The worldwide prevalence of refractive errors (RE), which is a common cause of treatable visual impairment among children, varies widely. We assessed the prevalence of correctable visual impairment (uncorrected RE) in primary school children in Qassim, Saudi Arabia.
MethodsA cross-sectional study was conducted in 21 primary schools. A total of 5176 children (mean age 9.5±1.8 years), 2573 boys (49.7%) and 2603 girls (50.3%), underwent a comprehensive eye examination. The examinations consisted of visual acuity, autorefraction, cover test, ocular motility, pupillary evaluation, anterior segment examination, cycloplegic auto-refraction and dilated fundus examination with direct ophthalmoscopy. The children were divided into groups based on their age and gender.
ResultsThe overall prevalence of RE in the better eye was 18.6% (n=963), and the prevalence of uncorrected RE 16.3% (n=846), with only 2.3% (n=127) of children wearing spectacles during examination. The prevalence of uncorrected myopia (5.8%) and myopic astigmatism (5.4%) was higher compared to that of hyperopic astigmatism (2.7%), mixed astigmatism (1.7%) and hyperopia (0.7%). The anisometropia prevalence was 3.6%. Risks for astigmatism, myopia and anisometropia were positively associated with age. In addition, myopia and anisometropia risks were also associated with female gender, while risk of astigmatism was correlated with male gender. Few children with vision reducing RE wore spectacles; an additional 16.3% of children could benefit from spectacle prescription.
ConclusionThe prevalence of uncorrected RE in children is relatively high and represents an important public health problem in school-aged children in Qassim province. Performance of routine periodical vision screening throughout childhood may reverse this situation.
La prevalencia mundial de los errores refractivos (ER), que son una causa común de disfunción visual tratable en niños, varia ampliamente. Evaluamos la prevalencia de la deficiencia visual corregible (ER no corregido) en escuelas de primaria de Qassim, Arabia Saudí.
MétodosSe realizó un estudio transversal en 21 escuelas primarias. Se sometió a un amplio examen visual a 5.176 niños (edad media 9,5±1,8 años): 2.573 chicos (49,7%) y 2.603 chicas (50,3%). El examen consistió en la evaluación de la agudeza visual, auto-refracción, cover test, motilidad ocular, evaluación pupilar, examen del segmento anterior, auto-refracción ciclopéjica y examen del fondo dilatado con oftalmoscopia directa. Se dividió a los niños en grupos, basándonos en su edad y sexo.
ResultadosLa prevalencia general de ER en el mejor ojo fue del 18,6% (n=963), y la prevalencia de ER no corregido fue del 16,3% (n=846), de los que únicamente el 2,3% (n=127) de los niños llevaban gafas durante el examen. La prevalencia de la miopía no corregida (5,8%) y astigmatismo miópico (5,4%) fueron superiores en comparación al astigmatismo hipermetrópico (2,7%), astigmatismo mixto (1,7%) e hipermetropía (0,7%). La prevalencia de anisometropía fue del 3,6%. Los riesgos de astigmatismo, miopía y anisometropía presentaban una asociación positiva con la edad. Además, los riesgos de miopía y anisometropía se asociaron también al sexo femenino, mientras que el correspondiente al se asoció al género masculino. Pocos niños con reducción visual por ER no corregido portaban gafas, y un 16,3% adicional de los niños podría beneficiarse de la prescripción de las mismas.
ConclusiónLa prevalencia de ER no corregido es relativamente elevada en niños de educación primaria, y representa un serio problema de salud pública en los niños en edad escolar de la provincia de Qassim. La realización de revisiones rutinarias y periódicas de la vista en la infancia podría revertir esta situación.
