Diabetic retinopathy is the leading cause of blindness among working-age adults in most developed countries. It affects eyes bilaterally and is generally believed to be symmetrical, yet there are few studies evaluating the symmetry of diabetic retinopathy. The purpose of the present study was to evaluate the symmetry of the amount of peripheral retinal ischemia in patients with diabetic retinopathy.
MethodsUltra-widefield fluorescein angiography images were obtained on both eyes of 54 subjects, mean age 56.4 years, from an urban eye clinic. A single, high quality image from the arteriovenous phase of the angiogram of each eye was selected for analysis. The total area of gradable fundus and area of nonperfusion seen in the arteriovenous phase of the ultra-widefield fluorescein angiogram were determined. An ischemic index (ISI) was calculated by dividing the non-perfused retinal area by the total retinal area and multiplying by 100.
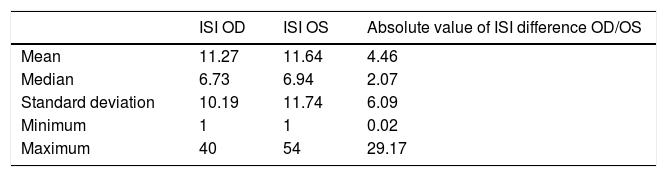
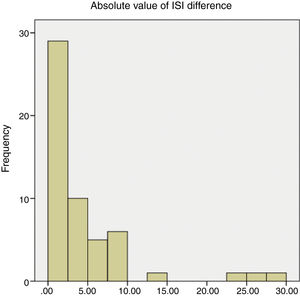
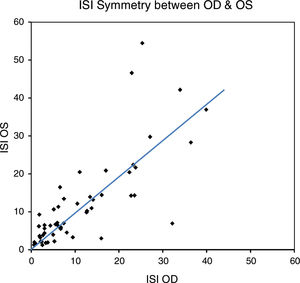
ResultsThe mean ISI OD was 11.27, mean ISI OS was 11.64. The mean absolute value (±SD) of ISI difference between OD and OS was 4.46±6.09. A difference in ISI of 10% or less was found in 92.6% of subjects. A statistically significant correlation was found in the ISI between right and left eyes (rs=0.80, p<0.0001) and there was no statistically significant difference in ISI between the right and left eyes (p=0.85).
ConclusionAsymmetrical retinopathy in diabetic patients is uncommon and additional pathological processes should be considered in the presence of asymmetric DR.
La retinopatía diabética constituye la causa principal de ceguera entre los adultos en edad productiva en muchos países desarrollados. Afecta a los ojos bilateralmente, y por lo general se piensa que es simétrica, aunque existen pocos estudios que evalúen la simetría en esta situación. El objetivo del presente estudio fue evaluar la simetría de la cantidad de isquemia en la retina periférica en pacientes con retinopatía diabética.
MétodosSe obtuvieron imágenes de ambos ojos mediante angiografía fluoresceínica de campo ultra-amplio, en 54 sujetos, con edad media de 56,4 años, en una clínica ocular urbana. Se seleccionó para análisis una única imagen de gran calidad de la fase arteriovenosa del angiograma de cada ojo. Se determinaron el área total de fondo graduable y el área de no perfusión observados en la fase arteriovenosa de la angiografía fluoresceínica de campo ultra-amplio. Se calculó el índice isquémico (ISI) dividiendo el área de la retina no perfundida entre el área total de la retina, multiplicado por 100.
ResultadosEl ISI OD medio fue de 11,27, el ISI OS medio fue de 11,64. El valor absoluto medio (± SD) de la diferencia de ISI entre OD y OS fue de 4,46 ± 6,09. Se encontró una diferencia de ISI del 10% o menos en el 92,6% de los sujetos. Se encontró una correlación estadísticamente significativa de ISI entre los ojos derecho e izquierdo (rs = 0,8, p < 0,0001), y no se encontró diferencia estadísticamente significativa de ISI entre los ojos derecho e izquierdos (p = 0,85).
ConclusiónLa retinopatía asimétrica en pacientes diabéticos es infrecuente, por lo que deberán considerarse procesos patológicos adicionales en presencia de RD asimétrica.
