To analyze the effects of Eye-Tracker performance on the pulse positioning errors during refractive surgery.
MethodsA comprehensive model, which directly considers eye movements, including saccades, vestibular, optokinetic, vergence, and miniature, as well as, eye-tracker acquisition rate, eye-tracker latency time, scanner positioning time, laser firing rate, and laser trigger delay have been developed.
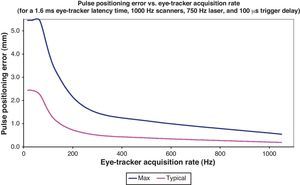
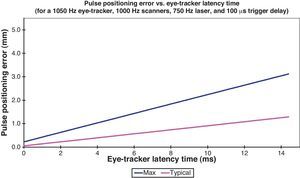
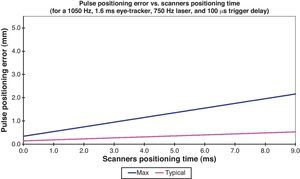
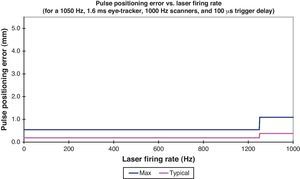
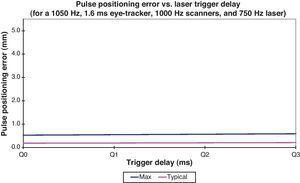
ResultsEye-tracker acquisition rates below 100Hz correspond to pulse positioning errors above 1.5mm. Eye-tracker latency times to about 15ms correspond to pulse positioning errors of up to 3.5mm. Scanner positioning times to about 9ms correspond to pulse positioning errors of up to 2mm. Laser firing rates faster than eye-tracker acquisition rates basically duplicate pulse-positioning errors. Laser trigger delays to about 300μs have minor to no impact on pulse-positioning errors.
ConclusionsThe proposed model can be used for comparison of laser systems used for ablation processes. Due to the pseudo-random nature of eye movements, positioning errors of single pulses are much larger than observed decentrations in the clinical settings. There is no single parameter that ‘alone’ minimizes the positioning error. It is the optimal combination of the several parameters that minimizes the error. The results of this analysis are important to understand the limitations of correcting very irregular ablation patterns.
Analizar los efectos del comportamiento con láser excímer en los errores de posicionamiento de pulso durante la cirugía refractiva.
MétodosSe ha desarrollado un modelo amplio, que considera directamente los movimientos oculares, incluyendo los sacádicos, vestibulares, opto-quinéticos, de vergencia y miniatura, así como el porcentaje de adquisición del eye-tracker, tiempo de latencia del eye-tracker, tiempo de posicionamiento del escáner, porcentaje de disparos láser y demora del disparador láser.
ResultadosLas tasas de adquisición del eye-tracker inferiores a 100Hz se corresponden con los errores de posicionamiento de pulso superiores a 1,5mm. Los tiempos de latencia del eye-tracker de alrededor de 15ms se corresponden con errores de posicionamiento de pulso de hasta 3,5mm. Los tiempos de posicionamiento del escáner de alrededor de 9ms se corresponden con errores de posicionamiento de pulso de hasta 2mm. Las tasas de disparo de disparos láser con más rápidas que las tasas de adquisición del eye-tracker duplican básicamente los errores de posicionamiento de pulso. Las demoras del disparador láser de alrededor de 300μs tienen un impacto menor o nulo sobre los errores de posicionamiento de pulso.
ConclusionesEl modelo propuesto puede utilizarse para comparar los sistemas láser utilizados en los procesos de ablación corneal en cirugía refractiva láser. Debido a la naturaleza pseudo-aleatoria de los movimientos oculares, los errores de posicionamiento de los pulsos individuales son mucho mayores que los descentramientos reportados a nivel clínico. No existe un único parámetro que minimice “por sí solo” el error de posicionamiento. Los resultados de este análisis son importantes para la comprensión de las limitaciones de la corrección con perfiles de ablación muy irregulares.
The available excimer lasers allow for the correction of refractive defects such as myopia,1 hyperopia,2 or astigmatism.3 Achieving accurate clinical outcomes and reducing the likelihood of a retreatment procedure are major goals of refractive surgery. For that, highly precise lasers are required.