According to the World Health Organization (WHO), refractive errors (RE) such as myopia, hypermetropia and astigmatism are the second leading cause of visual impairment (uncorrected RE) among all age, gender and ethnic groups.1 Such visual impairments originate from RE correctable by refraction (“correctable visual impairment”, CVI) or RE associated with ocular or neurological disease and, thus not-correctable by refraction (“non-correctable visual impairment”, NCVI).2 CVI (uncorrected RE) implies that visual impairment is present when there is no or inadequate refractive correction.2 There would be about 153 million cases of visual impairment globally, with 12.8 million children (5–15 years old) affected by uncorrected RE1 in both developed and developing countries.3 Thus uncorrected RE is a significant public health concern.4,5 Though some children with uncorrected RE are asymptomatic,6 others occasionally complain of headaches and inability to read the material on the chalkboard, which can have a serious impact on a child's learning ability, academic performance, and personality.2,7
The Refractive Error Study in Children (RESC) was conducted in China, Nepal, Chile, India, South Africa and Malaysia, using a population-based method and logMAR protocol to assess children aged 5–15 years. Overall, 56–94% cases of reduced vision were caused by uncorrected RE.2 The proportion of children whose visual acuity could have been improved with spectacles to 20/32 or better increased with early detection from as low as 0.9% in South Africa8 to 9% in China.9,10
Though many studies have assessed the RE prevalence among school-aged children worldwide, only few studies have been performed in Saudi Arabia. According to UNESCO (2007), in Saudi Arabia the gross enrollment ratio (GER) for boys in primary school is 99.9% and 96.3% for girls, with a total GER of 98.1%.11 Qassim Province is the seventh most populated province of Saudi Arabia (population: 1,016,756). This province is served by primary, intermediate and secondary schools. Children enter elementary education at the age of 6 years, and the duration of study is six years. To the best of our knowledge, there is no data available on the prevalence of uncorrected RE in primary school children in Qassim province. Therefore, the present study was aimed at determining the prevalence of uncorrected RE among primary school children in different areas of Qassim province, and at assessing the association between age, gender, and these visual impairments considering that both the earlier and recent reports indicate an association between growth and RE risk.9,10,12–16
MethodsSelection of study population and data collectionThe study population was selected using a random cluster sampling in 112,975 primary school subjects in Qassim province. Among 440 primary schools, 21 schools (clusters) were randomly selected. All schools were comparable in terms of size, curricular and extra-curricular activities, and student population composition. In this cross-sectional study, candidates were selected from the school register and included after parental and school authority consent. Information enlightening parents about the need to correct RE was provided to school authorities, and the school authorities collected informed consents. The study was approved by the regional ethical committee.
Data were collected from September 2010 to May 2011, by two teams of trained and certified optometrists and ophthalmologists from Qassim University Optometry Department. Visual acuity (VA) measurements for distance and near, autorefraction and ocular motility assessment, cover test (distance and near), pupil evaluation, anterior segment examination with a slit lamp biomicroscopy, cycloplegic autorefraction and dilated fundus examination with direct ophthalmoscopy were performed.
CycloplegiaFor cycloplegia, two drops of cyclopentolate eye drops (1%) were administered to both eyes at a 5min interval. After 20min, if a pupillary light reflex was still present, a third drop was administered. The light reflex and pupil dilation were checked after an additional 15-min interval. Dilating and light reflex statuses were recorded 40–60min after the first drop. Cycloplegia was considered complete if the pupil dilated 6mm or more, and light reflex was absent.
Cycloplegic autorefraction was carried out by Autorefractor Keratometer Topcon KR-8900 (OptoVision, Miami, FL, USA) for all the subjects.17 Children found with uncorrected RE or undercorrected RE (using disease definitions presented in “Uncorrected RE definitions” section) underwent post-mydriatic subjective refraction 48h later.
Visual acuityDistance VA was measured with a retroilluminated logMAR chart with tumbling “E” optotypes on each line (Precision Vision, Villa park, IL). VA measurements began at a distance of 4m with the top line (20/200). The child was requested to indicate the direction of the E optotypes either by pointing with his/her hand or by naming the direction. If the orientations of at least four of the five optotypes were correctly identified, the child was then tested by dropping down to the line 4 (20/100). If no or only one optotype was missed, the testing resumed at line 7 (20/50), continued to line 10 (20/25) and finally line 11 (20/20). If at any level the child failed to recognize four of the five optotypes, the line immediately above the failed line was tested, until success. The lowest line read successfully was assigned as the VA of the tested eye. The right eye was tested first and then the left eye, each time occluding the fellow eye (RESC). If the uncorrected VA was <20/32 in either eye, pinhole acuity was measured. If the child presented with glasses, the power of the lens was measured using Nidek LM500 Auto Focimeter/lensometer (Nidek, Gamagori, Japan).18 In addition, aided VA was recorded for children who had spectacles during examination.
