To determine the symptoms associated with accommodative and non-strabismic binocular dysfunctions and to assess the methods used to obtain the subjects’ symptoms.
MethodsWe conducted a scoping review of articles published between 1988 and 2012 that analysed any aspect of the symptomatology associated with accommodative and non-strabismic binocular dysfunctions. The literature search was performed in Medline (PubMed), CINAHL, PsycINFO and FRANCIS. A total of 657 articles were identified, and 56 met the inclusion criteria.
ResultsWe found 267 different ways of naming the symptoms related to these anomalies, which we grouped into 34 symptom categories. Of the 56 studies, 35 employed questionnaires and 21 obtained the symptoms from clinical histories. We found 11 questionnaires, of which only 3 had been validated: the convergence insufficiency symptom survey (CISS V-15) and CIRS parent version, both specific for convergence insufficiency, and the Conlon survey, developed for visual anomalies in general. The most widely used questionnaire (21 studies) was the CISS V-15. Of the 34 categories of symptoms, the most frequently mentioned were: headache, blurred vision, diplopia, visual fatigue, and movement or flicker of words at near vision, which were fundamentally related to near vision and binocular anomalies.
ConclusionsThere is a wide disparity of symptoms related to accommodative and binocular dysfunctions in the scientific literature, most of which are associated with near vision and binocular dysfunctions. The only psychometrically validated questionnaires that we found (n=3) were related to convergence insufficiency and to visual dysfunctions in general and there no specific questionnaires for other anomalies.
Determinar los síntomas asociados a las disfunciones acomodativas y binoculares no estrábicas, y evaluar los métodos utilizados para la obtención de los mismos.
MétodosSe realizó una revisión bibliográfica acotada de los artículos publicados entre 1988 y 2012 que analizaban cualquier aspecto de la sintomatología asociada a las disfunciones acomodativas y binoculares no estrábicas. La búsqueda se realizó en Medline (PubMed), CINAHL, PsycINFO y FRANCIS. Se identificaron un total de 657 artículos, de los que 56 cumplieron los criterios de inclusión.
ResultadosSe encontraron 267 formas diferentes de nombrar a los síntomas relativos a estas anomalías, que se agruparon en 34 categorías de síntomas. De los 56 estudios, 35 utilizaron cuestionarios y 21 de ellos obtuvieron los síntomas de las historias clínicas. Se encontraron 11 cuestionarios, de los que sólo 3 habían sido validados: el cuestionario Convergence Insufficiency Symptom Survey (CISS V-15) y su versión previa CIRS, ambos específicos para la insuficiencia de convergencia, y cuestionario de Conlon, desarrollado para anomalías visuales en general. El cuestionario más ampliamente utilizado (21 estudios) fue el CISS V-15. De las 34 categorías de síntomas, las más frecuentemente mencionadas fueron: dolor de cabeza, visión borrosa, diplopía, fatiga visual, y movimiento o parpadeo de las palabras en la visión de cerca, que se relacionaron fundamentalmente con la visión de cerca y las anomalías binoculares.
ConclusionesExiste una gran disparidad de síntomas en relación a las disfunciones acomodativas y binoculares en la literatura científica, muchos de las cuales se asocian a la visión de cerca y a las disfunciones binoculares. Los únicos cuestionarios psicométricamente validados (n=3) empleados se refieren a la insuficiencia de convergencia y a las disfunciones visuales en general, no existiendo cuestionarios específicos para otras anomalías.
In today's society, in which the emphasis on vision is associated with tasks requiring near vision, the visual system may be unable to perform this type of activity efficiently, leading to visual discomfort, fatigue or asthenopia and impaired visual performance.1 In many cases, the cause is an abnormality in any of the accommodative and/or vergence systems, which can lead to the development of what are termed accommodative and non-strabismic binocular dysfunctions.2 Accommodative and vergence dysfunctions can interfere with a child's academic progress or a person's ability to function efficiently in the course of his or her work. Children may abandon a task due to their inability to maintain adequate accommodation and/or vergence in the plane of fixation.1 In addition, those who perform extended periods of close vision work, such as reading or the prolonged use of computers, are more likely to report the symptoms and signs associated with these vision disorders.3,4 Nevertheless, the symptoms associated with prolonged near vision work can be reduced with the correct treatment to improve accommodative and vergence function.4,5
These dysfunctions are commonly encountered in clinical practice6 and present a variety of associated symptoms, including blurred vision, difficulty in focusing at different distances, headache and ocular pain, among others.7–10 In general, all of these symptoms are categorised under the generic name of asthenopia. However, the symptoms that the patient perceives may differ depending on the type of causative disorder2; it would therefore be reasonable to conclude that there are different types of asthenopia.11 In fact, one of the problems that clinicians face when diagnosing these dysfunctions is how to determine which symptoms are associated with each disorder and how to quantify their frequency and severity.12
The aim of this study is to determine by means of a scoping review the most common symptoms associated with accommodative and non-strabismic binocular dysfunctions described in the scientific literature published between 1988 and 2012. A further aim is to determine the manner in which subjects’ symptoms are obtained in order to quantify their frequency and severity. We elected to study a long period of time in this scoping review so as not to omit any possible relevant information on these anomalies.
Methods and materialsWe conducted a scoping review through an exhaustive search in health science databases for research published between 1988 and 2012. The search was performed in January 2013 using the Medline database (via PubMed), CINAHL, PsycINFO and FRANCIS.
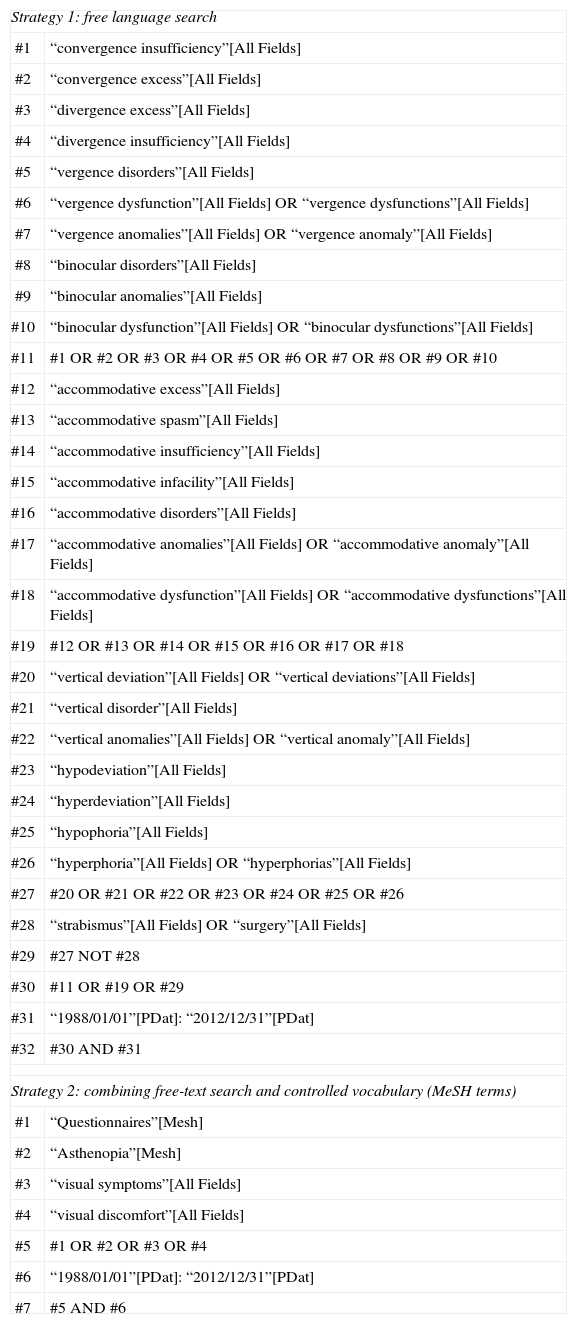
We designed two search strategies. The first strategy was based on the use of free-text terms related to accommodative and non-strabismic binocular dysfunctions, searching all database fields. The search equation included boolean operators, truncated symbols and wildcard characters specific to the selected databases. The second search strategy combined the use of controlled MeSH terms and free-text terms related to questionnaires, asthenopia, visual symptoms and visual discomfort. This second strategy was only implemented in Medline. Table 1 summarises the search equations employed in the two strategies.
