Presbyopia is the gradual inability to focus near objects with age. This study explores patients’ attitudes and beliefs towards presbyopia including preferred modes of near refractive correction.
MethodsIn the United Kingdom, twenty-four volunteers completed an online questionnaire and attended a structured, recorded focus group. Participants’ age ranged between 36 and 48 years, representing a pre-presbyopic and a presbyopic population. Attitudes and beliefs about presbyopia, its significance, and opinions about current refractive correction including multifocal contact lenses were transcribed and coded using content analysis for overarching themes and patterns.
ResultsSix participants (25%) were already wearing a near visual correction while 18 (75%) were not. Five key primary themes with clear inter-participant similarities were identified as ‘age-related’ (75%), ‘acceptance’ (50%), clear lack of ‘familiarity with the word presbyopia’ (65%), a mixed/ reluctant attitude ‘towards (multifocal) contact lenses’ (62.5%), and ‘comfort and convenience’ of a presbyopic correction (79%) whereby cost is of less importance.
ConclusionThe need for a reading correction was perceived as a sign of age. Spectacles were the most preferred mode of near vision correction, while comfort and convenience were seen as more important than cost. Patient education about presbyopia is lacking. Multifocal contact lenses are not necessarily the preferred visual correction even if the patient already wears contact lenses for distance.
Presbyopia is defined as the gradual inability to focus near objects on the retina due to insufficient accommodative ability following increasing age and the loss of elasticity in the crystalline lens.1–3 A variety of factors are involved including hardening of the lens, changes in the elasticity of the lens capsule, lens dimension, geometry of zonular attachments and ciliary muscle contraction. However, it is still unknown how much each factor is responsible for this loss of accommodative ability.4 In 2015, the number of people with presbyopia was estimated to be 1.8 billion (prevalence 25%, 95% confidence interval 23 %–27%) worldwide.5 Due to the growing ageing population, most of our population will spend roughly half their lives as presbyopes.3 The onset of presbyopia is therefore a common finding for eye care practitioners (ECPs), which is generally considered to take place somewhere between 38–45 years of age6 depending on factors such as a patient’s distance refractive error and amount of near work, while trauma, systemic disease, and drug side effects are other common modifiable risk factors for premature presbyopia.7
There are currently a number of corrective mechanisms for presbyopia, including spectacles (multifocal, bifocal), single vision contact lenses (CLs) alongside reading glasses, monovision contact lenses (one eye corrected optimally for distance and the other for near tasks), as well as multifocal and bifocal CLs.8 Studies have explored the effectiveness and visual benefits of these different modalities of correction for presbyopic patients.3,9 However, there are currently no up-to-date population-based studies investigating the use of multifocal contact lenses, a corrective mechanism that is associated with high dropout rates compared with other types of contact lenses, often due to an imbalance between distance and near vision.10
A survey amongst ECPs found that 50% would only recommended CLs very occasionally to their presbyopic patients.11 In addition, McDonnell et al. showed that presbyopia is associated with negative effects on vision targeted health related quality of life.12 Those 45 years of age or older (classified as presbyopes) reported significantly reduced clarity of vision, symptoms, dependence on correction, and satisfaction with their correction when compared to younger participants (non-presbyopes), after adjustment for sex, race, and socio-economic status.
This exploratory, cross-sectional study aimed to investigate pre-presbyopic and presbyopic patients’ attitudes and opinions on presbyopia and the methods in which it can be visually corrected, with a particular focus on (multifocal) contact lenses. Patients’ current knowledge on the process of presbyopia itself was explored, including their current and preferred future methods of refractive correction (single vision or varifocal spectacles, laser surgery, contact lenses including multifocal and monovision, or a combination), establishing the factors which influence these preferences.
MethodsParticipants were recruited between September 2018 and February 2019 from the School of Health at City, University of London and Moorfields Eye Hospital, London. The participants represented a variety of backgrounds in healthcare, academia, and engineering, and these were a combination of managerial, professional, as well as support staff. Inclusion criteria for the study were adults aged between 36–48 years. There were no exclusion criteria other than age, clinical optometric or ophthalmic background, and willingness to verbally share ideas and opinions in a focus group. This study received approval from the Optometry Research & Ethics Review panel at City, University of London (United Kingdom). Prior to completing the study, all volunteers provided written informed consent conforming to the tenets of the Declaration of Helsinki.
