To determine the prevalence of astigmatism and its determinants in schoolchildren aged 6–12 years.
MethodsThe students selected by stratified cluster random sampling in Shahroud, north of Iran. Optometric examination included uncorrected visual acuity, refraction with autorefractometer, manifest refraction with retinoscopy followed by subjective and cycloplegic refraction (after two drops of cyclopentolate 1% with 5min interval were instilled in each eye).
A cylinder power ≥0.75diopter (D) in at least one eye was considered as astigmatism. The prevalence of astigmatism was reported based on a cylinder power higher than 0.50, 1.00, and 2.00D in cycloplegic refraction, followed by power vector analysis.
ResultsAfter applying the inclusion criteria, the data of 5528 children were analyzed. The prevalence of astigmatism was 16.7% (95% CI: 15.6–17.7) in total, 16.6% (95% CI: 15.2–18.0) in boys and 16.8% (95% CI: 15.2–18.3) in girls (p=0.920) and decreased from 21.5% in 6-year-old children to 13.7% in 10-year-olds, and then again increased to 18.3% in children aged 12 years. Moreover, 17.2% (95% CI: 16.0–18.3) of urban and 12.1% (95% CI: 10.0–14.1) of rural children had astigmatism (p<0.001). The prevalence of with-the-rule, against-the-rule, and oblique astigmatism was 14.2%, 2.1%, and 0.33%, respectively. The mean cylinder power was −1.31, −0.46, and −0.44D in children with spherical myopia, emmetropia, and hyperopia, respectively (p<0.001). Urban students had a higher J0 and boys had a higher J45.
ConclusionThe prevalence of astigmatism in this study was lower than previous studies. Astigmatism prevalence was markedly higher in urban children.
Uncorrected refractive errors comprise 43% of visual impairment worldwide.1 Astigmatism is one of the most important refractive errors. Its prevalence is different in various parts of the world according to age, sex, ethnicity, and geographical location.2–6 Astigmatism is important from different aspects of vision and its development. First, it may cause different symptoms such as blur, asthenopia and headache.7,8 Second, the presence of marked astigmatism during the development of the visual system can cause meridional amblyopia in children.9,10 Finally, this type of refractive error may disturb emmetropization due to producing a blurred image on the retina.11,12 Other studies have shown that uncorrected astigmatism can result in the formation or progression of myopia, as well.11,13,14 Most changes due to astigmatism and its effects, especially its amblyogenic and myopigenic nature, are observed in individuals under 15 years of age.9,15,16
The prevalence of astigmatism has been reported 30–75% in different age groups.17–20 Few studies have been conducted in the age group 6–15 years worldwide. The prevalence of astigmatism is less than 25% in the majority of these studies.17,21–23 Similar studies have been conducted in Iran, as well. According to these studies, the prevalence of astigmatism in Iranian children was less than 20%.2,4,24 However, one study reported a prevalence of 45.3% in children aged 7–15 years,25 which is much higher than previous reports from Iran and other countries. The highest prevalence in this age range was about 42% in a study, conducted in China.26 Therefore, the reported prevalence from Iran is the highest prevalence in the world, and this study is among few studies that reported a prevalence of more than 25% in children below 15 years of age. A previous study in Shahroud showed that 1 in every 2 adults had astigmatism, which is a high prevalence in adults.27 It must be noted that when comparing different studies the criteria of astigmatism and the method and accuracy of measurement must be taken into account. The limited number of studies on astigmatism in children and its high prevalence in adults in Shahroud encouraged us to investigate the prevalence of astigmatism in Shahroud children. The results can be useful for prevention of astigmatism in children around the world. The aim of this study was to investigate the prevalence of different types of astigmatism in children aged 6–12 years old in an Iranian population.
MethodsThe primary school children of Shahroud, north of Iran, were sampled in this cross-sectional study which was performed in 2015. Considering the limited rural population, all rural students were invited to participate in the study, and a census was conducted in the villages. In urban areas, since the number of students varied in different schools, cluster random sampling was done. In general, there were 473 clusters in urban areas of which 200 were selected through systematic random sampling.28
After selecting the students and contacting their parents, they were invited to participate in the study. Among 6624 selected children, 5620 participated in the study. Upon receiving parental informed consent, the children were transported to the clinic for examinations on a preannounced day. All examinations were performed in one place. After applying the exclusion criteria, the final analysis was performed on the data of 5528 children. Having history of any ocular surgery (including intraocular, refractive, trauma and strabismus surgeries), having any inflammatory and infectious disease in the cornea and keratoconus were considered as exclusion criteria. Children with pathological myopia, high hyperopia, ptosis, tropia, congenital cataract and pterygium also removed from analysis. The eyes with sphere power higher than 6 diopter (high hyperopia) or lower than −10 diopter (pathological myopia) also removed for investigation of astigmatism with spherical refractive errors.
