To compare refractive-error quality of life, and spherical aberration in pseudophakic eyes with an aspherical intraocular lens (AcrySof IQ) vs. a conventional spherical intraocular lens (AcrySof Single-Piece).
Methods65 patients were randomized to implantation of either an aspherical IOL (Alcon AcrySof IQ) (30 eyes) or a spherical IOL (Alcon AcrySof Single-Piece (35 eyes). Three months postoperatively, complete ophthalmologic examinations including uncorrected visual acuity (UCVA), best spectacle-corrected visual acuity (BCVA), and a wavefront analysis were performed. Patients completed the National Eye Institute Refractive Error Quality of life Instrument (NEI RQL) to evaluate vision-related quality of life.
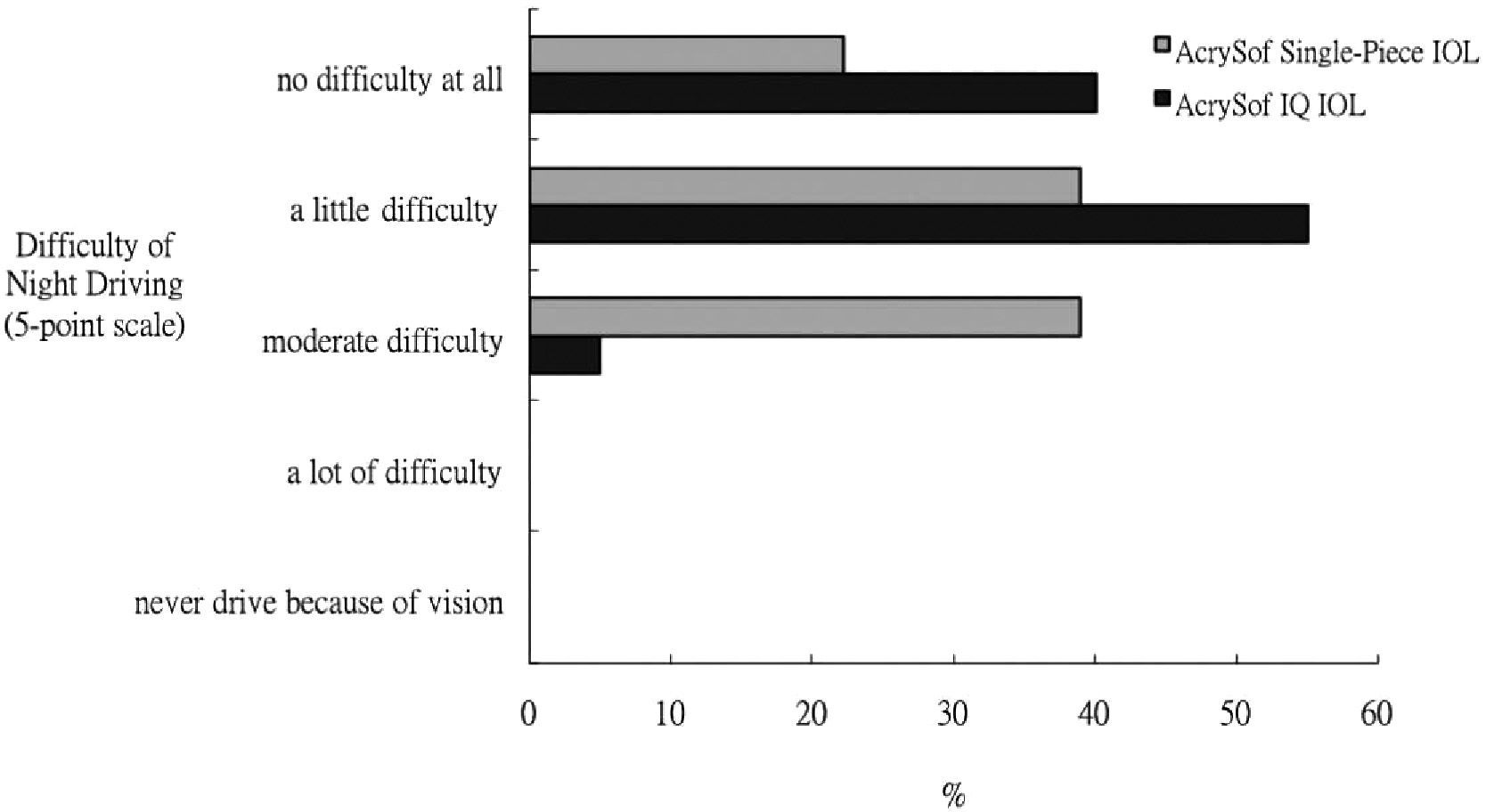
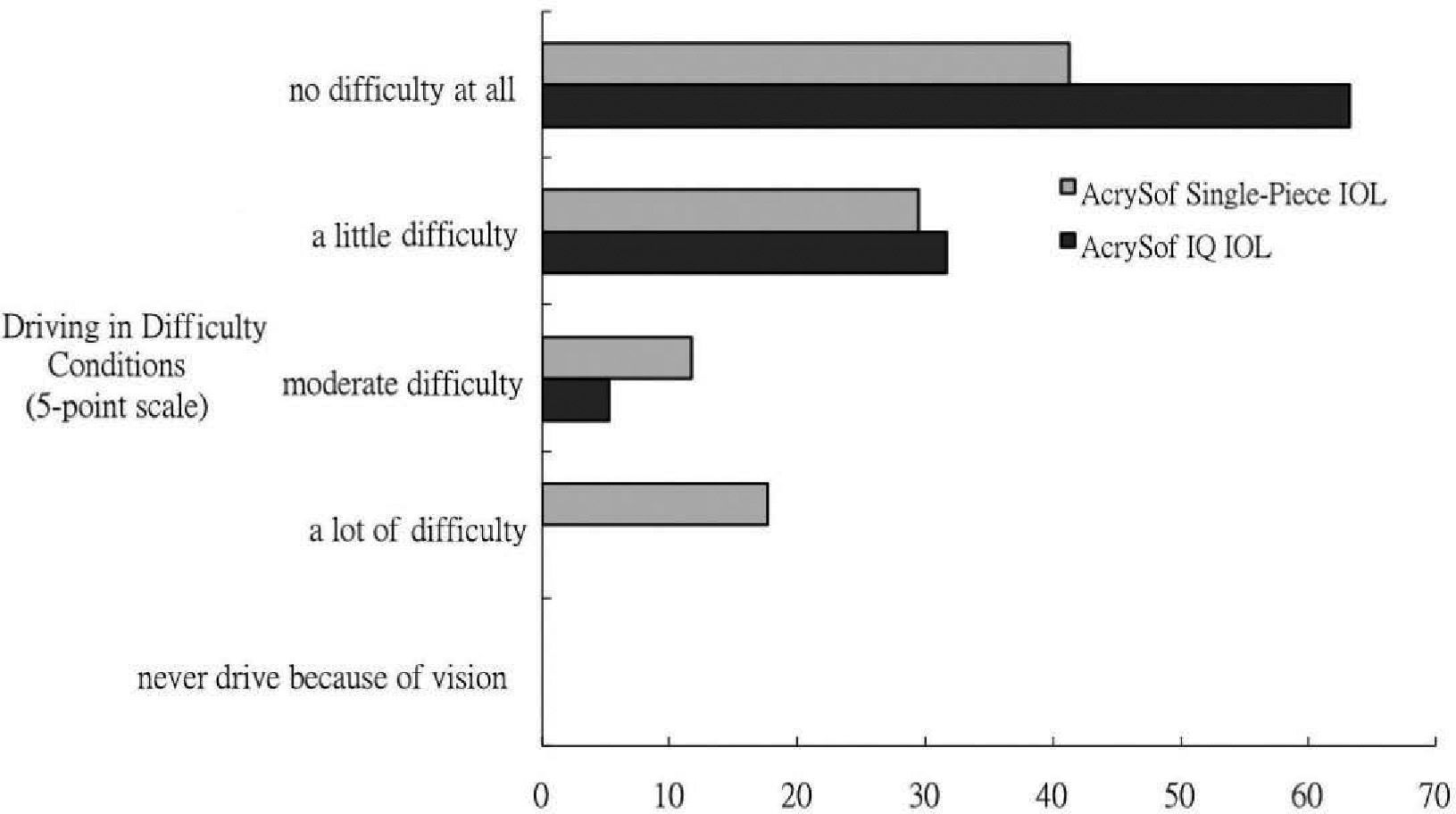
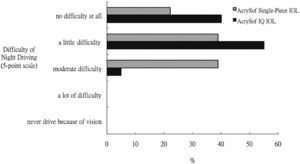
ResultsThe mean postoperative best-corrected visual acuity was 0.09±0.07 logMAR in the aspherical group and 0.12±0.08 in the spherical group, and the difference was not statistically significant. Spherical aberrations were significantly lower in the aspherical group (0.12±0.23μm), than in the spherical group (0.33±0.20μm) (P=0.001). Patients with aspherical AcrySof IQ IOLs implantation also experienced less difficulties driving at night (P=0.04), but the difference was not significant after Bonferroni correction.
ConclusionThe NEI RQL instrument is sensitive enough to detect the visual benefit of cataract surgery. The aspherical AcrySof IQ IOL reduces both spherical aberration and total higher-order aberrations, compared with the performance achieved by the spherical AcrySof Single-Piece IOL. Although the difference between the two IOLs is not statistically significant, there is a tendency toward the association of objective optical performance of aspherical AcrySof IQ IOLs with a subjective improvement in patients’ night driving.
