To investigate whether “normal” eyes viewing through keratoconic (KC) eye aberrations can achieve a similar visual performance (VP) to that of KC eyes.
MethodWe measured the high-contrast visual acuity (VA) and the 10, 15 and 20 c/deg contrast sensitivity (CS) of 6 KC eyes and 6 “normal” eyes while dynamically correcting their monochromatic aberrations. The VP of both populations was also measured when viewing through the usual sphero-cylindrical correction (i.e. spectacle correction) of each KC eye. In both cases, the desired wavefront was simulated thanks to a deformable mirror.
ResultsDuring dynamic correction, both KC and “normal” eyes showed similar (P>0.10) amounts of higher-order aberrations (in average, 0.10μm of RMS for a 5.5mm pupil). The difference between KC and “normal” eyes’ VP was 0.24 log units and 0.12 log-MAR in terms of CS and VA, respectively. When viewing through KC eye aberrations, “normal” eyes showed comparable or slightly better CS (difference of 0.05 log units) but lower VA (difference of 0.13 logMAR) than KC eyes.
ConclusionsKC subjects are adapted to their poor retinal image quality. However, this neural adaptation might only occur for usual “real life” visual tasks (i.e., VA-related tasks).
Investigar si un ojo “normal” que ve a través del patrón de aberraciones de un ojo con queratocono (QC) puede lograr una calidad visual (CV) similar a la que tiene un ojo con QC.
MétodosHemos medido la agudeza visual (AV) de alto contraste y la sensibilidad al contraste (SC) a 10, 15 y 20 ciclos/grado en 6 ojos con QC y en 6 ojos “normales”, a la vez que corregíamos de manera dinámica sus aberraciones monocromáticas. También se midió la CV de ambos grupos, pero esta vez anteponiendo la corrección esferocilíndrica habitual (es decir, la corrección de sus gafas) de cada uno de los ojos con QC participantes en el estudio. En ambos casos, el frente de onda deseado se generó por medio de un espejo deformable.
ResultadosDurante la corrección dinámica, tanto los ojos con QC como los “normales” presentaron una cantidad similar (P>0,10) de aberraciones de alto orden (RMS promedio: 0,10μm para un diámetro de pupila de 5,5mm). La diferencia de CV entre ojos con QC y ojos “normales” resultó ser igual a 0,24 unidades log. (SC) y a 0,12 logMAR (AV). Cuando se hizo ver a ojos “normales” a través del patrón de aberraciones de ojos con QC, se observó que los ojos “normales” tienen una SC comparable o ligeramente mejor que los ojos con QC (diferencia de 0,05 unidades log.) pero una AV más baja (diferencia de 0,13 logMAR).
ConclusionesLos sujetos con QC están adaptados a la mala calidad de su imagen retiniana. Sin embargo, esta adaptación neuronal podría producirse únicamente en el contexto de tareas visuales habituales de la “vida diaria” (es decir, aquellas presentes en un test de AV).
It is well known that the human eye suffers from monochromatic aberrations that degrade the retinal image quality and, thus, limit visual performance.1 However, these performance depends on the optical blur induced by the wavefront aberrations but also on the neural process that may counterbalance some of the degradation due to the optics of the eye.
In fact, some individuals seem to exhibit perceptual adaptation after a period of sustained blur, which results in an improvement in their visual acuity (VA). Mon-Williams et al.2 measured a VA increase of 0.10 logMAR, averaged across 15 subjects, after a 30-min period of +1.00 D induced defocus blur. After 45min of viewing through +1.00 D and +3.00 D lenses, Cufflin et al.3 found an improvement in VA of 0.17 logMAR and 0.23 logMAR respectively. They also noted that VA changes became significant after 30minutes of exposure to optical blur. After a longer period (i.e., 2hours) of +2.50 D induced defocus, George and Rosenfield4 measured a VA increase of 0.20 logMAR, averaged across 18 myopic and 13 emmetropic subjects. The difference between these 2 groups was not statistically significant. Rosenfield et al.5 obtained a similar VA improvement (0.23 logMAR, averaged across 22 slightly myopic subjects), after a 3-hour period spent without any refractive correction. On the contrary, after a 90 min period of blur adaptation during which 10 low myopes did not have their sphero-cylinder errors corrected (between 0 and -2 D), Pesudovs and Brennan6 observed a very small increase of 0.04 logMAR. This improvement in VA was low, taking into account the repeatability of the VA measurement.
