The Adaptation to Age-related Vision Loss (AVL) scale was developed to measure the adjustment of older adults who are adapting to late-life vision loss. The purpose of this study was to assess whether the AVL scale satisfies the Rasch model in a cataract population.
MethodsThe 24-item AVL scale (18 negatively and 6 positively coded) was mailed to 436 cataract patients for self-administration whilst they were on the waiting list for cataract surgery at the Flinders Eye Centre, Adelaide, South Australia. Rasch analysis was performed to determine whether the items were measuring a single construct (unidimensionality) as examined with fit statistics and principal components analysis (PCA) of the residuals. The ability of the scale to distinguish between the levels of adaptation of the participants (person separation) was investigated, with a value ≥2.0 established as the minimum acceptable.
ResultsThe AVL scale was unable to differentiate sufficiently between participants’ levels of adaptation, indicating poor person separation. One item did not fit the construct, causing misfit. Furthermore, the five positively worded items did not appear either to measure the same construct as other items, resulting in lack of unidimensionality evidenced by PCA. Following the deletion of these items, the AVL scale was one-dimensional but a single item continued to misfit, so it had to be deleted, resulting in an 18-item AVL scale. Even so, the discriminating abilities of the scale continued to be poor.
ConclusionsThe AVL scale is not an appropriate measure of adaptation to vision loss in a cataract population.
La Escala de adaptación a la pérdida visual relacionada con la edad (o sus siglas en inglés, AVL) se desarrolló para medir el ajuste de los adultos de edad avanzada ante la pérdida visual que suele aparecer en esta fase de la vida. El propósito de este estudio era evaluar si la escala AVL también se ajusta al modelo de Rasch en una población de personas con cataratas.
MétodosSe envió por correo postal el cuestionario correspondiente a la escala AVL de 24 elementos (18 codificados negativamente y 6 positivamente) a 436 pacientes del Flinders Eye Centre, Adelaida, South Australia (Australia) que se encontraban en la lista de espera para cirugía de cataratas. Los pacientes debían completar el cuestionario y devolverlo por correo. Se realizó un análisis de Rasch de los resultados para determinar si todos los elementos de la escala están midiendo un único parámetro (unidimensionalidad). Esto se llevó acabo utilizando estadísticos de ajuste así como análisis de componentes principales (o sus siglas ACP) de los residuos. Se evaluó la capacidad de la escala para discriminar entre los distintos niveles de adaptación de los participantes (denominada separación o fiabilidad), estableciendo un valor umbral de 2,0 como el valor mínimo aceptable.
ResultadosLa escala AVL no fue capaz de diferenciar de forma aceptable entre los distintos niveles de adaptación de los participantes, dando lugar a una mala separación (poca fiabilidad). Uno de los elementos no se ajustaba al parámetro, dando lugar a un desajuste. Además, los cinco elementos enunciados de manera positiva tampoco parecían medir el mismo parámetro que el resto de elementos, dando lugar a una falta de unidimensionalidad, puesta de manifiesto por medio del APC. Tras la eliminación de estos elementos, la escala AVL logró ser unidimensional, pero uno de sus elementos siguió sin ajustarse al modelo, por lo que hubo que eliminarlo, dando lugar finalmente a una escala AVL de 18 elementos. Incluso así, la facultad de la escala para discriminar entre grupos de participantes siguió siendo bastante deficiente.
ConclusionesLa escala AVL no es una forma adecuada de medir la adaptación a la pérdida visual en una población compuesta por personas con cataratas.