Comparar la calidad de vida relacionada con el error refractivo y la aberración esférica en ojos pseudofáquicos a los que se les implanta una lente intraocular asférica (Acrysof IQ) con aquellos a los que se les implanta una lente intraocular convencional esférica (Acrysof Single-Piece).
MétodosA 65 pacientes se les implantó una lente intraocular (LIO); a 30 de ellos se les asignó de manera aleatoria una LIO asférica (Alcon Acrysof IQ) y a los 35 restantes una LIO esférica (Alcon Acrysof Single-Piece). Transcurridos tres meses de la intervención, se realizó una revisión oftalmológica completa, que incluía la medida de la agudeza visual sin corrección (AVsc), de la agudeza visual con la mejor corrección (AVcc) y el análisis del frente de onda. Los pacientes completaron el cuestionario NEI-RQL (siglas de “Calidad de vida relacionada con el error refractivo, del National Eye Institute de EE.UU.”) para evaluar su calidad de vida en lo que respecta a visión.
ResultadosLa AVcc postoperativa fue 0,09±0,07 logMAR (media ± desviación típica) en el grupo de pacientes con LIO asférica y 0,12±0,08 en el grupo de pacientes con LIO esférica, pero la diferencia entre ambos grupos no resultó ser estadísticamente significativa. Sin embargo, la aberración esférica fue significativamente menor en el grupo de la LIO asférica (0,12±0,23μm) que en el de la LIO esférica (0,33±0,20μm) (P=0,001). Asimismo, aquellos pacientes a los que se les implantó la LIO asférica Acrysof IQ también tuvieron menos problemas de conducción nocturna (P=0,04), aunque esta diferencia no resultó ser significativa tras aplicar una corrección de Bonferroni.