ExaminationsFirst, non-cycloplegic auto refraction was done for all students using the Nidek ARK-510A autorefractokeratometer (Japan) by an experienced operator. Then, the results of auto refraction were refined with the Heine Beta retinoscope (HEINE Optotechnic, Hersching, Germany) and MSD trial lenses (MSD Meniscus Trial Lenses, Italy). In each stage, first the right eye and then the left eye were examined and their results were recorded. Finally, subjective refraction was done for all patients and the result of subjective refraction with best corrected visual acuity was recorded. The subjective process in this study included different stages comprising starting spherical check, astigmatic refinement, monocular spherical endpoint, spherical equalization (bi-ocular balance) and finally binocular spherical endpoint. To refine cylinder, we applied Jackson cross-cylinder. First, axis orientation and then the power of cylinder was checked and refined.
After subjective refraction, three drops of cyclopentolate 1% with 5min interval were instilled in each eye. The refraction was performed using autorefractometer after half an hour from the instillation of the last drop.
DefinitionsIn this study, the cylinder power was recorded as a negative value. The cylinder power was calculated based on cycloplegic refraction. A cylinder power ≥0.75 diopter (D) in at least one eye was used to calculate the prevalence of astigmatism. Moreover, to show the severity of astigmatism, cylinder powers more than 1 and 2D in at least one eye were reported. With-the-rule (WTR) astigmatism was defined as a cylinder power of at least 0.75D with the axis falling between 1° and 30° or 150° and 180°. Against-the-rule (ATR) astigmatism was defined as a cylinder power of at least 0.75D with the axis falling between 60° and 120°.4,29 Other astigmatic children with a cylinder power of at least 0.75D who did not match the definitions of ATR and WTR astigmatism were categorized as having oblique astigmatism.
Since astigmatism has a vectorially nature and is defined by two variables of power and axis, vector analyses were conducted, as well. J0 vector which is the vertical and horizontal components and J45 which is the oblique component of astigmatism were calculated for all eyes. The following formula was used to calculate the vectors:
For all vector analysis, because the correlation between fellow eyes was high (correlation coefficient=0.869), the right eye was used based on cycloplegic refraction. The results of right eye were used for all the comparisons between astigmatism and spherical refractive errors.
Statistical analysisThe prevalence of astigmatism is reported as percentage along with its 95% confidence interval (CI).
The mean values of J0 and J45 vectors were calculated for the whole population and also according to different age and sex groups.
The sampling weight was considered for calculating the prevalence of astigmatism, and the design effect was considered for calculating the standard error and 95% CI. Since the variable of astigmatism was a binary variable, logistic regression was applied to investigate its correlation with other variables.
Simple and multiple logistic regressions were used to investigate the relationships. Astigmatism magnitude ≥0.75D was used to evaluate the relationship between astigmatism and other variables. The STATA software version 11 was used for data analysis.
Ethical considerationsThe ethics committee of Shahroud University of Medical Sciences approved the study, which was conducted in accord with the tenets of the Helsinki Declaration. All students’ parents signed informed consent and all children in the study participated willingly.
ResultsIn this study, of 5528 analyzed subjects, 53.8% (n=2977) were boys and 46.2% (n=2551) were girls. The reason for this gender difference was that the percentage of nonparticipant girls (52.2%) was higher than boys.28 The mean age of the children was 9.23±1.71 years (range: 6–12 years). The mean age of the boys and girls was 9.27±1.71 and 9.19±1.72 years, respectively (p=0.101).
In Table 1, the mean cylinder power, the mean J0, J45 and the prevalence of astigmatism in the right eye, defined by cylinder power ≥0.75 diopter are presented by the types of refraction.
