This study analyses strategies and attitudes on myopia management reported by eye care practitioners (ECP) from Spain in 2022.
MethodsA questionnaire was distributed to ECPs worldwide via the internet through professional associations. The questionnaire was distributed by email to all registered Spanish optician-optometrists. Questions examined awareness of increasing myopia prevalence; perceived efficacy; uptake of available approaches; and reasons preventing further uptake of specific approaches.
ResultsOf 3,107 practitioners who participated in the study, 380 were Spanish ECPs. Using a 10-point scale, Spanish practitioners reported less concern about increasing pediatric myopia (8.3 ± 1.6) compared to ECP's worldwide (8.5 ± 1.9) (p < 0.001), but similar level of clinical activity in myopia control (7.8 ± 2.3 vs. 7.5 ± 2.5, respectively) (p > 0.05); however, around half of all prescribed treatments were single-vision distance spectacles/contact lenses both in Spain and in most regions, with Spanish practitioners prescribing less single-vision spectacles than African and Asian (p < 0.001), but more than Australasian practitioners (p = 0.04). No significant differences were found between Spain and the other regions in the perceived efficacy of combined therapy, orthokeratology, and outdoor time (p > 0.05), with the former being perceived as the most effective myopia control method followed by orthokeratology. No significant differences were found between Spain and the world's average in factors preventing the prescription of myopia control approaches (p > 0.05). Spanish practitioners reported that embracing myopia management has a positive, but lower impact on customer loyalty, practice revenue and job satisfaction compared with the other regions (all p < 0.001).
ConclusionsMyopia control is increasing, although around half of practitioners still prescribe single-vision distance spectacles/contact lenses to young/progressive myopes. Combined therapy followed by orthokeratology were perceived as the most effective treatments. Embracing myopia management improved patient loyalty and job satisfaction.
Given the increasing prevalence of myopia around the world, particularly among younger generations in East and Southeast Asia, myopia has become a global health problem, affecting nearly 30 % of the world's population. Furthermore, by 2050, the prevalence is projected to increase to 50 % globally, of which 10 % are forecasted to have high degrees of myopia.1 Myopia has a negative impact on both individuals and society as a whole.2 As the prevalence of myopia and high myopia increase, so do so the lifetime pathological manifestations of myopia, the direct health expenditure, and the indirect costs such as lost productivity and reduced quality of life, with the latter being affected depending on the type of visual correction used.3 As a result of all this, there is increasing interest in developing effective therapies to prevent myopia onset and slow myopia progression, with a number of approaches showing promising results; some of them have received regulatory approval specifically for this indication.
Due to the increasing interest in myopia management, Wolffsohn et al.4 conducted a global survey in 2015 to better understand current trends in myopia management in clinical practice. The same study was repeated in 2019 to evaluate how these trends might have changed over time.5 Both surveys identified a high level of eye care practitioner concern/activity about myopia; however, the majority of practitioners were found to prescribe single-vision interventions to young myopes, although an increased level of activity was found in the 2019 vs the 2015 survey. The same study was repeated a third time in 2022 to assess how global trends in myopia management attitudes and strategies in clinical practice might have changed compared to previous years.6 This latter study found that more practitioners across the globe are practicing myopia control, but there are still significant differences between and within continents. Furthermore, practitioners reported that embracing myopia control enhanced patient loyalty, increases practice revenue and improves job satisfaction.
The results found in Spain in the 2019 survey have been previously reported.7 In brief, it was found that the acceptance of myopia control methods by Spanish eye care practitioners was also relatively low. Orthokeratology was considered the most effective myopia control method. However, the prescription of single-vision spectacles/contact lenses also remained the most popular form of visual correction prescribed to myopic children. The main reasons for not prescribing myopia control methods were found to be elevated cost, insufficient information and variable treatment results,7 in line with the rest of the regions of the world assessed in the study. The present study reports the results found in Spain in the survey conducted in 2022 and compares these findings against those found in other parts of the world as well as against those found in previous surveys.
Materials and methodsThe methods of this study have been previously reported.6 In brief, a questionnaire was developed in English and subsequently translated into seven different languages (i.e., Chinese, French, German, Italian, Portuguese, Russian and Spanish). Questionnaires were then sent through various professional bodies to reach eye care practitioners worldwide (i.e., opticians, optometrists and ophthalmologists, among others) using SurveyMonkey software (Palo Alto, California, USA). Ethics approval for the study was obtained from the Aston University Research Ethics committee (Birmingham, United Kingdom). The nature of the study and data collection was described in the invitation to participate in the survey, thus informed consent was received from all respondents by submitting the survey. No personal or identifiable data was collected from any of the survey respondents. In Spain, the questionnaire was disseminated by email to all registered optician-optometrists in the country through the Spanish General Council of Optician-Optometrists as well as through other Spanish eye care organizations between March and November 2022. The questionnaire collected details of the type of professional that responded to the survey (i.e., optometrist, ophthalmologists or other), the principal working environment of the respondent (i.e., clinical practice, and academic or industry setting) as well as the number of years that the eye care practitioner has been qualified (in year ranges of 1–5, 6–10, 11–20, 21–30, and 31 or more). The questionnaire was made up of the following nine questions:
- 1.
Level of concern about the increase in the incidence of pediatric myopia in clinical practice (quantified from “not at all” to “extremely concerned” on a 10-point scale).
- 2.
Perceived effectiveness, defined as the expected level of reduction in the progression of pediatric myopia of several clinical methods of myopia control (quantified as a percentage from 0 to 100 %).
- 3.
How active they would consider their clinical practice in the area of myopia control (quantified from “not at all” to “extremely active” on a 10-point scale).
- 4.
Frequency with which different methods of myopia correction are prescribed to young/progressive myopic patients in an average month.
- 5.
Minimum patient age for which prescription of a myopia control method is considered (assuming that the management skills and motivation of the child/parent are sufficient).
- 6.
Minimum level of myopia that would need to be present to consider prescribing a myopia control method (specified in 0.50D steps).
- 7.
Minimum level of myopia progression (dioptres/year) that would prompt a practitioner to specifically adopt a myopia control approach (specified in 0.25D steps).
- 8.
Frequency with which single-vision under-correction is prescribed as a strategy to slow the progression of myopia (quantified as “never”, “sometimes” or “always”).
- 9.
If they had only ever fitted single-vision spectacles/contact lenses for myopic patients, what had prevented them from prescribing alternative refractive correction methods (multiple options could be selected)? These options were:
- •
They don't believe that these are any more effective
- •
The outcome is not predictable
- •
Safety concerns
- •
Cost to the patient makes them uneconomical
- •
Additional chair time required
- •
Inadequate information/knowledge
- •
Low benefit/risk ratio
- •
Other
- •
- 10.