ConclusionesEl cuestionario NEI-RQL es suficientemente sensible para detectar los beneficios visuales de la cirugía de cataratas. La LIO asférica Acrysof IQ hace que disminuya tanto la aberración esférica como las aberraciones totales de alto orden, en comparación con los resultados obtenidos con la LIO esférica Acrysof Single- Piece. A pesar de que la diferencia entre ambas LIO no es estadísticamente significativa, sí que parece que hay una tendencia para que la mejora de la calidad óptica que se logra con la LIO asférica Acrysof IQ se traduzca en una mejora de la conducción nocturna de los pacientes.
The improvement of cataract-extraction techniques and the development of better materials and designs of intraocular lens (IOLs) have resulted in a better quality of vision and less complications. However, patients often complain about glare and halos symptoms after surgery. With the introduction of wavefront analysis, patients having conventional spherical IOLs showed a large amount of positive spherical aberration postoperatively.1 Based on these observations, aspherical IOLs were recently designed to optimize image quality, by compensating the positive spherical aberration. Reduced spherical aberration and an improved contrast sensitivity were demonstrated in a series of clinical trials comparing the aspherical IOL with a variety of conventional spherical IOLs.2-5 However, it remains unclear the degree to which the observed improvements in the results of selected tests translates into improvements in subjective visual function after implantation of the aspherical IOL.
The 42–item Refractive Error Quality of Life (RQL) questionnaire, created by the National Eye Institute, has been specifically designed to assess the subjective visual and functional effects of refractive error and its correction, either with contact lenses, eyeglasses, or surgery. The NEI-RQL is accurate and sensitive enough to provide information about patient status that is not reflected by traditional clinical ophthalmic measures.6,7 It also measures the severity and the frequency of glare and halo symptoms, and the difficulties when driving at night or in complicated conditions. Since recent studies indicated that reduced spherical aberration results in an improvement of glare and halo symptoms,8,9 the NEI-RQL enables us to detect the relevant differences between the spherical and aspherical IOLs.
This randomized prospective study is to compare the vision-related quality of life (using NEI- RQL), spherical aberration, and visual acuity in eyes implanted with one of these two acrylic IOLs: an aspherical IOL (AcrySof IQ SN60WF) and a spherical IOL (AcrySof Single-Piece SA60AT).
Material and MethodsWe conducted a prospective randomized parallel-groups study to compare an aspherical IOL (AcrySof IQ, Alcon Laboratories, Ft. Worth, TX, U.S.A.) with a spherical IOL (AcrySof Single-Piece, Alcon Laboratories, Ft. Worth, TX, U.S.A.). The two selected lenses are similar in some aspects and differ in others (Table 1).This study was carried out at the National Taiwan University Hospital between September 2006, and March 2007. All the recruited subjects received an explanation of the research protocol, after which they provided written informed consent. The study was approved by the hospital's Ethical Committee and followed the tenets of the Declaration of Helsinki.
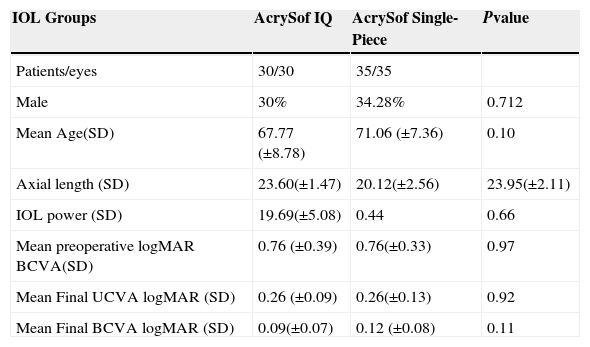
Demographics of the subjects in the study
| IOL Groups | AcrySof IQ | AcrySof Single-Piece | Pvalue |
| Patients/eyes | 30/30 | 35/35 | |
| Male | 30% | 34.28% | 0.712 |
| Mean Age(SD) | 67.77 (±8.78) | 71.06 (±7.36) | 0.10 |
| Axial length (SD) | 23.60(±1.47) | 20.12(±2.56) | 23.95(±2.11) |
| IOL power (SD) | 19.69(±5.08) | 0.44 | 0.66 |
| Mean preoperative logMAR BCVA(SD) | 0.76 (±0.39) | 0.76(±0.33) | 0.97 |
| Mean Final UCVA logMAR (SD) | 0.26 (±0.09) | 0.26(±0.13) | 0.92 |
| Mean Final BCVA logMAR (SD) | 0.09(±0.07) | 0.12 (±0.08) | 0.11 |
BCVA: best-spectacle corrected visual acuity; IOL: intraocular lens; SD: standard deviation.
Inclusion criteria for this study were the presence of cataract in both eyes, age between 50 and 80 years, a corneal astigmatism below 2.0 diopters, and a VA, as measured with the potential acuity meter (PAM), better than 0.2 logMAR units. Exclusion criteria were: complicated cataract, corneal opacities or irregularities, dry eye, amblyopia, anisometropia, surgical complications, IOL tilt or decentration, coexisting ocular pathologies, glaucoma, nondilating pupil, history of intraocular surgery, laser therapy, retinopathy, optic nerve or macular diseases, refusal or unable to maintain follow-up, and posterior capsule opacification. Eyes with intraoperative complications such as posterior capsule tear, vitreous loss, zonular dialysis, or uveal manipulation were also excluded.