Data collectionParticipants completed an online pre-questionnaire relating to their current distance and near visual correction, wearing time, and whether they had considered alternative near corrective options. This was followed with a focus group, which included 3–7 participants and lasting approximately 30−45 min. Each session was recorded for transcription and analyses purposes while preserving confidentiality and anonymity. Topic guides were provided to each volunteer prior to the session. The participants within each group were mixed in terms of their current visual corrections and visual needs, e.g. some wore a correction while some did not, and both presbyopes and pre-presbyopes were represented at each focus group. The format of the focus groups was centred around the questions on the topic guides which each individual participant was encouraged to answer/ discuss until opinions on all of the questions were gained. This often led to further discussions of interest. The focus groups were repeated until saturation was reached whereby no new themes were arising or expected to arise in any further subsequent discussions.
AnalysisAll the focus group discussions were transcribed manually after the sessions; this provided the basis for coding and analysis of the transcripts and establishing themes between the groups that were similar, recurring, or any new or unexpected themes (qualitative analysis). Attitudes and beliefs were subcategorised in ‘primary themes’ based on their similarities, which were used to determine the overarching ideas and attitudes within the discussions. Quantitative analysis included the percentages of participants who identified with these themes.
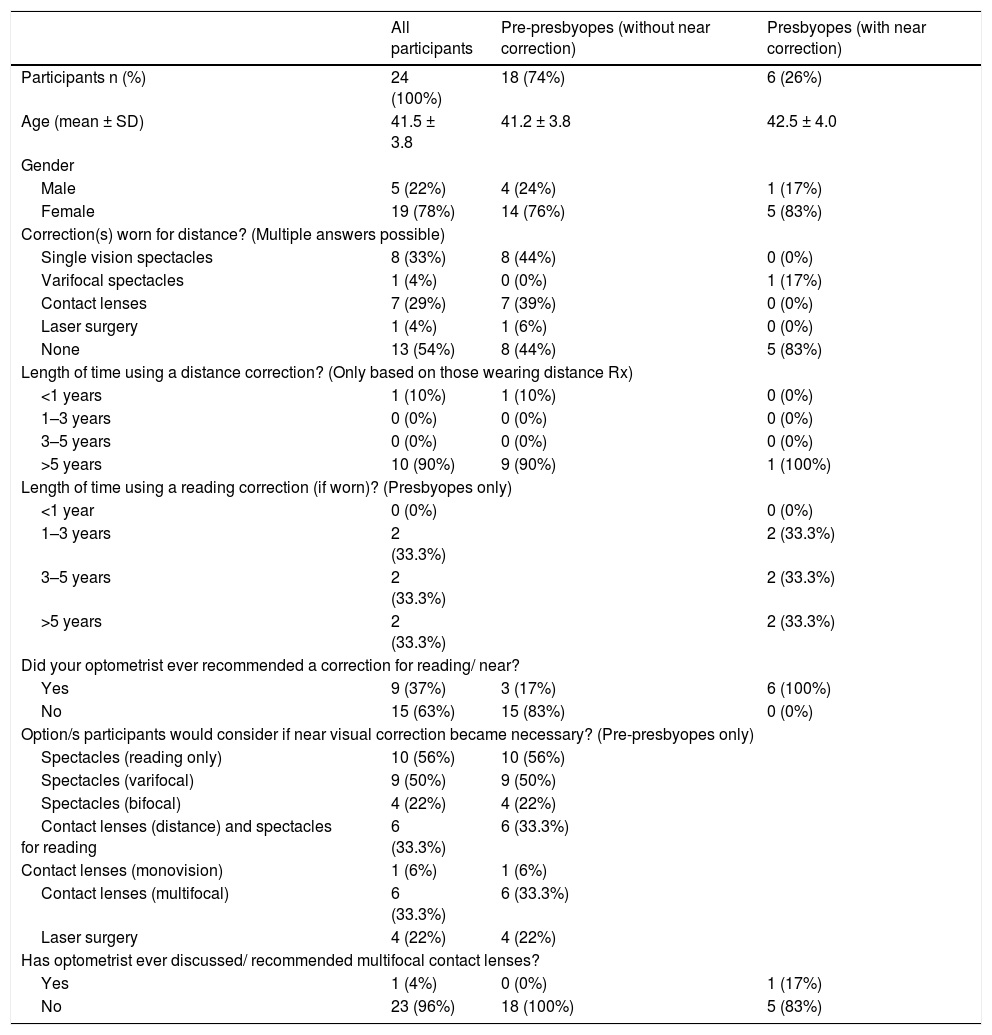
ResultsDemographic and responses to the electronic pre-questionnaire are summarized in Table 1. A total of 24 participants (19 females, 5 males), age range between 36 and 48 years, were divided in two groups: group A pre-presbyopes without near correction (n = 18) and group B presbyopes with a near correction (n = 6).