The cylinder power, astigmatism vectors and prevalence of astigmatism (cylinder power ≥0.75 diopter in right eye) by type of refraction in 6–12 years old children, Shahroud, Iran, 2015.
| Refraction types | Cylinder power (diopter) | J0 vector | J45 vector | Prevalence of astigmatism |
|---|---|---|---|---|
| Mean (95% CI) | Mean (95% CI) | Mean (95% CI) | % (95% CI) | |
| Autorefraction | ||||
| Cycloplegia | −0.44 (−0.46 to −0.43) | 0.136 (0.127 to 0.145) | 0.014 (0.010 to 0.018) | 16.6 (15.6–17.7) |
| Non-cycloplegia | −0.41 (−0.43 to −0.39) | 0.085 (0.076 to 0.094) | 0.009 (0.005 to 0.013) | 14.0 (13.0–14.9) |
| Retinoscopy | ||||
| Cycloplegia | −0.39 (−0.41 to −0.38) | 0.126 (0.117 to 0.135) | 0.009 (0.006 to 0.013) | 13.3 (12.3–14.2) |
| Non-cycloplegia | −0.39 (−0.40 to −0.37) | 0.124 (0.115 to 0.132) | 0.009 (0.006 to 0.012) | 13.0 (12.1–14.0) |
| Subjective refraction | −0.31 (−0.32 to −0.29) | 0.104 (0.096 to 0.112) | 0.009 (0.006 to 0.012) | 12.5 (11.6–13.5) |
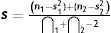
The mean cylinder power of the participants based on cycloplegic refraction was −0.39D (95% CI: −0.41 to −0.38D) in right eye. Fig. 1 presents the distribution of power vectors in right eye of the participants. As shown in this figure, the distribution of J45 vector was normal while the J0 vector had mild skewness to the right.
Table 2 shows the prevalence of astigmatism based on a cylinder power worse than −0.50, −1.00, and −2.00D according to age, sex, and living place. The prevalence of astigmatism based on a cylinder power worse than −0.50D was 16.7% (95% CI: 15.6–17.1). Logistic regression analysis showed no difference in the prevalence of astigmatism between boys and girls (p=.897).
The prevalence of astigmatism (in at least one eye) in schoolchildren by three definition, Shahroud, Iran, 2015.
| Independent variables | n | Cylinder power<−0.5D | Cylinder power<−1D | Cylinder power<−2D |
|---|---|---|---|---|
| % (95% CI) | % (95% CI) | % (95% CI) | ||
| Gender | ||||
| Female | 2551 | 16.8 (15.2–18.3) | 6.3 (5.2–7.3) | 2.7 (2.1–3.3) |
| Male | 2977 | 16.6 (15.2–18.0) | 6.5 (5.6–7.3) | 2.3 (1.7–2.8) |
| Region | ||||
| Urban | 4393 | 17.2 (16.0–18.3) | 6.5 (5.8–7.3) | 2.5 (2.1–3.0) |
| Rural | 1135 | 12.1 (10.0–14.1) | 5.1 (3.7–6.5) | 2.0 (1.1–3.0) |
| Age | ||||
| 6 | 220 | 21.5 (16.3–26.7) | 5.0 (2.3–7.7) | 2.0 (0.2–3.8) |
| 7 | 831 | 18.1 (15.5–20.7) | 6.1 (4.4–7.8) | 1.8 (0.9–2.6) |
| 8 | 996 | 18.0 (15.6–20.5) | 8.1 (6.1–10.1) | 2.9 (1.8–4.0) |
| 9 | 1050 | 16.5 (13.9–19.3) | 6.0 (4.3–7.6) | 2.9 (1.7–4.0) |
| 10 | 880 | 13.7 (11.4–16.0) | 4.3 (3.2–5.5) | 1.9 (1.0–2.8) |
| 11 | 924 | 14.9 (12.6–17.1) | 6.2 (4.7–7.6) | 2.0 (1.1–2.9) |
| 12 | 627 | 18.3 (15.5–21.1) | 8.3 (5.9–10.7) | 3.6 (2.2–5.0) |
| Total | 5528 | 16.7 (15.6–17.7) | 6.4 (5.7–7.1) | 2.5 (2.0–2.9) |
CI: confidence interval.
There was a nonlinear relationship between age and astigmatism. The prevalence of astigmatism worse than −0.50D was 21.5% in 6-year-old children which decreased to 13.7% in 10-year-olds but then increased to 18.3% in children aged 12 years. Table 3 shows the association of age, gender and residence place with astigmatism in logistic regression models.