These experiments demonstrated the influence on visual acuity of the neural adaptation to a blurred retinal image.
Recently, Artal et al.7 wondered whether the visual system was adapted to the particular pattern of optical aberrations of its own eye. They observed that the subjective blur induced by one's own aberrations had a lower impact than the subjective blur induced by a rotated version of these aberrations. This result confirmed the hypothesis of a neural adaptation of the visual system to a particular eye's monochromatic aberrations. Chen et al.8 found that the correction of 88% of the eye's aberrations provided the best subjective image quality, indicating a small adaptation (12% of the aberrations) of the visual system. However, this result was obtained on 3 subjects with small levels of higher-order aberrations. A larger adaptation could be observed in individuals with larger amounts of aberrations.
Eyes with keratoconus or penetrating keratoplasty are affected in larger measure by higher-order aberrations. Pantanelli et al.,9 averaging across 33 keratoconic eyes, obtained a higher-order-aberration RMS of around 2.24μm for a 6mm pupil diameter, which is around 5 times more than in “normal” eyes. In these eyes, the neural compensation of the visual system should be larger than in “normal” eyes.
Recently, Sabesan and Yoon10 measured a significantly worse VA in keratoconic eyes (-0.07 logMAR) than in “normal” eyes (-0.26 logMAR) following aberration correction. They concluded that a long-term visual experience with poor retinal image quality due to higher-order aberrations in keratoconic eyes might limit the visual performance achieved with a very high optical quality. However, this result could be also explained by saying that in keratoconic eyes there is a poorer neural process than in “normal” eyes.
The purpose of the present study was to investigate whether or not keratoconic eyes could be adapted to their usual aberrations. We determined whether “normal” eyes viewing through the aberration pattern of keratoconic eyes were able to achieve a similar visual performance to that of keratoconic eyes.
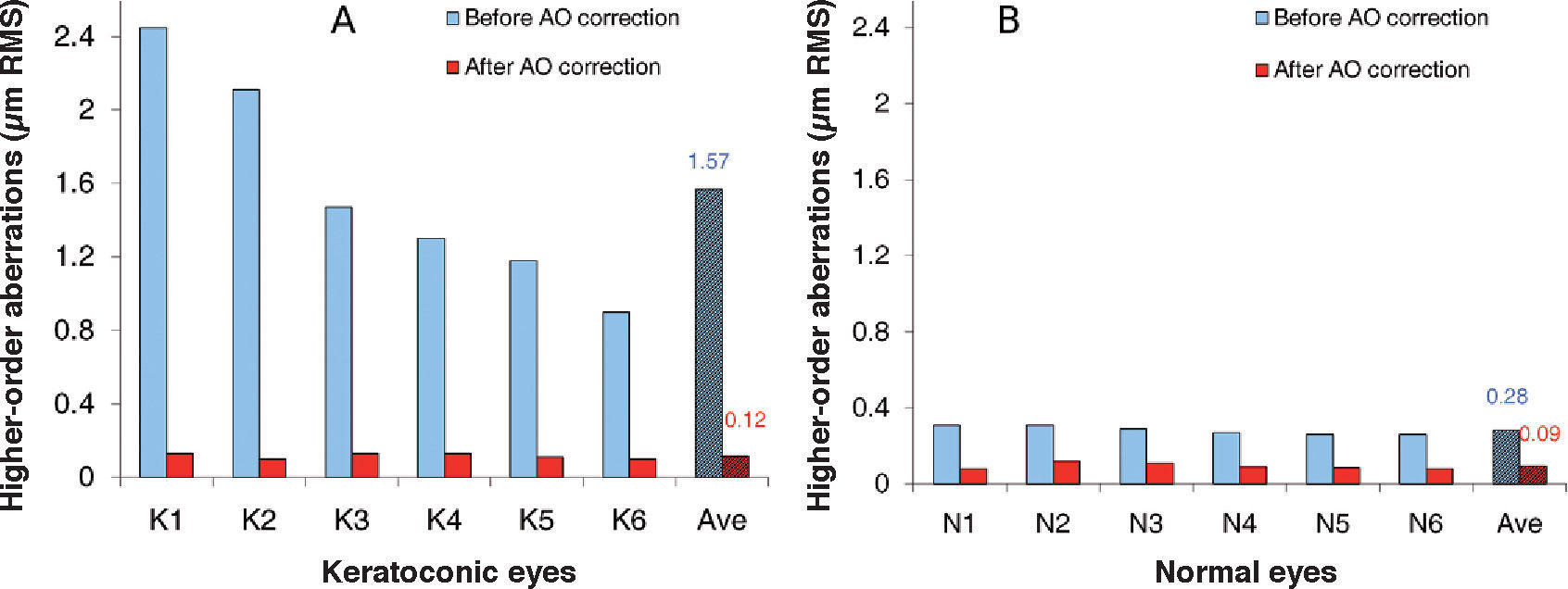
MethodSubjectsSix keratoconic (KC) eyes of 4 subjects, aged 25 to 39 (mean age: 31.8 years), were involved in this study. All these subjects were spectacle wearers. They had never before worn any contact lenses, meaning that their usual correction was their spectacle correction. They were recruited into the study just before a contact lens fitting procedure. Their spherical refractive error ranged from-7.50 to 0 D, with astigmatism being lower than or equal to 2.00 D. Six “normal” eyes of 6 subjects, aged 21 to 32 (mean age: 24.8 years) were also included. The magnitude of their spherical error ranged from -3.50 to +4.75 D, with astigmatism being lower than or equal to 1.50 D. The average amount of higher-orderaberration RMS was 1.57±0.59μm for the KC eyes and 0.28±0.02μm for the “normal” eyes, assessed over a 5.5mm pupil. The pupil diameter of KC and “normal” eyes was, in all cases, higher than 5.5mm under our testing conditions. The subjects had clear intraocular media.