Diabetes mellitus affects approximately 422 million individuals worldwide and the global prevalence has nearly doubled since 1980.1 Diabetic retinopathy (DR) is the leading cause of blindness among working-aged adults and affects about 92 million people globally.2 Owing to the systemic nature of the disease, DR affects eyes bilaterally and usually develops in a relatively symmetric pattern over time, although few studies have looked at this directly. Laron et al. investigated the spatial correspondence of abnormal multifocal electroretinogram responses in adolescents with type 1 diabetes and no retinopathy. Their results showed high agreement (68–94%) of inter-ocular correspondence of locations of abnormal multifocal electroretinogram implicit times, suggesting a symmetrical disease process even before the presence of clinically visible DR.3 Iino et al. prospectively followed a cohort of diabetic patients with and without symmetrical DR for the development of brain infarction. While not the main outcome of their study, they reported that only 12 of 142 (8.4%) patients had asymmetric retinopathy.4 Other studies have reported asymmetric DR in 5–10% of patients with proliferative disease.5
There has been increasing interest in peripheral retinal involvement in DR. Predominantly peripheral lesions have been associated with an increased risk of progression of both non-proliferative diabetic retinopathy and of conversion to proliferative disease. Predominantly peripheral lesions are identified by more than 50% of the lesion being located outside the seven standard fields of the Early Treatment Diabetic Retinopathy Study (ETDRS).6 These peripheral lesions are hypothesized to come from underlying capillary non-perfusion.7 Recent technological advances have greatly improved the evaluation of capillary function in the peripheral retina. Compared to standard fluorescein angiography which covers 15% of the retinal surface with the 45 degree images, ultra-widefield fluorescein angiography (UWFA) provides extended peripheral retinal views and covers 82% of the retina with the 200 degree field of view, captured in a single frame.8
The purpose of this study was to evaluate the symmetry of the amount of peripheral retinal nonperfusion in patients with diabetic retinopathy. In this article, we define symmetry as the likeness of the total value of peripheral non-perfusion as measured by ischemic index (ISI) in the right eye compared to the left eye. To our knowledge, no prior studies have reported on this.
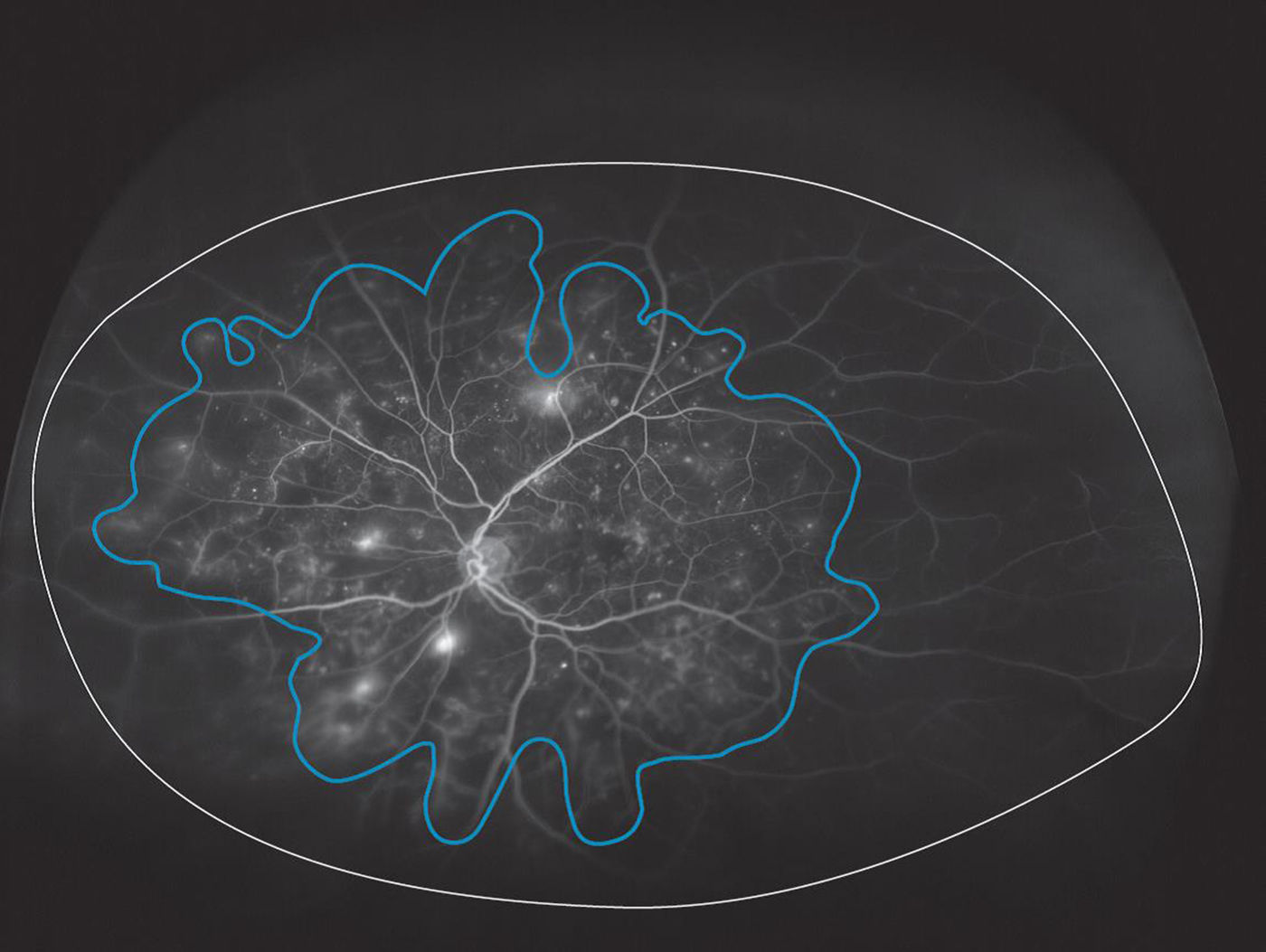
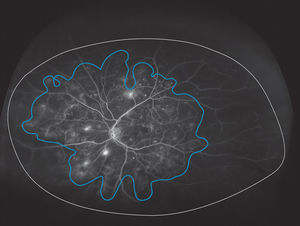