The association of astigmatism with gender, age and living region in schoolchildren, Shahroud, Iran, 2015.
| Independent variables | Simple logistic regression | Multiple logistic regression | ||
|---|---|---|---|---|
| OR (95% CI) | p-Value | OR (95% CI) | p-Value | |
| Gender (male=1/female=0) | 0.99 (0.86–1.15) | 0.897 | – | – |
| Region (rural=1/urban=0) | 0.66 (0.54–0.82) | <0.001 | 0.65 (0.53–0.80) | <0.001 |
| Age (year) | ||||
| 6 | 1 | 1 | ||
| 7 | 0.81 (0.56–1.17) | 0.251 | 0.78 (0.54–1.12) | 0.180 |
| 8 | 0.80 (0.57–1.14) | 0.219 | 0.78 (0.55–1.10) | 0.151 |
| 9 | 0.73 (0.50–1.04) | 0.084 | 0.70 (0.49–1.00) | 0.053 |
| 10 | 0.58 (0.40–0.83) | 0.004 | 0.56 (0.39–0.80) | 0.002 |
| 11 | 0.64 (0.45–0.91) | 0.013 | 0.61 (0.43–0.87) | 0.006 |
| 12 | 0.82 (0.57–1.17) | 0.263 | 0.78 (0.55–1.12) | 0.179 |
CI: confidence interval; OR: odds ratio.
According to Tables 2 and 3, the prevalence of astigmatism was significantly higher in urban children (p<.0001).
Astigmatism worse than 2.00D was seen in 2.5% (95% CI: 2.1–2.9) of the children with no significant difference between boys and girls (p=.296). Astigmatism worse than −2.00D increased in a non-linear fashion from 2.0% in 6 year-old-children to 3.6% in 12-year-olds (p<.0001).
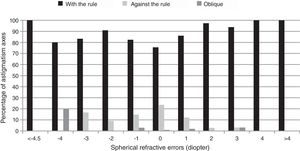
Table 4 shows the prevalence of different types of astigmatism. According to results, 14.2% (95% CI: 13.2–15.2) of the students had WTR, 2.1% (95% CI: 1.7–2.5) had ATR, and 0.3% (95% CI: 0.2–0.5) had oblique astigmatism. In general, WTR, ATR, and oblique astigmatisms were observed in 84.9%, 13.0%, and 2.1% of the astigmatic children, respectively.
Prevalence (%) of with-the-rule (WTR), against-the-rule (ATR), and oblique astigmatism according to the age, gender and residence place, Shahroud, Iran, 2015.
| Independent variables | WTR | ATR | Oblique |
|---|---|---|---|
| % (95% CI) | % (95% CI) | % (95% CI) | |
| Gender | |||
| Female | 14.5 (13.1–15.9) | 1.9 (1.3–2.4) | 0.4 (0.1–0.6) |
| Male | 14.0 (12.7–15.2) | 2.3 (1.8–2.9) | 0.3 (0.1–0.5) |
| Region | |||
| Urban | 14.7 (13.6–15.8) | 2.2 (1.7–2.6) | 0.3 (0.1–0.5) |
| Rural | 9.8 (8.0–11.6) | 1.9 (1.0–2.7) | 0.4 (0.1–0.8) |
| Age | |||
| 6 | 19.6 (13.9–25.2) | 1.4 (0.2–3.6) | 0.6 (0.3–1.7) |
| 7 | 16.5 (14.0–19.1) | 1.2 (0.5–1.9) | 0.3 (0.2–0.7) |
| 8 | 15.7 (13.3–18.0) | 2.2 (1.3–3.0) | 0.2 (0.2–0.5) |
| 9 | 14.8 (12.4–17.1) | 1.6 (0.7–2.4) | 0.2 (0.2–0.5) |
| 10 | 10.8 (8.7–13.0) | 2.3 (1.3–3.3) | 0.6 (0.2–1.0) |
| 11 | 12.0 (9.8–14.3) | 2.4 (1.3–3.5) | 0.4 (0.0–0.8) |
| 12 | 14.3 (11.8–16.8) | 3.7 (2.3–5.2) | 0.3 (0.2–0.6) |
| Total | 14.2 (13.2–15.2) | 2.1 (1.7–2.5) | 0.3 (0.2–0.5) |
CI: confidence interval.