Search strategy used in Medline by PubMed.
| Strategy 1: free language search | |
| #1 | “convergence insufficiency”[All Fields] |
| #2 | “convergence excess”[All Fields] |
| #3 | “divergence excess”[All Fields] |
| #4 | “divergence insufficiency”[All Fields] |
| #5 | “vergence disorders”[All Fields] |
| #6 | “vergence dysfunction”[All Fields] OR “vergence dysfunctions”[All Fields] |
| #7 | “vergence anomalies”[All Fields] OR “vergence anomaly”[All Fields] |
| #8 | “binocular disorders”[All Fields] |
| #9 | “binocular anomalies”[All Fields] |
| #10 | “binocular dysfunction”[All Fields] OR “binocular dysfunctions”[All Fields] |
| #11 | #1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 |
| #12 | “accommodative excess”[All Fields] |
| #13 | “accommodative spasm”[All Fields] |
| #14 | “accommodative insufficiency”[All Fields] |
| #15 | “accommodative infacility”[All Fields] |
| #16 | “accommodative disorders”[All Fields] |
| #17 | “accommodative anomalies”[All Fields] OR “accommodative anomaly”[All Fields] |
| #18 | “accommodative dysfunction”[All Fields] OR “accommodative dysfunctions”[All Fields] |
| #19 | #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 |
| #20 | “vertical deviation”[All Fields] OR “vertical deviations”[All Fields] |
| #21 | “vertical disorder”[All Fields] |
| #22 | “vertical anomalies”[All Fields] OR “vertical anomaly”[All Fields] |
| #23 | “hypodeviation”[All Fields] |
| #24 | “hyperdeviation”[All Fields] |
| #25 | “hypophoria”[All Fields] |
| #26 | “hyperphoria”[All Fields] OR “hyperphorias”[All Fields] |
| #27 | #20 OR #21 OR #22 OR #23 OR #24 OR #25 OR #26 |
| #28 | “strabismus”[All Fields] OR “surgery”[All Fields] |
| #29 | #27 NOT #28 |
| #30 | #11 OR #19 OR #29 |
| #31 | “1988/01/01”[PDat]: “2012/12/31”[PDat] |
| #32 | #30 AND #31 |
| Strategy 2: combining free-text search and controlled vocabulary (MeSH terms) | |
| #1 | “Questionnaires”[Mesh] |
| #2 | “Asthenopia”[Mesh] |
| #3 | “visual symptoms”[All Fields] |
| #4 | “visual discomfort”[All Fields] |
| #5 | #1 OR #2 OR #3 OR #4 |
| #6 | “1988/01/01”[PDat]: “2012/12/31”[PDat] |
| #7 | #5 AND #6 |
The inclusion criteria consisted of research published in English which examined any aspect of the symptoms associated with accommodative and non-strabismic binocular dysfunctions, regardless of the type of population studied, from children to adults. We wanted to obtain any type of studies in which authors described symptoms of patients with these anomalies obtained by means of questionnaires, case histories, or both. We excluded articles on strabismic binocular anomalies, papers on ophthalmic examination tests or eye diseases and non-original publications such as letters to the editor, editorials, theoretical reviews and conference proceedings. Published reports of a unique clinical case were also excluded.
The search identified 657 articles eligible for review. These were analysed in accordance with the established inclusion and exclusion criteria, leading to a final selection of 56 studies7–9,13–65 that reported some aspect of the symptomatology of accommodative and binocular dysfunctions. Two authors independently performed the data extraction (S.C.B. and P.C.M.) so that when there were inconsistencies, they were resolved by consensus. Reference lists from all identified studies were also examined.
Once the articles had been selected, all the terms used in each of the 56 studies to refer to the symptoms associated with the dysfunctions were extracted. Since relatively similar questions were often used to obtain the subjects’ symptoms, once these different ways of asking about the symptoms had been compiled they were grouped into categories that contained or referred to the same symptom.
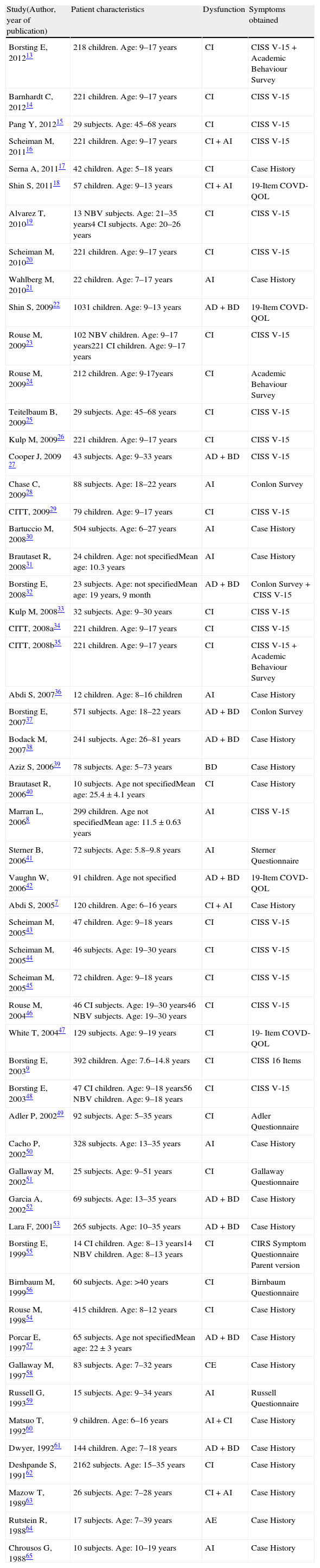
ResultsTable 2 shows the methodological characteristics of the 56 studies analysed. Besides author and year, the table also gives sample characteristics, type of dysfunction analysed and how each author obtained the symptoms referred to in each study. In the 35 studies8,9,13–16,18–20,22–29,32–35,37,41–49,51,55,56,59 which used questionnaires to analyse symptoms, a total of 11 different questionnaires9,24,41,42,48,49,51,55,56,59,66 were employed by the different authors.
Methodological characteristics of 56 articles of the review.