Demographics and online pre-questionnaire results. Parameters are shown in total amount of participants (percentage within the group) and mean ± standard deviation (SD) for age. Abbreviations: SD standard deviation; Rx refractive prescription.
| All participants | Pre-presbyopes (without near correction) | Presbyopes (with near correction) | |
|---|---|---|---|
| Participants n (%) | 24 (100%) | 18 (74%) | 6 (26%) |
| Age (mean ± SD) | 41.5 ± 3.8 | 41.2 ± 3.8 | 42.5 ± 4.0 |
| Gender | |||
| Male | 5 (22%) | 4 (24%) | 1 (17%) |
| Female | 19 (78%) | 14 (76%) | 5 (83%) |
| Correction(s) worn for distance? (Multiple answers possible) | |||
| Single vision spectacles | 8 (33%) | 8 (44%) | 0 (0%) |
| Varifocal spectacles | 1 (4%) | 0 (0%) | 1 (17%) |
| Contact lenses | 7 (29%) | 7 (39%) | 0 (0%) |
| Laser surgery | 1 (4%) | 1 (6%) | 0 (0%) |
| None | 13 (54%) | 8 (44%) | 5 (83%) |
| Length of time using a distance correction? (Only based on those wearing distance Rx) | |||
| <1 years | 1 (10%) | 1 (10%) | 0 (0%) |
| 1–3 years | 0 (0%) | 0 (0%) | 0 (0%) |
| 3–5 years | 0 (0%) | 0 (0%) | 0 (0%) |
| >5 years | 10 (90%) | 9 (90%) | 1 (100%) |
| Length of time using a reading correction (if worn)? (Presbyopes only) | |||
| <1 year | 0 (0%) | 0 (0%) | |
| 1–3 years | 2 (33.3%) | 2 (33.3%) | |
| 3–5 years | 2 (33.3%) | 2 (33.3%) | |
| >5 years | 2 (33.3%) | 2 (33.3%) | |
| Did your optometrist ever recommended a correction for reading/ near? | |||
| Yes | 9 (37%) | 3 (17%) | 6 (100%) |
| No | 15 (63%) | 15 (83%) | 0 (0%) |
| Option/s participants would consider if near visual correction became necessary? (Pre-presbyopes only) | |||
| Spectacles (reading only) | 10 (56%) | 10 (56%) | |
| Spectacles (varifocal) | 9 (50%) | 9 (50%) | |
| Spectacles (bifocal) | 4 (22%) | 4 (22%) | |
| Contact lenses (distance) and spectacles for reading | 6 (33.3%) | 6 (33.3%) | |
| Contact lenses (monovision) | 1 (6%) | 1 (6%) | |
| Contact lenses (multifocal) | 6 (33.3%) | 6 (33.3%) | |
| Laser surgery | 4 (22%) | 4 (22%) | |
| Has optometrist ever discussed/ recommended multifocal contact lenses? | |||
| Yes | 1 (4%) | 0 (0%) | 1 (17%) |
| No | 23 (96%) | 18 (100%) | 5 (83%) |
There was a clear lack of familiarity with the word presbyopia. This was in reference to either not having heard of the word at all, or having heard it but being unaware of what it meant. In total, 83% (n = 20) of all participants did not have a professional background in eye care and out of these individuals, 65% were not familiar with the term presbyopia and/or not aware what it means. A small number of participants (n = 2) however, either knew or could predict the meaning of the word due to its etymology and resemblance to other words. Several non-eye care professionals who held a greater understanding of biological sciences and optics (10% of participants) mentioned key phrases such as ‘loss of elasticity’.
Presbyopia is age-relatedThe majority of comments strongly suggested that presbyopia is perceived as age-related and aspects related to presbyopic correction, such as reading glasses, are a sign of age. Seventy-five percent of all participants mentioned terms relating to and including ‘getting older’ and a ‘decline’ with ‘age’ or ‘elasticity’. With regards to the age that participants assumed presbyopia to occur, the general consensus was ‘between 40–45 years’ or ‘mid 40s’. Without prompting, 29% (n = 7) of participants stated this age or age range when they spoke about their prior knowledge on presbyopia or when any information about presbyopia should be mentioned to the patient by an ECP.
Expectation and acceptance of presbyopiaThere seemed to be a general consensus (mentioned in some form by 50% of all participants) that the onset of presbyopia is expected or there is an acceptance that it will occur or is occurring. Among those who did not wear a reading correction at the time of the focus group, there seemed to be more of a reluctant outlook on this prospect (44%), with one participant even referring to ‘dreading’ it. There were a variety of other levels of severity in which this sense of reluctance was expressed by participants, including being ‘worried’ about handling more than one type of visual correction and the impending realisation that ‘it’s my time [to deal with presbyopia]’.