The patients were examined preoperatively as well as 1 day, 1 week, 1 month, and 3 months after surgery. At each visit we performed a thorough ophthalmologic examination that included uncorrected visual acuity (UCVA), best spectacle-corrected visual acuity (BCVA), early treatment diabetic retinopathy study (ETDRS) chart, biomicroscopy, autorefractor measurements (KR 7100P, Topcon, Tokyo, Japan), applanation tonometry; and fundus examination. Preoperatively, all the patients underwent an applanation A-scan ultrasonographic axial-length measurement (Sonomed Ultrasound A-1500, NY, U.S.A.) and the calculations were made using the SRK/T formula. IOL centration was also evaluated postoperatively using retroillumination. Wavefront analysis was performed only at the 3-month postoperative visit with a Hartmann-Shack sensor (Zywave, Bausch & Lomb Surgical, Rochester, NY, U.S.A.). The wavefront maps were analyzed using a 6mm pupil diameter and a Zernike polynomial expansion up to the sixth-order of Zernike coefficients.
Patients were randomly divided into two groups (using a simple 1:1 randomization ratio scheme) to have unilateral IOL implantation. All eyes had standardized phacoemulsification by the same surgeon (IJW). Surgery consisted of topical anesthesia, three-step clear corneal incision (2.75mm) at 180 degrees (temporal for right eyes and nasal for left eyes) and stop-chop technique, a 5.0mm continuous curvilinear capsulorrhexis, phacoemulsification cataract extraction, IOL implantation with an injector, IOL centration, and a sutureless incision.
The NEI-RQL Instrument was used to assess vision-related quality of life before and 3 months after cataract surgery. In general, questionnaires were completed without assistance; however, further explanations of particular questions were given by the study personnel if requested by the patient.
The NEI RQL instrument contained 42 questions, where each question belongs to one of 13 subscales. The subscales included: clarity of vision, expectations, near vision, far vision, diurnal fluctuations, activity limitations, glare, symptoms, dependence on corrections, worry, suboptimal corrections, and satisfaction with correction. The answer was converted into a 100-point scale, where higher scores indicate a higher self-reported quality of life (e.g., a higher “worry”-score to represent a better outcome, or less worry). Each subscale consists of one or more questions and, therefore, we calculated each subscale's score using the average of those questions specific to that subscale.6
Data and AnalysisFor the statistical analysis of visual acuity data, the logarithm of the minimal angle of resolution (LogMAR) was used as relevant unit. All data were given in the form: mean ±SD. Wavefront aberration data were recorded for a 6.00mm pupil. Statistical analysis was performed by means of Student's t test (for variance analysis) and using Z test (for the analysis of proportions).
For vision-related quality-of-life results, we used 2-tailed 2-sample t tests to compare the subscale scores regarding clarity of vision, far vision, diurnal fluctuations, activity limitations, glare, symptoms, worry, and satisfaction with correction. In each group, we used 2–tailed paired t tests to test for the significance of the mean change from baseline to the second assessment (difference from zero). As multiple comparisons were performed, we used the Bonferroni method to adjust the probability's level of significance. Nominal P values were considered to be significant when they were below 0.00625, in order to maintain an overall type I error equal to 0.05. To better represent the magnitude of change on each scale, the mean change was converted into a standardized effect size by dividing the mean change within each scale by the observed baseline's standard deviation of scores on each scale for the pooled study sample.10
ResultsOf the 74 eyes included in the study, 9 had to be excluded because of intraoperaitve capsule rupture (1eye), cystoid macular edema (1 eye), retinal detachment (1 eye), and loss of follow-up (6 eyes). This resulted in 65 patients being left in the study: 30 with an AcrySof IQ IOL and 35 with an AcrySof Single-Piece IOL. The drop-out rate was 12.16% (9 out of 74 patients). There were no significant differences between the groups in terms of age, gender, axial length, IOL power, mean preoperative BCVA, or mean postoperative BCVA and UCVA. All eyes in both groups had a mean postoperative BCVA of 20/32 or better. The demographics of the patients/ eyes included in the study are summarized in table 1.
At the study visit, which took place 3 months after surgery, in every implanted eye the posterior capsule could be appreciated against the IOL's optic and without any folds. No cases of posterior capsule opacification were noted.
The 3-month postoperative BCVA was similar in both groups; there was no difference in terms of BCVA between the AcrySof IQ IOL group (BCVA= 0.09±0.07) and the AcrySof Single-Piece IOL group (BCVA= 0.12±0.08) (P=0.11).Before the surgical intervention, wavefront aberrations could be measured in only 8 out of 65 subjects, mainly due to the interference of the cataract with the measurements. Therefore, we did not include the preoperative wavefront analysis in our study. The postoperative root-mean square (RMS) values associated to the total higher-order aberrations (HOAs), calculated for a 6.0mm pupil, were lower in the aspherical-IOL group (0.51±0.45 μm) than in the spherical- IOL group (0.77±0.36μm) (P=0.02). Particularly, further analysis using a Zernike polynomial expansion showed that the spherical aberration term (Z40) was significantly lower in the aspherical-IOL group (0.12±0.23 μm) than in the spherical-IOL one (0.33±0.20μm) (P=0.001).