The tenets of the Declaration of Helsinki were followed. Informed consent was obtained from each subject after verbal and written explanation of the nature and possible consequences of the study.
General MethodIn the first condition (condition A), 10, 15 and 20 c/ deg contrast sensitivity (CS) and high-contrast visual acuity (VA) were measured in random order for all 6 KC eyes and 6 “normal” eyes during dynamic correction of their monochromatic aberrations.
These medium spatial frequencies were selected to match the range of the main spatial frequencies present in everyday life (e.g., reading letter size, road-sign letter size).
In condition B, we measured the visual performance of the KC and “normal” eyes when viewing through the usual sphero-cylindrical correction (i.e. spectacle refractive correction) of each KC eye.
In both cases, the desired wavefront was simulated with the aid of a deformable mirror. In order to simulate in “normal” eyes the vision of each KC eye, we reshaped this mirror to generate the residual aberrations (i.e. residual secondorder aberrations and higher-order aberrations) measured in each KC eye when correcting them from their usual defocus and astigmatism terms (i.e. spectacle correction). Then, we assessed the visual performance of each “normal” eye while viewing through these residual aberrations.
The whole measuring process took around 1.5hours per KC eye and was completed in one session, including several rest periods between measurements. For each “normal” subject, the full process took around 5h and was completed in 7 sessions.
ApparatusWe used the CRX1™ adaptive-optics system (Imagine Eyes, Orsay, France) consisting of 2 basic elements: a wavefront sensor and a correcting device. The system optically conjugates the exit pupil plane of the subject with the correcting device, the wavefront sensor and an artificial pupil. The Shack-Hartmann wavefront sensor has a square array of 1024 lenslets. The wave-aberration measurements are made at a wavelength of 850 nm. The deformable mirror is a correcting system composed of 52 independent magnetic actuators used to either partially or totally correct for the eye's aberrations up to the 5th order (18 Zernike coefficients)11 or to add certain aberrations. The control of the deformable mirror's surface is accomplished by means of a commercially available program (HASO CSO™, Imagine Eyes), which reshapes the deformable mirror from its normally flat surface to the desired shape.
The observer viewed the generated visual tests on a microdisplay, through the adaptive optics system and a 5.5mm artificial pupil. The microdisplay subtended a visual angle of 114×86 arcmin, with a resolution of 800×600 pixels (pixel size = 0.143 arcmin). Its mean luminance was 42 cd/m2, corresponding to a retinal illuminance of 1000 Td for a 5.5mm pupil diameter.