Uncorrected RE definitionsUncorrected RE was defined as a 2-line improvement with refraction in the better eye. Unmet refractive need was defined as having <20/40 visual acuity in the better eye and achieving ≥20/40 after refraction (definition 1), or having <20/40 visual acuity in the better eye and achieving a ≥2-line improvement with refraction (definition 2).19 Uncorrected VA was defined using unaided VA, presenting VA was defined using spectacle corrected acuity, if worn. Hence, children were considered in need of refractive correction if uncorrected VA was less than 20/40 in the better eye, which improved by at least two lines with refractive correction. The 20/40 VA threshold used in defining need coincided with the definition of visual impairment used in RESC studies. Children with spectacles were considered undercorrected if presenting VA in the better eye was improved by at least 2 lines with refraction (definition 3). Subjects who were not using optical correction and who had distance VA of 20/20 or better were considered as emmetropes. Children with vision not fully correctable because of amblyopia or pathological changes were not separated from those considered to be in need of refractive correction when VA improvement of two or more lines could be achieved.20
Refraction measurements: RE classificationRE were classified into myopia, hyperopia and astigmatism. Refraction measurements, expressed as spherical equivalents (SE), were calculated as the algebraic sum of the spherical measurement and 0.5 times the cylindrical power. The age-specific and gender-specific prevalences of myopia ≤−0.50 SE diopters (D) and of hyperopia ≥2.0 SE diopters were calculated.18 Myopia was categorized as mild (−0.50 D to −3.0 D), moderate (−3.1 D to −6.0 D) and high (>−6.0 D). Hyperopia was categorized as mild (+2.0 D to +3.9 D), moderate (+4.0 D to +5.9 D), and high (≥+6.0 D). Astigmatism was defined as cylinder ≥0.75 D. Anisometropia was defined as an interocular difference of ≥1D SE.17 All definitions referred to values obtained after cycloplegic autorefraction. Astigmatism was further analyzed by dividing the subjects into three types: myopic astigmatism (compound myopic astigmatism and simple myopic astigmatism), hyperopic astigmatism (compound hyperopic astigmatism and simple hyperopic astigmatism) and mixed astigmatism.21
Statistical analysisData analysis was performed using SPSS version 16. The prevalence of uncorrected RE was calculated as the ratio of the number of subjects with uncorrected RE to the total number of individuals evaluated, and the prevalence of the unmet refractive need was calculated for each of the two definitions as the ratio of the number of individuals with unmet refractive need to the total number of individuals evaluated. The prevalence of different types of RE (myopia, hyperopia, and astigmatism) was presented as a percentage. As two teams were involved in data collection, Independent t-test was conducted to compare the mean cycloplegic autorefraction SE values of inter-examiner differences. z-Test for proportions was used to assess differences in prevalence of uncorrected RE between males and females. The relationship of age and gender to uncorrected RE was explored by using bivariate logistic regression. The association of different types of astigmatism with age groups and gender was investigated using chi square test. Differences with p<0.05 were considered significant. Odds ratio with 95% confidence interval was calculated for potential risk factors that were independently associated with different types of RE.
ResultsOverall prevalence of REThe mean SE of the two teams (team 1, mean=−0.005±0.45 D; team 2, mean=0.06±0.56 D), range of SE measurements (−0.27 to 0.14 D) and absolute mean difference (0.065 D) were calculated. The absolute mean difference, which represented SE measurement differences between 2 teams, was not significant (0.065, p=0.536), suggesting good agreement of SE between the teams.