| Study(Author, year of publication) | Patient characteristics | Dysfunction | Symptoms obtained |
| Borsting E, 201213 | 218 children. Age: 9–17 years | CI | CISS V-15+Academic Behaviour Survey |
| Barnhardt C, 201214 | 221 children. Age: 9–17 years | CI | CISS V-15 |
| Pang Y, 201215 | 29 subjects. Age: 45–68 years | CI | CISS V-15 |
| Scheiman M, 201116 | 221 children. Age: 9–17 years | CI+AI | CISS V-15 |
| Serna A, 201117 | 42 children. Age: 5–18 years | CI | Case History |
| Shin S, 201118 | 57 children. Age: 9–13 years | CI+AI | 19-Item COVD-QOL |
| Alvarez T, 201019 | 13 NBV subjects. Age: 21–35 years4 CI subjects. Age: 20–26 years | CI | CISS V-15 |
| Scheiman M, 201020 | 221 children. Age: 9–17 years | CI | CISS V-15 |
| Wahlberg M, 201021 | 22 children. Age: 7–17 years | AI | Case History |
| Shin S, 200922 | 1031 children. Age: 9–13 years | AD+BD | 19-Item COVD-QOL |
| Rouse M, 200923 | 102 NBV children. Age: 9–17 years221 CI children. Age: 9–17 years | CI | CISS V-15 |
| Rouse M, 200924 | 212 children. Age: 9-17years | CI | Academic Behaviour Survey |
| Teitelbaum B, 200925 | 29 subjects. Age: 45–68 years | CI | CISS V-15 |
| Kulp M, 200926 | 221 children. Age: 9–17 years | CI | CISS V-15 |
| Cooper J, 2009 27 | 43 subjects. Age: 9–33 years | AD+BD | CISS V-15 |
| Chase C, 200928 | 88 subjects. Age: 18–22 years | AI | Conlon Survey |
| CITT, 200929 | 79 children. Age: 9–17 years | CI | CISS V-15 |
| Bartuccio M, 200830 | 504 subjects. Age: 6–27 years | AI | Case History |
| Brautaset R, 200831 | 24 children. Age: not specifiedMean age: 10.3 years | AI | Case History |
| Borsting E, 200832 | 23 subjects. Age: not specifiedMean age: 19 years, 9 month | AD+BD | Conlon Survey+CISS V-15 |
| Kulp M, 200833 | 32 subjects. Age: 9–30 years | CI | CISS V-15 |
| CITT, 2008a34 | 221 children. Age: 9–17 years | CI | CISS V-15 |
| CITT, 2008b35 | 221 children. Age: 9–17 years | CI | CISS V-15+Academic Behaviour Survey |
| Abdi S, 200736 | 12 children. Age: 8–16 children | AI | Case History |
| Borsting E, 200737 | 571 subjects. Age: 18–22 years | AD+BD | Conlon Survey |
| Bodack M, 200738 | 241 subjects. Age: 26–81 years | AD+BD | Case History |
| Aziz S, 200639 | 78 subjects. Age: 5–73 years | BD | Case History |
| Brautaset R, 200640 | 10 subjects. Age not specifiedMean age: 25.4±4.1 years | CI | Case History |
| Marran L, 20068 | 299 children. Age not specifiedMean age: 11.5±0.63 years | AI | CISS V-15 |
| Sterner B, 200641 | 72 subjects. Age: 5.8–9.8 years | AI | Sterner Questionnaire |
| Vaughn W, 200642 | 91 children. Age not specified | AD+BD | 19-Item COVD-QOL |
| Abdi S, 20057 | 120 children. Age: 6–16 years | CI+AI | Case History |
| Scheiman M, 200543 | 47 children. Age: 9–18 years | CI | CISS V-15 |
| Scheiman M, 200544 | 46 subjects. Age: 19–30 years | CI | CISS V-15 |
| Scheiman M, 200545 | 72 children. Age: 9–18 years | CI | CISS V-15 |
| Rouse M, 200446 | 46 CI subjects. Age: 19–30 years46 NBV subjects. Age: 19–30 years | CI | CISS V-15 |
| White T, 200447 | 129 subjects. Age: 9–19 years | CI | 19- Item COVD-QOL |
| Borsting E, 20039 | 392 children. Age: 7.6–14.8 years | CI | CISS 16 Items |
| Borsting E, 200348 | 47 CI children. Age: 9–18 years56 NBV children. Age: 9–18 years | CI | CISS V-15 |
| Adler P, 200249 | 92 subjects. Age: 5–35 years | CI | Adler Questionnaire |
| Cacho P, 200250 | 328 subjects. Age: 13–35 years | AI | Case History |
| Gallaway M, 200251 | 25 subjects. Age: 9–51 years | CI | Gallaway Questionnaire |
| Garcia A, 200252 | 69 subjects. Age: 13–35 years | AD+BD | Case History |
| Lara F, 200153 | 265 subjects. Age: 10–35 years | AD+BD | Case History |
| Borsting E, 199955 | 14 CI children. Age: 8–13 years14 NBV children. Age: 8–13 years | CI | CIRS Symptom Questionnaire Parent version |
| Birnbaum M, 199956 | 60 subjects. Age: >40 years | CI | Birnbaum Questionnaire |
| Rouse M, 199854 | 415 children. Age: 8–12 years | CI | Case History |
| Porcar E, 199757 | 65 subjects. Age not specifiedMean age: 22±3 years | AD+BD | Case History |
| Gallaway M, 199758 | 83 subjects. Age: 7–32 years | CE | Case History |
| Russell G, 199359 | 15 subjects. Age: 9–34 years | AI | Russell Questionnaire |
| Matsuo T, 199260 | 9 children. Age: 6–16 years | AI+CI | Case History |
| Dwyer, 199261 | 144 children. Age: 7–18 years | AD+BD | Case History |
| Deshpande S, 199162 | 2162 subjects. Age: 15–35 years | CI | Case History |
| Mazow T, 198963 | 26 subjects. Age: 7–28 years | CI+AI | Case History |
| Rutstein R, 198864 | 17 subjects. Age: 7–39 years | AE | Case History |
| Chrousos G, 198865 | 10 subjects. Age: 10–19 years | AI | Case History |
CI: convergence insufficiency, AI: accommodative insufficiency, AD: accommodative dysfunction, BD: binocular dysfunction, CE: convergence excess, AE: accommodative excess, NBV: normal binocular vision.
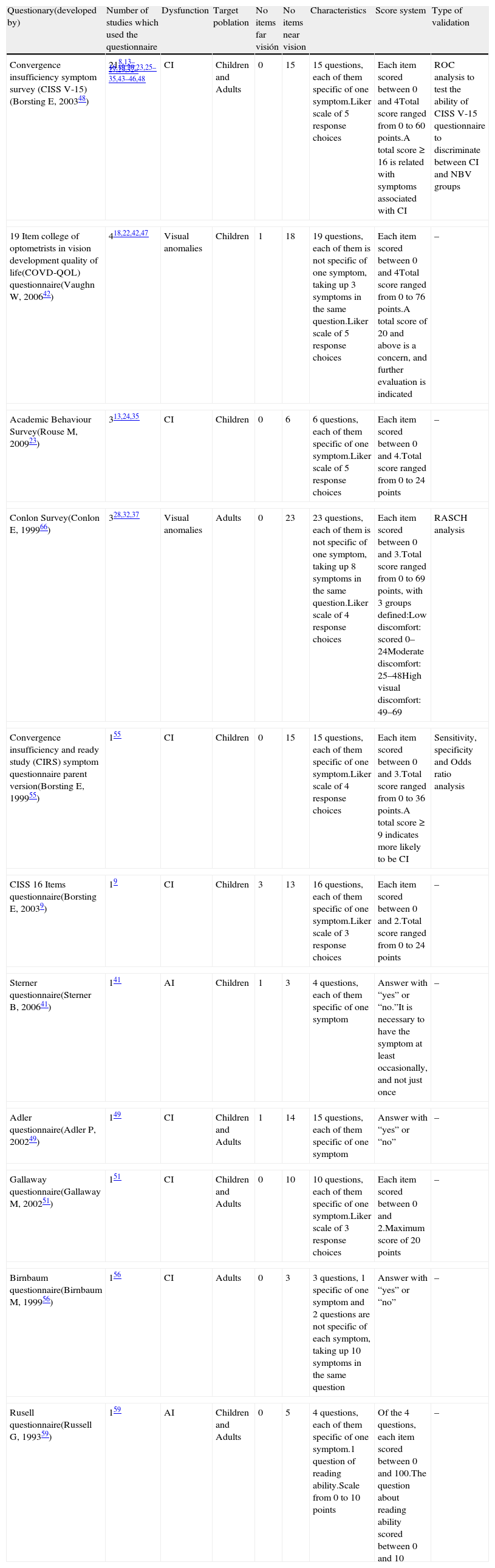
Table 3 shows the characteristics of the 11 questionnaires found in the 56 studies, indicating the authors who developed each questionnaire, which authors used each of them, the type of dysfunction to which they refer, the target population on which they were used, the number of items they contain and how many of these items are associated with far or near vision. It also shows the characteristics of each individual questionnaire, specifying the number of questions asked and how they are calibrated, what scoring system is used and whether the questionnaire has been psychometrically validated.