Current laser systems have repetition rates as fast as 500Hz,4 with spot sizes as small as 0.5mm.5 This means, for a high fidelity in refractive correction, it is necessary to position the laser spots every 2ms with a very high precision. Since the patient's eye is not fixated, any eye movement disturbs this precision.6
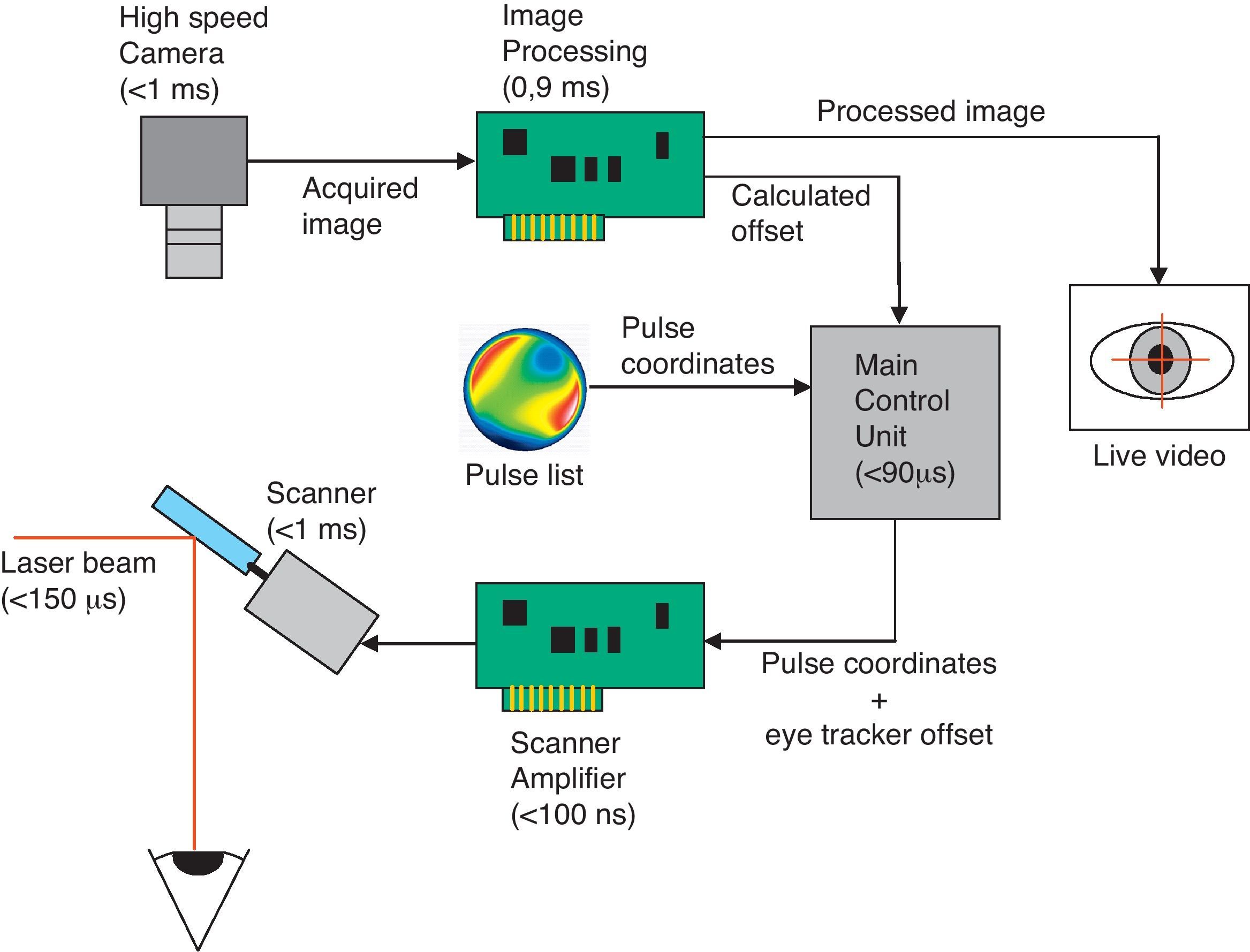
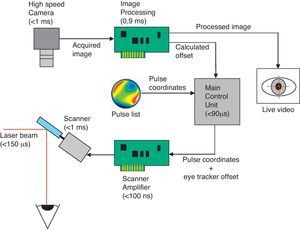
Usually, eye tracking7 is solved by machine vision: a camera acquires an image of the eye, an image processing unit searches the pupil and calculates the position as an offset, a laser and scanner control unit adds this offset to the pulse coordinates, and a scanner positions the laser beam (Fig. 1).
How does an eye tracker work? Usually, eye tracking is solved by machine vision: a camera acquires an image of the eye, an image processing unit searches the pupil and calculates the position as an offset, a laser and scanner control unit adds this offset to the pulse coordinates, finally, a scanner positions the laser beam.
The problem in machine vision is the needed time for acquiring the image, processing the image and reacting. In manufacturing processes for goods inspection, there is always time between image acquisition and reaction, e.g. sorting bad parts from good parts. In refractive surgery the time between acquiring the image and repositioning the scanner (reacting) produces a slack in the spot position.8
We present a theoretical investigation, whose aim is to objectively analyze the effects of individual parameters characterizing eye-tracking systems (eye-tracker acquisition rate, eye-tracker latency time, scanner positioning time, laser firing rate, and laser trigger delay) on the optical outcome, namely on the accuracy of the positioning single pulses during refractive surgery under consideration of realistic eye-movements (saccades, vestibular, optokinetic, vergence, and miniature).
Materials and methodsWe have developed a comprehensive model, which directly considers eye movements, including saccades, vestibular, optokinetic, vergence, and miniature, as well as, eye-tracker acquisition rate, eye-tracker latency time, scanner positioning time, laser firing rate, and laser trigger delay to analyze the effects of Eye-Tracker performance on the pulse positioning errors during refractive surgery. This statistical model has been applied for the simulation of worst and typical case scenarios, independent on human errors.