Contact lens correction including multifocal contact lensesThere was a notable negative stance towards contact lenses for the correction of distance and near vision from both presbyopic and pre-presbyopic participants who were not contact lens wearers for distance vision (n = 17; 71% of all participants). However, the majority of pre-presbyopes (those not wearing a near correction) who were wearing contact lenses for distance (29% of pre-presbyopes, n = 7) seemed more open to the idea of contact lens correction when discussing their (future) near prescription. Interestingly, of these 7 participants, 2 (28%) shared relatively negative comments about multifocal contact lenses, which were related to a) the feeling of ‘being lazy’ which increased with age (and therefore preferring spectacles instead), or b) contact lens wear being ‘awkward, moderately [uncomfortable], in general a bit of a disappointing experience that I would avoid if I had other options’.
None of the 6 participants requiring a near correction (26%) were currently multifocal contact lens wearers. Two main reasons were noted, these being 1) previous unsuccessful multifocal lens wear including a poor visual experience, and 2) never heard of the existence of these type of contact lenses. In comparison, the remainder of the current contact lens wearers were generally enthusiastic about the idea of contact lens wear for presbyopia including multifocal contact lenses and monovision. However, they had not received any information about these options by their ECP.
Comfort and convenience more important than costOf all participants, 79% (n = 19) indicated that cost, comfort and convenience factors, as well as vision were the most important when considering corrective options for near. Although financial consideration was an issue that was mentioned by just under half (46%) of all the participants in some form, the general attitude also indicated a preference towards comfort, convenience and standard of vision over cost of the correction. Cosmetic factors were only mentioned in relation to the use of bifocal spectacles. Without prompting, a total of 4 participants commented on this type of spectacles in a negative sense, with one individual referring to her grandmother’s ‘big glasses with the squares’, stating that she thought ‘is what it's going to be like as I get older’. Unexpectedly, none of the participants commented on reluctance to wear single distance or reading/varifocal spectacles due to poor cosmetics or other aspects relating to appearance.
Information for patientsA final prominent theme that was mentioned regularly throughout the discussions was the issue of where the information on presbyopia should originate from; the overall consensus was that the optometrist or other eye care practitioner are the professionals who should provide this information to their patients. However, there was also a belief that there is scope for the general practitioner (GP) to play a role, possibly as part of the NHS Health Check for adults in England aged 40–74 (www.nhs.uk/conditions/nhs-healthcheck/).
DiscussionThis study describes the attitudes and beliefs towards presbyopia, and the forms in which this can be corrected with a secondary focus on contact lenses. Unique to this study was the use of focus groups instead of questionnaires only in a demographic that mainly consisted of pre-presbyopes. Generally, participants were aware of presbyopia as a ‘natural ageing process’; however, the term ‘presbyopia’ itself was not considered common knowledge. It may be somewhat surprising that the majority of participants were not aware of the term presbyopia or what it meant, despite the epidemiology of presbyopia being 100%.13 Our results are similar to previous work which indicated that there is a general lack of awareness of the topic, which is thought to be one of the main reasons for a 34% prevalence of unmanaged presbyopia even in developed countries.9
Any ECP (optometrist or other) is advised to focus on providing patients with sufficient information about presbyopia and to communicate all the available corrective options and their benefits. The principle belief throughout the group discussions was that information about presbyopia and its corrective means should come from an eye-care practitioner rather than a GP practice. Although most participants in our study shared this belief in discussion, some mentioned potential alternatives including the NHS or GP. Instead of waiting for the ECP to introduce the topic of presbyopia once patients notice changes to their near vision, it was suggested to include this possibly as part of the NHS Health Check for adults in England aged 40–74. The current research on this health initiative indicates much of the focus is on the reduction of cardiovascular morbidity14; however, with nearly all of adults displaying presbyopic symptoms from 40 years onwards and it being the most common physiologic ocular change after the age of 4015, it appears logical to have this mentioned as a prompt for check-up. In terms of when the topic of presbyopia and/or correction should be introduced, several patients mentioned they would like to be informed about presbyopia an adequate length of time prior to the associated changes in vision, with a ‘forewarning 5 or 10 years before it’s likely to happen,’ and ‘a vague idea that you’re expecting your vision to get worse and therefore you’re going to need a check-up every now and again’. In addition, Fylan and Grunfeld16 reported that 70% of participants within their study wished for their ECP to inform them more about their eyesight in general, as well as difficulties with their vision.