Patient-reported outcomes (i.e., questionnaires or scales) are increasingly being used in ophthalmology to evaluate the effectiveness of treatments, including cataract surgery.1-4 While several visual function questionnaires have been developed for this purpose, some of these have, however, been used in other disease groups as well.5-7 For example, the Visual Function-14 questionnaire (VF-14) was developed to measure functional limitations caused by cataract and the outcomes of cataract surgery,7 but has been shown to be valid in retinal diseases and glaucoma too.8,9 Another questionnaire, the Impact of Vision Impairment questionnaire (IVI), was developed to assess the participation in daily activities by visually impaired individuals.7,9-11 Recently, using Rasch analysis, three subscales of the IVI (accessing information, mobility and independence and emotional well being) were shown to be valid in a cataract population too.10 This adaptability suggests that such questionnaires could potentially be administered to populations other than the one they were validated for, provided the validity of these questionnaires has been demonstrated in these other populations also. The excellent performance of the IVI in a cataract population encouraged us to assess in this population the performance of another questionnaire specifically developed for elderly people with vision loss: the Adaptation to Age-related Vision Loss Scale (AVL).11
The AVL scale was developed to meet an identified need in the field of vision rehabilitation: to assess the psychosocial adaptation of elderly people to vision loss. Strong psychometric properties have been reported for the AVL scale.11 A shortened version of the AVL scale (i.e., AVL 12) has also been proposed recently with sound psychometric properties.12 Although the reliability and validity of the AVL scale had been previously demonstrated, this was carried out using traditional classical test theory (CTT).15,16 A major criticism of this method is that the scoring (and, thus, the interpretation) is based on ordinal-level data.1,13,14 Modern psychometric models, specifically Rasch analysis, offer several advantages over CTT, including the important property of invariance: this means that the item parameters and person estimates do not depend either on the items administered or on the people to whom the questionnaire is administered.18-20 Currently, Rasch analysis is being used to develop new measures21-23 and to evaluate existing ones (for example, IVI24 and VF-1415) to determine whether or not the assumptions of the Rasch model are met. The AVL scale has not yet been examined using Rasch analysis. While the AVL scale was developed to assess the adaptation to vision loss resulting from chronic ocular conditions such as age-related macular degeneration (ARMD), other conditions such as cataract cause vision loss, albeit temporarily until surgery. Depending on the country or on the particular region within a given country, the length of the waiting list is variable and patients may have to wait for a considerable amount of time (average waiting period = 3-4 months at our centre) before undergoing cataract surgery. In the intervening period, therefore, patients would have to learn to adapt to their vision loss (which is not as severe in magnitude as with ARMD). In this context, we wanted to investigate if adapting to vision loss was a cause of concern in our cataract population. Therefore, the aim of the present study was to establish whether or not the AVL scale fits the stringent requirements of the Rasch model for the measurement of the adaptation to vision loss in patients with cataract.
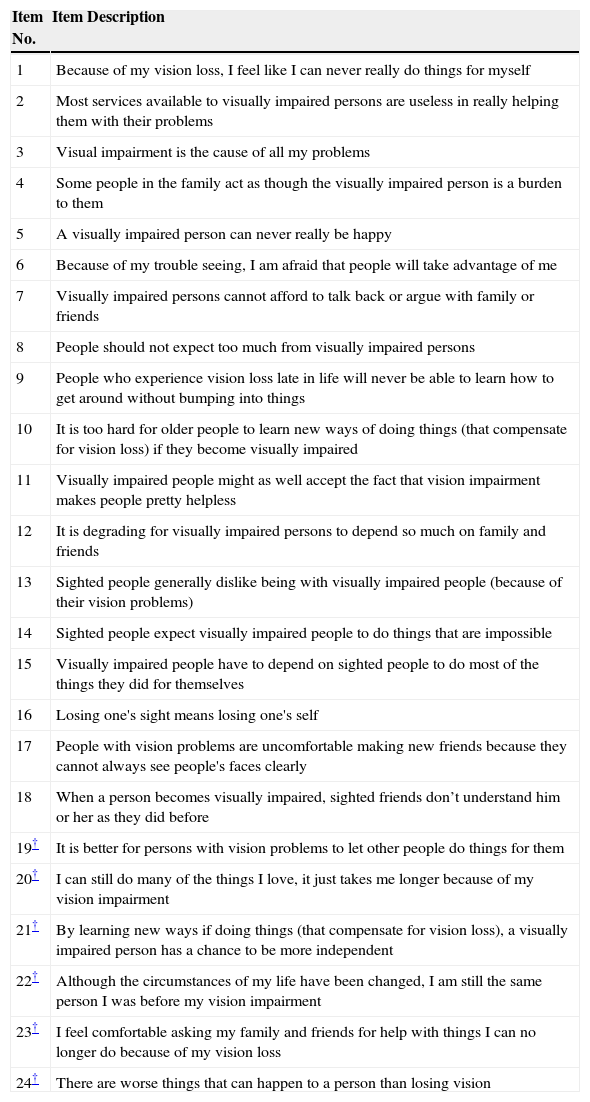
MethodsInstrumentAdaptation to Age-related Vision Loss ScaleTable 1 contains the 24 statements (known as “items”) of the AVL scale.11 All items are scored dichotomously (0 = agree, 1 = disagree). However, an additional ‘don’t know’ category is provided for each item and such responses are treated as missing data in the Rasch analysis. A majority of items (19) are negatively worded; in those cases a higher score reflects a better adaptation. However, to avoid the possibility of an acquiescence response set, 5 items are positively worded, and for them a higher score reflects a poorer adaptation. All positively worded items were re-coded prior to data analysis, so that for all items higher scores always suggested a better adaptation.