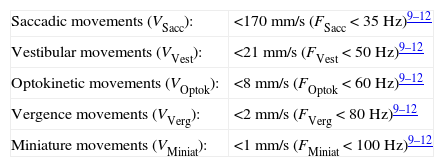
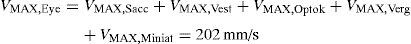
Eye movements9–12The velocity of the eye movements (VEye) is given by the combination of the velocities and frequencies of:
A maximum value occurs in the unlikely event that all components of the eye movements contribute in the same direction:
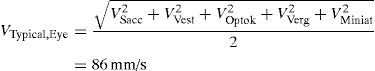
A typical value assumes that the relative orientation of all components of the eye movements are randomly assigned and all movement components occur at half of their maximum velocity:
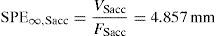
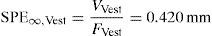
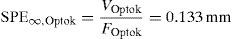
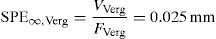
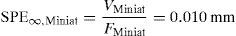
Limit for the spot positioning errorA numerical limit for the spot positioning error (SPE∞) can be imposed based on the fact that eye movements cannot keep constantly moving and show a frequency nature.
For each eye movement component the amplitude limit of SPE∞ can be expressed as:
Spot positioning errorThe spot positioning error (SPE) depends on several parameters:
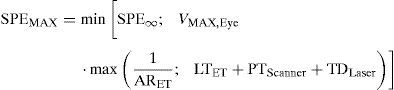
A maximum value occurs when the Eye-Tracker needs to take a full iteration process for that pulse and the scanner needs its complete positioning time to place the next pulse:
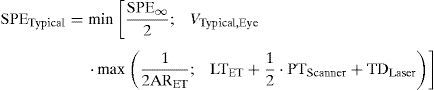
A typical value occurs when the Eye-Tracker needs to take a half iteration process for that pulse and the scanner needs a half of its positioning time to place the next pulse:
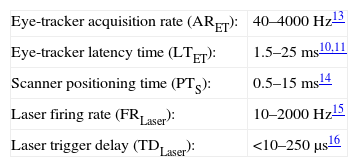
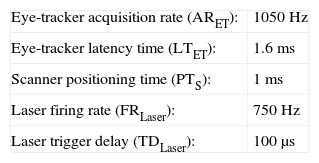
SimulationsWe have considered as reference a state-of-the-art system configuration with following parameters:
We have then analyzed the effect of the different parameters individually by modifying its assumed value within the range found for real systems used in refractive surgery and keeping constant all other parameters at the reference values.
ResultsThe pulse positioning error depends on eye movements, including saccades, vestibular, optokinetic, vergence, and miniature, as well as, eye-tracker acquisition rate, eye-tracker latency time, scanner positioning time, laser firing rate, and laser trigger delay. As the eye movements increase their velocity, the pulse positioning error increases.
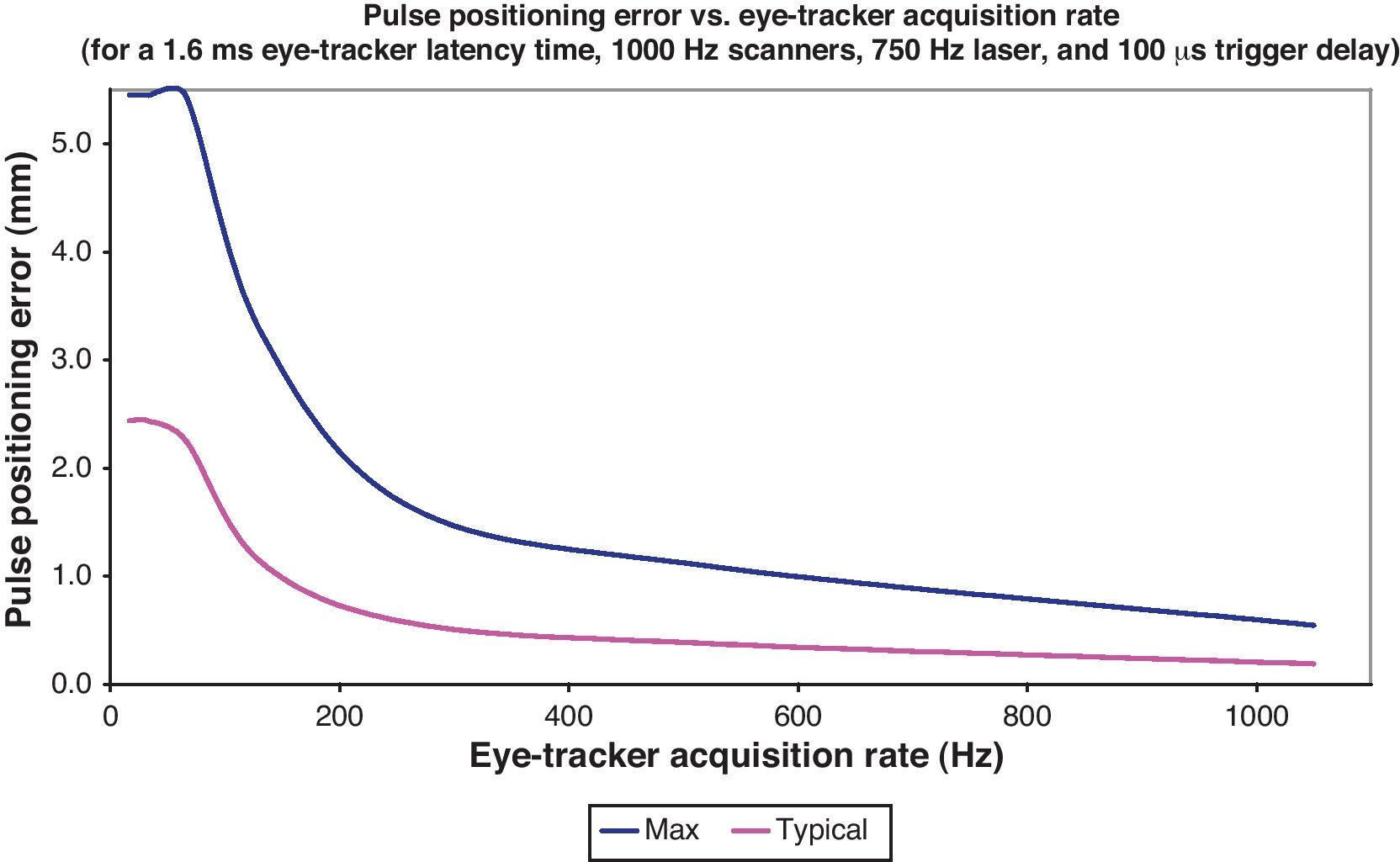
As the eye-tracker acquisition rate increases, the pulse positioning error decreases. This change is shown in Fig. 2. Eye-tracker acquisition rates below 100Hz correspond to pulse positioning errors above 1.5mm typically. Eye-tracker acquisition rates above 1000Hz correspond to pulse positioning errors below 0.5mm (typically below 0.2mm).