MethodsThe study protocol and informed consent were approved by the Illinois College of Optometry Institutional Review Board and followed the tenets of the Declaration of Helsinki. Informed consent was obtained from all subjects and 58 individuals with DR were enrolled from the Illinois Eye Institute, an urban primary eye clinic in this cross-sectional, prospective study. Patients with prior panretinal photocoagulation treatment or a history of significant retinal vascular pathology (vein occlusion, artery occlusion or retinal macroaneurysm) were excluded. UWFA images were obtained on both eyes at the same visit using an Optos C200 MA scanning laser ophthalmoscope (Optos PLC, Dunfermline, United Kingdom) following standard intravenous infusion with 5cc of 10% sodium fluorescein. The same certified retinal photographer obtained all images; taping of eyelids was performed at the discretion of the photographer. Two subjects were excluded from the study because of poor quality of UWFA images in both eyes. In another two subjects’, good quality UWFA images were obtained in the left eyes but not in right eyes; one of these subjects had mild nonproliferative DR (NPDR) and the other severe NPDR. Images were saved digitally and reviewed using the V2 Vantage Review software (Optos, PLC) to allow enhancement and high resolution zoom functionality. All images were reviewed by a single fellowship-trained retinal specialist (S.I.) and compared to Optos fundus images for identification of eyelid or eyelash artifact. As previously described9–11 a single, high quality image, based on clarity and greatest field of view, was selected from the arteriovenous phase (between 45s and 2min) of the angiogram for each eye. Each image was graded for the presence or absence of capillary non-perfusion and the reviewer was allowed to enhance the images by adjusting contrast, brightness, gamma and using the smoothing and zoom functions. Using the area measurement function in the V2 Vantage Review software (Optos, PLC), the reviewer determined both the total area of gradable fundus and area of peripheral nonperfusion seen in the arteriovenous phase of the UWFA (Fig. 1). The total gradable retinal area and peripheral non-perfusion area was calculated by area of pixels.2 Retinal vascular leakage was not considered to be nonperfusion. An ISI was calculated by dividing the non-perfused retinal area by the total retinal area and multiplying by 100. An ISI value of 0 indicates a fully perfused retina while an ISI of 100 indicates complete absence of retinal capillary perfusion. Images were saved as Joint Photographic Experts Group (jpeg) files and data stored in Excel. Self-reported data were collected from patients at the time of enrollment including: age, race, type of diabetes, length of diagnosis, and hemoglobin A1c. An electronic medical record review of each patient enrolled provided data on visual acuity and clinical grading of DR severity.