Item content of the Adaptation to Age-related Vision Loss Scale
| Item No. | Item Description |
| 1 | Because of my vision loss, I feel like I can never really do things for myself |
| 2 | Most services available to visually impaired persons are useless in really helping them with their problems |
| 3 | Visual impairment is the cause of all my problems |
| 4 | Some people in the family act as though the visually impaired person is a burden to them |
| 5 | A visually impaired person can never really be happy |
| 6 | Because of my trouble seeing, I am afraid that people will take advantage of me |
| 7 | Visually impaired persons cannot afford to talk back or argue with family or friends |
| 8 | People should not expect too much from visually impaired persons |
| 9 | People who experience vision loss late in life will never be able to learn how to get around without bumping into things |
| 10 | It is too hard for older people to learn new ways of doing things (that compensate for vision loss) if they become visually impaired |
| 11 | Visually impaired people might as well accept the fact that vision impairment makes people pretty helpless |
| 12 | It is degrading for visually impaired persons to depend so much on family and friends |
| 13 | Sighted people generally dislike being with visually impaired people (because of their vision problems) |
| 14 | Sighted people expect visually impaired people to do things that are impossible |
| 15 | Visually impaired people have to depend on sighted people to do most of the things they did for themselves |
| 16 | Losing one's sight means losing one's self |
| 17 | People with vision problems are uncomfortable making new friends because they cannot always see people's faces clearly |
| 18 | When a person becomes visually impaired, sighted friends don’t understand him or her as they did before |
| 19† | It is better for persons with vision problems to let other people do things for them |
| 20† | I can still do many of the things I love, it just takes me longer because of my vision impairment |
| 21† | By learning new ways if doing things (that compensate for vision loss), a visually impaired person has a chance to be more independent |
| 22† | Although the circumstances of my life have been changed, I am still the same person I was before my vision impairment |
| 23† | I feel comfortable asking my family and friends for help with things I can no longer do because of my vision loss |
| 24† | There are worse things that can happen to a person than losing vision |
The study population has been described previously.10,16 Participants were 436 cataract patients drawn from the waiting list for cataract extraction surgery in either their first (58.2%) or their second eye at the Flinders Medical Centre, Adelaide. These participants were mailed the AVL scale for self-administration and they returned the completed AVL scale in a prepaid envelope. Inclusion criteria were as follows: aged 18 or older, spoke English without the need for an interpreter and had no severe cognitive impairment. As it is typical within a cataract population, patients with co-existing systemic and ocular conditions were included. The mean patient age was 74.0 years (SD=9.3) and 54.8% of them were female. The mean binocular visual acuity was 6/9.5-1. Three hundred and twelve patients (71.6%) had systemic co-morbidities and 203 of them (46.6%) had ocular comorbidities. Ethical approval was obtained from the Flinders Clinical Research Ethics committee and all participants provided informed consent. The study was conducted in accordance with the tenets of the Declaration of Helsinki.