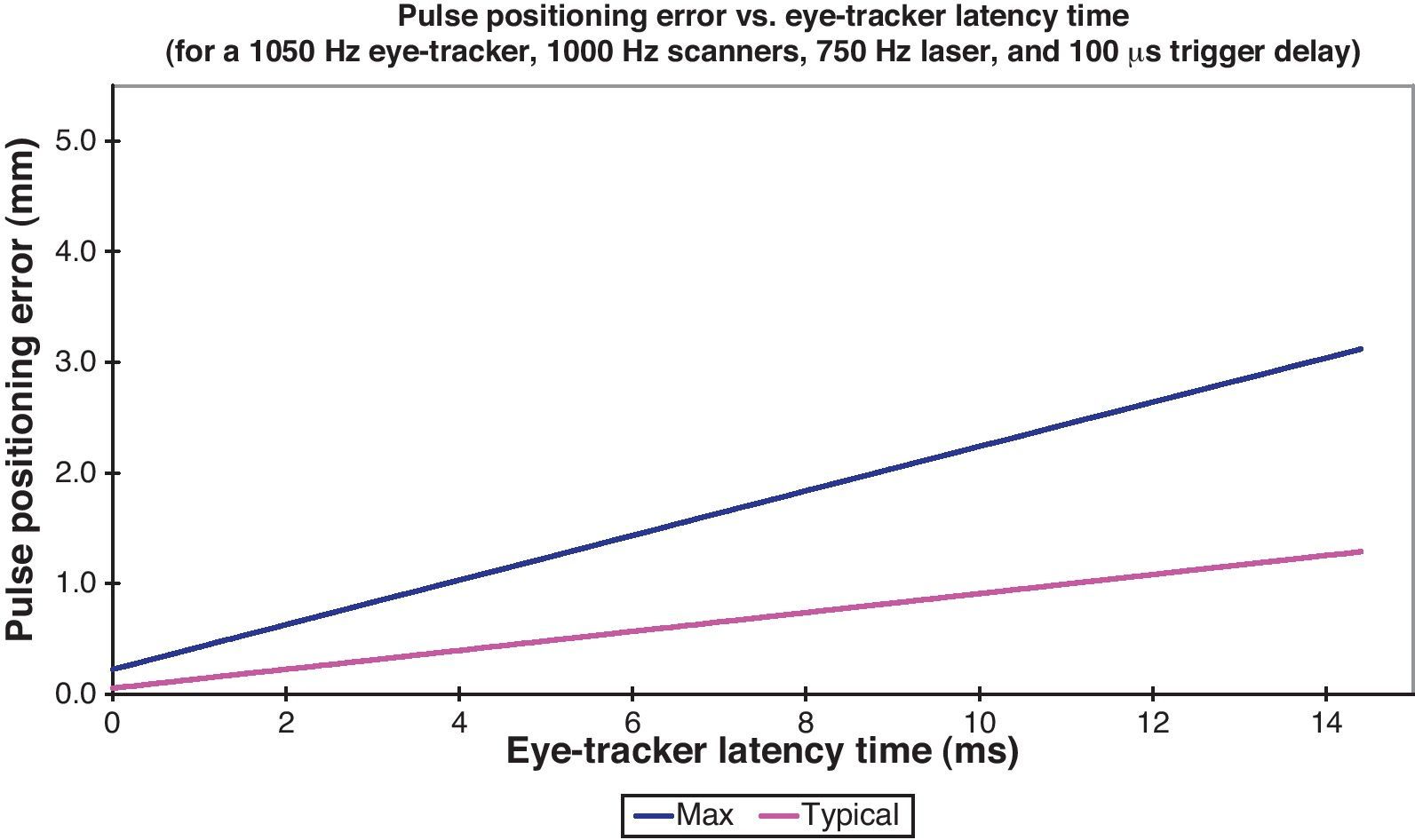
As the eye-tracker latency time decreases, the pulse positioning error decreases. This change is shown in Fig. 3. Eye-tracker latency times to about 15ms correspond to pulse positioning errors of up to 3.5mm. Eye-tracker latency times below 1.5ms correspond to pulse positioning errors below 0.5mm (typically below 0.2mm).