The adaptive optics system required precise alignment of the subject's pupil with the optical axis of the set-up (i.e., with the wavefront sensor and the deformable mirror). The pupil size and position was monitored using a CCD camera. The control handwheel of the CRX1™ system permitted to maintain the pupil position providing a quick, smooth and fine adjustment. The subject's pupil was not artificially dilated since the experiments were performed in dim surrounding illumination, providing pupil diameter values above 5.5mm and avoiding reflections.
Condition A: Correcting the Wavefront AberrationMonochromatic aberrations up to the 5th order were dynamically compensated using a closed-loop system working at 1Hz that comprised a double pass of light through the eye. The mirror is continuously reshaped so that the total (eye-device) aberration encountered along the line of sight is minimized. The most accurate retinal images of the visual-performance tests are provided by these dynamically adjusting wavefronts, which enable the compensation of small eye decentration and variations due to the tear film or accommodation. We measured the visual performance of the KC and “normal” eyes during the correction of their monochromatic aberrations.
Condition B: KC Eyes’ Higher-order AberrationsThe spherical error of the usual refractive correction (i.e. spectacle correction) was introduced using a Badal optometer and the spectacles’ astigmatism was simulated aided by the deformable mirror. These values were kept constant, independently of the wavefront fluctuations that may occur in the eye during the visual tests, in order to simulate usual spectacle correction. We measured the residual aberrations (uncorrected second-order aberrations + higher-order aberrations) of each KC eye after second-order aberration compensation with their usual refractive correction.
In order to demonstrate a possible adaptation of KC eyes to their particular aberration pattern, we assessed the visual performance of “normal” eyes under the same aberration conditions. First of all, the “normal” eyes’ aberrations were dynamically corrected by means of the adaptive optics system. Additionally, to simulate the vision of KC eyes, we reshaped again the deformable mirror to induce the measured residual aberrations of each KC eye (i.e., uncorrected second-order aberrations + higher-order aberrations). Then, we assessed the visual performance of each “normal” eye while viewing through the aberration pattern of each of the 6 KC eyes.
We assumed that the spectacles’ defocus term of each KC eyes was their preferred subjective defocus value. Consequently, we took this spherical error as equivalent to the defocus value subjectively adjusted by the “normal” subjects by means of the deformable mirror when viewing a 0.8 logMAR-E-letter through the residual aberrations of each KC eye (i.e. astigmatism + higher-order aberrations). Since KC eyes were not necessarily optimally corrected, we added to the subjectively optimized defocus value (DNEAdjust), a factor (ΔKCEObj−Spec) equal to the defocus difference between the objective value (i.e., the defocus term of the aberration measurement) and the spectacles’ defocus term. So, “normal” eyes viewed through a defocus term (DNE) defined as follows:
The average value of this additional factor (ΔKCEObj−Spec) was equal to 0.20 D, which implies that the defocus adjustment determined by the “normal” eyes was comparable to the spectacles defocus term of KC eyes (i.e., their subjective adjustment).
Measuring the Visual PerformanceThe 10, 15 and 20 c/deg CS was measured using a 4 alternative forced-choice method. Oriented sinusoidal gratings (at 0°, 45°, 90° and 135°) were randomly generated and displayed on the microdisplay. A modified best PEST (Parameter Estimation by Sequential Testing) method12 based on 30 presentations was used to determine contrast thresholds. The sine-wave gratings were truncated by a windowing function consisting of a circular window subtending a visual angle of 1° surrounded by a sinusoidal function subtending a visual angle of 0.14° to smooth the field's edge. The presentation time of each grating was 500ms. The subject indicated the grating orientation by pressing the appropriate button on a numerical keypad. For each spatial frequency, 3 CS measurements were performed and the average was retained.
We measured the high-contrast VA using the Freiburg visual Acuity Test (FrACT) software.13 The acuity threshold was also determined through a best PEST procedure based on 30 presentations. The test used an 8 alternative forced-choice method. The subject's task was to identify the Landolt-C's gap position, indicating it by means of a keypad. The VA value that was retained was the average of the 3 measurements.