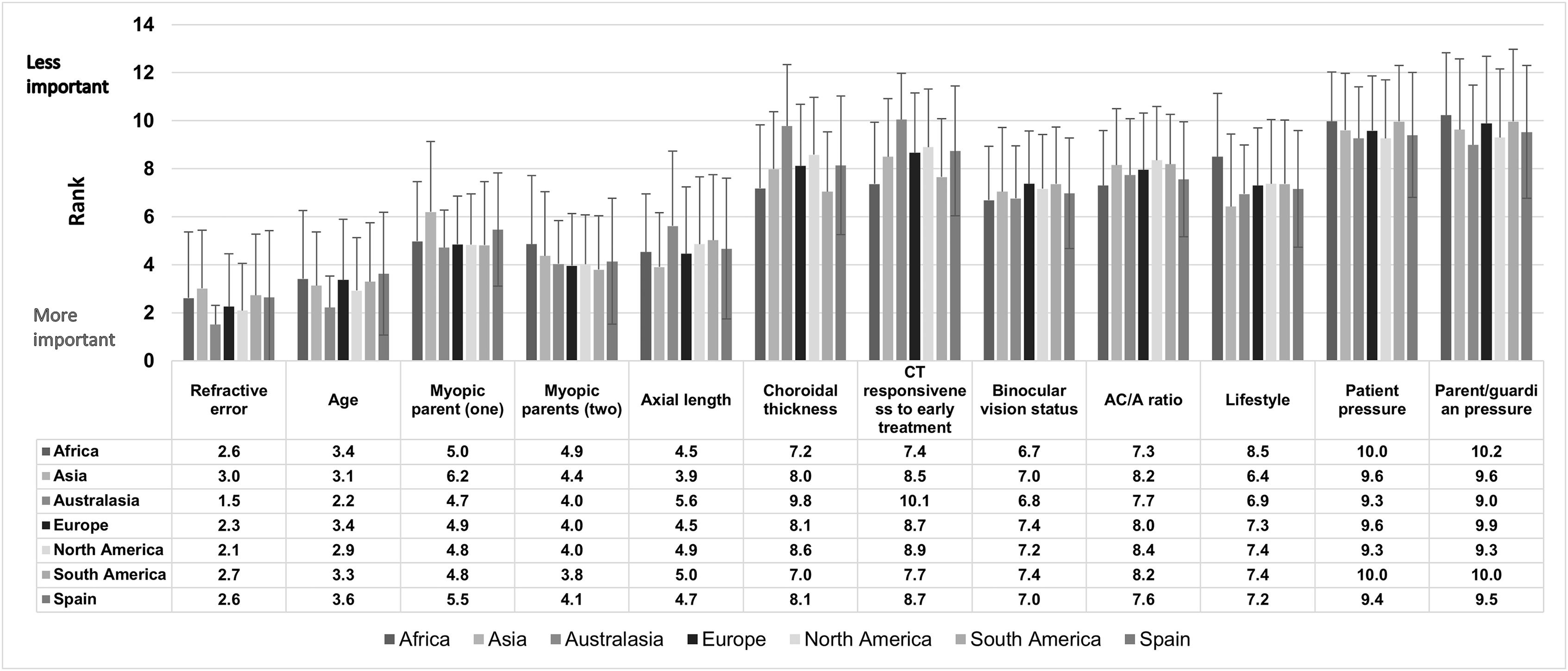
Selection of criteria for the decision to adopt a myopia control method (quantified on a scale of 1–12 based on the least important to the most important).
- •
Refractive error
- •
Age
- •
Myopic parent (one)
- •
Myopic parents (two)
- •
Axial length
- •
Choroidal thickness
- •
Choroidal thickness responsiveness to early treatment
- •
Binocular vision status
- •
AC/A ratio
- •
Lifestyle
- •
Patient pressure
- •
Parent/guardian pressure
- •
- 11.
Criteria for the selection of the first strategy to start myopia control in a young myope. The options (all relevant options could be selected) consisted of:
- •
There is only one method available to me
- •
I am only comfortable using/trained to use one method
- •
Age
- •
Refractive error (non-cycloplegic)
- •
Cycloplegic refraction
- •
Axial length
- •
Choroidal thickness
- •
Binocular vision status
- •
Patient preference
- •
Parent/guardian preference
- •
Other (please specify)
- •
- 12.
Frequency of follow-up of myopic children who have adopted a myopia control method (in months).
- 13.
Reason for modifying a myopia control method/approach. The options (all relevant options could be selected) consisted of:
- •
I don't
- •
Progression of refractive error
- •
Progression of axial length
- •
Changes in choroidal thickness
- •
A new treatment with a scientifically reported greater effectiveness became available
- •
Poor compliance
- •
Complications
- •
Other (please specify)
- •
- 14.
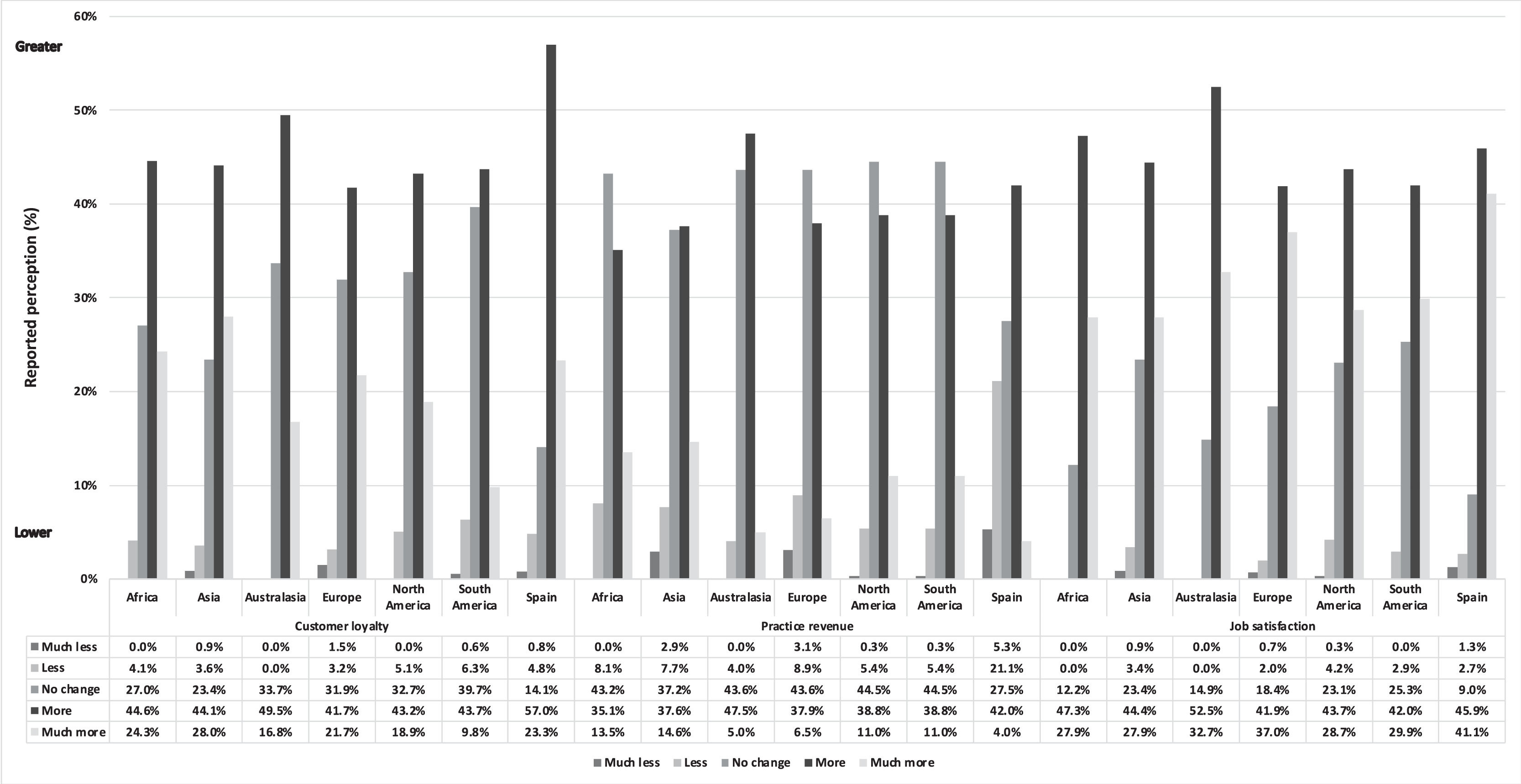
How has managing myopia changed their patient loyalty, practice revenue and job satisfaction (each rated as “much less”, “less”, “no change”, “more” or “much more”).