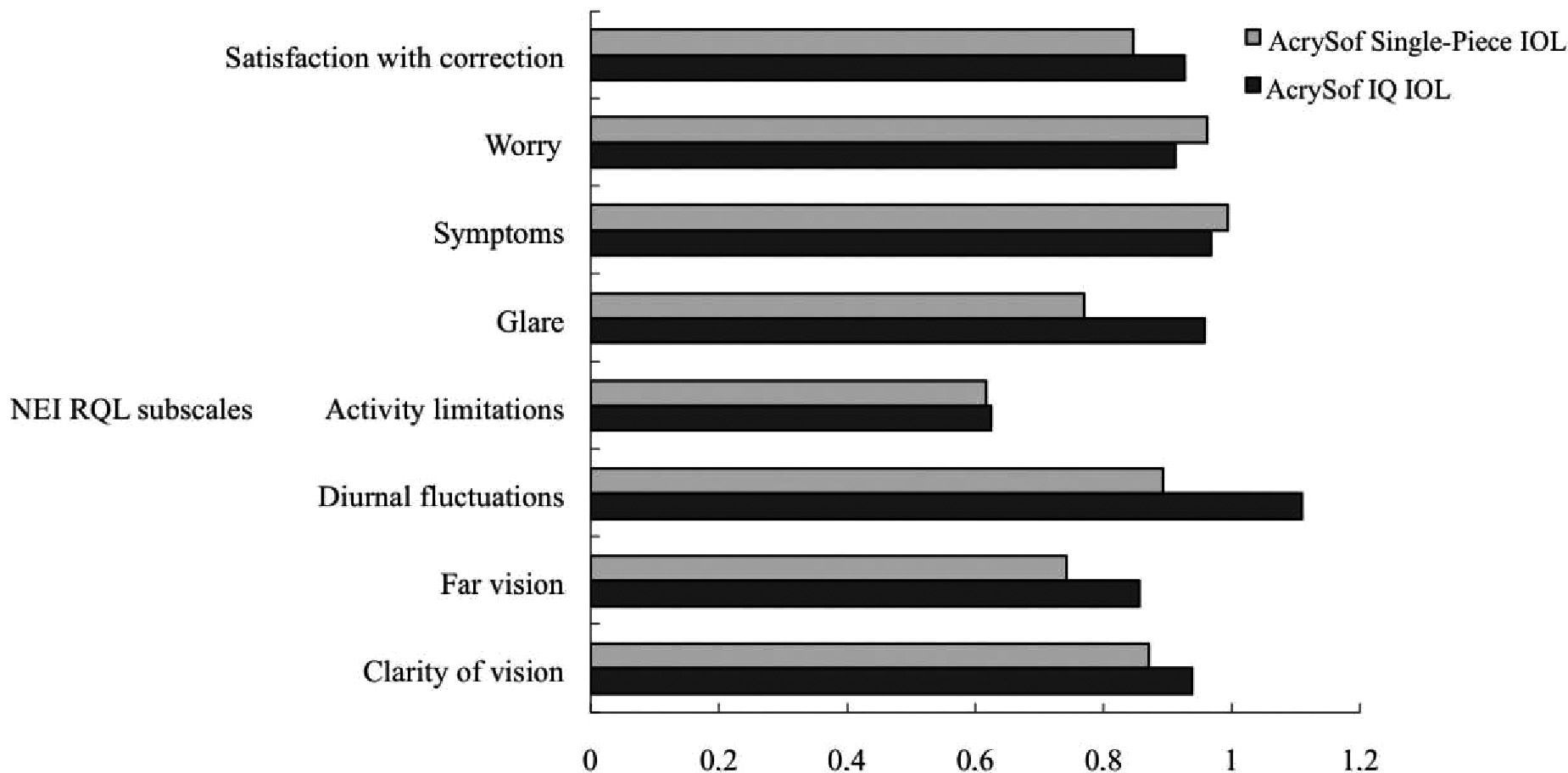
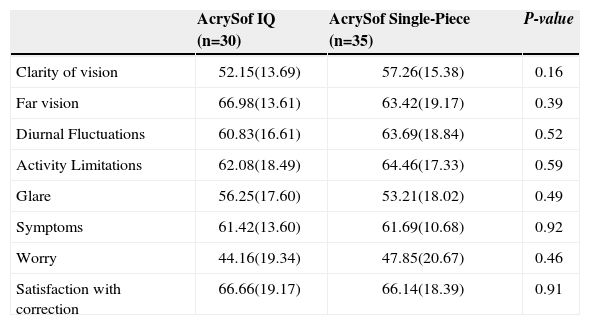
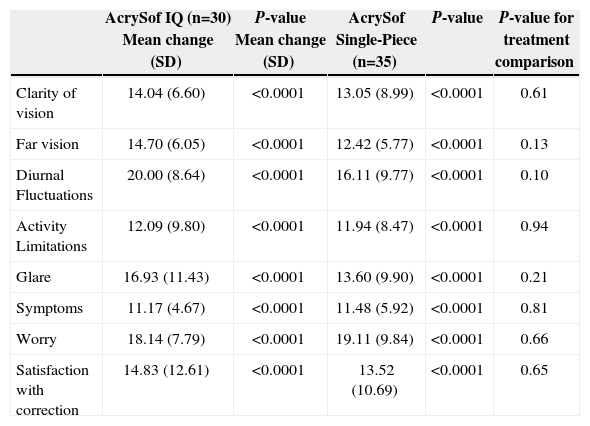
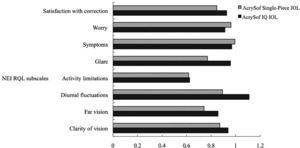
Baseline NEI RQL scores are presented in table 2, which shows that there were no significant differences between the two groups. Table 3 summarizes the changes in NEI RQL score between the two groups. Again, there were no significant differences between the two groups neither overall nor at a subscale level. All the scales showed an statistically significant improvement for both groups. For all the scales, the impact of the mean changes could be observed, as they were converted into standardized effect sizes (Figure 1). According to commonly used guidelines, an effect size of 0.8 or greater is considered to be “important”, 0.5 indicates “moderate”, and 0.2 means “small”.10 Both groups showed an important improvement on the majority of scales. The improvements on diurnal fluctuations and glare were slightly higher for the aspherical IOL group.