Kolmogorov–Smirnov test showed that ISI was not normally distributed. Mean ISI of OD and OS was calculated. Spearman correlation was performed to measure the correlation in ISI between the right and left eyes (n=54) and correlation between mean ISI (n=56) and severity of DR. A Mann–Whitney test was used to test the difference in ISI between the two eyes. All data were analyzed using Statistical Package for Social Sciences (IBM SPSS version 21.0; SPSS Inc., Chicago, IL). A p value of <0.05 was considered statistically significant.
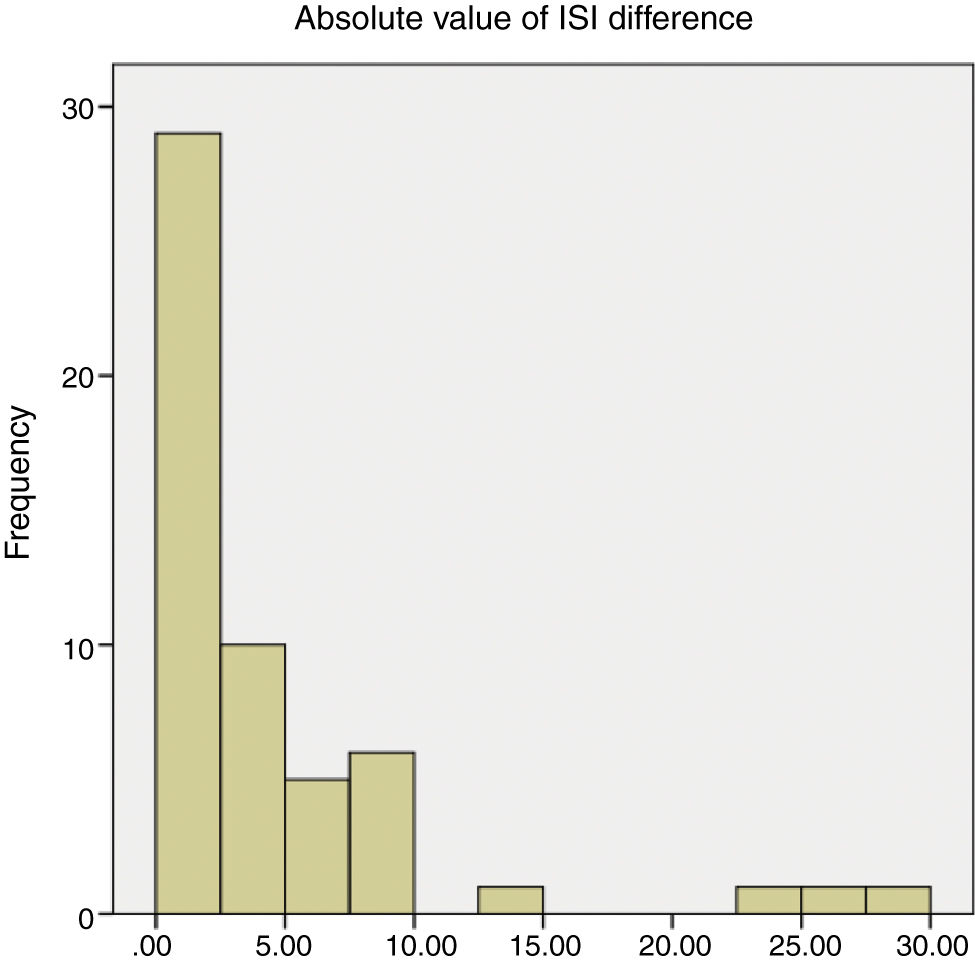
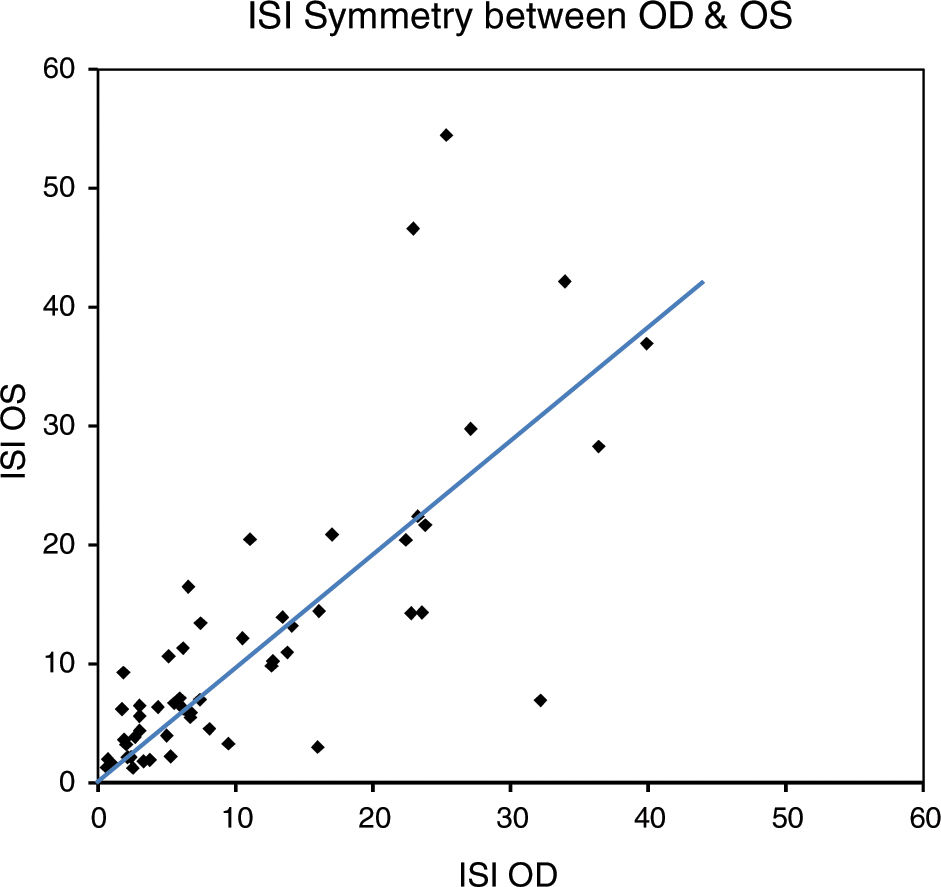
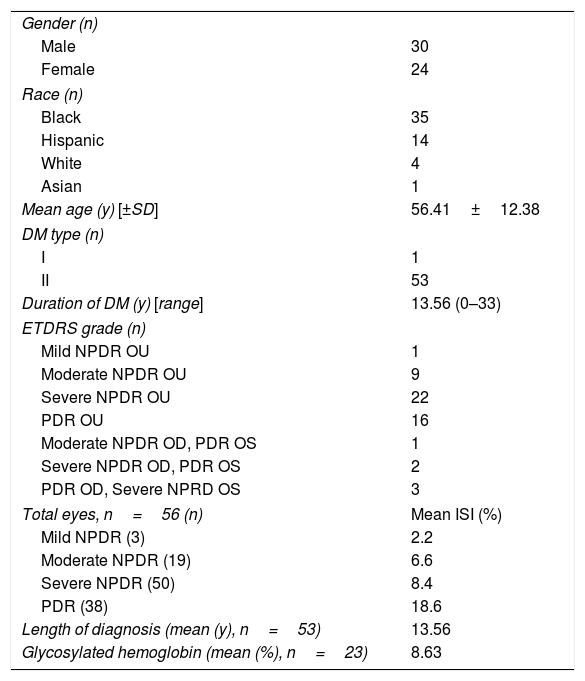
ResultsBaseline characteristics of all 54 subjects are displayed in Table 1. Descriptive statistics for the ISI OD, OS and the difference in ISI are displayed in Table 2. The mean (±SD) ISI was 11.27 and 11.64 in the right and left eyes, respectively. The mean absolute value of ISI difference between OD and OS was 4.46±6.09. Fig. 2 displays the distribution of the absolute value of ISI difference between OD and OS. A difference in ISI of 10% or less was found in 92.6% of subjects and 72.2% had a difference of 5% or less between the two eyes. For the bilateral data (n=54), a statistically significant correlation was found in the ISI between right and left eyes (rs=0.80, p<0.001) (Fig. 3) and there was no statistically significant difference in ISI between the right and left eyes (p=0.85). ISI OD (rs=0.319, p=0.015), ISI OS (rs=0.521, p<0.001) and mean ISI (rs=0.470, p<0.001) were shown to be significantly correlated with severity of DR.
