The aim of this study was to measure the reading eye movements in subjects with traumatic brain injury (TBI) using ReadAlyzer. ReadAlyzer is an objective eye movement recording device that tracks the eye movements while reading.
MethodsReading eye movements were measured using ReadAlyzer in 30 subjects with TBI (mild, moderate and severe) who had binocular vision and reading related symptoms and 60 asymptomatic controls.
ResultsThere was a significant decrease in reading eye movement parameters in subjects with TBI compared to controls. Reading eye movement parameters are represented in median and interquartile range (IQR). Subjects with TBI presented with an increased number of fixations/100 words (median 137, IQR 106–159) and regressions/100 words (24, 12–36), and reduced reading rate (154, 128–173) words per minute. They also had a lesser grade level equivalent (4.0, 3.0–7.0) and reduced comprehension (70, 60–80) percentage compared to controls (Mann–Whitney U test, p<0.05). Reading eye movement parameters were also significantly affected in mild and moderate-severe TBI subjects compared to controls (Kruskal–Wallis test, p<0.05).
ConclusionReading eye movement performance using ReadAlyzer was found to be decreased in traumatic brain injury. Reading assessment may serve as a clinical measure to understand the oculomotor system following TBI.
El objetivo de este estudio fue medir los movimientos oculares durante el proceso de lectura en sujetos con lesión cerebral traumática (TBI) utilizando ReadAlyzer, un dispositivo de registro objetivo del movimiento del ojo, que rastrea los movimientos oculares durante la lectura.
MétodosSe midieron los movimientos oculares durante la lectura utilizando ReadAlyzer en 30 sujetos con TBI (leve, moderada y grave) con síntomas relacionados con la vision binocular y la lectura, así como en 60 controles asintomáticos.
ResultadosSe produjo una disminución significativa de los parámetros del movimiento ocular durante la lectura en los sujetos con TBI, en comparación con los controles. Los parámetros del movimiento ocular durante la lectura se representan como mediana y rango intercuartílico (IQR). Los sujetos con TBI presentaron un incremento del número de fijaciones /100 palabras (137, 106–159) y regresiones/100 palabras (24, 12–36), así como una reducción de la tasa de lectura (154, 128–173) palabras por minuto. También reflejaron un menor grado de equivalencia de nivel (4, 3–7) y una reducción de la comprensión (70, 60–80) porcentual, en comparación con los controles (prueba U de Mann–Whitney, p<0,05). Los parámetros del movimiento ocular durante la lectura se vieron también significativamente afectados en los pacientes de TBI leve y moderada-severa, en comparación con los controles (prueba de Kruskal–Wallis, p<0,05).
ConclusiónSe observó un descenso del desempeño del movimiento ocular durante la lectura, utilizando ReadAlyzer, en las lesiones cerebrales traumáticas. La evaluación de la lectura puede servir como medida clínica para comprender el sistema oculomotor tras una lesión cerebral traumática.
Reading is one of the most important visual functions in daily living. The act of reading is highly complex involving an integrated function of oculomotor, sensory, cognitive, and attentional aspects.1
A normal reading is comprised of accurate, rhythmical and reflexively executed sequences of saccadic eye movements interspersed with brief fixational pauses.1,2 Reading related saccadic eye movements are 1–3 degrees in amplitude and a saccadic duration of 30–60msec.2 The presence of accurate saccadic tracking, synchronised ocular accommodation and vergence is required for efficient reading. For an adult subject with normal visual function, the expected reading rate is 250–280 words per minute with 90 fixations per 100 words and 15 regressions per 100 words.2
In traumatic brain injury (TBI), multiple brain areas and their functions are adversely affected because of the diffuse axonal injury (DAI). Physical damage to the underlying structures, such as stretching, twisting, and shearing of the neurons can result in a range of sensory, oculomotor, perceptual and structural abnormalities.1,3 Symptoms following TBI may persist from a few seconds to a few minutes after the event and usually resolve within 12 weeks but may continue for months or even years.4
Impairment of the oculomotor subsystem following TBI also adversely affect the naturalistic pattern of reading. Ninety per cent of the visually symptomatic mild TBI (mTBI) group exhibited oculomotor dysfunction (OMD) following the head trauma.3 Studies have shown that reading eye movement parameters are impaired due to head injuries. Thiagarajan et al. had investigated reading eye movements in mild TBI using Visagraph and found that the subjects had significantly reduced the reading rate and decreased grade-level efficiency.1 During reading, an individual with TBI exhibits hypometric saccades (<1-degree amplitude) and increased saccadic latencies (>200msec).2,5 Considering the extensive neural network of the oculomotor subsystems, global damage in TBI could compromise precise oculomotor control, leading to reading dysfunction and an unreceptive quality of life (QoL).1 Road traffic accidents (RTAs) represent a major burden causing TBI worldwide, and also in India.3,6–8 There is limited literature on clinically based evaluation of reading eye movement parameters with objective eye movement recordings in TBI.