Multiple logistic regression showed that WTR astigmatism was more prevalent in urban students (OR=0.62, 95% CI: 0.49–0.76) (p<.0001) and younger ages (OR=0.92, 95% CI: 0.87–0.96). ATR astigmatism was significantly associated with an increase in age (OR=1.19, 95% CI: 1.06–1.34). Oblique astigmatism had no significant association with age, sex, and residence place.
Power vector analysesTable 5 presents the mean values of J0 and J45 vectors based on cycloplegic refraction for the whole population and also according to different age and sex groups in right eye.
The mean (95% confidence intervals) of J0 and J45 in cycloplegic refraction according to gender, age and residence place in schoolchildren, Shahroud, Iran, 2015.
| Independent variables | J0 (diopter) | J45 (diopter) |
|---|---|---|
| Gender | ||
| Male | 0.120 (0.108 to 0.133) | 0.019 (0.015 to 0.023) |
| Female | 0.132 (0.121 to 0.144) | −0.002 (−0.006 to 0.003) |
| Region | ||
| Urban | 0.129 (0.120 to 0.139) | 0.009 (0.005 to 0.013) |
| Rural | 0.093 (0.075 to 0.111) | 0.014 (0.006 to 0.021) |
| Age | ||
| 6 | 0.169 (0.133 to 0.206) | 0.011 (−0.0001 to 0.022) |
| 7 | 0.153 (0.133 to 0.172) | 0.009 (−0.0009 to 0.019) |
| 8 | 0.148 (0.129 to 0.167) | 0.010 (0.002 to 0.017) |
| 9 | 0.133 (0.114 to 0.153) | 0.011 (0.004 to 0.019) |
| 10 | 0.102 (0.084 to 0.121) | 0.009 (0.002 to 0.016) |
| 11 | 0.092 (0.072 to 0.111) | 0.005 (−0.002 to 0.012) |
| 12 | 0.114 (0.088 to 0.141) | 0.013 (0.0003 to 0.026) |
| Total children | 0.126 (0.117 to 0.135) | 0.009 (0.006 to 0.013) |
The association of other independent variables and power vectors in simple and multiple linear regression models are shown in Table 6. According to the results of multiple models, urban students had a higher J0 which decreased significantly with age. J45 was only significantly associated with sex and boys had a higher J45 (p<.0001).
The association of J0 and J45 with gender, age and residence place in schoolchildren in simple and multiple linear regression models, Shahroud, Iran, 2015.
| Independent variables | J0 | J45 | ||||||
|---|---|---|---|---|---|---|---|---|
| Simple linear regression | Multiple linear regression | Simple linear regression | Multiple linear regression | |||||
| Coefficients (95% CI) | p-Value | Coefficients (95% CI) | p-Value | Coefficients (95% CI) | p-Value | Coefficients (95% CI) | p-Value | |
| Gender | ||||||||
| Male/female | −0.012 (−0.029 to 0.005) | .156 | −0.011 (−0.027 to 0.005) | .171 | 0.021 (0.014 to 0.027) | <.0001 | 0.021 (0.014 to 0.027) | <.0001 |
| Region | ||||||||
| Rural/urban | −0.036 (−0.056 to −0.016) | .0001 | −0.041 (−0.060 to −0.021) | <.0001 | 0.005 (−0.004 to 0.013) | .289 | 0.005 (−0.003 to 0.014) | .271 |
| Age (year) | ||||||||
| 6 | Reference group | – | Reference group | – | Reference group | – | Reference group | – |
| 7 | −0.017 (−0.056 to 0.023) | .414 | −0.021 (−0.060 to 0.019) | .305 | −0.002 (−0.017 to 0.013) | .811 | −0.0003 (−0.015 to 0.014) | .971 |
| 8 | −0.022 (−0.064 to 0.020) | .309 | −0.026 (−0.067 to 0.015) | .219 | −0.001 (−0.015 to 0.012) | .873 | 0.0001 (−0.012 to 0.012) | .996 |
| 9 | −0.036 (−0.077 to 0.006) | .091 | −0.040 (−0.081 to 0.001) | .056 | 0.001 (−0.013 to 0.014) | .939 | 0.001 (−0.010 to 0.013) | .824 |