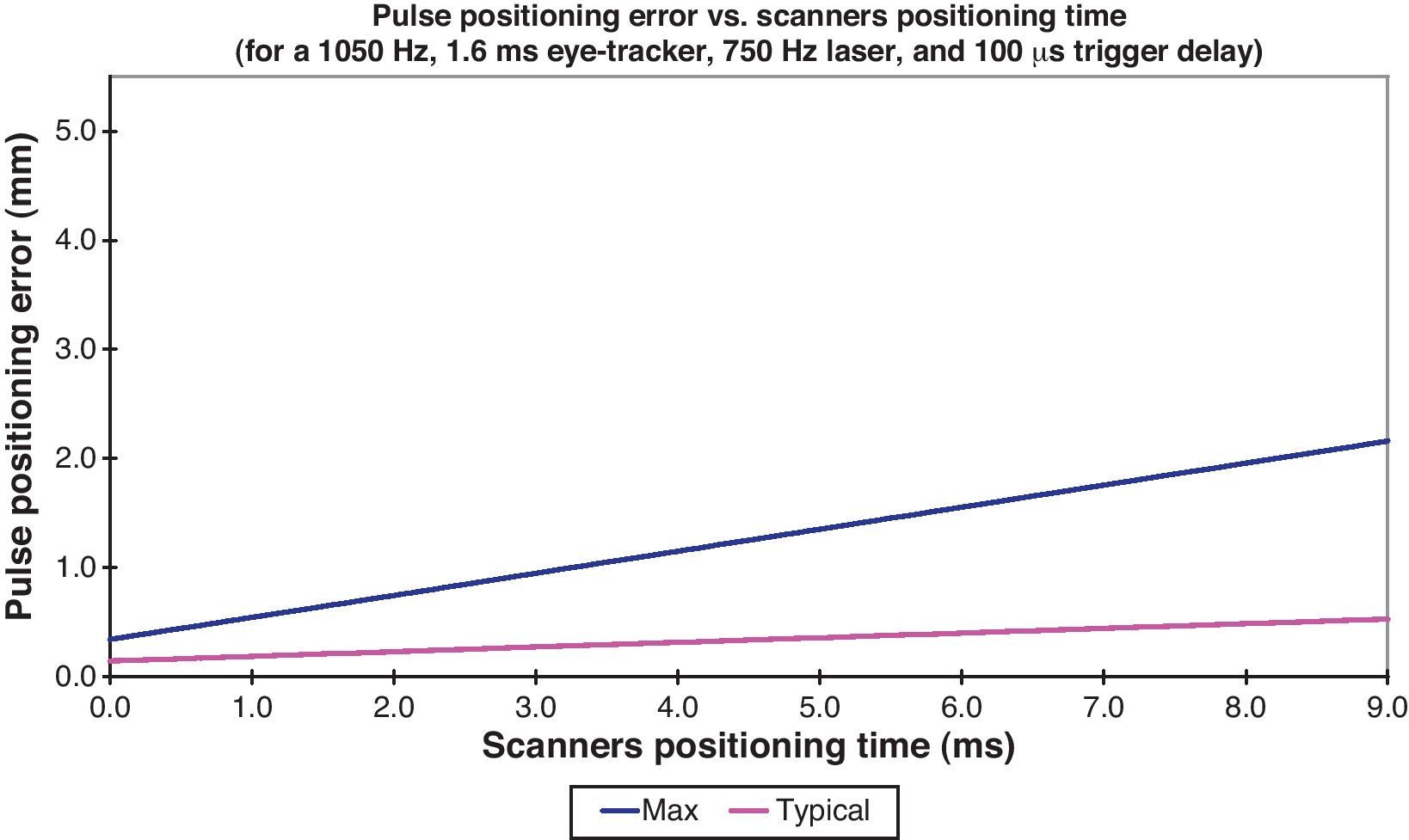
As the scanner positioning time decreases, the pulse positioning error decreases. This change is shown in Fig. 4. Scanner positioning times to about 9ms correspond to pulse positioning errors of up to 2mm. Scanner positioning times below 0.8ms correspond to pulse positioning errors below 0.5mm (typically below 0.2mm).