Rasch AnalysisRasch analysis17 was conducted using the Andrich rating scale model18 with Winsteps software (version 3.68) J.M Linacre, Chicago, Illinois, USA.19 Rasch analysis transforms ordinal scores into a logit (i.e. log odds) scale and allows for interval-level measurement. Four fundamental indicators were used to evaluate instrument quality.20 These included (i) fit, or the extent that items in the AVL scale measured a single construct (i.e., unidimensionality), (ii) item difficulty, or the hierarchical ordering of tasks from ‘difficult to endorse’ (i.e., difficult to agree with) to ‘easily endorsed’ (i.e., easy to agree with) items in the case of the AVL scale, (iii) targeting, or the extent to which the set of items is of appropriate endorsability (i.e. level of agreement or disagreement) for the level of participant's adaptation, and (iv) separation, or the extent to which the items distinguish distinct levels of adaptation within the participants. A participant who has adapted well to his/her vision loss would find it difficult to agree with most of the items (i.e. would choose the ‘disagree’ option) and, therefore, would have a higher logit score.
Fit (or misfit) was indicated by the infit mean square (MnSq) statistic, which denotes the extent to which participant's ratings deviate from expectation. A value greater than 1.3 was considered a misfit, and indicates that the item is measuring something different to the rest of the items, violating the fundamental principle of unidimensionality.21 Furthermore, when items fit the model's expectations, the residuals22 (observed minus expected scores) should be randomly distributed with all meaningful variance in the data being accounted for by the Rasch dimension of item endorsability-participant's adaptation to vision loss. In practice, however, some inter-item correlations typically remain and principal components analysis (PCA) describes the additional factors that may be extracted from the data.23-25 When this occurs, it indicates that something other than the main construct is being measured, which will interfere with the measurement of the primary construct. The cut-off used to assume that an item was loaded on a given factor was 0.3. A variance of 60% or greater accounted for by the first factor (i.e., dimension) was considered to be the minimum-acceptable level.26 Additional contrasts with eigenvalues > 2.0 were considered as violations of unidimensionality.
Item difficulty or hierarchy refers to the distribution of the items from the most to the least difficult on the personitem map. Winsteps software provides this map, which also helps in identifying gaps and redundancies in the item distribution so that appropriate items can be added to fill the gaps and redundant items can perhaps be deleted.
It is important to ascertain how well the instrument is targeted (i.e. how well the item endorsability matched the participant's adaptation to vision loss). A good measure should be able to differentiate persons across the full spectrum of adaptation to vision loss in the population.27 Therefore, the instrument requires items to vary in endorsability over the full range of participant's adaptation to vision loss. Rasch analysis illustrates the targeting of item endorsability to participant's adaptation to vision loss in the person-item map, and reports the difference in targeting between items and participants in terms of the difference in means. Ideal targeting exists when the mean of items equals the mean of persons;27,28 the greater the difference between these means, the poorer the targeting.27
The person separation statistic indicated the extent to which the AVL scale could distinguish persons according to their level of adaptation. A value of 2.0 was considered to be the minimum acceptable.27
ResultsThe use of the ‘don’t know’ category ranged between 9% (item No. 1) and 55% (item No. 2) among the participants.
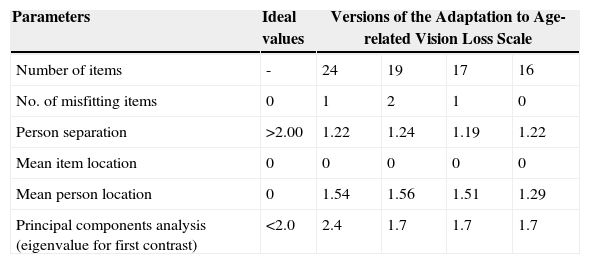
The person separation was poor, indicating that the AVL scale was unable to distinguish between desired strata (i.e., at least three) of participant ability (see Table 2). One item (item No. 2) was a misfit, violating the first requirement for unidimensionality. This was further supported by PCA of residuals, which, with an eigenvalue of 2.4 for the first contrast, indicated multidimensionality. The pattern of positive and negative item loadings in the first contrast defined two dimensions, with the five positively worded items comprising half of the items in the “positive dimension”. In an attempt to restore unidimensionality, it was essential that the second dimension, consisting of these five items, was removed and, as a result, these items were deleted. The only way to maintain items from a second dimension is to treat them as a separate scale. Upon testing, these items did not form a separate valid scale (person separation = 0.0). The deletion of the five items left 19 items for further analysis. The items were also poorly targeted to this population. A mean person ability of 1.56 logits indicates that many of the participants did not endorse any of the items as representing issues for them.