The results reported by Asian, Australasian, European [excluding Spain], North American and South American eye care practitioners were analyzed and compared against those reported by Spanish eye care practitioners.
Statistical analysisData analysis was conducted using SPSS 25.0 software (SPSS Inc., Chicago, Illinois, USA). Normality of the data was assessed using the Shapiro Wilk normality test. As all variables were found not to have a normal distribution, data was analyzed using the Kruskal–Wallis, Mann–Whitney U and Chi-square tests. The level of statistical significance was taken as 5 %.
ResultsDemographicsA total of 3,107 eye care practitioners responded to the survey, of whom 74 were from Africa, 1,396 from Asia, 101 from Australasia, 931 from Europe, 338 from North America, and 177 from South America. Among the 931 surveys collected in Europe, 380 provided data from Spanish eye care practitioners. Of all the questionnaires obtained worldwide, 64.5 % were provided by optometrists, 27.5 % by ophthalmologists, 5.2 % by contact lens opticians and the remaining 2.8 % by other eye care practitioners. In Spain, 99.0 % of all questionnaires obtained were provided by optometrists, 0.8 % by ophthalmologists and the remaining 0.3 % by other eye care practitioners; this is estimated to account for approximately 2 % of all practicing optometrists in the country.
Most practitioners who participated in this study, both worldwide and from Spain, reported working in clinical practice (worldwide: 78.1 %; Spain: 80.0 %). The remaining practitioners reported working in an academic (worldwide: 8.3 %; Spain: 3.2 %) or industry (worldwide: 5.5 %; Spain: 5.2 %) setting. Worldwide and in Spain, most eye care practitioners reported being qualified to practice between 11 and 30 years.
Self-reported concern about the increasing frequency of childhood myopiaOverall, practitioners worldwide reported a higher concern regarding the increase in childhood myopia (8.5 ± 1.9) in comparison to practitioners from Spain (8.3 ± 1.6) (p < 0.001). Practitioners in Spain were less concerned than those from Asia (p < 0.001), but showed similar level of concern as those from Africa, Australasia, Europe, South America and North America (p > 0.05). Within Europe, practitioners from Spain were more concerned than those from Denmark (p = 0.034) and Switzerland (p = 0.002), but reported a similar level of concern as those from the other European countries (p > 0.05). In contrast with the other regions, no significant differences were found among Spanish practitioners between level of concern and years of experience (p > 0.05).
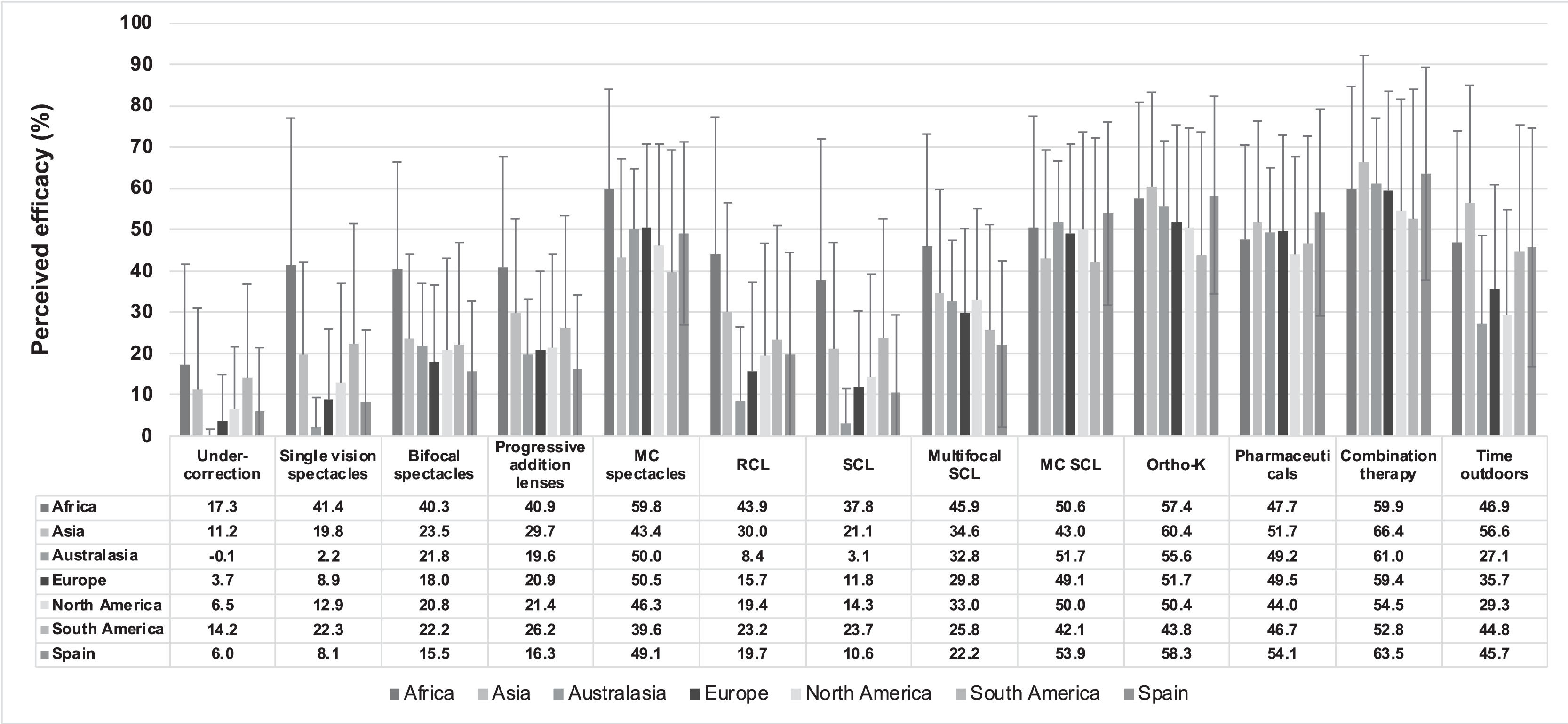
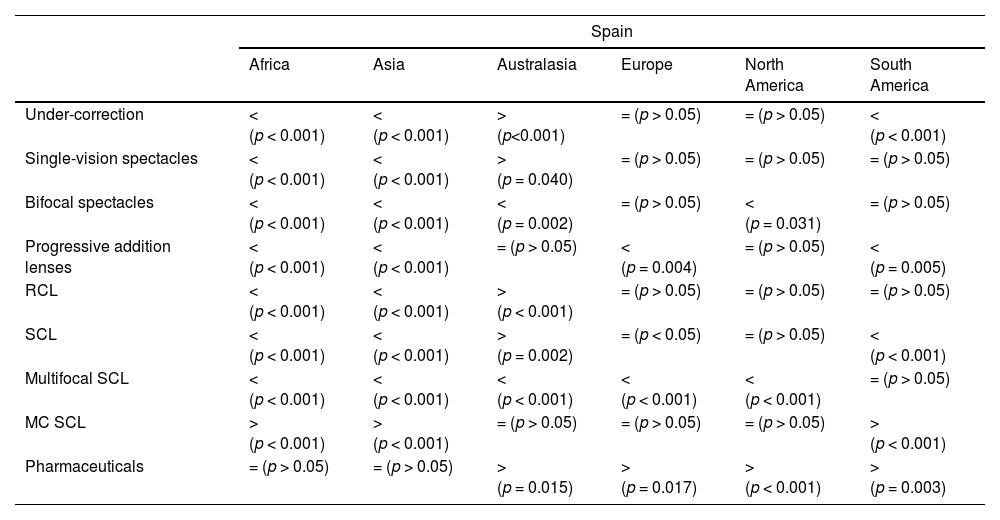
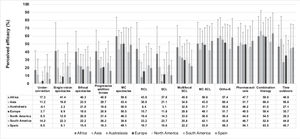