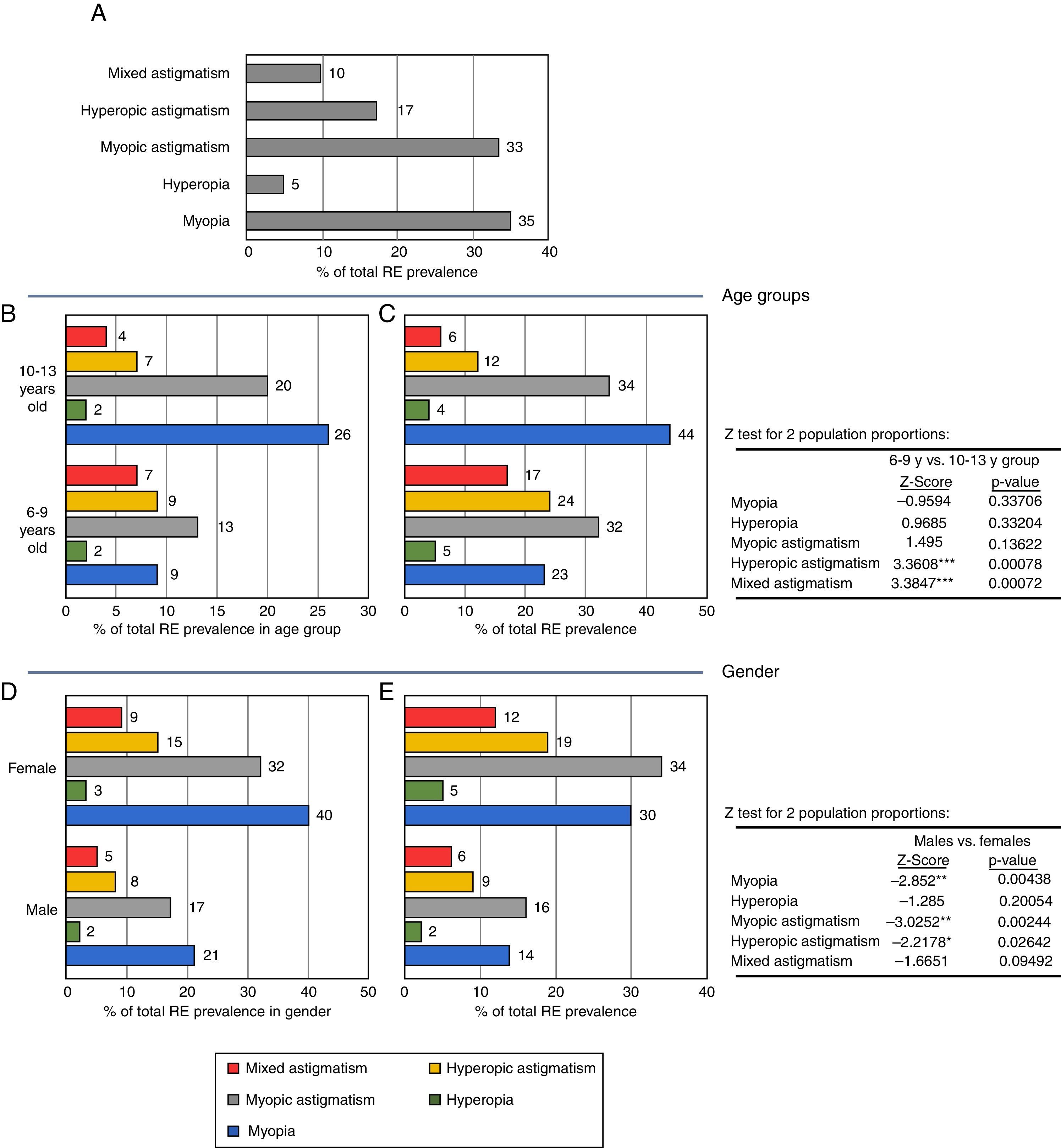
Baseline characteristics of children included in this study are shown in Table 1. From the 21 primary schools randomly selected, 5392 students were recruited, of which 5176 (96%) participated in the study. All the respondents were of Saudi ethnicity. They were divided into 2 groups based on their age: 6–9 years old (group 1) and 10–13 years old (group 2) participants. The overall prevalence of RE in the better eye was 18.6% (n=963; 95% CI 17.5–19.6) and the prevalence of uncorrected RE was 16.3% (n=846, 95% CI 15.3–17.3). The prevalence of different types of RE is shown in Fig. 1A. The prevalences of myopia (6.5%) and myopic astigmatism (6.2%) were higher compared to that of hyperopia (0.9%), hyperopic astigmatism (3.2%) and mixed astigmatism (1.8%).