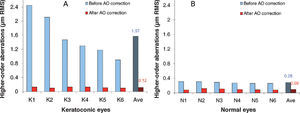
ResultsCondition A: Correcting the Wavefront AberrationFigure 1 shows the RMS associated to higher-order aberrations both before and after the dynamic correction of the aberration pattern of KC eyes and “normal” eyes. The average RMS (associated to higher-order aberrations over a 5.5mm pupil) was 1.57±0.59μm, and ranged from 0.90 to 2.45μm among KC eyes. Regarding “normal” eyes, the RMS before adaptive-optics correction, equal to 0.28±0.02μm, was similar for all subjects. After dynamic correction of the eye's aberrations, the average RMS (again, that associated to higher-order aberrations over a 5.5mm pupil) was reduced to 0.12±0.02μm and to 0.09±0.02μm for KC and for “normal” eyes, respectively. These results indicate that both groups achieved comparable levels of aberration correction (P>0.10).
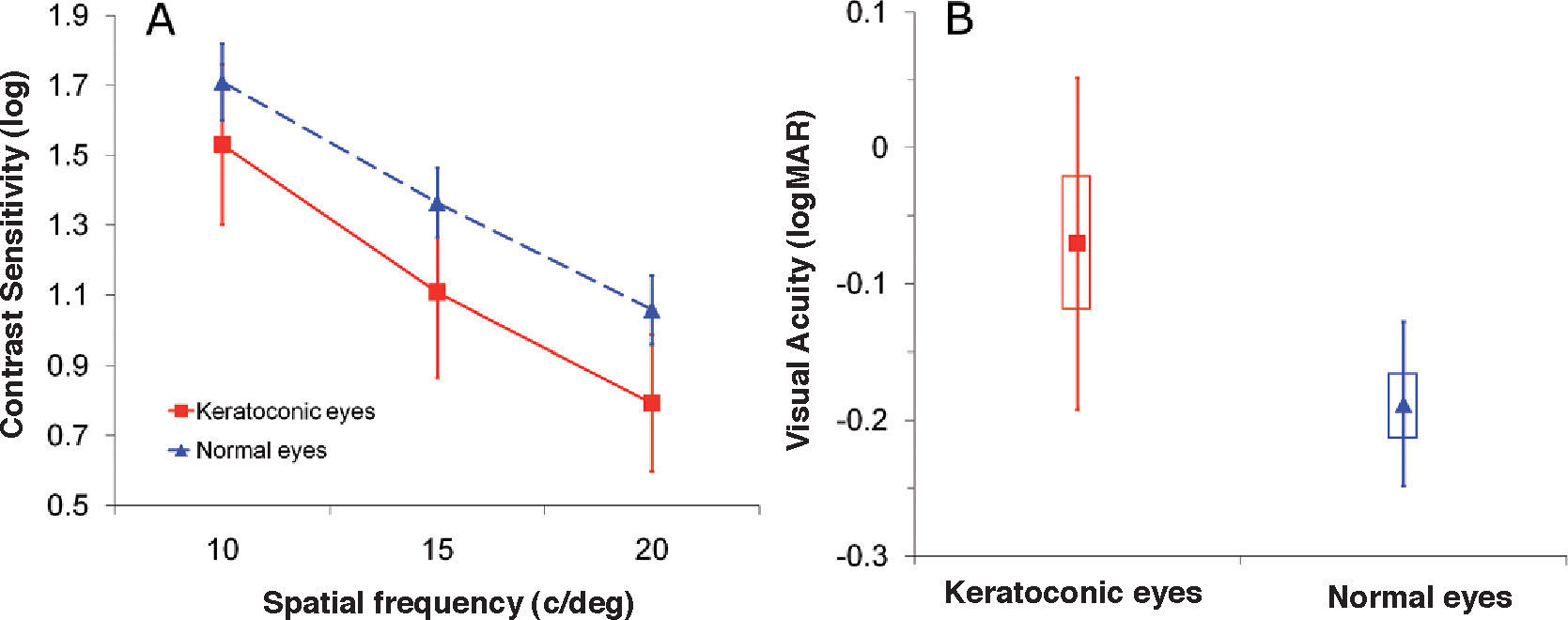
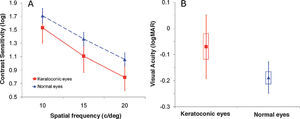
Figure 2 shows the average visual performance of the KC eyes and “normal” eyes, measured after dynamic correction of the aberrations. The visual performance was lower for the KC eyes than for “normal” eyes: the average difference between the 2 groups was 0.24 log units and 0.12 logMAR, in terms of CS and VA respectively. The measured visual performance showed larger interocular variations within the KC group, compared to the “normal”eyes group.