Baseline characteristics for subjects, n=54.
| Gender (n) | |
| Male | 30 |
| Female | 24 |
| Race (n) | |
| Black | 35 |
| Hispanic | 14 |
| White | 4 |
| Asian | 1 |
| Mean age (y) [±SD] | 56.41±12.38 |
| DM type (n) | |
| I | 1 |
| II | 53 |
| Duration of DM (y) [range] | 13.56 (0–33) |
| ETDRS grade (n) | |
| Mild NPDR OU | 1 |
| Moderate NPDR OU | 9 |
| Severe NPDR OU | 22 |
| PDR OU | 16 |
| Moderate NPDR OD, PDR OS | 1 |
| Severe NPDR OD, PDR OS | 2 |
| PDR OD, Severe NPRD OS | 3 |
| Total eyes, n=56 (n) | Mean ISI (%) |
| Mild NPDR (3) | 2.2 |
| Moderate NPDR (19) | 6.6 |
| Severe NPDR (50) | 8.4 |
| PDR (38) | 18.6 |
| Length of diagnosis (mean (y), n=53) | 13.56 |
| Glycosylated hemoglobin (mean (%), n=23) | 8.63 |
DM, diabetes mellitus; NPDR, nonproliferative diabetic retinopathy; PDR, proliferative diabetic retinopathy.
A number of conditions have been reported to be associated with asymmetric DR, including ipsilateral carotid artery disease and posterior vitreous detachment.5 A retrospective review of diabetic patients with asymmetric retinopathy showed that history of branch vein occlusion was a statistically significant risk factor for asymmetry while chorioretinal scarring was protective against proliferative disease. Yet in the majority of patients (34/57), no intraocular risk factors or protective factors were identified.12 Cases of asymmetric DR warrant further investigation to identify any additional contributing pathology, including ocular ischemic syndrome which is associated with high morbidity and mortality.13
The results of our study support the hypothesis that DR is symmetrical and are consistent with other reports of symmetry in the literature based on Photos.3,4 Utilization of UWFA allows for evaluation of symmetry at a microvascular level, inclusive of the retinal periphery. This may be helpful in more precisely identifying the degree of retinopathy compared to standard funduscopic assessment. Price et al. compared severity of diabetic retinopathy grading between Optos ultra-widefield (UWF) images and the seven-standard fields of the ETDRS, and found 19% of the UWF images were assigned a more severe retinopathy level compared to that with the seven-field view.14 Similarly, Rocha et al. compared the level of DR identified in UWF images with that identified with UWFA and found that for nonproliferative DR, UWFA identified more severe DR than ultra-widefield fundus Images.15 Therefore, UWFA may be more precise in identification of DR than clinical fundus exam or UWF images.
There can be a wide range of clinical findings at similar stages of disease in DR. An eye with extensive hemorrhaging in four quadrants would be classified as severe nonproliferative DR per ETDRS grading classification, yet an eye with very few hemorrhages but subtler ischemic findings such as venous beading in two quadrants or intra-retinal microvascular abnormalities in just one quadrant would be classified the same. Clinicians must be diligent not to overlook the subtler signs of ischemia when grading DR. Wessel et al. reported 3.9 times more nonperfusion, 1.9 times more neovascularization and 3.8 times more panretinal photocoagulation scars in UWFA images compared to the seven standard field ETDRS Images.16 Thus, supplemental evaluation with UWFA may help eliminate misidentification of asymmetry that may seem apparent clinically or identify asymmetry that might otherwise be missed. This can help to both avoid and seek additional work-up to rule out unilateral carotid or ophthalmic artery disease as is often suspected in unilateral presentations of DR.13 Calculation of an ISI aides in the evaluation of symmetry by providing a means to quantify and compare the extent of capillary non-perfusion between eyes.