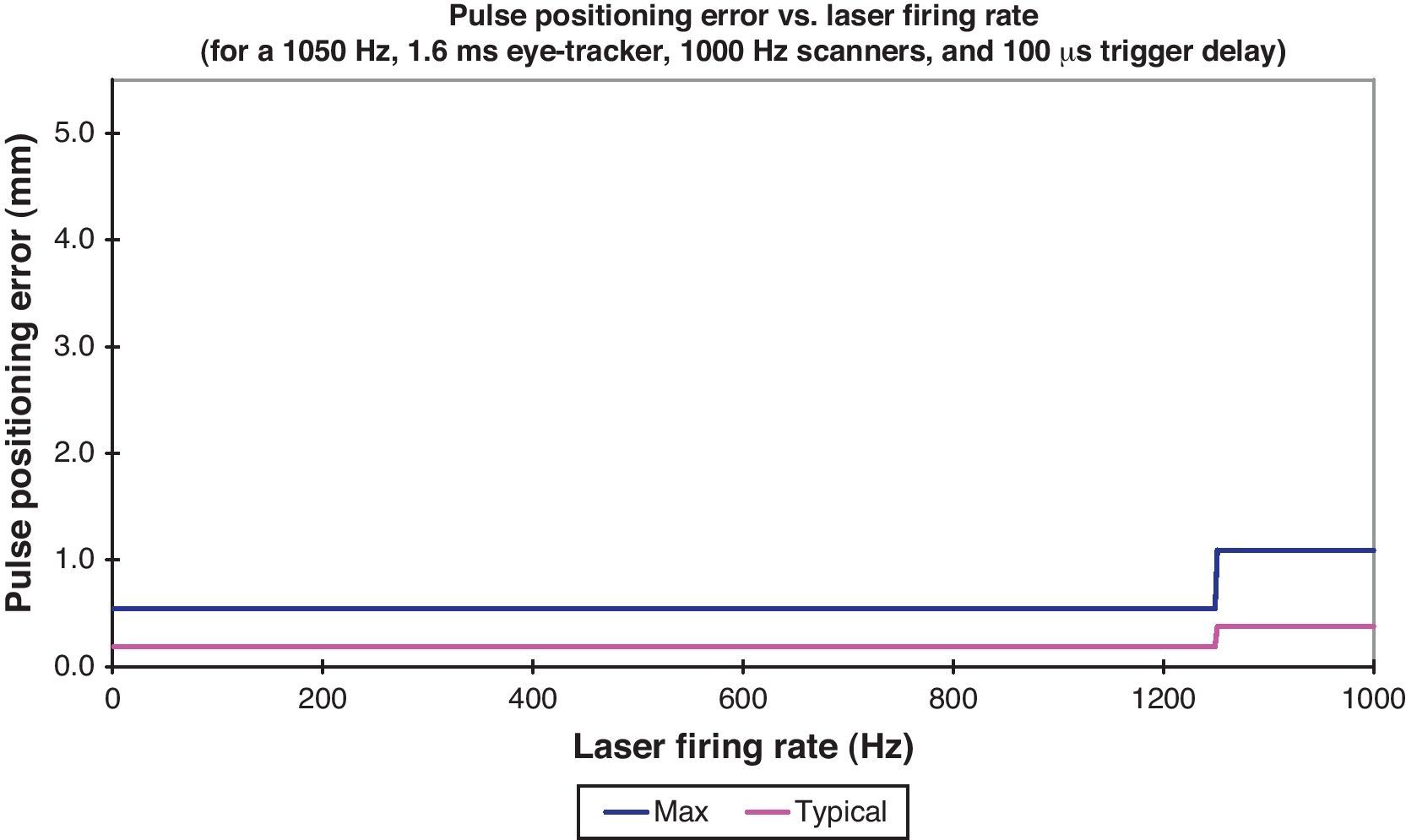
As the laser firing rate increases above the eye-tracker acquisition rate, the pulse positioning error increases. This change is shown in Fig. 5. Laser firing rates faster than eye-tracker acquisition rates basically double pulse positioning errors.
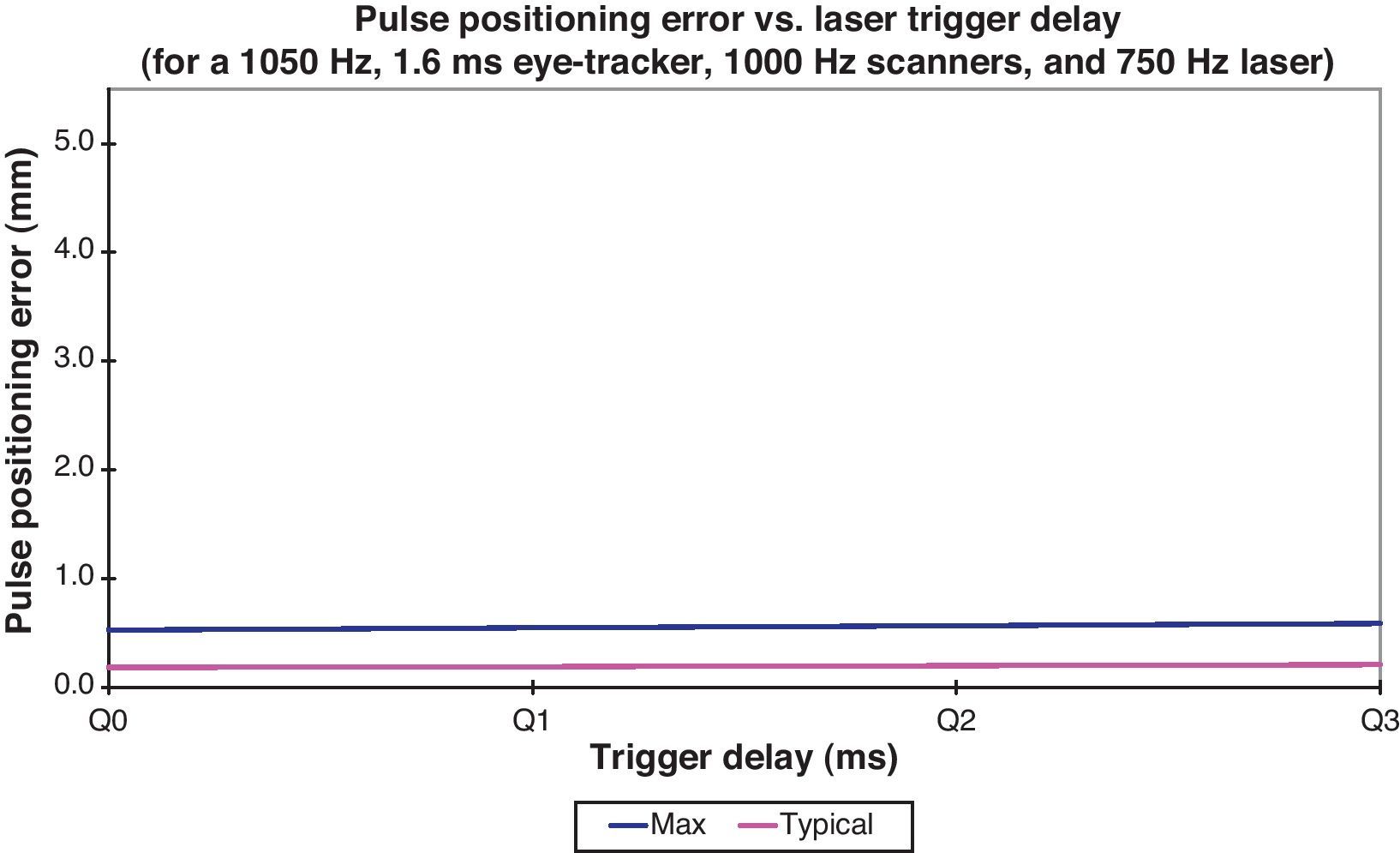
As the laser trigger delay decreases, the pulse positioning error decreases. This change is shown in Fig. 6. Laser trigger delays to about 300μs have minor to no impact on pulse positioning errors.
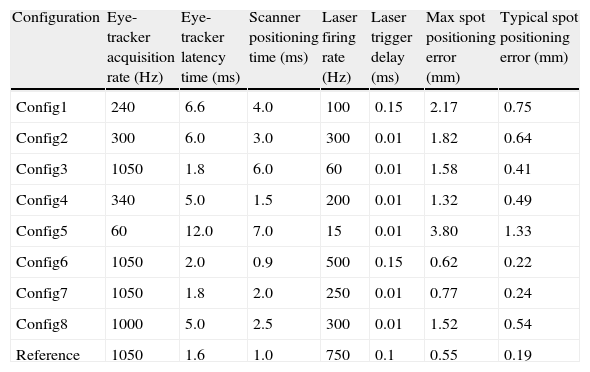
Table 1 shows a summary of the effects of different system configurations.
Effects of different system configurations.
| Configuration | Eye-tracker acquisition rate (Hz) | Eye-tracker latency time (ms) | Scanner positioning time (ms) | Laser firing rate (Hz) | Laser trigger delay (ms) | Max spot positioning error (mm) | Typical spot positioning error (mm) |
| Config1 | 240 | 6.6 | 4.0 | 100 | 0.15 | 2.17 | 0.75 |
| Config2 | 300 | 6.0 | 3.0 | 300 | 0.01 | 1.82 | 0.64 |
| Config3 | 1050 | 1.8 | 6.0 | 60 | 0.01 | 1.58 | 0.41 |
| Config4 | 340 | 5.0 | 1.5 | 200 | 0.01 | 1.32 | 0.49 |
| Config5 | 60 | 12.0 | 7.0 | 15 | 0.01 | 3.80 | 1.33 |
| Config6 | 1050 | 2.0 | 0.9 | 500 | 0.15 | 0.62 | 0.22 |
| Config7 | 1050 | 1.8 | 2.0 | 250 | 0.01 | 0.77 | 0.24 |
| Config8 | 1000 | 5.0 | 2.5 | 300 | 0.01 | 1.52 | 0.54 |
| Reference | 1050 | 1.6 | 1.0 | 750 | 0.1 | 0.55 | 0.19 |
Achieving accurate clinical outcomes and reducing the likelihood of a retreatment procedure depend on accurate and precise lasers. In parallel to the clinical developments, increasingly capable, reliable, and safer laser systems with better resolution and accuracy are required.
The pulse positioning error is an effect that should be considered in commercial laser systems using sophisticated high-performance eye-tracker, scanner systems and algorithms that cover most of the possible variables. The analytical expressions provided in this work are useful to compute reasonable expected and maximum values for the spot positioning errors. The model directly considers eye movements, including saccades, vestibular, optokinetic, vergence, and miniature, as well as, eye-tracker acquisition rate, eye-tracker latency time, scanner positioning time, laser firing rate, and laser trigger delay. Separate analysis of the effect of each parameter was performed.
In Eqs. (3) and (4), SPE depends on the maximum of the two magnitudes within brackets and not on the sum of these magnitudes. The dependency on the maximum instead of the sum, comes from the fact that the camera only needs an integration time definitely shorter than the period between two consecutive frames, so after integration and before acquisition of the next frame is started, already image computations can take place.