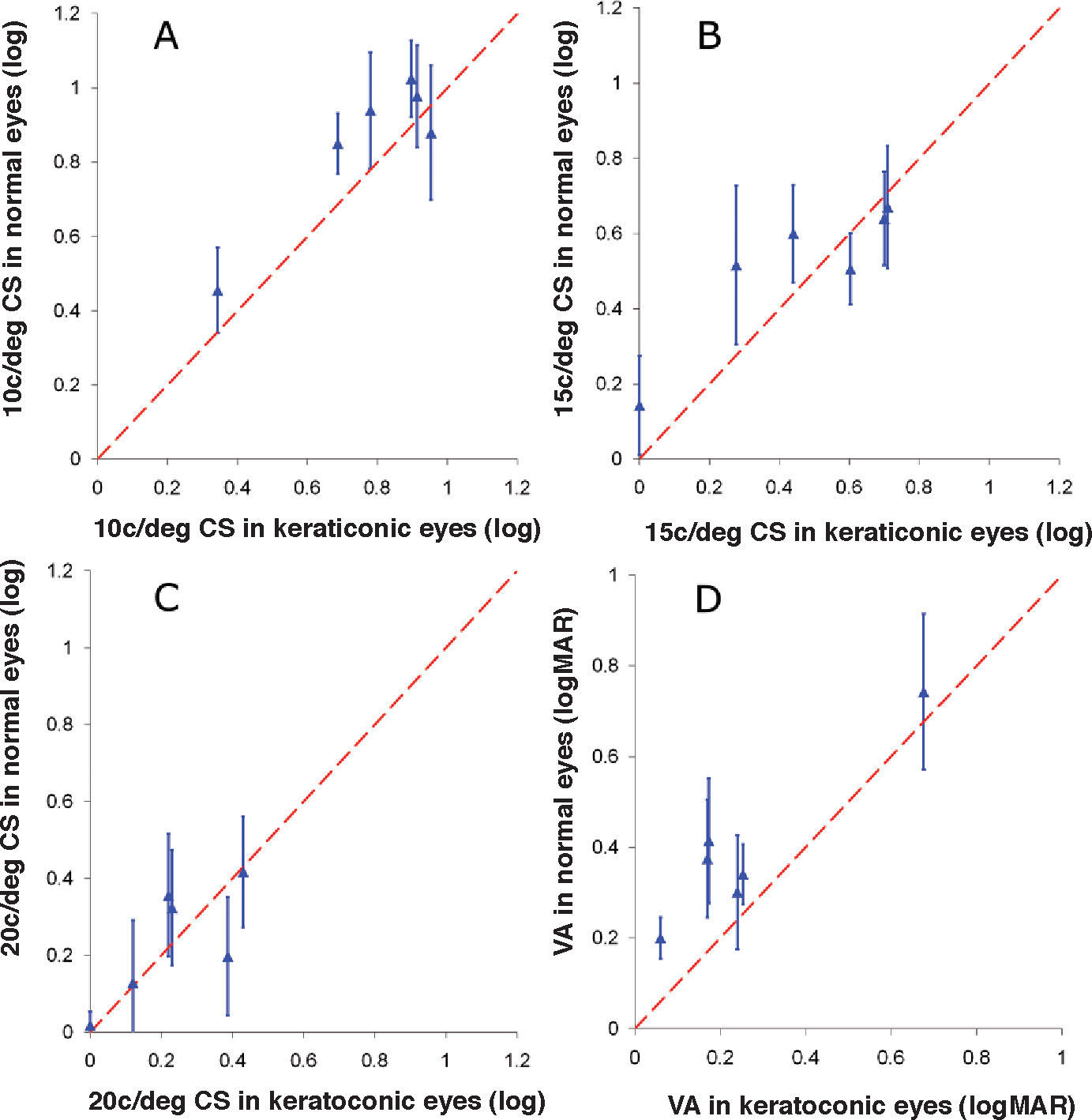
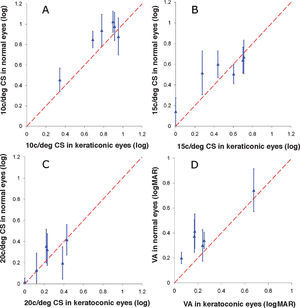
Condition B: KC Eyes’ Higher-order AberrationsFigure 3 shows the average visual performance of “normal” subjects, for each simulated KC eye, as a function of the 6 KC eyes’ visual performance when viewing through their usual aberration pattern. KC and “normal” eyes were under the same aberration conditions (i.e., uncorrected secondorder aberrations + higher-order aberrations of the corresponding KC eye). Dashed lines correspond to equal-CS and equal-VA lines between KC and “normal” eyes.