Quantification of retinal nonperfusion may be clinically useful but the determination of perfused and nonperfused retina can be challenging. Interpretation of UWFA images is complicated by reduced image clarity in the retinal periphery and eyelid/eyelash artifact. Both can create difficulty separating perfused and nonperfused areas, thus affecting the perfused to nonperfused ratio. These limitations were minimized in this study by comparing UWFA to color Optos images obtained in the same sitting. This allowed S.I. to identify and exclude eyelid/eyelash artifacts from gradable fundus area.
Our study is limited by the variability in image quality and subjectivity inherent in grading UWFA images. Tsui and colleagues investigated the reliability of a calculated ISI by means of intergrader and intragrader agreement on UWFA and compared agreement of DR images to those with branch vein occlusion (BRVO). In their study, grading and calculation of an ISI was performed by eight retinal specialists on two separate days. Intra- and intergrader variation had a standard deviation of 12.5% for DR and 2.9% (intragrader) and 2.5% (intergrader) for BRVO. Their study suggests a greater variation in ISI calculation for patients with DR compared to BRVO though it is unclear if this standard deviation is actually high or clinically relevant.17 In contrast to Tsui's findings, Wessel et al. found excellent intergrader correlation for nonperfusion in diabetic patients imaged with UWFA.16 In our study, utilization of a single, experienced grader eliminates intergrader variability. Additionally, images from both eyes were graded on the same day which may have a positive effect on intragrader variability. However, we also recognize that the grading of both eyes in succession could impart bias due to the expectation of symmetry with DR, but, at the time of the grading the specialist was blinded as to the purpose of the study. Because the purpose of the study was to evaluate symmetry of peripheral nonperfusion in eyes with DR, the absolute value of nonperfusion is not as critical as consistency in grading between eyes. We consider a 12.5% (or less) intragrader standard deviation to be acceptable and thus a single, experienced grader sufficient for our study.
Since the conclusion of this study, advances in software have allowed for correction of peripheral warp present in ultra-widefield images. Due to the elliptical mirror used in the Optos system, images are distorted in a nonlinear manner which results in peripheral lesions appearing larger than they are.18 The actual area of lesions with a similar number of pixels can differ significantly because the retinal area covered by a single pixel changes from the center to the periphery of the image.19 Tan and colleagues used stereographic projection software to determine the actual retinal area (mm2) of total gradable and nonperfused retina in a cohort of patients with retinal vein occlusions and compared corrected measures of nonperfusion to the original ISI calculated in pixels as described previously. They found that corrected nonperfusion percentage correlated well with uncorrected ISI (Spearman correlation R=0.978, p<0.001) and the mean difference was 1.4%. In the majority of eyes (84.4%), the difference between uncorrected and corrected nonperfusion percentage was within ±5%.19 While correction of peripheral nonlinear warp has merit, it is unlikely to greatly affect the outcome of our study.
Our data is skewed toward more severe retinopathy with 45/56 patients having at least severe nonproliferative DR in 1 or both eyes. It is possible that a more balanced representation of DR could yield different results.
ConclusionOur findings suggest that peripheral retinal nonperfusion is symmetrical in diabetic retinopathy and supports the conclusions of other studies that additional pathological processes should be considered in the presence of asymmetric DR. Future studies might look to see if the symmetry of DR as assessed by ISI is affected in patients with varying levels of carotid artery occlusion or if ISI changes following cataract surgery.
FundingThis study was supported in-part by a research grant from the Illinois Society for the Prevention of Blindness.
Conflicts of interestThe authors have no conflicts of interest to declare.
The authors would like to thank Rebecca Tudor CRA for her involvement in this study.