| 10 | −0.067 (−0.108 to −0.026) | .001 | −0.071 (−0.110 to −0.031) | .001 | −0.002 (−0.015 to 0.011) | .788 | −0.002 (−0.014 to 0.010) | .722 |
| 11 | −0.078 (−0.119 to −0.036) | <.0001 | −0.082 (−0.123 to −0.042) | <.0001 | −0.006 (−0.019 to 0.007) | .392 | −0.005 (−0.017 to 0.007) | .414 |
| 12 | −0.055 (−0.100 to −0.010) | .017 | −0.060 (−0.104 to −0.015) | .009 | 0.002 (−0.015 to 0.019) | .810 | 0.003 (−0.012 to 0.018) | .685 |
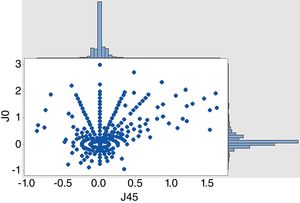
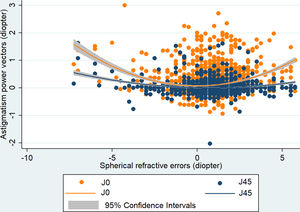
Fig. 2 presents cylinder power changes according to the severity of sphere. According to the results, the highest amount of astigmatism in myopic subjects worse than −4.5D was about 2.4D, the amount of astigmatism decreased with a decrease in spherical refractive error, and the lowest amount of astigmatism (0.35D) was seen in subjects with a spherical refractive error of about 1D; then, with an increase in hyperopia, the cylinder power again increased to about 1.6D in subjects with hyperopia worse than 4D.
Fig. 3 presents the relationship between spherical refractive error and different astigmatic axes in individuals with astigmatism in right eye. With an increase in spherical refractive error, WTR astigmatism increased. The highest prevalence of ATR astigmatism was seen in emmetropic children.
Fig. 4 shows the association of J0 and J45 in different spherical powers in right eye by scatter plot and quadratic fitted lines. In a non-linear pattern The J0 increased by moving spherical power from zero. The highest J0 and J45 were seen in individuals with myopia more than 4.5D. However, J45 did not change markedly in different spherical powers.
DiscussionThis is one of the few studies on the prevalence of astigmatism in the age group of 6–12 years. We evaluated the prevalence of different types of astigmatism and its changes with factors such as age, sex, and spherical refractive errors in a mixed sample of urban and rural children. The most common form of astigmatism in this study was WTR followed by ATR astigmatism. Oblique astigmatism had the lowest prevalence in the study population. The prevalence of WTR decreased and the prevalence of ATR increased with increase in age while the prevalence of oblique astigmatism did not change significantly. Since all findings have been also reported in previous studies,3,25,30 we do not address them here.
In this study 16.7% of the children had at least 0.50D astigmatism. Studies on the prevalence of astigmatism in similar age groups have reported a prevalence of 12–21%.6,24,31 These results are consistent with our finding. A study was conducted on children aged 6–15 years in an Iranian city (Dezful) recently25 which showed a prevalence of 45.3% for astigmatism that is markedly higher than our finding and the results of most previous studies. Since the definitions were rather similar in this study and previous studies conducted in Iran and their methodologies are not very much different, the marked difference may be attributed to environmental factors affecting astigmatism.17,32,33
Different studies have evaluated the prevalence of different refractive errors in the age group 6–15 years in various parts of the world whose results are summarized in Table 7.
Comparison of the prevalence of astigmatism in children in different studies.