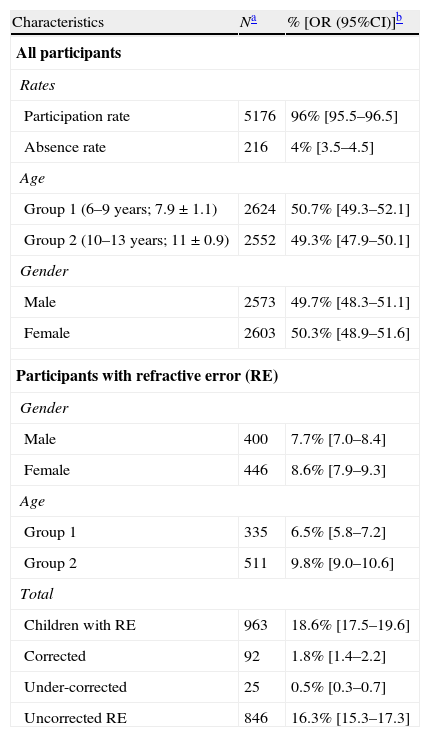
Characteristics of students included (study population).
| Characteristics | Na | % [OR (95%CI)]b |
| All participants | ||
| Rates | ||
| Participation rate | 5176 | 96% [95.5–96.5] |
| Absence rate | 216 | 4% [3.5–4.5] |
| Age | ||
| Group 1 (6–9 years; 7.9±1.1) | 2624 | 50.7% [49.3–52.1] |
| Group 2 (10–13 years; 11±0.9) | 2552 | 49.3% [47.9–50.1] |
| Gender | ||
| Male | 2573 | 49.7% [48.3–51.1] |
| Female | 2603 | 50.3% [48.9–51.6] |
| Participants with refractive error (RE) | ||
| Gender | ||
| Male | 400 | 7.7% [7.0–8.4] |
| Female | 446 | 8.6% [7.9–9.3] |
| Age | ||
| Group 1 | 335 | 6.5% [5.8–7.2] |
| Group 2 | 511 | 9.8% [9.0–10.6] |
| Total | ||
| Children with RE | 963 | 18.6% [17.5–19.6] |
| Corrected | 92 | 1.8% [1.4–2.2] |
| Under-corrected | 25 | 0.5% [0.3–0.7] |
| Uncorrected RE | 846 | 16.3% [15.3–17.3] |
Refractive error (RE), age and gender. (A) Prevalence of uncorrected refractive errors. Note the high prevalence of myopia and myopic astigmatism. (B) RE subtype prevalence in function of total RE prevalence in age groups. Note the high prevalence of myopia and myopic astigmatism in 10–13 years old students. (C) Uncorrected RE distribution in age groups: RE subtype prevalence in function of total RE prevalence and age group. Note the two-fold increase in mixed astigmatism and hyperopic astigmatism in 10–13 years old students as compared with 6–9 years old ones. (D) Refractive error (RE) subtype prevalence in function of total RE prevalence in gender. Note the high prevalence of myopia and myopic astigmatism in both genders. (E) Uncorrected RE distribution in genders: RE subtype prevalence in function of total RE prevalence and gender. Note the high prevalence of RE in females, in particular myopic astigmatism and myopia. z test: *p<0.05, **p<0.01, ***p<0.001.
Few of the children with vision reducing RE were wearing spectacles; an additional 16.3% of children could benefit from spectacle prescription.
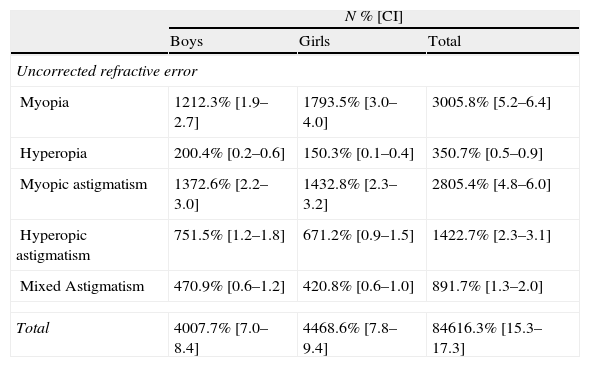
Prevalence of uncorrected RE by genderUncorrected RE prevalence was slightly higher in girls (8.6%, n=446, 95% CI 7.9–9.3) compared to boys (7.7%, n=400, 95% CI 7.0–8.4), but such difference was not statistically significant (z-test for proportions, p=0.08). The prevalence of various types of uncorrected RE (according to the definitions) by gender is shown in Table 2. The overall prevalence of uncorrected myopia (5.8%) and myopic astigmatism (5.4%) was higher than that of uncorrected hyperopia (0.7%), hyperopic astigmatism (2.7%) and mixed astigmatism (1.7%). Of 511 children diagnosed with uncorrected astigmatism, 280 (54.8%) had myopic astigmatism, 142 (27.8%) hyperopic astigmatism, and 89 (17.4%) mixed astigmatism. Instead, myopia was mild in 87% cases, moderate in 10.9%, and severe in 2.1%. Mild, moderate and severe hyperopia was observed in 36.4%, 52.3%, and 11.4% of the hyperopic participants, respectively. The mean SE of myopia for boys and girls were −1.69±1.63 D and −1.65±1.11 D respectively; the mean SE of hyperopia for boys and girls were +2.87±2.19 D and +3.16±2.12 D respectively. The rate of anisometropia of 1.0D or more was found in 3.6% (n=189, 95% CI; 3.1–4.1%).