Overall performance of all versions of the Adaptation to Age-related Vision Loss Scale
| Parameters | Ideal values | Versions of the Adaptation to Age-related Vision Loss Scale | |||
| Number of items | - | 24 | 19 | 17 | 16 |
| No. of misfitting items | 0 | 1 | 2 | 1 | 0 |
| Person separation | >2.00 | 1.22 | 1.24 | 1.19 | 1.22 |
| Mean item location | 0 | 0 | 0 | 0 | 0 |
| Mean person location | 0 | 1.54 | 1.56 | 1.51 | 1.29 |
| Principal components analysis (eigenvalue for first contrast) | <2.0 | 2.4 | 1.7 | 1.7 | 1.7 |
Although unidimensionality was restored through the deletion of the above-mentioned items, the person separation continued to remain below acceptable levels (1.24). Again, the previously misfitting item (No. 2, infit MnSq, 1.51) was still a misfit, as was an additional item, (No. 19, infit MnSq 1.32). This misfit indicated that they were not in tandem with the rest of the items in contributing to the measurement of underlying trait. So these items were deleted, one at a time, starting with the most misfitting item; i.e., item No. 2. Thus, 17 items remained. However, there was yet another item that misfited (item No. 8, infit MnSq 1.34), which required deletion. Finally, 16 items remained that fited the Rasch model; i.e., that exhibited infit MnSq values within the desired range (0.7-1.3). Person separation, however, failed to improve (1.22) (see Table 2). This indicates that further revision was not going to result in a valid instrument.
DiscussionThe AVL was developed to measure adjustment to latelife or age-related vision loss in elderly people. Considering cataract is one of the leading causes of vision loss worldwide, we hypothesized that the AVL scale would be suitable for the assessment of adaptation to vision loss in an elderly population currently awaiting cataract extraction. However, the results from the present study indicate that the AVL scale failed to meet the expectations of the Rasch model in this cataract population.
Two fundamental problems surround the use of the AVL scale in this cataract population. First, there was poor person separation, which indicated that the scale was unable to discriminate among the various levels of adaptation to vision loss. This may partly be related to the use of the dichotomous rating scale. It has also been suggested that dichotomous rating scales are disliked by older patients because they are too restrictive.29 A polytomous rating scale is likely to provide greater information about the construct hierarchy, as has already been achieved for the shortened version, the AVL12.12 An added reason for the poor discriminating abilities of the AVL scale could be related to the lack of variation in the levels of adaptation among the participants, with a majority of our participants suffering from only mild visual impairment (mean binocular visual acuity = 6/9.5-1). The content of the items in the AVL scale reveals that they appear to be better suited to the severely visually impaired population. Thus it is likely that the AVL scale may function differently (perhaps better) in another cataract population that is more severely impaired, for instance, in regions such as Africa where the threshold for cataract surgery is lower than that in Australia.30
In comparison with chronic conditions that result in visual impairment, such as age-related macular degeneration, ocular disorders such as cataract cause only temporary vision loss, reversible through surgery. Recent advances in surgical techniques coupled with heightened awareness regarding the benefits of cataract surgery mean that cataract patients can expect surgery to restore their vision to preoperative levels.31 Thus, these patients often have no long-term concerns regarding their vision loss. Such a belief may have resulted in an extreme scoring pattern, leading to a large ceiling effect. The average participant had higher logit score (mean = 1.54, see Table 2) as he/she disagreed with most of the items, indicating a better adaptation to vision loss. This could mean that these participants with cataract didn’t have significant visualrelated problems. However, all cataract patients were drawn from the cataract-surgery waiting list, and the key indicator for cataract surgery is, precisely, visual disability attributed to cataract.32-34 Therefore, this population, by definition, does have visual disability, a fact that was also previously demonstrated.35