Characteristics of 11 questionnaires obtained in the review.
| Questionary(developed by) | Number of studies which used the questionnaire | Dysfunction | Target poblation | No items far visión | No items near vision | Characteristics | Score system | Type of validation |
| Convergence insufficiency symptom survey (CISS V-15)(Borsting E, 200348) | 218,13–16,19,20,23,25–27,29,32–35,43–46,48 | CI | Children and Adults | 0 | 15 | 15 questions, each of them specific of one symptom.Liker scale of 5 response choices | Each item scored between 0 and 4Total score ranged from 0 to 60 points.A total score≥16 is related with symptoms associated with CI | ROC analysis to test the ability of CISS V-15 questionnaire to discriminate between CI and NBV groups |
| 19 Item college of optometrists in vision development quality of life(COVD-QOL) questionnaire(Vaughn W, 200642) | 418,22,42,47 | Visual anomalies | Children | 1 | 18 | 19 questions, each of them is not specific of one symptom, taking up 3 symptoms in the same question.Liker scale of 5 response choices | Each item scored between 0 and 4Total score ranged from 0 to 76 points.A total score of 20 and above is a concern, and further evaluation is indicated | – |
| Academic Behaviour Survey(Rouse M, 200923) | 313,24,35 | CI | Children | 0 | 6 | 6 questions, each of them specific of one symptom.Liker scale of 5 response choices | Each item scored between 0 and 4.Total score ranged from 0 to 24 points | – |
| Conlon Survey(Conlon E, 199966) | 328,32,37 | Visual anomalies | Adults | 0 | 23 | 23 questions, each of them is not specific of one symptom, taking up 8 symptoms in the same question.Liker scale of 4 response choices | Each item scored between 0 and 3.Total score ranged from 0 to 69 points, with 3 groups defined:Low discomfort: scored 0–24Moderate discomfort: 25–48High visual discomfort: 49–69 | RASCH analysis |
| Convergence insufficiency and ready study (CIRS) symptom questionnaire parent version(Borsting E, 199955) | 155 | CI | Children | 0 | 15 | 15 questions, each of them specific of one symptom.Liker scale of 4 response choices | Each item scored between 0 and 3.Total score ranged from 0 to 36 points.A total score≥9 indicates more likely to be CI | Sensitivity, specificity and Odds ratio analysis |
| CISS 16 Items questionnaire(Borsting E, 20039) | 19 | CI | Children | 3 | 13 | 16 questions, each of them specific of one symptom.Liker scale of 3 response choices | Each item scored between 0 and 2.Total score ranged from 0 to 24 points | – |
| Sterner questionnaire(Sterner B, 200641) | 141 | AI | Children | 1 | 3 | 4 questions, each of them specific of one symptom | Answer with “yes” or “no.”It is necessary to have the symptom at least occasionally, and not just once | – |
| Adler questionnaire(Adler P, 200249) | 149 | CI | Children and Adults | 1 | 14 | 15 questions, each of them specific of one symptom | Answer with “yes” or “no” | – |
| Gallaway questionnaire(Gallaway M, 200251) | 151 | CI | Children and Adults | 0 | 10 | 10 questions, each of them specific of one symptom.Liker scale of 3 response choices | Each item scored between 0 and 2.Maximum score of 20 points | – |
| Birnbaum questionnaire(Birnbaum M, 199956) | 156 | CI | Adults | 0 | 3 | 3 questions, 1 specific of one symptom and 2 questions are not specific of each symptom, taking up 10 symptoms in the same question | Answer with “yes” or “no” | – |
| Rusell questionnaire(Russell G, 199359) | 159 | AI | Children and Adults | 0 | 5 | 4 questions, each of them specific of one symptom.1 question of reading ability.Scale from 0 to 10 points | Of the 4 questions, each item scored between 0 and 100.The question about reading ability scored between 0 and 10 | – |
CI: convergence insufficiency, AI: accommodative insufficiency; NBV: normal binocular vision.
An analysis of the different symptoms named in the 56 studies revealed that up to 267 different expressions were used to ask about symptoms, both in the case histories and in the 11 questionnaires related to these dysfunctions. Of these, 162 expressions appeared in publications reporting the use of questionnaires while the remaining 105 were employed in publications which did not use a questionnaire.
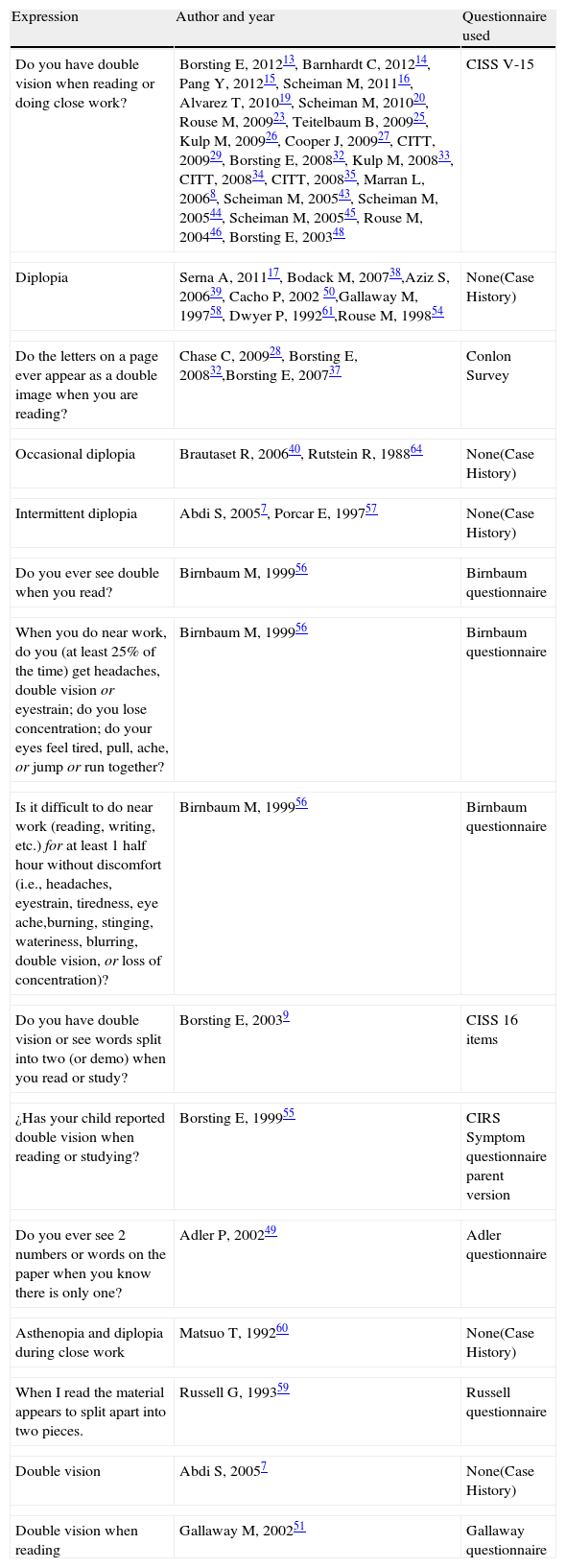
Due to this high number of different ways to name the symptoms (267), it was decided to group terms which described the same symptom by category. The aim was to obtain categories of symptoms in order to summarise those which actually referred to the same concept and thus avoid duplication of information. Table 4 shows an example of this phenomenon as regards the category of “double vision”. The 15 different ways used to name the symptom of double vision were grouped into the same category, called “diplopia”. Table 4 also shows the different ways employed to ask about double vision, the different studies that used them and whether they were compiled using a questionnaire.