Prevalence of various types of uncorrected RE by gender.
| N % [CI] | |||
| Boys | Girls | Total | |
| Uncorrected refractive error | |||
| Myopia | 1212.3% [1.9–2.7] | 1793.5% [3.0–4.0] | 3005.8% [5.2–6.4] |
| Hyperopia | 200.4% [0.2–0.6] | 150.3% [0.1–0.4] | 350.7% [0.5–0.9] |
| Myopic astigmatism | 1372.6% [2.2–3.0] | 1432.8% [2.3–3.2] | 2805.4% [4.8–6.0] |
| Hyperopic astigmatism | 751.5% [1.2–1.8] | 671.2% [0.9–1.5] | 1422.7% [2.3–3.1] |
| Mixed Astigmatism | 470.9% [0.6–1.2] | 420.8% [0.6–1.0] | 891.7% [1.3–2.0] |
| Total | 4007.7% [7.0–8.4] | 4468.6% [7.8–9.4] | 84616.3% [15.3–17.3] |
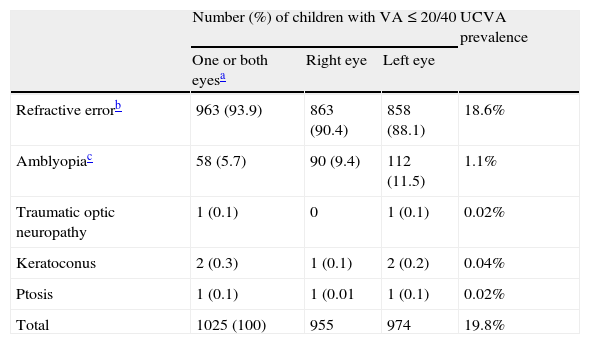
The distribution of uncorrected RE according to age groups is shown in Fig. 1B and C. A concomitant increase in prevalence of myopia and myopic astigmatism with increase in age was observed (Fig. 1B). Uncorrected RE was observed in 337 (38.2%) participants in Group 1 and in 509 (61.8%) in Group 2 (Fig. 1C). Factors responsible for uncorrected visual acuity (UCVA) of 20/40 or worse in one or both eyes are summarized in Table 3. The prevalence of UCVA of 20/40 or worse was 19.8%. The main cause was RE (93.9% of UCVA cases) and other causes were traumatic optic neuropathy, ptosis and keratoconus.
Ocular disorders and uncorrected visual acuity (UCVA).
| Number (%) of children with VA≤20/40 | UCVA prevalence | |||
| One or both eyesa | Right eye | Left eye | ||
| Refractive errorb | 963 (93.9) | 863 (90.4) | 858 (88.1) | 18.6% |
| Amblyopiac | 58 (5.7) | 90 (9.4) | 112 (11.5) | 1.1% |
| Traumatic optic neuropathy | 1 (0.1) | 0 | 1 (0.1) | 0.02% |
| Keratoconus | 2 (0.3) | 1 (0.1) | 2 (0.2) | 0.04% |
| Ptosis | 1 (0.1) | 1 (0.01 | 1 (0.1) | 0.02% |
| Total | 1025 (100) | 955 | 974 | 19.8% |
UCVA: uncorrected visual acuity.