Interestingly, a survey of nearly 800 presbyopic patients found that only 9 percent of current contact lens wearers reported being told about multifocal contact lenses when they complained to their practitioners about initial near vision problems.17 Surprisingly, nearly 50% of 398 ECPs report that they would present the options for multifocal CLs to their patients, although often they do so to selected groups only.18 Here, mentioning presbyopia early must be considered as well: avoid communicating this change in focussing ability when reading or close work becomes a problem for the emerging presbyopic patient, but consider sharing this information prior to the onset of presbyopia to encourage awareness. As recognised by Charman,3 the multifocal contact lens market has seen only limited success when compared to contact lenses for distance vision, and these lens types are still ‘preferred only by a minority of older patients, most of whom are early presbyopes’. It has been suggested that any new CL wearer with either emmetropia or low amounts of refractive error (also known as ametropia) for distance, and those unwilling to accept a visual compromise, would have a low probability for successful presbyopic contact lens wear.8 This perhaps highlights an area of focus for ECPs: manage patients’ expectations without being too cautious as well as emphasise the freedom of contact lenses over spectacles. The focus for primary eye care professionals seems to indicate that emphasis should be placed on provision of information about alternative means of correction to early and pre-presbyopes. It must be noted that lack of patient education is not the only reason for the smaller multifocal contact lens market; it has been recognised that dropping out of contact lens wear with age can be attributed to a lack of available suitable higher near prescriptions, as well as an increase in dry-eye related problems,19,20 and the possibility that overall cosmetic concern reduces with age.21
Cost, convenience, and comfort were highlighted as a primary theme by all our participants. It has been noted that discomfort in contact lens wear is a major reason for subsequent discontinuation, alongside dryness, vision and handling,22 with vision-related problems reported as the main issue for presbyopic wearers in particular.10 To participants already wearing a habitual distance prescription, convenience and comfort were considered more important than the relative cost of (multifocal) contact lenses. It has been reported that although ECPs perceive cost as the number one aspect in the patient’s choice of presbyopic correction, patients themselves do not always see it that way.16 Similarly, cost was not seen as a barrier by our participants, nor previously reported to impact discontinuation of contact lens wear in (pre-) presbyopes.23,24 Although expense has been shown to affect contact lens discontinuation,22 this was mainly reported by younger contact lens wearers.
LimitationsParticipants’ recall of receiving information about presbyopia may have affected the accuracy of our results, although efforts were made to reduce the recall period by only including those within the pre- and early presbyopic age range (36–48 years). In addition, the use of focus groups stimulated memories and thoughts through group dynamics, providing an opportunity to reduce recall bias and debate ideas and attitudes prompted either by the facilitator or other members of the focus group.25 This was considered advantageous over self-administered surveys and/ or interviews.
The small sample size with limited demographic representation was also considered a limitation. Although focus groups are expected to be more accurate compared to individual questionnaires or interviews, they are very time-consuming and expensive to run. The methodology described by Guest et al.26 was adopted to identify the full range of primary themes around presbyopia and its preferred visual correction. No new themes were identified during the fourth focus group, which led to a sample of 24 participants. This sample included a wide range of professional backgrounds and choice of visual corrections, as well as a representation of genders, ethnicities, pre- and early presbyopes, and distance refractive errors, albeit too small for sub-analysis. For example, due to its relatively small sample size, this study was not able to conduct a comparison between sexes on the subject of presbyopic correction. Although it is believed that the attitude towards multifocal contact lenses could be similar,27 it is possible that perceptions about presbyopia differ between men and women. This is based on reports of differences between men and women in the prevalence, age of onset, and severity of presbyopia,28 as well in the working distance and arm length and the types of tasks for which men and women use near vision.29
ConclusionsThe need for a reading correction was generally perceived as a sign of age and responses suggested that deterioration in vision is expected with age. Spectacles were the preferred mode of near vision correction. Presbyopia was not a well-known condition overall, and the majority of participants were unaware of exactly what it meant. Most participants indicated that information about presbyopia should be provided by an optometrist in comparison to other health care professionals (e.g. General Practitioner). Furthermore, there were mixed opinions towards the idea of wearing multifocal contact lenses; a positive attitude was mostly driven by the participants’ previously successful contact lens experience. Comfort and convenience were much more important than cost, as long as visually they were comfortable and suitable for their lifestyle.
FundingThe undergraduate student (Brooke Hutchins) was awarded an educational grant from industry sponsor Johnson and Johnson Vision Care Institute, as part of the STEP® Educational Project 2018. The study was designed and undertaken independently from Johnson and Johnson.
Conflicts of interestThe authors have no conflicts of interest to declare.
Part of this work has been presented as a poster at the British Contact Lens Association conference in Manchester (UK) in May 2019.