Baseline mean scores (SD in parentheses) of two treatment groups
| AcrySof IQ (n=30) | AcrySof Single-Piece (n=35) | P-value | |
| Clarity of vision | 52.15(13.69) | 57.26(15.38) | 0.16 |
| Far vision | 66.98(13.61) | 63.42(19.17) | 0.39 |
| Diurnal Fluctuations | 60.83(16.61) | 63.69(18.84) | 0.52 |
| Activity Limitations | 62.08(18.49) | 64.46(17.33) | 0.59 |
| Glare | 56.25(17.60) | 53.21(18.02) | 0.49 |
| Symptoms | 61.42(13.60) | 61.69(10.68) | 0.92 |
| Worry | 44.16(19.34) | 47.85(20.67) | 0.46 |
| Satisfaction with correction | 66.66(19.17) | 66.14(18.39) | 0.91 |
Mean change on RQL-42 questionnaires from baseline to the second assessment (positive values indicate improvement)
| AcrySof IQ (n=30) Mean change (SD) | P-value Mean change (SD) | AcrySof Single-Piece (n=35) | P-value | P-value for treatment comparison | |
| Clarity of vision | 14.04 (6.60) | <0.0001 | 13.05 (8.99) | <0.0001 | 0.61 |
| Far vision | 14.70 (6.05) | <0.0001 | 12.42 (5.77) | <0.0001 | 0.13 |
| Diurnal Fluctuations | 20.00 (8.64) | <0.0001 | 16.11 (9.77) | <0.0001 | 0.10 |
| Activity Limitations | 12.09 (9.80) | <0.0001 | 11.94 (8.47) | <0.0001 | 0.94 |
| Glare | 16.93 (11.43) | <0.0001 | 13.60 (9.90) | <0.0001 | 0.21 |
| Symptoms | 11.17 (4.67) | <0.0001 | 11.48 (5.92) | <0.0001 | 0.81 |