Practitioners’ perceived effectiveness of management options for myopia controlPractitioners around the world perceived combination therapy as the most effective method of myopia control (62.4 % [95% confidence intervals {CI}: 61.5–63.4]), followed by orthokeratology (56.3 % [CI: 55.5–57.2]), pharmaceuticals (50.3 % [CI: 49.4–51.2]) and soft contact lenses approved for myopia control (46.7 % [CI: 45.8–47.7]). Similarly, Spanish practitioners also reported combined treatment methods (63.5 % [CI: 60.9–66.2]), followed by orthokeratology (58.3 % [CI: 55.8–60.8]) and pharmaceuticals (54.2 % [CI: 51.5–56.7]) as the most effective myopia control methods (Fig. 1). Comparison between Spain and some of the other regions revealed significant differences in terms of the perceived efficacy of single-vision distance undercorrection, single-vision spectacles, bifocal spectacles, progressive addition lenses, myopia control spectacles, rigid contact lenses, single-vision soft contact lenses, multifocal contact lenses, myopia control soft contact lenses and pharmaceuticals (Table 1). In contrast, the efficacy of orthokeratology, combined therapy and outdoor time was reported to be equally effective by Spanish practitioners in comparison with those from the other regions in (p < 0.05). The fewer years of Spanish practitioners’ experience the higher the level of efficacy reported for single-vision spectacles (p = 0.005), myopia control spectacles, and myopia control soft contact lenses (both p < 0.001). On the other hand, the more years of professional experience the greater the perceived effectiveness of orthokeratology reported by Spanish practitioners (p = 0.037). Taking the results reported by optometrists worldwide alone (given that Spanish optometrists cannot prescribe pharmaceuticals such as atropine), optometrists from North America (44.0 ± 23.0; p < 0.001) and Australasia (47.8 ± 22.8; p = 0.003) reported lower perceived efficacy for pharmaceutical treatments than Spanish optometrists (54.5 ± 25.6); however, no significant differences were found between optometrists from Spain vs. those from the other remaining regions (p > 0.05).
Statistical differences in the perceived effectiveness of myopia control methods between Spain and other regions. RCL, rigid contact lenses; SCL, soft contact lenses; MC SCL, soft contact lens approved for myopia control. Similar levels of efficacy reported by Spanish practitioners; >, Spanish practitioners reported significantly higher levels of efficacy; <, Spanish practitioners reported significantly lower levels of efficacy.
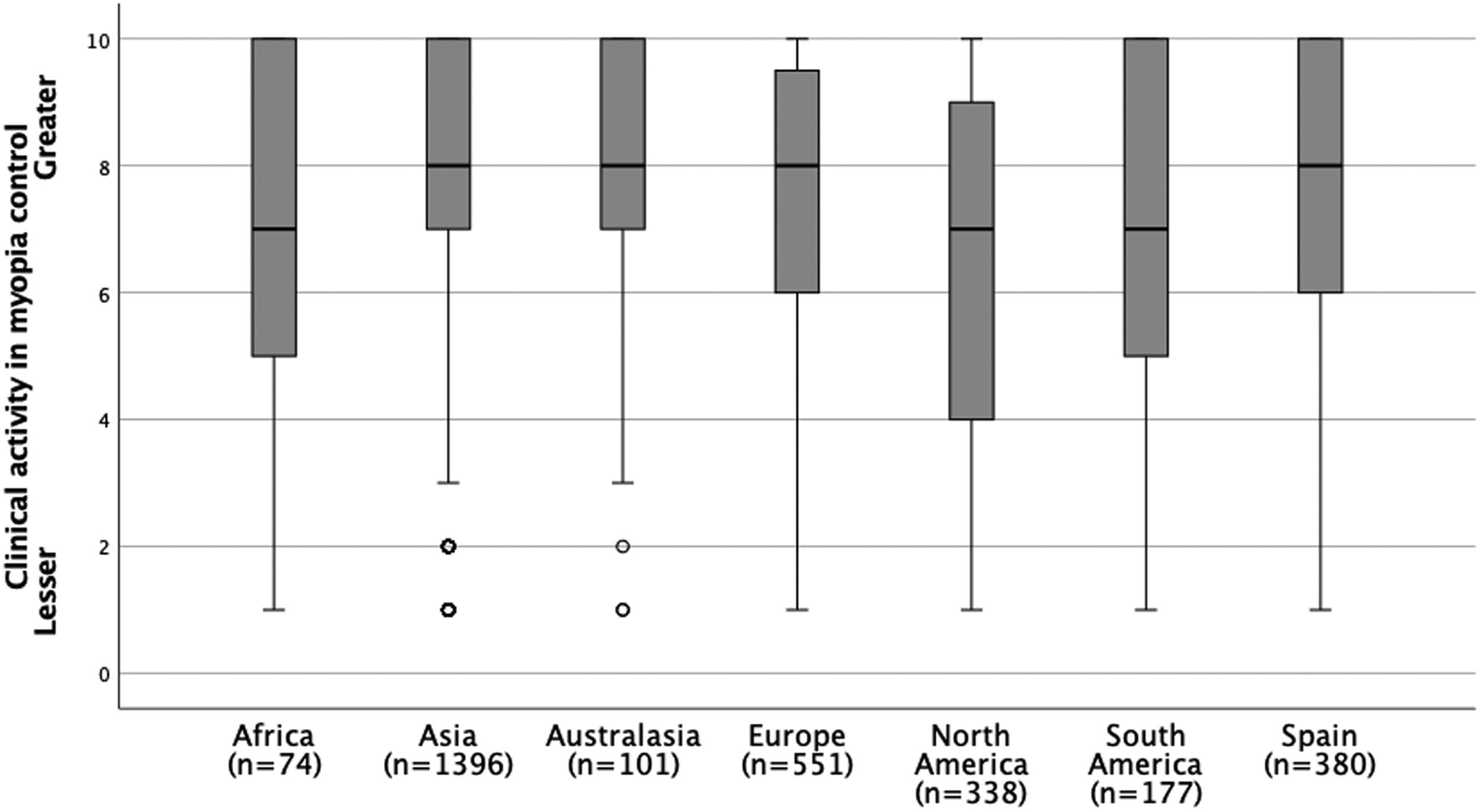
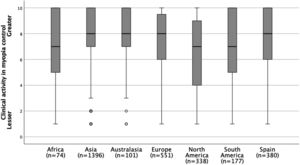
A similar level of perceived clinical activity in the field of myopia control was reported by practitioners from Spain (7.8 ± 2.3) compared with practitioners from the other regions (7.5 ± 2.5) (p > 0.05) (Fig. 2). Spanish practitioners, as well as those from other European countries, reported significant differences between the different age ranges of practitioner experience for the perceived level of clinical activity in myopia control (p < 0.001); as years of practitioner experience increases the perceived level of clinical activity in myopia control also increases.