| Country | n | Published year | Age (year) | Definition (D) | Prevalence (%) | Refraction type |
|---|---|---|---|---|---|---|
| China34 | 3070 | 2010 | 5–15 | ≥0.75 | 3.75 | Cycloplegic autorefraction |
| China26 | 4364 | 2004 | 5–15 | ≥0.75 | 42.7 | Cycloplegic autorefraction |
| Taiwan35 | 11175 | 2004 | 7–18 | ≥1.00 | 18.4 | Cycloplegic autorefraction |
| India(New Dehli)21 | 6447 | 2002 | 5–15 | ≥0.75 | 9.8 | Cycloplegic autorefraction |
| Nepal30 | 5067 | 2000 | 5–15 | ≥0.75 | 3.5 | Cycloplegic autorefraction, |
| China (shunyi)36 | 5884 | 2000 | 5–15 | >0.75 | 9.5 | Cycloplegic autorefraction |
| India(Andra Pradesh)37 | 4074 | 2002 | 7–15 | ≥0.75 | 5.9 | Cycloplegic autorefraction |
| Australia38 | 1765 | 2006 | 6–7 | ≥1.00 | 4.8 | Cycloplegic autorefraction |
| Singapore17 | 1028 | 2002 | 7–9 | ≥1.00 | 19.2 | Cycloplegic refraction |
| Chile (la Florida)39 | 5303 | 2000 | 5–15 | >0.75 | 27.2 | Cycloplegic autorefraction |
| India23 | 4029 | 1997 | 3–18 | ≥ 0.50 | 8.7 | NA |
| United States40 | 1740 | 1997 | 0–19 | ≥ 1.00 | 44.2 | NA |
| Vauatu41 | 788 | 1988 | 6–19 | ≥ 1.00 | 0.3 | NA |
| Malaysia22 | 7055 | 2008 | 6–12 | ≥ 0.75 | 0.6 | Non_cycloplegic autorefraction |
| Morocco42 | 5456 | 2009 | 6–16 | ≥ 0.75 | 3.5 | Cycloplegic retinoscopy |
| Poland43 | 5724 | 2007 | 6–18 | ≥ 0.75 | 4.0 | Cycloplegic retinoscopy |
| Sweden44 | 143 | 2006 | 4–15 | ≥0.75 | 22.0 | NA |
| Nepal45 | 133 | 2012 | 5–15 | ≥ 0.75 | 47.0 | Cycloplegic retinoscopy |
| Turkey46 | 2106 | 2013 | 6–14 | ≥ 0.75 | 14.3 | Cycloplegic autorefraction |
| Iran (Shiraz)24 | 1872 | 2010 | 7–15 | ≥ 0.75 | 11.2 | Cycloplegic autorefraction |
| Iran (Dezful)25 | 1375 | 2015 | 6–15 | ≥0.50 | 45.3 | Cycloplegic autorefraction |
| Iran (Khaf)31 | 2124 | 2014 | 0–15 | ≥0.50 | 14.3 | Non-cycloplegic autorefraction |
| China47 | 1783 | 2019 | 10–15.6 | ≥1.00 | 17.4 | Cycloplegic autorefraction |
| Current Study | 5528 | 2019 | 6–12 | >0.50 | 16.7 | Cycloplegic refraction |
D: Diopter; NA: not available.
Studies conducted in Poland,43 Malaysia,22 China,34,48 and Ethiopia49 have reported a markedly lower prevalence of astigmatism as compared to current study. The prevalence of astigmatism in the above studies ranges from 0.2% to 3.75%. However, the prevalence of astigmatism is much higher in children aged 5–15 years in studies conducted in Chile,39 Nepal,30 USA,40 and China,26 ranging from 27 to 44%. The reason for the difference may be environmental, genetic, and ethnic differences in these areas. Numerous studies have shown the prevalence of astigmatism is affected by geographical factors, living in urban or rural areas, ethnic differences, etc.31,50–52
As mentioned earlier, the prevalence of astigmatism was 21.5% in 6-year-old children, which decreased linearly till 10 years to 13.7%. Then, it started to increase in children aged 11 and 12 years, reaching 18.3% in 12-year-olds. The results of other studies on the prevalence of astigmatsim are very different depending on the age range of the participants.4,6,25,31 Although some studies found no significant changes in the prevalence of astigmatism in this age group,4 the majority of the studies have reporetd a decreasing trend for stigmatism from the neonatal period to adolescence followed by an increasing trend in middle ages.33,38 However, the results of this study were slightly different from other studies,4,6,25,31,33 which could be due to genetic and environmental factors. Although it is hard to explain this finding, the effect of near work at this age on astigmatism and corneal changes may be the probable reasons.53,33,54
The results of this study showed no difference in the prevalence of astigmatism between boys and girls although the results of different studies in this regard are controversial. Some studies have reported a higher prevalence in girls21,37 while some other studies have shown no gender preponderance.2,4,17,52,55 Results also showed no significant difference in the prevalence of WTR and oblique astigmatism between boys and girls while ATR astigmatism was more prevalent in boys.