The assessment of reading eye movements is highlighted in this study because eye movements are considered to be novel visual biomarkers assessing the functional integrity of the brain to predict the high-risk population from persisting with symptoms of TBI.9,10 Therefore, we present a study that has investigated the impact of TBI on reading eye movements using ReadAlyzer, an objective eye movement recording device.
Material and methodsStudy designA prospective comparative study was conducted between June 2015 and April 2016 in the Neuro-Optometry Clinic at a tertiary eye care center in India. The study adhered to the tenets of Declaration of Helsinki and the investigational procedures were reviewed and accepted by the Institutional Review Board and Medical Ethics Committee.
SubjectsThirty subjects with TBI and 60 controls were included in the study. The sample size was estimated as 30 subjects diagnosed with TBI and 60 age-matched controls considering a 1:2 ratio between the cases and the controls.11 Subjects with TBI were referred from the neuro-ophthalmology department with any one of the symptoms, such as reading difficulty, headache, eye strain or dizziness. Age-matched subjects who volunteered to participate in the study were chosen as controls. Inclusion and exclusion criteria for the cases and the controls are presented (Table 1). A duly signed, written informed consent was obtained from all the study participants. All the subjects received a comprehensive eye examination which included history taking, refraction, pupillary evaluation, extraocular motility, anterior and posterior segment examination. This was followed by neuro-optometric evaluation.
Inclusion and Exclusion Criteria for study subjects.
| Inclusion criteria | Exclusion criteria | |
|---|---|---|
| Cases | Age range: 18–60 years
|
|
| Controls | Age range: 18–60 yearsProficiency with the English languageaNormal binocular vision parametersNon-symptomatic for reading or near workStable systemic conditions (For example: Diabetes Mellitus & Hypertension under control) |
|
Neuro-optometric examination: A detailed history of the nature of injury and symptoms during the post-injury period was obtained from subjects with TBI. At the time of recruitment, they were classified into mild, moderate, and severe grades based on the Glasgow Coma Scale (GCS), post-traumatic amnesia (PTA) and loss of consciousness (LOC) reported either in the records of emergency department or hospital discharge summary or by iteratively questioning the subject, or the subject’s caretaker, about the traumatic event. GCS is a 3 to 15 point scale used to assess a patient's level of consciousness and neurologic functioning; and scoring is based on motor, verbal, and ocular responses. A score between 13 and 15 is mild, 9 to 12 is moderate and 3 to 8 is severe. PTA is the time elapsed from injury to the moment when patients can demonstrate continuous memory of what is happening around them. PTA<1 day is mild, 1–7 days is moderate and >7 days is severe. Duration of loss of consciousness is classified as mild (LOC<30min, moderate (LOC 30min to 6h), or severe (LOC>6h).12,13
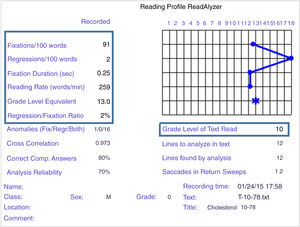
Reading eye movement assessment: Reading eye movements were assessed objectively using ReadAlyzer™ (Compevo AB, Markvardsgatan, Stockholm, Sweden). ReadAlyzer consists of infra-red emitters and detectors mounted in a safety goggle. It can determine the eye positions by sensing several infrared reflections from the cornea. The measuring speed of the instrument is 60Hz with a better angular resolution compared to Visagraph II. Head movements are automatically compensated for analysis by the ReadAlyzer software.14–16 The subject wore the eye movement goggles and the near interpupillary distance was adjusted. The test paragraphs were placed 40cm from the corneal plane or habitual correction centred along the subject’s midline.