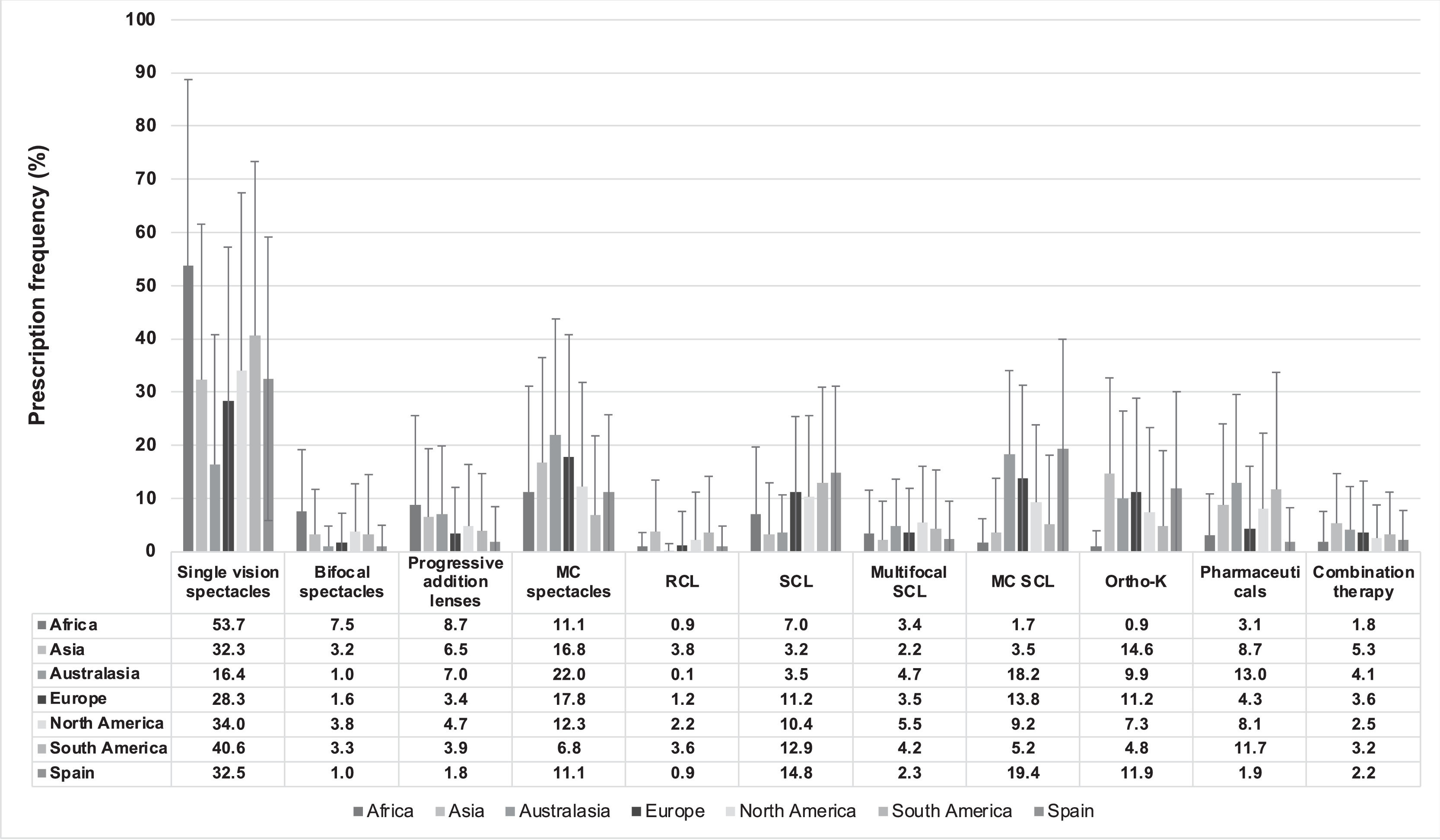
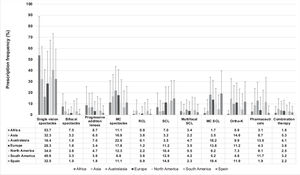
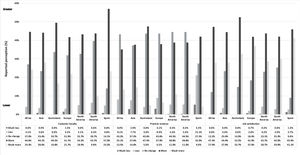
Frequency of prescription of different myopia progression correction methods by practitionersOverall, the most widely prescribed option for young progressive myopes was single-vision spectacles, accounting for 32.2 % (CI: 31.1–33.3) and 32.6 % (CI: 29.8–35.3 %) of all prescriptions reported worldwide and in Spain, respectively (Fig. 3). Myopia control spectacles represented 15.9 % (CI: 15.1–16.7) and 11.1 % (CI: 9.6–12.6) of all prescriptions reported by eye care practitioners worldwide and in Spain, respectively. The prescription frequency of bifocal spectacles, progressive addition lenses (both p < 0.001), myopia control spectacles (p = 0.012), rigid contact lenses, single-vision soft contact lenses, multifocal contact lenses, myopia control soft contact lenses, pharmaceuticals and combined treatments was significantly different between Spanish practitioners and those from the other regions (p < 0.001). In contrast, the prescription frequency of single-vision spectacles and orthokeratology was reported to be similar between Spanish practitioners and those from the other regions (p > 0.05). In Spain, a greater number of years of practitioner experience was associated with a lower prescription frequency of single-vision spectacles, rigid contact lenses and single-vision soft contact lenses (p < 0.001). In contrast, more years of practitioner experience was associated with increased prescription of progressive addition lenses and orthokeratology (p < 0.001).
Frequency of prescription of different myopia correction methods for myopia progression in a typical month. MC, myopia control; RCL, rigid contact lenses; SCL, single-vision soft contact lenses; MC SCL, myopia control soft contact lenses; Ortho-K, overnight orthokeratology. Error bars represent one standard deviation.