The vestibulo-ocular reflex is a reflex eye movement that stabilizes images on the retina during head movement by producing an eye movement in the direction opposite to head movement (horizontal, vertical, or torsional), thus preserving the image on the center of the visual field. Since slight head movement is present all the time, the vestibulo-ocular reflex is very important for stabilizing vision. The vestibulo-ocular reflex needs to be fast, but eye movements lag the head movements by up to 10ms. Furthermore, The ‘gain’ of the horizontal and vertical vestibulo-ocular reflex is usually close to one, but the gain of the torsional vestibulo-ocular reflex is generally low. During refractive surgery, both lag and gain are also influenced by the refractive errors of the patient.
The eye-tracker acquisition rate plays the most important role in the determination of pulse positioning errors. The range for eye-tracker acquisition rates of the excimer laser systems for refractive surgery available in the market runs from about 40Hz to about 4000Hz. Eye-tracker acquisition rates below 100Hz correspond to pulse positioning errors above 1.5mm typically, demonstrating the importance of having a fast acquisition eye-tracker. Eye-tracker latency times run from 1.5ms to ∞ (representing no eye-tracking system) or to 25ms. Eye-tracker latency times to about 15ms correspond to pulse positioning errors of up to 3.5mm. Therefore, it is important to have a fast processing eye-tracker.
The range for scanner positioning times of the excimer laser systems for refractive surgery available in the market runs from about 0.5ms to about 15ms. Scanner positioning times to about 9ms correspond to pulse positioning errors of up to 2mm. This requires the use of fast reacting scanners. Laser firing rates run from 10Hz to 2000Hz. Laser firing rates faster than eye-tracker acquisition rates basically double pulse positioning errors. This fact emphasizes the importance of having a faster acquisition eye-tracker than laser firing rate.
The range for laser trigger delay of the excimer laser systems for refractive surgery available in the market runs from below 10μs to about 250μs. Laser trigger delays to about 300μs have minor to no impact on pulse positioning errors.
Today, several approaches to import, visualize, and analyze high detailed diagnostic data of the eye (corneal or ocular wavefront data) are offered. At the same time, several systems are available to link diagnostic systems for measurement of corneal and ocular aberrations of the eye to refractive laser platforms. These systems are state-of-the-art with flying spot technology, high repetition rates, fast active eye trackers, and narrow beam profiles. Consequently, these systems offer new and more advanced ablation capabilities.
The model described here provides analytical expressions for pulse positioning errors, based upon comprehensive parameters. Due to the pseudo-random nature of actual eye movements, the proposed model provides results of positioning errors of single pulses much larger than observed decentrations in the clinical settings and to those reported in the recent literature.17–19
Many customized laser systems are still based in placido topographic systems. And placido based topographic systems present high variation in irregular corneas.20 So even the most sophisticated build system in aspects of eye tracker latency time and scanners response time still relies on possibly unreliable topographic measurement. The variability pattern correlates with the pattern of corneal topography: steeper corneal areas possessed higher variability values compared with flatter areas of the same cornea.20
In our work, all random eye movements are treated as rectilinear ones without regard to their expected lengths (=amplitudes) before stopping or changing direction. If the time frames considered in this work exceed the typical time it takes to change the movement direction, the positioning errors can be highly overestimated by the model. Furthermore, from stochastic assumptions it can be predicted that if the time frame for stopping or changing direction for any movement component is much shorter than the system latency time, the contribution of this movement component tends to be ‘zero’, or more realistic it becomes unpredictable.
The power spectral density of the motion data shows main frequency contents being below 60Hz.10,11 An interpretation of the observed frequency spectra was given in terms of a model, which assumes that the dynamics of the eye muscle system are linear and that the active state input producing tremor has a flat frequency spectrum.12 From this it was deduced that the eye behaves as an overdamped second-order system with time constants of 0.002 and 0.02s. From here, it seems that some 50–60Hz are the primary frequencies and 500Hz the maximum frequency, which means that more than twice 500Hz eye-tracker sampling rate is enough to track all relevant eye movements.
Even though a large number of detailed parameters are considered, this model is still characterized by a relatively low degree of complexity.
There is no single parameter that alone minimizes the positioning error. It is the optimal combination of several parameters that is necessary to minimize the error. Finally, for placing the pulse the latency time of the system is more relevant than the sampling rate.
ConclusionsOur model provides an analytical expression for the positioning errors of single pulses, resulting in much larger errors than observed decentrations in the clinical settings and to those reported in the recent literature. The results of this analysis are important to understand the limitations of correcting very irregular ablation patterns. This model may complement previous analytical approaches and may sustain the observations reported by others. The model incorporates several factors that were ignored in previous models and due to its analytical approach, it is valid for different laser devices used in refractive surgery, for which the specific laser characteristics are known.
The development of more accurate models to improve emmetropization and the correction of ocular aberrations is an important issue. We hope that this model will be an interesting and useful contribution to refractive surgery and will take us one-step closer to this goal.
Financial supportPrivate financial support was provided by SCHWIND Eye-tech-solutions, Kleinostheim, Germany. This research received no specific grant from any funding agency in the public or not-for-profit sectors.
Conflict of interestSamuel Arba-Mosquera is employee at SCHWIND Eye-tech-solutions. Ioannis M. Aslanides has no commercial or proprietary interests in the materials presented herein.
Presented at meetings: ESCRS 2007 Stockholm.