A lack of unidimensionality was a second limitation of the AVL scale in the present study. Unidimensionality is a fundamental requirement of the Rasch model. Indeed, recent observations that even slight multidimensionality can affect person estimates have further emphasized the importance of unidimensionality as a measurement property of a questionnaire.36 A lack of unidimensionality was being caused by the five items that were positively coded in the AVL scale, indicating that they did not appear to measure the same underlying construct as the rest of the items. However, the actual content of these items does not appear to be drastically different from the rest of the items and offers no immediate suitable explanation for their multidimensional behavior. Nevertheless, it is likely that some participants may have got used to disagreeing with most of the negatively worded items in the first half of the questionnaire (i.e., items 1-18) and that, as a result, they would have misread the positively worded items (i.e., items 19-24) in the latter half, resulting in unexpected responses. While the authors of the AVL scale coded the five items differently from the rest of the items to deter an acquiescence response set, it may have proved to be counter-productive. The most misfitting item was item No. 2, related to services for the visually impaired. Items misfited for a variety of reasons, such as poor construction, and therefore they run the risk of being poorly understood or they may also be ambiguously worded. However, a more likely explanation in the present case would be related to missing responses to this item from a little over half of the participants (55%), indicating that a majority of the cataract patients may have been unaware of the services that exist for the visually impaired. In the original development of the AVL scale, as well as in its subsequent shortened version, the authors however, recommended the AVL scale to be best used as a unidimensional measure. Factor analytic techniques were used to examine unidimensionality during the original development of the AVL scale. Technically, these analyses require interval-scaled data, and not the ordinal data derived from questionnaires.11 Nevertheless, Rasch analysis can also make use of ordinal data, but the important difference is that it converts ordinal into interval-level data, which are used in the PCA of residuals. Consequently, Rasch analysis provides a sound approach to test the unidimensionality of a set of items that yield ordinal data.17 Although unidimensionality could finally be restored once the multidimensionality-causing items (i.e., the positively coded 5 items) were deleted from the AVL scale, the discriminating abilities (person separation) of this AVL scale failed to improve.
The results from the present study perhaps indicate that a questionnaire should only be used for the specific condition(s) for which the questionnaire has been developed and tested. However, as pointed out in the Introduction, questionnaires such as the VF-14 and the IVI, while originally developed for the cataract and for the visually impaired population, respectively, have also been shown to be valid in other disease groups.8-10 This is because both these questionnaires contain items related to visual disability or activity limitation, a characteristic common across ocular conditions, be it cataract or glaucoma. Similar to the IVI, the AVL was developed for the visually impaired population, but the contents vary significantly. The IVI, in addition to the activity limitation items, also contains items related to emotional well-being. This scale has been shown to be valid in the cataract population.10 In comparison, items in the AVL scale refer only to the adaptation to vision loss, an attribute that is more applicable to people with severe visual impairment and, therefore, which is not applicable to disorders such as cataract that result in rather mild vision loss, as it happens in our population.
In conclusion, the AVL scale is not a suitable instrument for the assessment of adaptation to vision loss in an Australian cataract population. Thus, as envisaged by the authors of the AVL scale themselves, the items may better suit older persons whose visual impairment is due to other age-related conditions (such as ARMD) that cause irreversible vision loss.
Sources of support: This work was supported in part by the National Health and Medical Research Council (Canberra, Australia), Centre of Clinical Research Excellence Grant 264620. Konrad Pesudovs is supported by the National Health and Medical Research Council (Canberra, Australia), Career Development Award 426765.
Financial disclosure: The authors have no personal financial interest in the development, production, or sale of any device discussed herein.