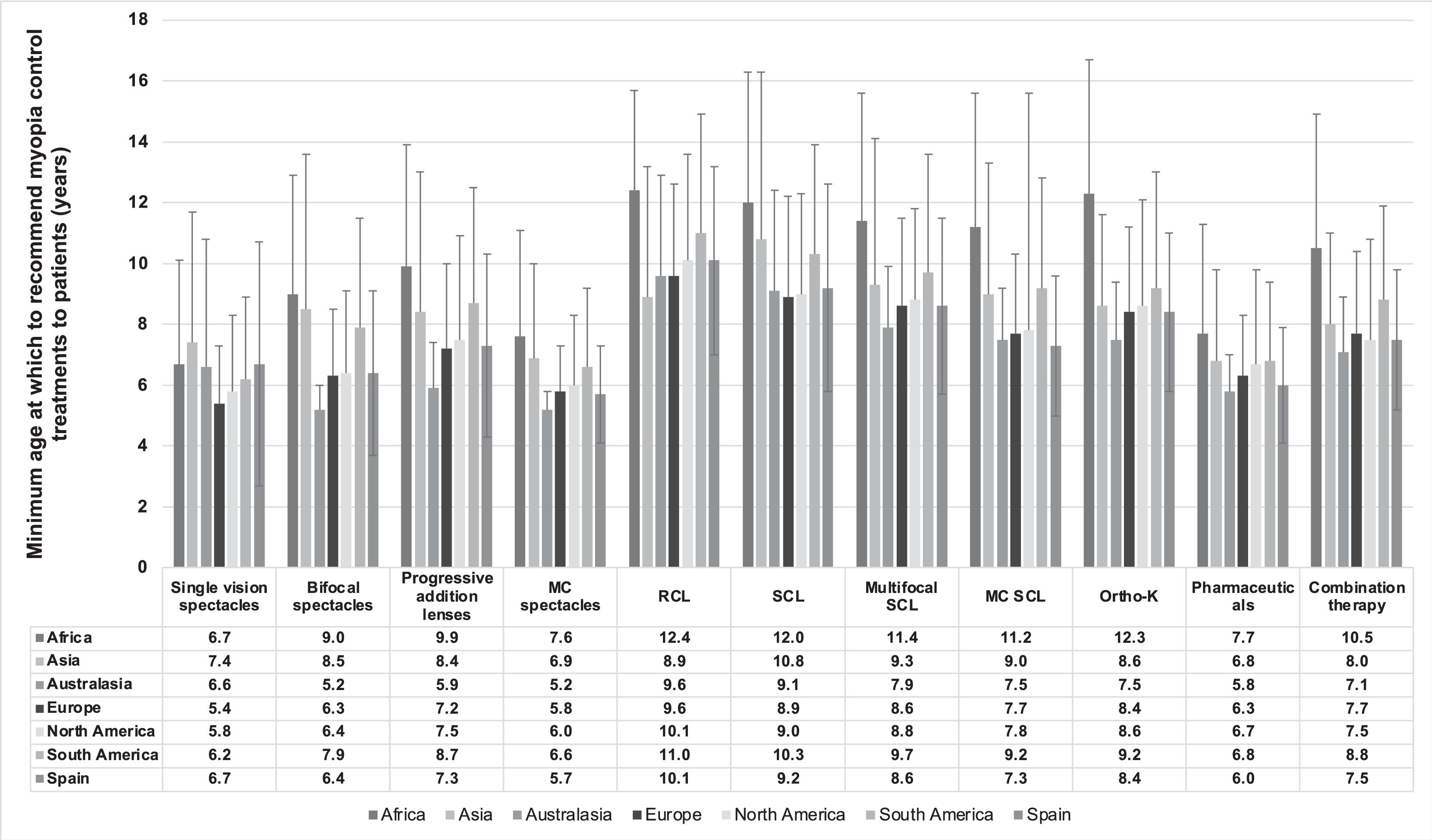
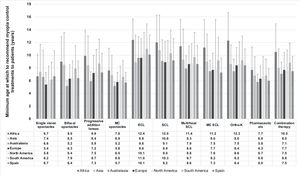
The minimum age at which a myopia control method would be prescribed was found to be significantly different between regions (p < 0.001) (Fig. 4). Myopia control treatments were reported to be prescribed at an older age by eye care practitioners worldwide (8.0 ± 2.4 years [CI: 7.9–8.1]) in comparison with Spanish practitioners (7.5 ± 1.0 years [CI: 7.3–7.7]) (p < 0.001). The prescription of single-vision spectacles, bifocal spectacles, myopia control spectacles, rigid contact lenses, myopia control soft contact lenses and pharmaceuticals were reported to be prescribed at an earlier age by practitioners in Spain compared to practitioners from the other regions (p < 0.001). The age at which to prescribe the remaining myopia management options was found to be similar between regions (p > 0.05). Spanish practitioners recommend the prescription of myopia control soft contact lenses at an earlier age than single-vision soft contact lenses (p < 0.001). In Spain, significant differences between the different categories of practitioners’ experience were only found in the average minimum age at which bifocal spectacles would be prescribed (p = 0.002); as the years of practitioner experience increased the age at which this treatment would be prescribed decreased.
Minimum age (in years) at which eye care practitioners from different regions would recommend different myopia control treatments to patients. MC, myopia control; RCL, rigid contact lenses; SCL, soft contact lenses; MC SCL, myopia control soft contact lenses; Ortho-K, overnight orthokeratology. Error bars represent one standard deviation.
Significant differences were found in the minimum degree of myopia to begin myopia management, with practitioners in Spain recommending prescribing to patients with a slightly higher degree of myopia (−1.06 ± 0.61D [CI: −1.13 to −1.00]) in comparison with practitioners from the other regions (−1.04 ± 0.81D [CI: −1.07 to −1.01]) (p<0.001). African practitioners reported a higher degree of myopia to begin myopia management (−1.59 ± 1.22 D [CI: −1.89 to −1.31]) in comparison with Asian (−0.99 ± 0.74 D [CI: −1.02 to −0.95]), Australasian (−0.64 ± 0.37 D [CI: −0.72 to −0.57]), European (−0.90 ± 0.65 D [CI: −0.96 to −0.85]), North American (−1.29 ± 1.08 D [CI: −1.41 to −1.17]) and South American practitioners (−1.41 ± 0.87 D [CI: −1.54 to −1.28]) (p < 0.001). In Spain, no significant differences were found in the minimum degree of myopia for which a myopia control method would be prescribed between the different age ranges of practitioners’ experience (p > 0.05).
Minimum level of myopia progression that necessitates myopia controlPractitioners from Australasia and Europe reported recommending a myopia control intervention to patients with lower annual myopia progression rates (0.26–0.50 D/year) in comparison with those from the other regions (0.51–0.75 D/year for all others) (p < 0.001). Within Europe, Spanish practitioners reported recommending a myopia control intervention to patients with a higher annual myopia progression (0.51-0.75 D/year) than those from France, Italy, Portugal, Russia, Norway and the United Kingdom (all 0.26–0.50 D/year; p < 0.001); and to patients with lower annual myopia progression rates than those from Latvia (0.76-1.00D/year; p < 0.001). In Spain, no significant differences were found in the minimum level of myopia progression that necessitates myopia control with regards to the number of years of professional experience (p > 0.05).