Eye movements were recorded for the cases and controls while the subject read a short English paragraph silently. The highest-grade level paragraph (Grade 10 – for adults) was used for measurement. There were five different passages in Grade 10. The subject read one practice paragraph following which two trials were made with different passages. The second trial was taken as the final reading to assure a stable baseline measurement.17 A comprehension test comprising 10 “Yes” or “No” responses were also administered to confirm the subject’s comprehension. After the recording, the system performed an automatic analysis and provided a report in a “Reading Profile” format (Fig. 1). Reading parameters included fixations per 100 words (progressive saccades), regressions per 100 words (backward saccades), fixation duration (seconds) which is the average length of time (in parts of a second) the eyes paused or fixated, reading rate (words per minute), grade level equivalent (GLE) which is the weighted average of the grade levels for the subject’s fixations, regressions and reading rate yielding a combined grade level, and comprehension (%) which is the percentage of correct answers. There are also large right-to-left oblique saccadic eye movements called saccades in return-sweep which occur when one must shift to the next line of print.17 The minimum comprehension for inclusion was set at 60% for all the study subjects considering that English is not the native language.
Results were analysed using SPSS (Statistical Package for Social Sciences, Version 17.0, SPSS Inc., Chicago). Non-parametric tests were done as the data did not follow normality (Shapiro–Wilk test) and appropriate coding was generated for categorical variables. Mann–Whitney U test was used to compare the values between TBI cases and controls. Kruskal–Wallis test was used to compare the values between different grades of TBI with controls. As the moderate and severe TBI groups had a lesser sample size, these two groups were combined as MS-TBI for analysis. Spearman’s correlation was used to understand the relationship between variables. Median and interquartile range (IQR) were used to represent the data. The alpha error was set as 5%.
ResultsResults from ninety subjects (30 cases and 60 controls) were included for statistical analysis. The mean age±SD of the TBI and controls was 28.7±8.5 years (18.4–58.9) and 28.4±7.7 years (20.4–57.0), respectively. The difference in age was not statistically significant between the two groups (p>0.05). There were 18 mild TBI (mTBI) and 12 moderate-severe (MS-TBI) (4 moderate and 8 severe) cases of TBI. A post-hoc power analysis was conducted due to lesser sample size in MS-TBI group. The statistical power of the study was 99.3%.
Aetiologies of TBIIn the present study, road traffic accidents (RTA) (n=24, 80%) was the most common cause of TBI followed by hit (n=4, 13%) and fall from height (n=2, 7%). All RTA’s were related to two-wheelers. Four subjects reported head injury due to an object that struck their head and two subjects due to falling from a height. The median (IQR) post-injury periods of mild, moderate and severe TBI were 2 (0.6–5), 1.2 (0.5–5.9), 2.5 (0.7–3.7) years, respectively.
Symptoms of TBI subjectsTBI subjects in the current study self-reported their symptoms which persisted over the past six months from the onset of TBI (Fig. 2). In the total TBI sample, reading difficulty (87%) was the most frequent visual issue followed by eye strain (47%), headache (40%), vertigo/dizziness (10%) and double vision (10%). A majority of mTBI subjects reported symptoms of reading difficulty, eyestrain and dizziness, and, MS-TBI subjects had issues such as a headache primarily followed by reading difficulty and eye strain (Table 2).
Reading eye movement parameters: TBI vs controlsThe results of the oculomotor-based reading eye movement assessment using ReadAlyzer™ were compared with age-matched controls (Table 3). Subjects with TBI presented with increased number of fixations/100 words: 137 (106–159), regressions/100 words: 24 (12–36), reduced reading rate of 154 (128–173) words per minute, lesser comprehension: 70 (60–80) percentage, lower grade level equivalent: 4.0 (3.0–7.0) and increased return sweep saccades: 1.7 (1.2–2.4) (represented in median (IQR); p<0.01).