Example of 15 different expressions used to ask about diplopia named in the 56 studies of the review.
| Expression | Author and year | Questionnaire used |
| Do you have double vision when reading or doing close work? | Borsting E, 201213, Barnhardt C, 201214, Pang Y, 201215, Scheiman M, 201116, Alvarez T, 201019, Scheiman M, 201020, Rouse M, 200923, Teitelbaum B, 200925, Kulp M, 200926, Cooper J, 200927, CITT, 200929, Borsting E, 200832, Kulp M, 200833, CITT, 200834, CITT, 200835, Marran L, 20068, Scheiman M, 200543, Scheiman M, 200544, Scheiman M, 200545, Rouse M, 200446, Borsting E, 200348 | CISS V-15 |
| Diplopia | Serna A, 201117, Bodack M, 200738,Aziz S, 200639, Cacho P, 2002 50,Gallaway M, 199758, Dwyer P, 199261,Rouse M, 199854 | None(Case History) |
| Do the letters on a page ever appear as a double image when you are reading? | Chase C, 200928, Borsting E, 200832,Borsting E, 200737 | Conlon Survey |
| Occasional diplopia | Brautaset R, 200640, Rutstein R, 198864 | None(Case History) |
| Intermittent diplopia | Abdi S, 20057, Porcar E, 199757 | None(Case History) |
| Do you ever see double when you read? | Birnbaum M, 199956 | Birnbaum questionnaire |
| When you do near work, do you (at least 25% of the time) get headaches, double vision or eyestrain; do you lose concentration; do your eyes feel tired, pull, ache, or jump or run together? | Birnbaum M, 199956 | Birnbaum questionnaire |
| Is it difficult to do near work (reading, writing, etc.) for at least 1 half hour without discomfort (i.e., headaches, eyestrain, tiredness, eye ache,burning, stinging, wateriness, blurring, double vision, or loss of concentration)? | Birnbaum M, 199956 | Birnbaum questionnaire |
| Do you have double vision or see words split into two (or demo) when you read or study? | Borsting E, 20039 | CISS 16 items |
| ¿Has your child reported double vision when reading or studying? | Borsting E, 199955 | CIRS Symptom questionnaire parent version |
| Do you ever see 2 numbers or words on the paper when you know there is only one? | Adler P, 200249 | Adler questionnaire |
| Asthenopia and diplopia during close work | Matsuo T, 199260 | None(Case History) |
| When I read the material appears to split apart into two pieces. | Russell G, 199359 | Russell questionnaire |
| Double vision | Abdi S, 20057 | None(Case History) |
| Double vision when reading | Gallaway M, 200251 | Gallaway questionnaire |
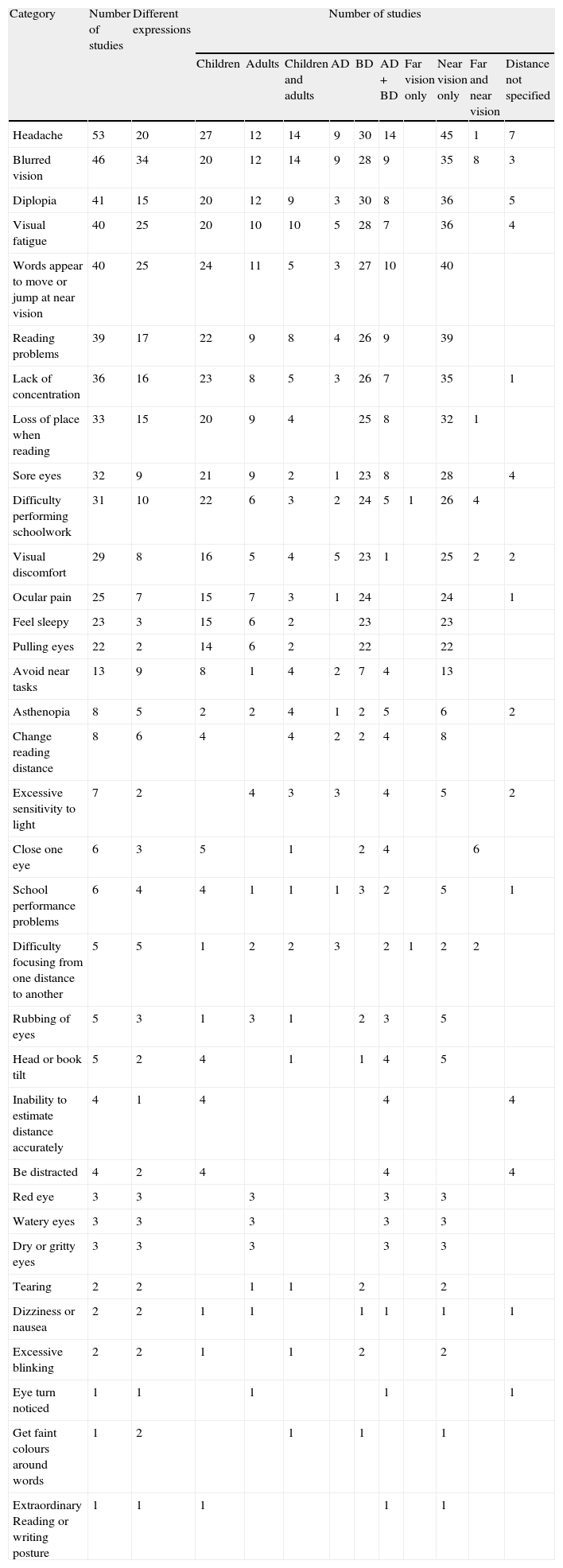
Following a qualitative process, each of 267 expressions used to ask about symptoms were reviewed and designated to a category that embodied the meaning of the symptom. Thus, the 267 different forms were grouped into 34 categories of symptoms. Table 5 shows the 34 categories of symptoms established, and specifies how many different forms refer to each category and the number of studies that report on this symptom. For each category, it also indicates the number of studies which referred to children, adults or both, accommodative dysfunction, binocular dysfunction or both, and whether each category is associated with far vision, near vision or both, according to the number of authors who specified this.
Relation of the 34 categories of symptoms found in the 56 articles of the review.