Averaged 10, 15, 20 c/deg contrast sensitivity (A, B, C) and high-contrast visual acuity (D) measured in “normal” subjects for each KC eye aberration pattern, as a function of KC eye’ visual performance. Dashed lines represent equal visual performance lines between KC and “normal” eyes. Error bars correspond to standard deviations between subjects.
Whatever the spatial frequency was, the CS of “normal” subjects was always slightly better than that measured in KC eyes (with an average difference of 0.05 log units). The difference was larger at 10 c/deg (0.09 log units) than at 20 c/deg (0.01 log units).
On the contrary, KC eyes always showed a better VA than “normal” eyes (with an average difference of 0.13 logMAR).
DiscussionDuring dynamic correction of the eye's aberrations (i.e., condition A), KC and “normal” eyes showed comparable amounts of residual aberrations (see Figure 1). The adaptive optics correction can provide a retinal image with a very high quality (i.e., an RMS of around 0.10μm for a 5.5mm pupil size) both in KC and “normal” eyes, irrespective of the initial magnitude of the aberrations. This average residual level of aberrations was comparable to the values obtained by Sabesan et al.14 and Sabesan and Yoon (Sabesan R, et al. IOVS 2009;50: ARVO E-Abstract 3048) (0.09μm for a 6mm pupil size) and by Yoon (Yoon G. IOVS 2009; 50: ARVO E-Abstract 2030) (0.10μm for a 6mm pupil size), who also compensated KC and “normal” eyes’ aberrations using an adaptive optics system.
During the dynamic correction of the higher-order aberrations of KC eyes, we measured an average VA of 0.07 logMAR (see Figure 2). This VA was comparable to the 0.08 logMAR obtained by Sabesan and Yoon10 (average across 4 KC eyes) and to the value of 0.07 logMAR obtained by Yoon (Yoon G. IOVS 2009; 50: ARVO E-Abstract 2030) (average across 8 KC eyes). However, Rocha et al. (Rocha KM, et al. IOVS 2009;50: ARVO E-Abstract 3049) measured an average VA of 0.36 logMAR (across 12 KC eyes). The initial RMS associated to higher-order aberrations of the KC eyes was comparable among studies: 1.57μm for a 5.5mm pupil diameter in our study, 1.36μm for a 6mm pupil diameter in Sabesan and Yoon's10 and 1.88μm for a 6mm pupil diameter in Rocha et al.’s (Rocha KM, et al. IOVS 2009;50: ARVO E-Abstract 3049); Yoon (Yoon G. IOVS 2009;50: ARVO E-Abstract 2030) did not provide this value. The static correction procedure used by Rocha et al. (Rocha KM, et al. IOVS 2009;50: ARVO E-Abstract 3049) to compensate the aberrations could explain why they obtained worse VA values.
Like Sabesan and Yoon10 and Yoon (Yoon G. IOVS 2009; 50: ARVO E-Abstract 2030), we measured a better visual performance in “normal” eyes than in KC eyes during dynamic correction of the eye's aberrations. We obtained a lower CS (with a difference of 0.23 log units) and a lower VA (with a difference of 0.12 logMAR) for KC eyes than for normal subjects. Sabesan and Yoon10 and Yoon (Yoon G. IOVS 2009; 50: ARVO E-Abstract 2030) obtained a VA difference between KC and “normal” eyes of 0.16 logMAR and 0.19 logMAR, respectively.
Recently Yoon (Yoon G. IOVS 2009;50: ARVO E-Abstract 2030) computed the theoretical VA of 8 KC eyes and 8 “normal” eyes based on the residual aberrations obtained after aberration correction; a neural contrast sensitivity function (NCSF) previously published was also included in their model. He found that the calculated VA was better than the measured VA, while no difference was found between calculations and measurements in “normal” eyes. Based on this fact, he concluded that there was a long-term visual adaptation of KC eyes to their blurred image quality. However, the fact that KC eyes showed worse visual performance than “normal” eyes after aberration correction and that the visual benefit of correcting higher-order aberrations was not well predicted by optical theory was not sufficient to claim that there is a visual adaptation of KC eyes to their usual aberrations. Indeed, the limited visual performance of KC eyes could also be explained by a poorer neural processing (NCSF) of KC subjects.