| Worry | 18.14 (7.79) | <0.0001 | 19.11 (9.84) | <0.0001 | 0.66 |
| Satisfaction with correction | 14.83 (12.61) | <0.0001 | 13.52 (10.69) | <0.0001 | 0.65 |
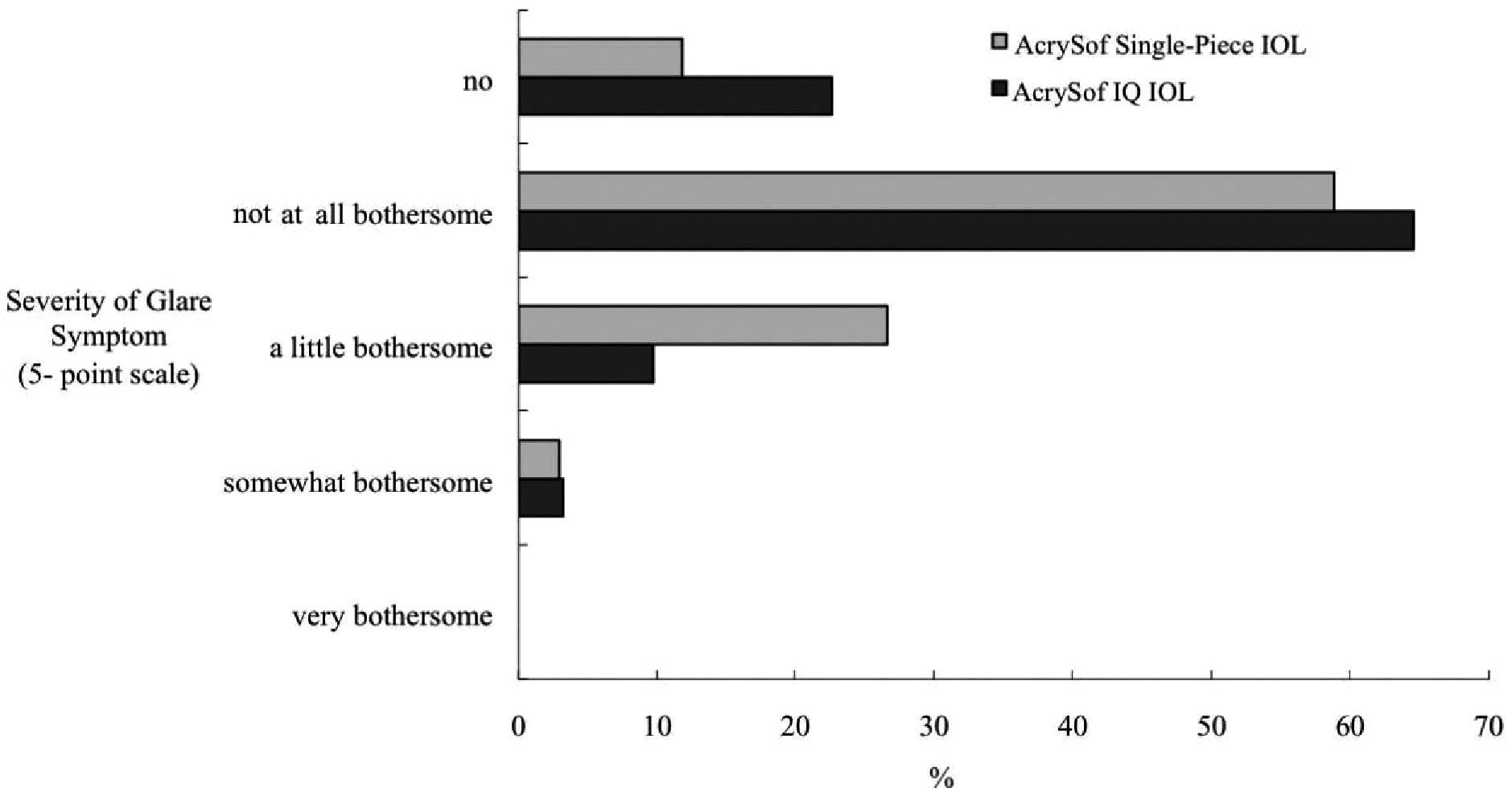
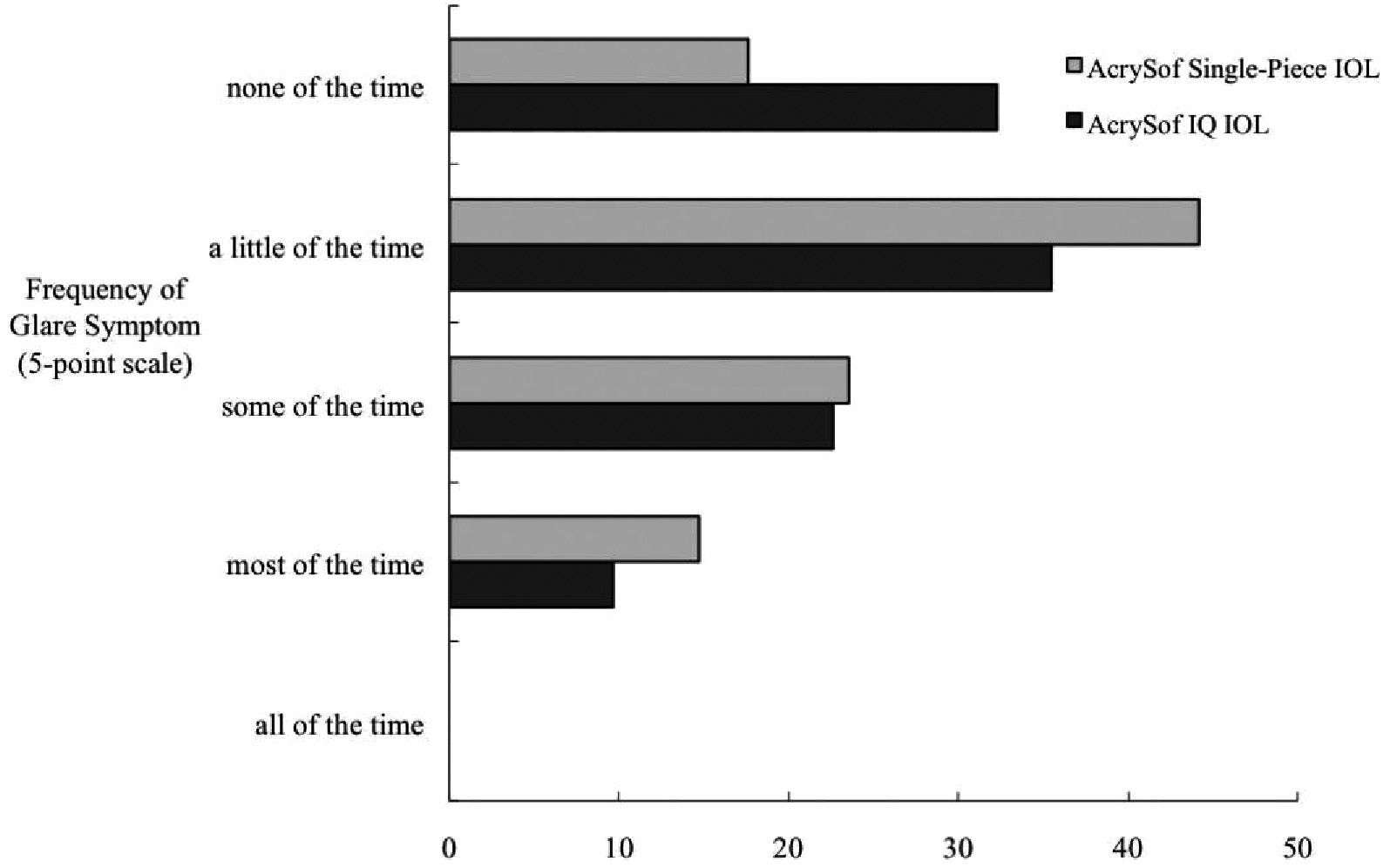
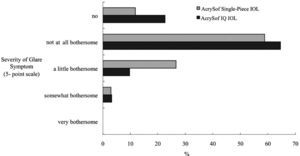
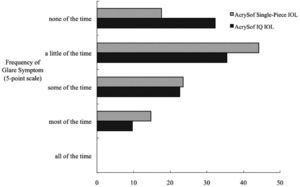
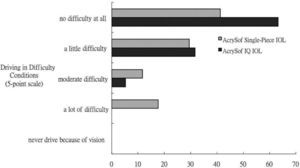
Although similar improvements were observed in both groups, we performed treatment comparison on items 17, 38, 9, and 10 to ascertain whether there was any difference between the two lens types in terms of glare symptoms, difficulty driving at night, and difficulty driving in complicated conditions (bad weather, heavy traffic, etc.). As shown in Figures 2 and 3, for the items that focus upon the severity and frequency of glare symptoms (items 17 and 38), there were no statistical differences between the two lens types (P=0.25 and P=0.58, respectively). For the item on the difficulties experienced driving at night, there was significant statistical difference between the two lens types (P=0.04) (Figure 4). If we adjusted for the effects of multiple testing, the differences would not have been statistically significant. The difference for the item on the difficulties of driving in complicated conditions was not significant (P=0.2) as seen in figure 5.