| Category | Number of studies | Different expressions | Number of studies | |||||||||
| Children | Adults | Children and adults | AD | BD | AD+BD | Far vision only | Near vision only | Far and near vision | Distance not specified | |||
| Headache | 53 | 20 | 27 | 12 | 14 | 9 | 30 | 14 | 45 | 1 | 7 | |
| Blurred vision | 46 | 34 | 20 | 12 | 14 | 9 | 28 | 9 | 35 | 8 | 3 | |
| Diplopia | 41 | 15 | 20 | 12 | 9 | 3 | 30 | 8 | 36 | 5 | ||
| Visual fatigue | 40 | 25 | 20 | 10 | 10 | 5 | 28 | 7 | 36 | 4 | ||
| Words appear to move or jump at near vision | 40 | 25 | 24 | 11 | 5 | 3 | 27 | 10 | 40 | |||
| Reading problems | 39 | 17 | 22 | 9 | 8 | 4 | 26 | 9 | 39 | |||
| Lack of concentration | 36 | 16 | 23 | 8 | 5 | 3 | 26 | 7 | 35 | 1 | ||
| Loss of place when reading | 33 | 15 | 20 | 9 | 4 | 25 | 8 | 32 | 1 | |||
| Sore eyes | 32 | 9 | 21 | 9 | 2 | 1 | 23 | 8 | 28 | 4 | ||
| Difficulty performing schoolwork | 31 | 10 | 22 | 6 | 3 | 2 | 24 | 5 | 1 | 26 | 4 | |
| Visual discomfort | 29 | 8 | 16 | 5 | 4 | 5 | 23 | 1 | 25 | 2 | 2 | |
| Ocular pain | 25 | 7 | 15 | 7 | 3 | 1 | 24 | 24 | 1 | |||
| Feel sleepy | 23 | 3 | 15 | 6 | 2 | 23 | 23 | |||||
| Pulling eyes | 22 | 2 | 14 | 6 | 2 | 22 | 22 | |||||
| Avoid near tasks | 13 | 9 | 8 | 1 | 4 | 2 | 7 | 4 | 13 | |||
| Asthenopia | 8 | 5 | 2 | 2 | 4 | 1 | 2 | 5 | 6 | 2 | ||
| Change reading distance | 8 | 6 | 4 | 4 | 2 | 2 | 4 | 8 | ||||
| Excessive sensitivity to light | 7 | 2 | 4 | 3 | 3 | 4 | 5 | 2 | ||||
| Close one eye | 6 | 3 | 5 | 1 | 2 | 4 | 6 | |||||
| School performance problems | 6 | 4 | 4 | 1 | 1 | 1 | 3 | 2 | 5 | 1 | ||
| Difficulty focusing from one distance to another | 5 | 5 | 1 | 2 | 2 | 3 | 2 | 1 | 2 | 2 | ||
| Rubbing of eyes | 5 | 3 | 1 | 3 | 1 | 2 | 3 | 5 | ||||
| Head or book tilt | 5 | 2 | 4 | 1 | 1 | 4 | 5 | |||||
| Inability to estimate distance accurately | 4 | 1 | 4 | 4 | 4 | |||||||
| Be distracted | 4 | 2 | 4 | 4 | 4 | |||||||
| Red eye | 3 | 3 | 3 | 3 | 3 | |||||||
| Watery eyes | 3 | 3 | 3 | 3 | 3 | |||||||
| Dry or gritty eyes | 3 | 3 | 3 | 3 | 3 | |||||||
| Tearing | 2 | 2 | 1 | 1 | 2 | 2 | ||||||
| Dizziness or nausea | 2 | 2 | 1 | 1 | 1 | 1 | 1 | 1 | ||||
| Excessive blinking | 2 | 2 | 1 | 1 | 2 | 2 | ||||||
| Eye turn noticed | 1 | 1 | 1 | 1 | 1 | |||||||
| Get faint colours around words | 1 | 2 | 1 | 1 | 1 | |||||||
| Extraordinary Reading or writing posture | 1 | 1 | 1 | 1 | 1 | |||||||
AD: accommodative dysfunction, BD: binocular dysfunction.
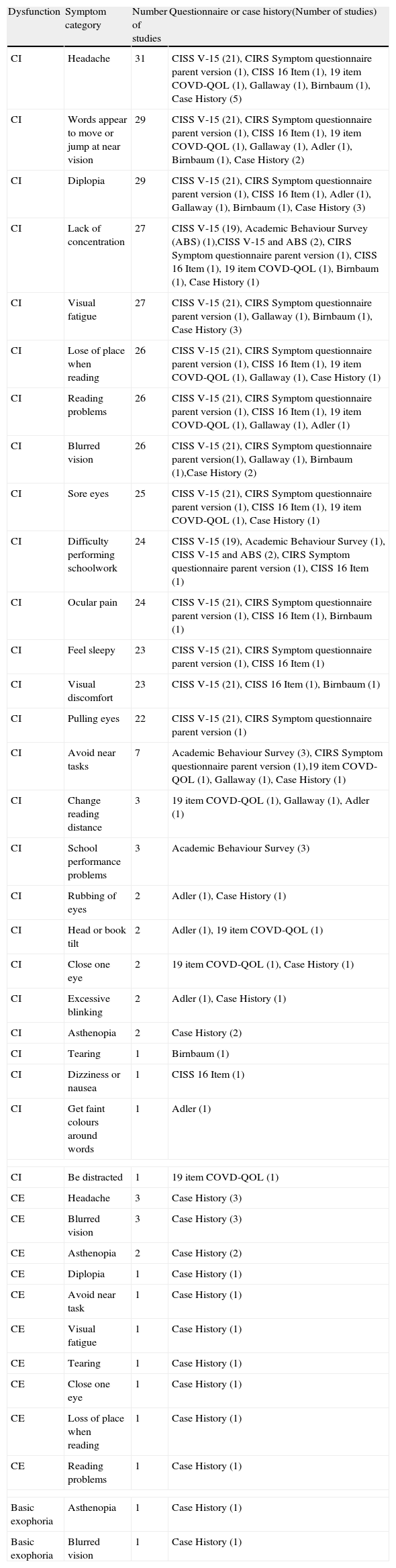
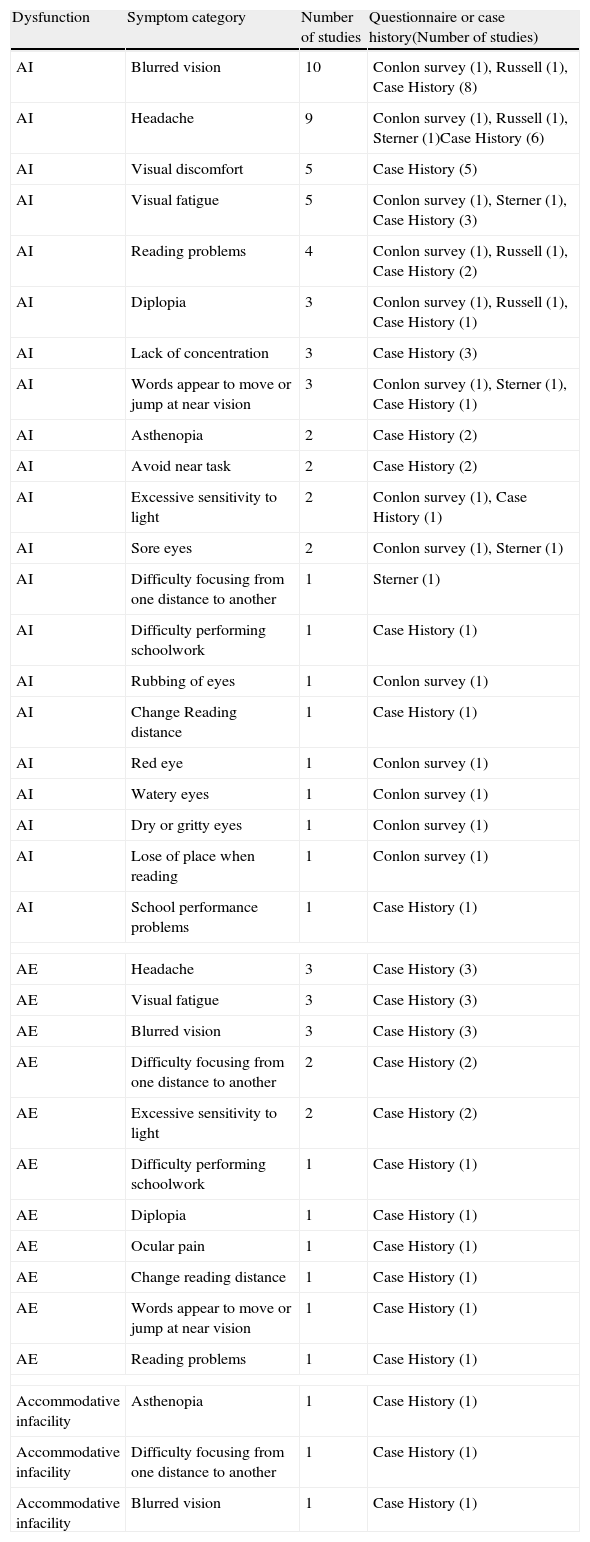
Tables 6 and 7 show the symptoms associated with each particular binocular and accommodative dysfunction. There have only been included the anomalies for which the authors described symptoms particularly associated with each dysfunction. In both of them there is also information about the number of studies which refer to each symptom and if the category has been named by a particular questionnaire or by means of the case histories with their number of studies.