When viewing through a KC eye aberration pattern (i.e., condition B), visual performance differences also occurred between KC and “normal” eyes (Figure 3). The VA of KC eyes was always better than the VA measured on “normal” subjects (with an average difference of 0.13 logMAR). Sabesan and Yoon (Sabesan R, et al. IOVS 2009;50: ARVO E-Abstract 3048) obtained similar results (an average difference of 0.12 logMAR) when measuring VA in 3 “normal” eyes viewing through 4 KC eye aberrations. This difference in terms of VA between KC and “normal” eyes could be explained by the presence, in KC eyes, of a compensation mechanism that makes up for the poor retinal image quality by improving the post-receptor treatment. Some authors2-5 had previously measured a significant improvement of VA after exposure to optical blur induced by defocus for several minutes (ranging from 30 to 180min), which suggests the possible existence, for VA-related tasks, of neural adaptation to a blurred retinal image.
However, for “normal” eyes we obtained a slightly higher CS (with an average difference of 0.05 log units) than for KC eyes, meaning that no adaptation occurred in terms of CS. To explain this difference, one can argue that, due to their poor optical quality, KC eyes never experienced such “higher” spatial frequencies (i.e. 10, 15 and 20 c/deg), thus excluding the possibility of a neural adaptation. However, our results (Figure 2) showed a better CS in “normal” eyes at 10 c/deg (with a difference of 0.09 log units) than in KC eyes, whereas the average 20 c/deg CS was comparable between the 2 groups.
The adaptation of KC eyes to their retinal image should be mainly related to the demands of everyday visual tasks. Indeed, the VA test we used, which is close to reading, was more comparable to a real-life task than the CS test, which involves detecting sinusoidal gratings. Besides, if VA was measured using sinusoidal gratings, VA differences between KC and “normal” eyes may not be so important. The results obtained by George and Rosenfield4 confirmed this hypothesis, since they did not measure a significant increase in VA (0.03 logMAR) when using sinusoidal gratings after a 2-hour period of +2.50 D induced defocus, whereas they observed a VA difference of around 2 lines when measuring VA with a Landolt-C optotype.
Moreover, the VA task we used in this study, entailing the detection of the Landolt-C's gap orientation, required a more complex neural process in the visual cortex than the contrast detection required by the CS task.
Improvement of the VA due to the compensation mechanism occurring at the post-receptoral stage of the KC eye's visual system seems to raise the hypothesis of an adaptation occurring in deeper neural stages.
Sabesan and Yoon (Sabesan R, et al. IOVS 2009;50: ARVO E-Abstract 3048) observed that the VA difference between “normal” and KC subjects was correlated with the initial amount of higher-order aberrations in KC eyes. The poorer the retinal image was (i.e., the higher the level of higher-order aberrations), the greater the difference in terms of VA.
On the contrary, Rosenfield et al.5 didn’t observe any difference (in terms of VA improvement) among 22 myopic subjects measured after a 3-hour period without their refractive compensation. The results were plotted as a function of the initial level of myopia (which ranged from -1.00 to -3.50 D). Similarly, we did not observe a correlation between the amount of higher-order aberrations of KC eyes and the neural compensation (i.e., VA difference between KC subjects and “normal” subjects viewing through the aberration pattern of the KC eyes).
This neural adaptation may also explain the recent results of Legras et al.,15 who succeeded in predicting the visual benefit in terms of contrast sensitivity (r2=0.79) when correcting the monochromatic aberrations of 25 subjects, but failed to predict the improvement in terms of visual acuity (r2=0.30), where the predicted values were higher than the measured ones. This is due to measured visual acuities being better with the sphero-cylindrical correction, indicating that the subjects could be adapted to their own retinal image.
In conclusion, compared to “normal” eyes, KC eyes showed poorer visual performance with the same optical image quality but better VA when wearing their usual sphero- cylindrical correction, suggesting that KC eyes may be adapted to their poor retinal image quality. However, when measuring visual performance with a test that is less comparable to real life and less complex (i.e. CS measurement), KC and “normal” subjects produced comparable results. Consequently, a hypothetical neural adaptation might only occur for usual “real life” visual tasks.