Comparison of reading test parameters obtained from ReadAlyzer between controls and TBI.
| Reading test parameters | TBIb median (IQR) [n=30] | Controls median (IQR) [n=60] | Pa |
|---|---|---|---|
| Fixations/100 words (No.) | 137 (106–159) | 92 (76–102) | <0.001 |
| Regressions/100 words (No.) | 24 (12–36) | 10 (7–14) | <0.001 |
| Fixation Duration (sec) | 0.30 (0.27–0.33) | 0.29 (0.27–0.32) | 0.2 |
| Reading rate (words per min) | 154 (128–173) | 214 (199–244) | <0.001 |
| Comprehension (%) | 70 (60–80) | 90 (70–100) | 0.008 |
| Grade Level Equivalent (GLE) | 4.0 (3.0–7.0) | 10.0 (8.0–12.0) | <0.001 |
| Saccades in Return Sweeps (No.) | 1.7 (1.2–2.4) | 1.5 (1.3–1.8) | 0.022 |
To understand the reading eye movements based on the severity of TBI, a comparison between three groups (controls, mTBI and MS-TBI) was conducted which showed a statistically significant difference between the three groups (p<0.01) (Table 4). Post hoc analysis revealed a significant difference between controls and mTBI (p<0.01), controls and MS-TBI (p<0.01) and no difference was noted between mTBI and MS-TBI (p=0.43).
Comparison of reading test parameters obtained from ReadAlyzer between controls, mTBI and MS-TBI.
| Reading test parameters | Controls median (IQR) [n=60] | mTBI median (IQR) [n=18] | MS-TBI median (IQR) [n=12] | Pa |
|---|---|---|---|---|
| Fixations/100 words (No.) | 92 (76–102) | 128 (103–147) | 149 (117–160) | <0.001 |
| Regressions/100 words (No.) | 10 (7–14) | 20 (10–30) | 27 (16–38) | <0.001 |
| Fixation duration (sec) | 0.29 (0.27–0.32) | 0.30 (0.27–0.33) | 0.30 (0.27–0.33) | 0.48 |
| Reading rate (words per min) | 214 (199–244) | 162 (135–184) | 147 (116–165) | <0.001 |
| Comprehension (%) | 90 (70–100) | 80 (60–90) | 70 (60–80) | 0.02 |
| Grade Level equivalent (GLE) | 10 (8.0–12.0) | 5.5 (3.0–7.2) | 3.5 (3.0–4.0) | <0.001 |
| Saccades in return sweeps (No.) | 1.5 (1.3–1.8) | 1.9 (1.3–2.3) | 1.6 (1.2–2.4) | 0.001 |
Post hoc analysis revealed a significant difference between controls and mTBI, controls and MS-TBI (Mann–Whitney U test, p<0.05) and no difference was noted between mTBI and MS-TBI.
mTBI, Mild TBI; MS-TBI, Moderate-Severe TBI; p, p value.
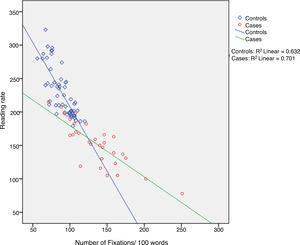
The relationship between the number of fixations/100 words and reading rate in TBI subjects showed a significantly strong negative correlation (Fig. 3) (Spearman’s r=−0.823, n=30, p=<0.001) in subjects with TBI. A similar result was observed for the controls as well (Spearman’s r=−0.79, n=60, p=<0.001)
DiscussionIn our study, reading eye movement parameters in subjects with TBI were evaluated and compared with age-matched controls. The current research is the first one in India to report reading eye movement parameters in TBI due to RTAs.
It is important to address the physical and visual issues following TBI as it can result in morbidity, mortality, disability and socio-economic losses in many developing countries.6 In India, an assessment of the injury pattern of RTAs had shown collisions resulting in head injuries which were caused frequently by two-wheelers (62%) and less likely by four-wheelers (12%);7 whereas, in western countries, most of the accidents were found to be due to four-wheelers (79%). In the present study, twenty-four subjects (80%) reported RTA due to two-wheelers and were diagnosed to have TBI. This scenario is due to the unprecedented motorization and safety procedures among the two-wheeler drivers.7,8
In the current study, subjects with TBI (60%) gave up their regular reading habits due to troubling eye-related symptoms. The evaluation of clinically based reading eye movements has provided insight into the functional integrity of the brain. ReadAlyzer™ was used to evaluate the reading eye movements. It has been a valid, clinical tool that provided consistent, objective and automated results on reading eye movement parameters. The advantage of this instrument is that the infrared cameras have allowed real-time observation of eye movements during recording. Dynamics of saccades such as saccadic latency and accuracy are also known to be affected by ageing.18 Therefore, the study sample recruitment was done by ensuring that controls were age-matched to a TBI subject.