Symptoms associated with each binocular dysfunction found in the 56 articles.
| Dysfunction | Symptom category | Number of studies | Questionnaire or case history(Number of studies) |
| CI | Headache | 31 | CISS V-15 (21), CIRS Symptom questionnaire parent version (1), CISS 16 Item (1), 19 item COVD-QOL (1), Gallaway (1), Birnbaum (1), Case History (5) |
| CI | Words appear to move or jump at near vision | 29 | CISS V-15 (21), CIRS Symptom questionnaire parent version (1), CISS 16 Item (1), 19 item COVD-QOL (1), Gallaway (1), Adler (1), Birnbaum (1), Case History (2) |
| CI | Diplopia | 29 | CISS V-15 (21), CIRS Symptom questionnaire parent version (1), CISS 16 Item (1), Adler (1), Gallaway (1), Birnbaum (1), Case History (3) |
| CI | Lack of concentration | 27 | CISS V-15 (19), Academic Behaviour Survey (ABS) (1),CISS V-15 and ABS (2), CIRS Symptom questionnaire parent version (1), CISS 16 Item (1), 19 item COVD-QOL (1), Birnbaum (1), Case History (1) |
| CI | Visual fatigue | 27 | CISS V-15 (21), CIRS Symptom questionnaire parent version (1), Gallaway (1), Birnbaum (1), Case History (3) |
| CI | Lose of place when reading | 26 | CISS V-15 (21), CIRS Symptom questionnaire parent version (1), CISS 16 Item (1), 19 item COVD-QOL (1), Gallaway (1), Case History (1) |
| CI | Reading problems | 26 | CISS V-15 (21), CIRS Symptom questionnaire parent version (1), CISS 16 Item (1), 19 item COVD-QOL (1), Gallaway (1), Adler (1) |
| CI | Blurred vision | 26 | CISS V-15 (21), CIRS Symptom questionnaire parent version(1), Gallaway (1), Birnbaum (1),Case History (2) |
| CI | Sore eyes | 25 | CISS V-15 (21), CIRS Symptom questionnaire parent version (1), CISS 16 Item (1), 19 item COVD-QOL (1), Case History (1) |
| CI | Difficulty performing schoolwork | 24 | CISS V-15 (19), Academic Behaviour Survey (1), CISS V-15 and ABS (2), CIRS Symptom questionnaire parent version (1), CISS 16 Item (1) |
| CI | Ocular pain | 24 | CISS V-15 (21), CIRS Symptom questionnaire parent version (1), CISS 16 Item (1), Birnbaum (1) |
| CI | Feel sleepy | 23 | CISS V-15 (21), CIRS Symptom questionnaire parent version (1), CISS 16 Item (1) |
| CI | Visual discomfort | 23 | CISS V-15 (21), CISS 16 Item (1), Birnbaum (1) |
| CI | Pulling eyes | 22 | CISS V-15 (21), CIRS Symptom questionnaire parent version (1) |
| CI | Avoid near tasks | 7 | Academic Behaviour Survey (3), CIRS Symptom questionnaire parent version (1),19 item COVD-QOL (1), Gallaway (1), Case History (1) |
| CI | Change reading distance | 3 | 19 item COVD-QOL (1), Gallaway (1), Adler (1) |
| CI | School performance problems | 3 | Academic Behaviour Survey (3) |
| CI | Rubbing of eyes | 2 | Adler (1), Case History (1) |
| CI | Head or book tilt | 2 | Adler (1), 19 item COVD-QOL (1) |
| CI | Close one eye | 2 | 19 item COVD-QOL (1), Case History (1) |
| CI | Excessive blinking | 2 | Adler (1), Case History (1) |
| CI | Asthenopia | 2 | Case History (2) |
| CI | Tearing | 1 | Birnbaum (1) |
| CI | Dizziness or nausea | 1 | CISS 16 Item (1) |
| CI | Get faint colours around words | 1 | Adler (1) |
| CI | Be distracted | 1 | 19 item COVD-QOL (1) |
| CE | Headache | 3 | Case History (3) |
| CE | Blurred vision | 3 | Case History (3) |
| CE | Asthenopia | 2 | Case History (2) |
| CE | Diplopia | 1 | Case History (1) |
| CE | Avoid near task | 1 | Case History (1) |
| CE | Visual fatigue | 1 | Case History (1) |
| CE | Tearing | 1 | Case History (1) |
| CE | Close one eye | 1 | Case History (1) |
| CE | Loss of place when reading | 1 | Case History (1) |
| CE | Reading problems | 1 | Case History (1) |
| Basic exophoria | Asthenopia | 1 | Case History (1) |
| Basic exophoria | Blurred vision | 1 | Case History (1) |
CI: convergence insufficiency, CE: convergence excess.
Symptoms associated with each accommodative dysfunction found in the 56 articles.
| Dysfunction | Symptom category | Number of studies | Questionnaire or case history(Number of studies) |
| AI | Blurred vision | 10 | Conlon survey (1), Russell (1), Case History (8) |
| AI | Headache | 9 | Conlon survey (1), Russell (1), Sterner (1)Case History (6) |
| AI | Visual discomfort | 5 | Case History (5) |
| AI | Visual fatigue | 5 | Conlon survey (1), Sterner (1), Case History (3) |
| AI | Reading problems | 4 | Conlon survey (1), Russell (1), Case History (2) |
| AI | Diplopia | 3 | Conlon survey (1), Russell (1), Case History (1) |
| AI | Lack of concentration | 3 | Case History (3) |
| AI | Words appear to move or jump at near vision | 3 | Conlon survey (1), Sterner (1), Case History (1) |
| AI | Asthenopia | 2 | Case History (2) |
| AI | Avoid near task | 2 | Case History (2) |
| AI | Excessive sensitivity to light | 2 | Conlon survey (1), Case History (1) |
| AI | Sore eyes | 2 | Conlon survey (1), Sterner (1) |
| AI | Difficulty focusing from one distance to another | 1 | Sterner (1) |
| AI | Difficulty performing schoolwork | 1 | Case History (1) |
| AI | Rubbing of eyes | 1 | Conlon survey (1) |
| AI | Change Reading distance | 1 | Case History (1) |
| AI | Red eye | 1 | Conlon survey (1) |
| AI | Watery eyes | 1 | Conlon survey (1) |
| AI | Dry or gritty eyes | 1 | Conlon survey (1) |
| AI | Lose of place when reading | 1 | Conlon survey (1) |
| AI | School performance problems | 1 | Case History (1) |
| AE | Headache | 3 | Case History (3) |
| AE | Visual fatigue | 3 | Case History (3) |
| AE | Blurred vision | 3 | Case History (3) |
| AE | Difficulty focusing from one distance to another | 2 | Case History (2) |
| AE | Excessive sensitivity to light | 2 | Case History (2) |
| AE | Difficulty performing schoolwork | 1 | Case History (1) |
| AE | Diplopia | 1 | Case History (1) |
| AE | Ocular pain | 1 | Case History (1) |
| AE | Change reading distance | 1 | Case History (1) |
| AE | Words appear to move or jump at near vision | 1 | Case History (1) |
| AE | Reading problems | 1 | Case History (1) |
| Accommodative infacility | Asthenopia | 1 | Case History (1) |
| Accommodative infacility | Difficulty focusing from one distance to another | 1 | Case History (1) |
| Accommodative infacility | Blurred vision | 1 | Case History (1) |
AI: accommodative insufficiency, AE: accommodative excess.