As mentioned in “Results” section, although the J0 showed no difference between boys and girls, the mean J45 was significantly higher in boys. In other words, regarding the cylindrical power, the horizontal and vertical components of astigmatism have no relationship with gender while oblique astigmatism has a higher power in boys. These gender-related differences in prevalence and magnitude of astigmatism may indicate a possible sex-linked inheritance mode0,33,56 or different biometric indexes between two sexes.57
Living in urban or rural areas is an important factor in the prevalence of astigmatism. The prevalence of astigmatism is much higher in studies conducted in urban populations of Iran [Tehran],6 Chinese preschool children,52 Chile,39 and Mexico35 in comparison with studies conducted in rural populations of Iran [Khaf],31 India [Andra Pradesh],37 Nepal,30 China [Shunyi],58 etc. The results of most studies have shown that the prevalence of refractive errors is generally higher in the urban versus the rural population, and the prevalence of astigmatism is not an exception. Similar to previous studies, current study showed a higher prevalence of astigmatism in the urban versus the rural population. One of the possible reasons may be the higher prevalence of myopia in the urban population.36,50 As mentioned in “Results” section, the prevalence of astigmatism was higher in myopic individuals. Further analysis of data confirmed this hypothesis and revealed that prevalence of myopia in urban area (4.8%) was significantly higher than rural area (2.5%, p<.0001).
The results showed that J0 was higher in urban areas while no marked difference was observed in J45. Therefore, it could be concluded that vertical and horizontal components of astigmatism, i.e. WTR and ATR astigmatism, have a higher mean power in urban areas while the mean power of oblique astigmatism does not change markedly according to the place of residence. This finding is most probably related to spherical refractive errors and astigmatism vectors. Since J0 values were higher in higher spherical refractive errors, especially myopic spherical errors, considering the higher prevalence of myopia and high myopia in urban areas,36,50 a higher mean J0 is expected in urban areas. On the other hand, results showed no significant difference in J45 between urban and rural areas due to its weak association with different spherical powers.
The results of this study showed that with an increase in spherical ametropia, especially myopia, the power of cylindrical ametropia increased, as well. The lowest cylindrical power was observed in weak hypermetropia and the highest cylindrical power was seen in high myopia.
In addition, evaluation of the relationship of J0 and J45 vectors with different values of spherical power showed similar results. Contrary to J45 vector, J0 showed a significant correlation with spherical ametropia; in other words, J0 increased significantly with an increase in the magnitude of spherical ametropia.
Similar finding has been reported in previous studies, as well.38,43,47 One of the reasons for high cylinder powers, especially WTR, in myopic patients may be the relationship between a long axial length and WTR astigmatism.44 The second reason for the high prevalence of astigmatism and its higher cylinder powers in high myopia may be that patients with myopia, especially high myopia, squint for a better vision,59,60 which applies pressure on the cornea and increases the curvature of the vertical meridian, resulting in more WTR astigmatism.60 High spherical refractive errors were mostly associated with WTR astigmatism while the prevalence of ATR astigmatism increased with a decrease in the spherical error. The results of this study are in line with previous findings.38,61,62 Farbrother et al.62 conducted a study on 90884 individuals to evaluate the relationship between the astigmatic axis and the amount of spherical ametropia and reported that an increase in the spherical and cylindrical power increased the odds of WTR astigmatism. They also showed that ATR astigmatism was mostly seen in low ametropia, especially low myopia. We found that oblique astigmatism had no significant association with the amount of spherical ametropia. The results of a study by Shih61 on Taiwanese children also confirmed a relationship between the astigmatism type and spherical ametropia. One of the explanations for the association between low and moderate myopia and the higher prevalence of uncorrected ATR astigmatism may be the theory of myopic shift during the process of emmetropization as a result of a constant blurred retinal image due to uncorrected ATR astigmatism.16,63–65 In fact, according to this theory, the constant blurriness of the retinal image in children at the ages of emmetropization stimulates the growth of the axial length and increases myopia.
ConclusionThe prevalence of astigmatism in this study was not high in comparison with previous studies; however, its prevalence was markedly higher in urban children. The most common and the rarest type of astigmatism in our study population was WTR and oblique astigmatism, respectively. The cylinder power was the lowest in children with hypermetropia and increased with an increase in the spherical refractive error. The prevalence of WTR astigmatism increased and the prevalence of ATR astigmatism decreased with an increase in spherical ametropia. Oblique astigmatism had no significant association with spherical ametropia. There was no difference in the prevalence of astigmatism between boys and girls.
FundingNone declared.
Conflict of interestsNone declared.
Shahroud School Children Eye Cohort Study is funded by the Noor Eye Hospital and Shahroud University of Medical Sciences (Project number: 9329).