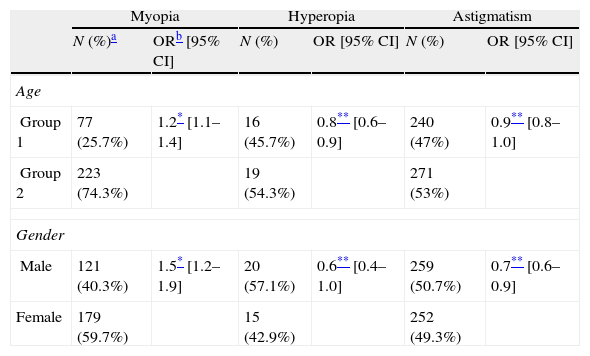
The distribution of uncorrected RE according to gender is shown in Fig. 1D and E, and Table 4 shows results of bivariate logistic regression analysis assessing the association of different types of uncorrected RE (myopia, hyperopia and astigmatism) with age groups and gender. Higher prevalence of myopia with increasing age was statistically significant (OR, 1.21; 95% CI, 1.09–1.35; p<0.001). Prevalence of myopia was significantly higher in girls compared to boys (OR, 1.52; 95% CI, 1.23–1.87; p<0.001). A significantly lower prevalence of hyperopia with increasing age was observed (OR, 0.79; 95% CI; 0.63–0.98, p<0.05), and boys had higher prevalence than girls (OR, 0.61; 95% CI, 0.37–1.00; p<0.05). Astigmatism prevalence increased with age (OR, 0.88; 95% CI, 0.79–0.96; p<0.05), and boys had higher prevalence (OR, 0.74; 95% CI, 0.60–0.90; p<0.05).
Analysis of the association of uncorrected RE with age and gender using logistic regression analysis.
| Myopia | Hyperopia | Astigmatism | ||||
| N (%)a | ORb [95% CI] | N (%) | OR [95% CI] | N (%) | OR [95% CI] | |
| Age | ||||||
| Group 1 | 77 (25.7%) | 1.2* [1.1–1.4] | 16 (45.7%) | 0.8** [0.6–0.9] | 240 (47%) | 0.9** [0.8–1.0] |
| Group 2 | 223 (74.3%) | 19 (54.3%) | 271 (53%) | |||
| Gender | ||||||
| Male | 121 (40.3%) | 1.5* [1.2–1.9] | 20 (57.1%) | 0.6** [0.4–1.0] | 259 (50.7%) | 0.7** [0.6–0.9] |
| Female | 179 (59.7%) | 15 (42.9%) | 252 (49.3%) | |||
Chi-square analysis of the association of different types of astigmatism (myopic, hyperopic and mixed astigmatism) with age groups and gender revealed a statistically significant difference in the prevalence of myopic astigmatism between group 2 and group 1 children (OR, 1.8; 95% CI; 1.4–2.3, p<0.05), but no significant difference between genders (OR=1.1, p<0.05). No significant difference was found in the prevalence of hyperopic astigmatism (respectively mixed astigmatism) between age groups (OR=0.8, respectively 0.7) or genders (OR=0.9, respectively 0.9).
DiscussionThe present data reveal associations between age, gender, and different types of RE in primary school students in Qassim Province, Saudi Arabia. The present study included a large sample size of children of Saudi ethnicity, from both urban and suburban areas, with a near equal gender distribution. The overall prevalence of RE was 18.6%, and astigmatism and myopia were the most common RE.
Uncorrected RE, gender and ageMyopia was the second most common type of uncorrected RE in this study (5.8%). Its prevalence in Qassim was comparable to prevalence reported in Chile (5.8%)22 and Iran (4.3%),17 but lower than that in China (14.9%),10 Malaysia (20.7%),24 Hong Kong (36.7%)12 and Singapore (36.3%).25 The difference in prevalence with the latter studies can be due, in part, to the population age studied (6–13 vs. 5–15/7–15 years old). This hypothesis is supported by the observation of increased prevalence of myopia with age, and by previous studies.9,10,12,13 RESC studies from China reported notable upward trends for myopia beginning with 7–8 years old groups and coinciding with age at which schooling with intensive near work begins; another upward trend was apparent at 11–12 years old, around the beginning of secondary school and puberty.9,23 Thus, it appears that more time spent on near work and less time spent outdoors could have been the major causes of myopia. This hypothesis is also agreed to by various studies showing that higher education level increases the risk of myopia.12,13,16
Besides, in the present study the prevalence of myopia was higher in girls, than in boys. This finding corroborates various reports, including for instance Pärssinen and Lyyra's report where the prevalence of myopia and its progression were significantly higher in girls than in boys in the third and fourth grade students.26 Other studies from China9,23 and India 13 reported comparable observations. On the contrary, some studies failed to show any association between gender and myopia risk.22,27 Such difference between findings can be due at least partly to the age of females in the study populations, as strongly indicated by various large cohort studies focusing on children age and RE prevalence, where rates of progression of myopia in boys and girls were attributable to peak height velocity.16,26,28 In these studies, variations in the onset and progression of myopia were associated with growth spurts, and interestingly, both boys and girls with earlier peak height velocity had correspondingly earlier onset and progression of myopia,16 but overall, peak height velocity was more commonly earlier in girls, where it was associated with earlier axial length (AL) peak and spherical equivalent (SE) velocity.28 In the present study performed on primary school children in the age range of 6–13 years old, i.e. in the phase of active growth, it appears that our findings are in agreement with the latter studies. It may be interesting to measure height and AL measurement in future studies, to unequivocally confirm the growth spurts (thus age), gender, and RE association hypothesis in Qassim province. In addition to study population age, discrepancies between studies can also be due to ethnicities, and methodological approaches such as definitions of RE (myopia, hyperopia and astigmatism) or methods for RE measurement (cycloplegic retinoscopy or cycloplegic autorefraction).