Using undercorrection as a strategy to control myopiaSingle-vision undercorrection was reported to be an ineffective strategy to slow myopia progression by 83.5 % of all eye care practitioners who participated in this survey (Africa: 64.9 %; Asia: 82.2 %; Australasia: 99.0 %; Europe: 87.1 %; North America: 85.2 %; South America: 68.9 % and Spain: 87.4 %); 14.1 % reported having prescribed it at least once (Africa: 29.7 %; Asia: 15.6 %; Australasia: 1.0 %; Europe: 10.7 %; North America: 13.0 %; South America: 23.7 % and Spain: 10.0 %); and 2.5 % reported that they always recommend this approach (Africa: 5.4 %; Asia: 2.1 %; Australasia: 0.0 %; Europe: 2.2 %; North America: 1.8 %; South America: 7.3 % and Spain: 2.6 %). Significant differences were found between regions in the use of undercorrection as a strategy for myopia control (p < 0.001), with this method being used least in Australasia and most in Africa and South America in comparison with the other regions (p < 0.001). Significant differences were found between the different age ranges of Spanish practitioners’ experience in the prescription of undercorrection (p = 0.005); as years of practitioner's experience increased so did so undercorrection prescription frequency.
Reasons for not prescribing an alternative method to single-vision correctionNo significant differences were found in the factors that prevented the prescription of a myopia control method between Spanish practitioners and the those from the other regions (p > 0.05). Both globally and in Spain, high cost followed by insufficient information were reported as the major reasons why myopia control methods were not prescribed. Other reasons that prevent Spanish practitioners from prescribing myopia control approaches were commented upon in the free-text section of the survey and emphasised the need to provide the general public with scientific information about effective myopia control methods. Further factors that prevented practitioners from prescribing myopia control methods included concerns about patient safety, lack of perceived treatment availability and tools needed to prescribe them, and low benefit/risk ratio.
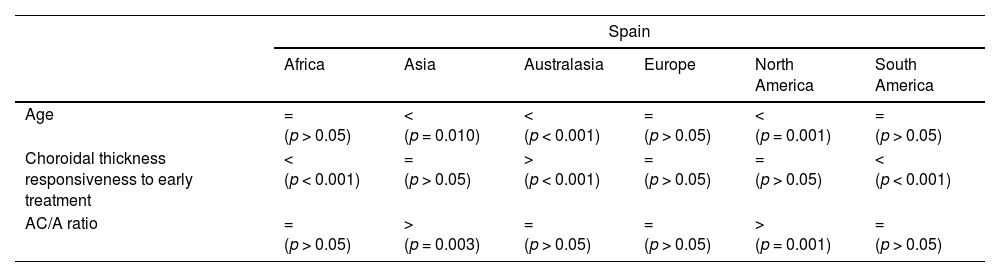
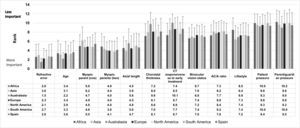
Ranked criteria for starting myopia control in a young progressing myopeOverall, as well as in Spain, the main criteria used to start adopting a method of myopia control included refractive error and age, followed by having myopic parents and axial length (Fig. 5). Significant differences were found between Spain and the other regions with regards to age (p < 0.001), choroidal thickness responsiveness to early treatment (p = 0.041) and AC/A ratio (p < 0.001) (Table 2). No significant differences were found between Spain and the other regions in the other criteria proposed for starting myopia control in a young progressing myope (p > 0.05). In Spain, no significant differences were found between years of experience and the criteria used to adopt a myopia control approach (p > 0.05).
Statistical differences in the ranked criteria for starting myopia control in young progressing myopes between Spain and the other regions. = Similar ranked criteria; >, Spanish practitioners reported significantly higher ranked criteria; <, Spanish practitioners reported significantly lower ranked criteria.
Worldwide, 75.5 % of all the eye care practitioners considered age as the primary reason to adopt a myopia control approach. Significant differences were found in the factors considered when choosing which myopia management strategy to use first between Spanish practitioners and the world's mean (p = 0.048). Whereas in Spain the main factors were age, refractive error (non-cycloplegic) and parent/guardian preference, globally they were age, refractive error (non-cycloplegic) and cycloplegic refraction. Other reasons that also influenced decision-making for choosing which myopia management strategy to use first in Spain were axial length, patient preference and binocular vision.
Frequency of myopia control follow-ups in myopic childrenSpanish practitioners (5.3 ± 2.7 months [CI 4.8 – 5.8]) recommend follow-up appointments over a longer period of time compared to the world's mean (4.6 ± 4.0 months [CI: 4.4 – 4.8]) (p < 0.001). There were differences in such recommendation between regions: Africa = 5.7 ± 2.6 months (CI: 4.9–6.5); Asia = 4.3 ± 4.5 months (CI: 4.0 – 4.5); Australasia = 5.4 ± 1.3 (CI: 5.0 – 5.7); and Europe = 5.5 ± 2.0 (CI: 5.3 – 5.7) (p < 0.001). In Spain, no significant differences were found between the different age ranges of practitioners’ experience and the frequency of myopia control follow-up appointments (p > 0.05).
Triggers to adjust myopia management strategyOf all the eye care practitioners who participated in this survey, 84.4 % reported that progression of refractive error was the main reason for changing the myopia control method prescribed, followed by progression of axial length (60.6 %) and poor compliance (55.0 %). No significant differences were found in the reasons for selecting another myopia control method between Spanish practitioners and those from the other regions (p > 0.05).
Impact of myopia management on your practiceGlobally, 26.2 % of eye care practitioners believe that as a result of embracing myopia management in practice patient loyalty has not changed; 45.4 % reported that it has improved; and 23.8 % felt it has improved considerably. However, 3.9 % and 0.8 % reported it is lower or much lower than before offering myopia management, respectively. In terms of practice revenue, 39.2 % reported embracing myopia management does not affect practice revenue; 39.2 % that it has improved; and 10.7 % that it has improved considerably. However, 9.3 % and 2.6 % reported it is lower or much lower than before offering myopia management, respectively. Regarding job satisfaction, 20.2 % of the participants reported that embracing myopia management does not affect job satisfaction; 44.3 % that it has improved; and 31.9 % that it has improved substantially. On the other hand, 2.9 % and 0.8 % reported it is lower or much lower than before offering myopia management, respectively. Significant differences were found between Spanish practitioners and those from the other regions with regard to patient loyalty, practice revenue and job satisfaction, with Spanish practitioners reporting that embracing myopia management in practice has a lower impact on customer loyalty, practice revenue and job satisfaction compared with the other regions (all p < 0.001) (Fig. 6). No significant differences were found between reported years of practitioner experience and the reported perception of embracing myopia management on customer loyalty, practice revenue and job satisfaction.