The results of this scoping review show the disparity of symptoms associated with accommodative and non-strabismic binocular dysfunctions, and that these are fundamentally related to binocular dysfunctions and mainly associated with close vision tasks. There is no consensus concerning which symptoms should be considered in the diagnosis of each of these anomalies. The review also revealed that there are no specific questionnaires for most of the accommodative and binocular dysfunctions except for convergence insufficiency (CI).
CI is the dysfunction which has received most research attention; 50% of the studies analysed concerned this binocular anomaly. According to the scientific literature, CI is one of the most common anomalies of binocular vision, with prevalence values in the clinical population that range between 2.25% and 33%.6 It is also one of the binocular vision anomalies that has received most research attention, not only in studies related to its diagnosis8,46,48,52,55 but also in several recent clinical trials concerning this disorder.34,43–45 It is therefore logical that it should be the dysfunction on which most information is available about its symptomatology. In fact, the scientific literature shows that the remaining accommodative and non-strabismic binocular dysfunctions have been studied to a lesser extent.5,6,10
When analysing symptoms related to different populations, the review shows that most of the studies are related to children (29 reports), with 12 studies about adults and 15 articles related to both populations. It should be noticed that symptoms reported by adults and children could be different between them, not only when considering the case history but using a particular questionnaire. Moreover, a child's response to a certain question could be different if it was administered by a parent versus the examiner. However, the review shows that authors have not differentiated questions for case histories nor for the questionnaires reported by adults and children.
As regards the way in which symptoms are obtained, we observed that 21 studies7,17,21,30,31,36,38–40,50,52–54,57,58,60–65 analysed symptoms using patients’ descriptions of their case histories or on the basis of questions posed by the person conducting the examination. Of the 11 questionnaires used, the CI-specific CISS V-15 questionnaire was the most frequently employed, having been used in 21 studies8,13–16,19,20,23,25–27,29,32–35,43–46,48, followed by the 19-item College of Optometrists in Vision Development Quality of Life (QOVD-QOL) questionnaire18,22,42,47 (developed for visual abnormalities in general) and the Conlon survey28,32,37 developed for visual disorders in general and the Academic Behaviour Survey13,24,35 (for CI). The remaining questionnaires were used once only.9,41,49,51,55,56,59 Consequently, although in general more studies were based on the use of questionnaires (35 studies), most of them used the CISS V-15 and thus there were actually a higher percentage of articles in which subjects’ symptoms were obtained from their case histories.
As regards psychometric validation, only three of the questionnaires used had been validated, the CISS V-15,48 CIRS symptom questionnaire parent version55 and the Conlon survey.66 The CISS V-15,48 is a CI-specific questionnaire that has proven useful in differentiating subjects with CI from those with normal binocular vision and has been widely used to develop the diagnosis of this disorder in both child and adult populations, and to monitor the effectiveness of different treatments in the various clinical trials conducted to date. However, since it has only been validated for CI, its use cannot be generalised to other dysfunctions unless validating for other anomalies.
In the same way the CIRS symptom questionnaire parent version55 has been proved to be a valid instrument for differentiating children with CI from those with normal binocular vision, although it has only been used on one occasion.
Meanwhile, the Conlon survey,66 validated by RASCH analysis, was developed to analyse the symptoms associated with any type of visual anomaly, including accommodative and binocular dysfunctions, and has shown to be a reliable and valid measure of visual discomfort for adults.
Despite the existence of these three validated questionnaires, our results indicate that there is a lack of specific questionnaires for each of the existing accommodative and binocular dysfunctions. The 11 questionnaires identified were used for different dysfunctions, although the vast majority of them (7) were employed for CI.9,24,48,49,51,55,56 The Russell59 and Sterner41 questionnaires were used to analyse accommodative insufficiency (AI), while the two remaining questionnaires42,66 were employed for accommodative and binocular dysfunctions in general.
The existence of 267 different ways of naming the symptoms that can be grouped into 34 categories indicates a wide disparity in forms of referring to the same symptom. A clear example is the case of the symptom of “blurred vision”, for which 34 different ways of referring to it were found.
An analysis of the 34 symptom categories shows that most of these categories were related to children although the great majority of these symptoms have also been used for adult populations and for the combination of children and adults. This finding is related to the fact that most of the studies are focused in children population. However it is worth noting that there are several symptoms (“head or book tilt”, “inability to estimate distance accurately”, “be distracted” and “extraordinary reading or writing posture”) which have been only reported in children population. The same happens when considering symptoms as “red eye”, “watery eyes”, “dry or gritty eyes” and “eye turn noticed” which have only been reported in adults population, although certainly there are only few studies which have reported them. These findings show that authors do not seem to differentiate symptoms for children and adults.
In addition to that, the vast majority of these categories were associated with binocular dysfunctions compared to symptom categories related to accommodative dysfunctions. In general, it should be noted that symptoms overlap between accommodative and binocular anomalies. No category was associated exclusively with accommodative dysfunctions, although two symptoms in a high number of studies (“feel sleepy” and “pulling eyes”) were only related to binocular anomalies. These findings confirm that it is difficult to disjoin accommodation from vergence system. Due to the link between both systems, a deficiency in one system could cause an abnormality in the other so that symptoms would overlap. For that reason, it should be difficult to determine a very specific question which could only be related to either an accommodative deficiency or a vergence one.
Similarly, it is worth noting that the vast majority of authors associated the symptoms with near vision rather than with far vision. Some categories were associated with both distances, and there were even cases where the authors did not specify the distance associated with the symptoms. No category was exclusively associated with far vision. This finding is clearly related to the fact that CI is the most frequently studied dysfunction67,68 and its symptoms are mainly associated with near vision; thus most categories are related to near vision. It is possible that if other dysfunctions had been analysed, the findings in this respect might have indicated the existence of other symptoms more specific to far vision. Nevertheless, the present analysis indicates that there is a lack of specific questionnaires related to dysfunctions affecting far vision.
Of the symptoms cited most frequently, the category of “headache” appeared in almost all of the 56 articles analysed. The other frequently mentioned symptoms are all mainly related to binocular dysfunctions and are particularly closely associated with near vision. It is also evident that few symptoms were specific to each entity and many overlap. This information may influence clinical management as it is difficult to associate a particular dysfunction with a particular symptom.
When each particular accommodative and binocular dysfunction was considered separately, certain singularities were observed with respect to some symptoms, for example when referring to diplopia in accommodative dysfunctions such as accommodative insufficiency or accommodative excess. CI was associated with the vast majority of symptoms identified; 26 of 34 categories were associated with this dysfunction. This finding highlights the importance given in the scientific literature to CI over and above other dysfunctions. The symptoms most commonly associated with CI are precisely those symptoms which coincide with the questions in the CISS V-15.
The other dysfunctions also had different categories of associated symptoms. However, only a limited number of authors referred to each category for dysfunctions such as convergence excess, accommodative insufficiency, accommodative infacility, accommodative excess or basic exophoria.
In summary, the results of this scoping review demonstrate that gaps exist in our current knowledge. There is a wide range of symptoms related to accommodative and non-strabismic binocular dysfunctions reported in the scientific literature. There is no consensus concerning which symptoms should be considered in the diagnosis of each of these anomalies observing that few symptoms were specific to each entity and many overlap. According to the questionnaires, only the use of three validated symptom questionnaires were reported in the scientific literature, and two of them were specific for CI. However, no specific questionnaires were found for being for the remaining accommodative and binocular dysfunctions when there is the suspicion of an accommodative or binocular anomaly. This coverts the task of identifying the type of symptoms and their frequency and severity in something extremely difficult in spite of being an important aspect for diagnostic purposes. So, future studies should be done in this sense. Further questionnaires might be developed to address symptoms related to accommodative and nonstrabismic binocular dysfunctions other than CI.
This work has been supported by “Vicerrectorado de Investigación, Desarrollo e Innovación” of the University of Alicante, Spain (GRE10-06).