Moreover, the observation of a high prevalence of anisometropia in this study (6–13 years old), which corroborates various previous studies,29 was in disagreement with studies using 7–15 years old children.12,30 Although the total prevalence rate of uncorrected RE was marginally higher in girls and with age, such difference was not statistical significant, probably due to the fact that the prevalence of the most common type of uncorrected RE in this study, i.e. astigmatism, increased with age but mostly in boys, as also reported in other large cohort studies.10,31–33 In addition, a significantly lower prevalence of hyperopia with increasing age, particularly marked in boys, was also observed. Though the etiology of uncorrected RE is poorly understood, considerable differences are to be expected in the pathogenic mechanisms of diseases displaying so much different clinical manifestations and course.34–36 Such differences may account, at least partly, for the disagreements in trends of correlations between age/gender and uncorrected RE herein reported. However, the consistency of age/gender and specific uncorrected RE with previous studies points to a role of hormonal mechanisms in uncorrected RE pathogenesis, as suggested by various population-based genomic and proteomic studies.15,37,38
Prevalence of uncorrected RE in primary school studentsRE contributed to 93.9% of UCVA of 20/40 or worse and 94.6% of amblyopia, and the prevalence of uncorrected RE in Qassim primary school children (16.3%) was higher compared to that in geographic areas with broad screening programs such as Kelantan in Malaysia (7.0%),39 Guangzhou (9.8%)9 and Shunyi (9.7%)10 districts in China, Cairo city in Egypt (12.7%),40 and Al-Hassa, Saudi Arabia (12.4%)14 in children of similar age ranges. Furthermore, in our study 87.6% of the children with RE were uncorrected. Factors responsible for uncorrected RE in that province may include the lack of awareness and recognition of the health threat represented by uncorrected RE in school children at family level associated with cultural disincentives to compliance, lack of availability of refractive services, and inadequate manpower.1,41 Considering that altogether the findings of the present study warrant the need for screening RE in primary school students, particularly in Qassim province, the implementation of child eye health programs for an effective and sustainable delivery of eye care to children, which may be integrated within school health programs for instance, is mandatory given the implications for public health. In addition, we suggest the performance of periodical vision screening throughout childhood, which is a cost-effective approach for early detection of visual impairment in children, and is by far preferable to complete eye examination after onset of marked visual impairment or blindness associated with uncorrected RE.
ConclusionRE in school age children is an important public health problem because it has a substantial impact on learning capabilities and educational potential. Even though the treatment of RE can be simple and successful, our data show that the condition continues to be a significant risk factor leading to visual impairment in Qassim province. Though uncorrected RE is prevalent among primary school children. Only a small percentage of the children with RE wore spectacles. Thus, periodic vision screening in school children is recommended. Parents and teachers should be educated about the need for an early comprehensive eye care/screening and correction with spectacles.
Conflicts of interestThe author has no conflicts of interest to declare.
This study was funded by Qassim University Deanship of Scientific Research. The author thanks the administrative authorities of education of Qassim Province for their cooperation and Qassim University Optometry Department staff for their support in data collection. The author also thanks Prof. Scheiman M. and Prof. Kovin Naidoo, for reviewing and giving their expert opinion on this manuscript.