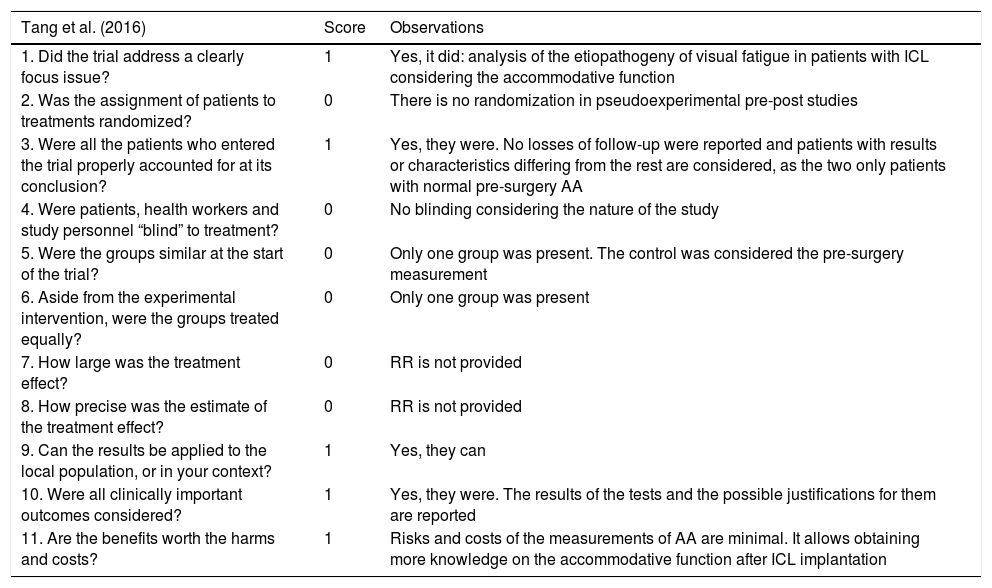
Evaluation of the quality of the study «Accommodation after an implantable collamer lens implantation in high myopia patients» (Tang, 2016) with the CASPe tool.
| Tang et al. (2016) | Score | Observations |
|---|---|---|
| 1. Did the trial address a clearly focus issue? | 1 | Yes, it did: analysis of the etiopathogeny of visual fatigue in patients with ICL considering the accommodative function |
| 2. Was the assignment of patients to treatments randomized? | 0 | There is no randomization in pseudoexperimental pre-post studies |
| 3. Were all the patients who entered the trial properly accounted for at its conclusion? | 1 | Yes, they were. No losses of follow-up were reported and patients with results or characteristics differing from the rest are considered, as the two only patients with normal pre-surgery AA |
| 4. Were patients, health workers and study personnel “blind” to treatment? | 0 | No blinding considering the nature of the study |
| 5. Were the groups similar at the start of the trial? | 0 | Only one group was present. The control was considered the pre-surgery measurement |
| 6. Aside from the experimental intervention, were the groups treated equally? | 0 | Only one group was present |
| 7. How large was the treatment effect? | 0 | RR is not provided |
| 8. How precise was the estimate of the treatment effect? | 0 | RR is not provided |
| 9. Can the results be applied to the local population, or in your context? | 1 | Yes, they can |
| 10. Were all clinically important outcomes considered? | 1 | Yes, they were. The results of the tests and the possible justifications for them are reported |
| 11. Are the benefits worth the harms and costs? | 1 | Risks and costs of the measurements of AA are minimal. It allows obtaining more knowledge on the accommodative function after ICL implantation |
CASPe scoring: 5/11.
According to the current systematic review, the evidence describing the impact of the pIOLs implantation on the accommodative function is scarce and with poor quality. In addition, the clinical methods applied in the two studies included in the systematic review are very different between them. Therefore, these studies cannot be considered as comparable, although both show a loss of accommodation amplitude after surgery. This potential accommodative loss can be explained by two theories. From the optical point of view, biometric changes occurring during accommodation suggest that the power of the eye for a specific distance may be different from the expected if the optic eye system remains static and only lens power changes.21–25 Furthermore, the change in light vergence and the size of the retinal image evidenced by Langenbucher17 show that more accommodation is required to focus a near object with pIOLs compared to spectacles. Although this study has the inherent limitations of theoretical models (use of paraxial optics and thin lenses), the impact of pIOLs on accommodation is unquestionable. Another hypothesis is that the decreased amplitude of accommodation observed after surgery may be due to the interaction between the pIOL and ciliary muscle in patients with posterior chamber pIOLs, as the ICL model. Indeed, a more significant incrustation of the pIOL haptics in the ciliary muscle during accommodation has been observed in studies evaluating ultrasonic biomicroscopy images.12 However, this hypothesis should be corroborated in future studies evaluating larger samples sizes using ultrasound biomicroscopy technology.
Besides the decrease in the amplitude of accommodation, the two studies evaluated in our systematic review showed a decreased positive relative accommodation and better accommodation facility after the implantation of posterior chamber pIOLs. However, these results have not been confirmed by other authors in other studies. Furthermore, it is unknown if these potential changes in accommodation reported in these two studies are maintained in the medium-long term. It should be considered that according to the current systematic review the quality of the two studies evaluated is limited. Therefore, considering the limited number of studies on accommodative changes after the implantation of ICL and the relatively poor quality of them, there is no scientific evidence supporting that these changes occur or do not occur. Likewise, it cannot be concluded that ICL implantation has a negative or positive effect on accommodation, being necessary more studies with high quality standards to confirm this. Indeed, this may be a very interesting research area for the future that could be extended to any type of phakic IOL.
According to literature, researchers and speakers in congresses cannot stay that there is great evidence on the limitation in accommodation that is generated by phakic IOLs because this is untrue. This has recently happened, and this was the main reason for conducting this systematic review. For this reason, we would like to publish this paper and to highlight that until more research is conducted, nobody cannot state that there is strong evidence on the potential limitation on accommodation generated by phakic IOLs.
In conclusion, scientific literature addressing how pIOL implantation affect the accommodative function is poor and with biases limiting its quality. Therefore, the scientific evidence on this issue is insufficient and more research is needed to improve the knowledge about refractive surgery with pIOLs and accommodation to minimize post-surgery complications in the visual function.
Conflicts of interestThe authors have no proprietary or commercial interest in the medical devices that are involved in this manuscript. The author David P Piñero has been supported by the Ministry of Economy, Industry and Competitiveness of Spain within the program Ramón y Cajal, RYC-2016-20471.