DiscussionThis study reports on a survey conducted in 2022 that assessed trends in myopia management attitudes and strategies in clinical practice found specifically in Spain and compares these findings against global trends in myopia management. Furthermore, this study also provides an update of the same survey that was carried out in 2019 allowing an assessment as to how these trends might have changed over time.7 As was found in the 2019 survey, most participants in this study were optometrists, which was expected given that the survey was disseminated by email by the Spanish General Council of the Colleges of Opticians-Optometrists to all registered optician-optometrists in the country.
The self-reported level of concern about the increasing frequency of pediatric myopia was generally high across all six continents. That Spanish practitioners were less concerned than Asian practitioners, but showed similar level of concern as other regions assessed is attributed to the high prevalence rate of pediatric myopia in Asia,1,2 thus practitioners in this part of the world typically show the greatest level of concern compared with all other continents in this and previous reports.2,4,5,7 Although in the 2015 and 2019 surveys orthokeratology was considered the best myopia control method in Spain7 as well among most regions of the world,5 in the 2022 survey combined treatments were reported to be the most effective myopia control method followed by orthokeratology both in Spain and around the world; the latter might be attributed to recent studies reporting improved myopia control efficacy with atropine combined with orthokeratology in comparison with orthokeratology treatment alone.3,8 Despite considered to be the most efficacious, combination therapy was one of the least prescribed myopia control techniques across all regions, ranging from around 2 % in Africa and Spain to 5 % in Asia. The latter might be attributed to poor access to low dose atropine preparations and optometrists in many parts of the world, including Spain, not being licensed to prescribe atropine. Spanish practitioners reported a similar level of perceived clinical activity in the field of myopia control compared with practitioners worldwide both in this study as well as in the 2019 survey, indicating that the adoption of myopia management in practice appears to be similar among regions worldwide.9–11
Despite the relatively high self-reported level of concern about the increasing frequency of pediatric myopia as well as the relatively high self-perceived clinical activity in myopia control, around half of all prescribed treatments to progressive/young myopes were single-vision distance spectacles/soft contact lenses both in Spain and in most regions around the world. However, the prescription of single-vision spectacles in Spain has decreased from 49.7 % in 2019 to 32.5 % in 2022 and that of single-vision soft contact lenses from 19.1 % in 2019 to 14.8 % in 2022.7 That large numbers of eye care practitioners still do not prescribe myopia control treatments to progressive/young myopes was reported to be related to insufficient training in the field as well as the lack of specialist equipment for the appropriate prescription of these treatments.
Overall, eye care practitioners worldwide recommend prescribing myopia control treatment at an older age (8.0 ± 2.4 years) than Spanish practitioners (7.5 ± 1.0 years). Spanish, Australasian and European practitioners reported recommending a myopia control intervention to patients with lower annual myopia progression rates (0.26–0.50 D/year) than those from the other regions assessed (0.51–0.75 D/year for all others). These regional differences in the recommendation of myopia control approaches with regards to age as well as to the degree of myopia and the annual myopia progression rate might be related to the region's predominant ethnicity, with higher degrees of myopia and rates of myopia progression typically found in Asian compared to Caucasian children, practitioners’ scope of practice as well as cultural and regional preferences. Over 80 % of practitioners both globally and in Spain reported never prescribing undercorrection as a method for myopia control in 2022; this figure is up compared to the results of the 2019 survey (i.e., globally: 78 %; Spain: 69 %). The reduced use of undercorrection as a method for myopia control is attributed to the well-established evidence showing that single-vision distance undercorrection is ineffective in reducing myopia progression in children.12
The main reasons why eye care practitioners do not adopt myopia control methods, including high cost followed by inadequate information, appear to be the remarkably similar in 2022 compared to 2019;7 this highlights the importance to increase accessibility, both financially and geographically, through collaborative efforts between practitioners and the eye care industry.13 Another of the main reasons for not prescribing a myopia control method was reported to be insufficient dissemination of information regarding effective myopia control methods to potential patients. The Spanish General Council of the Colleges of Opticians-Optometrists is conducting campaigns on the importance of reducing myopia progression through the use of effective methods that are expected to increase the adoption of myopia control methods by Spanish practitioners.14–16
Overall, as well as in Spain, the criteria used to start adopting a myopia control method included refractive error and age, followed by having myopic parents and axial length. Likewise, Spanish as well as practitioners from most parts of the world, recommend follow-up appointments within 6 months. Similarly, progression of refractive error was the main reason for changing the myopia control method employed, followed by progression of axial length and the availability of new methods with better reported efficacy. Such consistency in the criteria used between practitioners from different regions is attributed to evidence and guidelines in myopia management supporting these criteria.13,17
Embracing myopia control in clinical practice was reported to increase patient loyalty and enhance job satisfaction by practitioners from the different regions assessed, whereas practice revenue showed more mixed results. These findings might not be surprising as pursuing myopia management has potential benefits for all stakeholders concerned, particularly eye care practitioners, patients and the eye care industry.
In conclusion, this global survey of current trends in eye care practitioner myopia management attitudes and strategies in clinical practice has identified that both the level of concern about increasing frequency of pediatric myopia and perceived clinical activity in myopia control was generally high both in Spain and globally. However, despite this relatively high level of concern and self-perceived clinical activity in myopia control, around half of all prescribed treatments to progressive/young myopes were single-vision distance spectacles and single-vision distance soft contact lenses both in Spain and in most regions around the world. Combined treatments are now considered to be the most effective therapy followed by orthokeratology, albeit the former is still one of the least prescribed myopia control techniques across all regions, including Spain as optometrists in this country are not licensed to prescribe drugs. The main reasons why eye care practitioners, both globally and in Spain, do not adopt myopia control methods are high cost followed by insufficient information. Overall, as well as in Spain, the criteria used to start adopting a method of myopia control included refractive error and age, followed by having myopic parents and axial length. Embracing myopia control in clinical practice was reported to increase patient loyalty and enhance job satisfaction by practitioners from the different regions assessed. These results highlight that the adoption of myopia control strategies in clinical practice is likely to have clinical, professional, regulatory, public health, and economic implications for patients, eye care practitioners, academics, manufacturers, regulatory and professional bodies, and other stakeholders concerned, including the general public. Being trained to prescribe myopia control treatments to patients increases clinical skills and professionalism, ultimately leading to better standards of care and increased job satisfaction for eye care practitioners and improved treatment outcomes and quality of life for patients. However, to be able to offer patients on-label treatments specifically approved for myopia control requires efforts from manufactures and regulatory bodies to bring such treatments to market.18 As insufficient training is among the common reasons preventing practitioners the prescription of a myopia control approach, a wider adoption of myopia control strategies in clinical practice requires ongoing efforts from academics and professional bodies in providing continuing education in the field.19 Finally, embracing myopia control is also likely to have public health and economic implications both for eye care practitioners and society due to increased practice revenue through increased patient loyalty as well as through a reduction in both the incidence and severity of suffering myopia-related ocular pathology later in life that potentially leads to reduced ocular health expenditure.2
The authors thank the Spanish General Council of the Colleges of Opticians-Optometrists for disseminating the survey to Spanish practitioners, and to CooperVision Iberia and Menicon Iberia for also doing so through their data bases. The survey was facilitated by the International Myopia Institute and supported by the World Council of Optometry.