Our study is the first prospectively randomized and controlled trial using the NEI RQL instrument to compare an aspherical IOL with a spherical IOL. Although the statistical difference between the two IOLs is not significant, there is a tendency toward the idea that AcrySof IQ IOL's objective optical performance is associated with a subjective improvement in patients’ night driving.
A previous study had shown that a large proportion of people who underwent cataract surgery had experienced difficulties at night driving, even 5 years after surgery.11 Night-driving problems have been a common complaint among those patients who have night-vision symptoms.12,13 Those symptoms, such as halo and glare, have been reported to be associated with the amount of high-order aberrations. 8,9,14 Although our study and previous studies3,5 have proved that the root mean square (RMS) of spherical aberration and the RMS of total higher-order aberrations (HOAs) were lower when implanting a aspherical IOL than when using the spherical IOL, it was not clear whether patients with aspherical IOLs have better subjective vision, especially as far as night vision is concerned.
Denoyer et al.,15 who used the Activities of Daily Vision Scale (ADVS), found that the patients with the Tecnis Z9000 IOLs (aspherical) showed a better subjective quality of distance vision than those patients with the spherical CeeOn Edge 911 IOLs. However, the differences between the two groups in terms of driving scores and glare-disability scores were not significant. Although the distance-vision subscale had items asking about “difficulty going down steps at night” and “difficulty reading the street signs at night” which were believed to be associated with spherical aberration, the authors didn’t indicate whether or not there was any difference on these items between the two IOL groups. The Moorfields IOL Study Group,16 who used the Visual Function-14 (VF-14) and additional questionnaires evaluating the severity and frequency of dysphotopsia symptoms, compared the vision-related quality of life results yielded by the Tecnis Z9000 IOLs (aspherical) and by the AcrySof MA60AC IOLs (spherical). No significant difference was obtained between the two groups. Although we didn’t find a significant difference between the two groups, there is a slightly greater improvement on most aspects of quality of life in the aspherical IQ IOL group. In addition, those patients in the AcrySof IQ IOL group also had less difficulties when driving at night.
The average pupil diameters in mesopic conditions was larger for the participants in Denoyer et al's study15 than for those taking part in Moorfields IOL Study Group's study,16 but we don’t know whether or not a larger pupil diameter resulted in a more significant visual benefit. In addition, our study showed that the patients with AcrySof IQ IOL had slightly less difficulty driving at night. We need more sensitive tests to be able to detect the differences between the two types of IOLs regarding night driving activities and glare and halo symptoms. Further clinical studies should be preformed to assess these aspects.
Reduced contrast sensitivity has been reported to be associated with a cessation of night driving.17 Fremman et al. also demonstrated that contrast sensitivity is associated with the night-driving-difficulty subscale in glaucoma patients.18 Although we didn’t measure the subjects’ contrast sensitivity, there is a growing evidence that eyes with aspherical IOLs have a better contrast sensitivity than those with spherical IOLs, especially in mesopic conditions.3,5,15 Thus, these studies may explain why our patients with aspherical IOLs had less difficulty driving at night.
The Visual Function-14(VF-14), the National Eye Institute Visual Functioning Questionnaire (NEI VFQ-25) and the ADVS have been used in the past to assess the benefit of cataract surgery.20-22 The NEI RQL instrument has been used to evaluate the change in vision-related quality of life of keratorefractive surgery patients,7 while our study is the first one to use it as a tool to evaluate the difference between these two IOLs. We chose this particular questionnaire since it had more items on glare symptoms and night driving, which are associated with the impact of spherical aberration on the patient's quality of life. Our study has also proved that most of the scales in the NEI RQL instrument were sensitive enough to detect the benefit of cataract surgery.
One limitation of our study is that we could not detect subtle decentration of the IOL and we didn’t measure its tilt angle. Changes in IOL position, such as optic tilt and decentration, can influence the optical performance of IOLs.23,24 Altmann et al had shown that even a minimal IOL decentration (0.3mm) is sufficient to negate the theoretical optical advantages of an aspherical IOL.25 On the contrary, Tabernero et al had indicated that the tolerances to IOL tilt and decentration were large enough to obtain an optical benefit from an aspherically designed IOL within the limits imposed by modern cataract surgery.26 We believed centration of the IOL may play a role in these vision-related symptoms; that is why we had excluded very strong IOL tilt and decentration cases to minimize the impact of these effects on our results.
In conclusion, cataract surgery improves patients’ quality of life, and the NEI RQL instrument is sensitive enough to detect the visual benefit of surgery. The AcrySof IQ IOL reduces spherical aberrations and total HOAs. Although the difference between the two IOLs is not statistically significant, there is a tendency toward the AcrySof IQ IOL's objective optical performance to be associated with a subjective improvement in patients’ night driving.