In the present study, controls also had a lesser reading rate: 214 (199–244) words per minute compared to the established Taylor’s normative data. These differences suggested that reading an English text is based on familiarity with language and vocabulary.2 As English is a second language in India, the fluency and speed of reading are variable when compared to native English speakers. Hence, reading eye movement parameters of TBI subjects were assessed by comparing with age-matched controls due to the lack of an evident age-based normal reading rate for our population. All the subjects (TBI and controls) in the present study held a basic degree with fluency in English.
Individuals with TBI in the present study demonstrated significantly reduced reading rate, increased number of fixations, and a higher number of regressions. The results suggested that subjects with TBI had a low degree of saccade automation that resulted in an excessive number of unwanted saccades which reflected in their reading. We hypothesize that this could be due to the low gain in the saccadic amplitude of the primary saccade resulted in a hypometric saccade. Therefore, a corrective subsequent saccade was made to achieve the anticipated saccadic amplitude as observed in previous studies.1,19 These corrective saccades resulted in an increased number of fixations and regressions with poor reading eye movements. Subjects with TBI also had reduced comprehension which revealed a problem with inference and short-term memory in answering the questions along with basic demands of oculomotor coordination compared to controls.11 With all these parameters being reduced, the grade level equivalent was also lesser in subjects with TBI, as they read five grade levels lesser than controls. This finding of an increased number of inaccurate reading eye movements is consistent with a study reported by Thiagarajan, et al. on mTBI population which was measured using Visagraph (2014).1
Comparison of reading eye movement parameters between mild TBI (mTBI) vs. moderate and severe TBI (MS-TBI) with controls highlights that the oculomotor system is compromised both in mTBI and MS-TBI. Mild TBI and MS-TBI did not show any statistically significant difference even though the outcome measures were relatively affected in MS-TBI. Alternatively, the extent of reading dysfunction in TBI might not be truly dependent on injury severity. There lies a possibility that visual functions are vulnerable to damage regardless of the severity of the injury. Similarly, the symptoms of reading difficulty were profound in mTBI compared to MS-TBI inferencing that mTBI is similarly affected like MS-TBI. It has been described that the susceptibility of extensive neural networks affected multiple brain regions associated with control, execution, initiation and generation of saccades leading to reading dysfunction.1,3 The degree of reading impairment increased with the severity of the injury as an important clinical finding. These clinically based reading eye movements were addressed previously in mTBI, but not in MS-TBI using ReadAlyzer. Oculomotor testing is thus sensitive to detect subtle defects in all grades of TBI.
Having understood the visual sequelae in TBI, it is also important to rehabilitate these subjects with oculomotor vision therapy. Studies have shown that oculomotor rehabilitation can significantly improve overall reading and result in behavioural changes with a progressive effect on the QoL.1,20,21 This improvement has also been observed in the case of mTBI with convergence insufficiency and reading dysfunction that the authors reported earlier.22 Neuro-optometric vision therapy facilitated the subject to recuperate from the compromised state and perform better in his/her daily routine activities.
The limitations of the study include inadequate sample size in moderate and severe TBI groups. Visual symptoms were not quantified using a validated questionnaire used for TBI. Subjects only with proficiency in the English language were used as the reading passages were in English. Test paragraph with different regional languages that match the corresponding grade level equivalent may serve for non-English proficiency subjects. However, a post-hoc power calculation also suggested that the sample size is adequate enough to validate the results of this study.
This study adds evidence to the impaired reading eye movement performance in TBI invariable to the severity. The information on clinically based reading eye movements when translated into the natural reading process facilitated the interpretation of reading dysfunction.
ConclusionReading eye movement parameters are affected in traumatic brain injury irrespective of the severity of the injury. Extensive future research in the objective assessment of eye movements may help the clinicians to evaluate the reading deficits and also to monitor recovery and improvement with intensive neuro-optometric intervention.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interestThe authors have no conflicts of interest to declare.
The authors would like to acknowledge Mr. Kurt Mirdell, Developer of Visagraph II and ReadAlyzer for answering technical queries.










![Symptoms of all TBI subjects [n (%)].](https://static.elsevier.es/multimedia/18884296/0000001300000003/v2_202006170710/S1888429619301025/v2_202006170710/en/main.assets/thumbnail/gr2.jpeg?xkr=ue/ImdikoIMrsJoerZ+w90elkTtpMHXMkN9jatH7+0Y=)