To compare central corneal swelling after eight hours of sleep in eyes wearing four different silicone hydrogel lenses with three different powers.
MethodsTwenty-nine neophyte subjects wore lotrafilcon A (Dk, 140), balafilcon A (Dk, 91), galyfilcon A (Dk, 60) and senofilcon A (Dk, 103) lenses in powers −3.00, −10.00 and +6.00 D on separate nights, in random order, and on one eye only. The contra-lateral eye (no lens) served as the control. Central corneal thickness was measured using a digital optical pachometer before lens insertion and immediately after lens removal on waking.
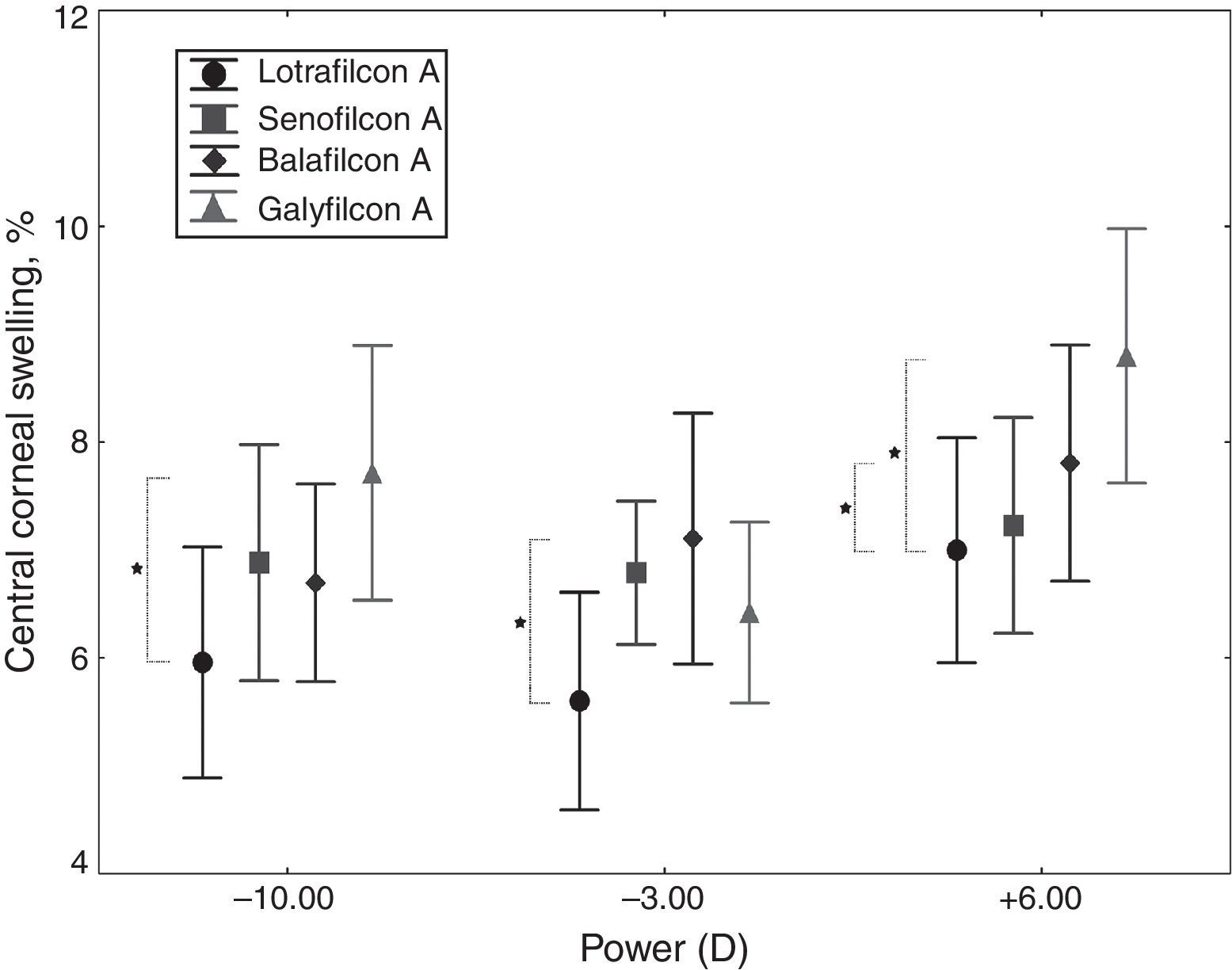
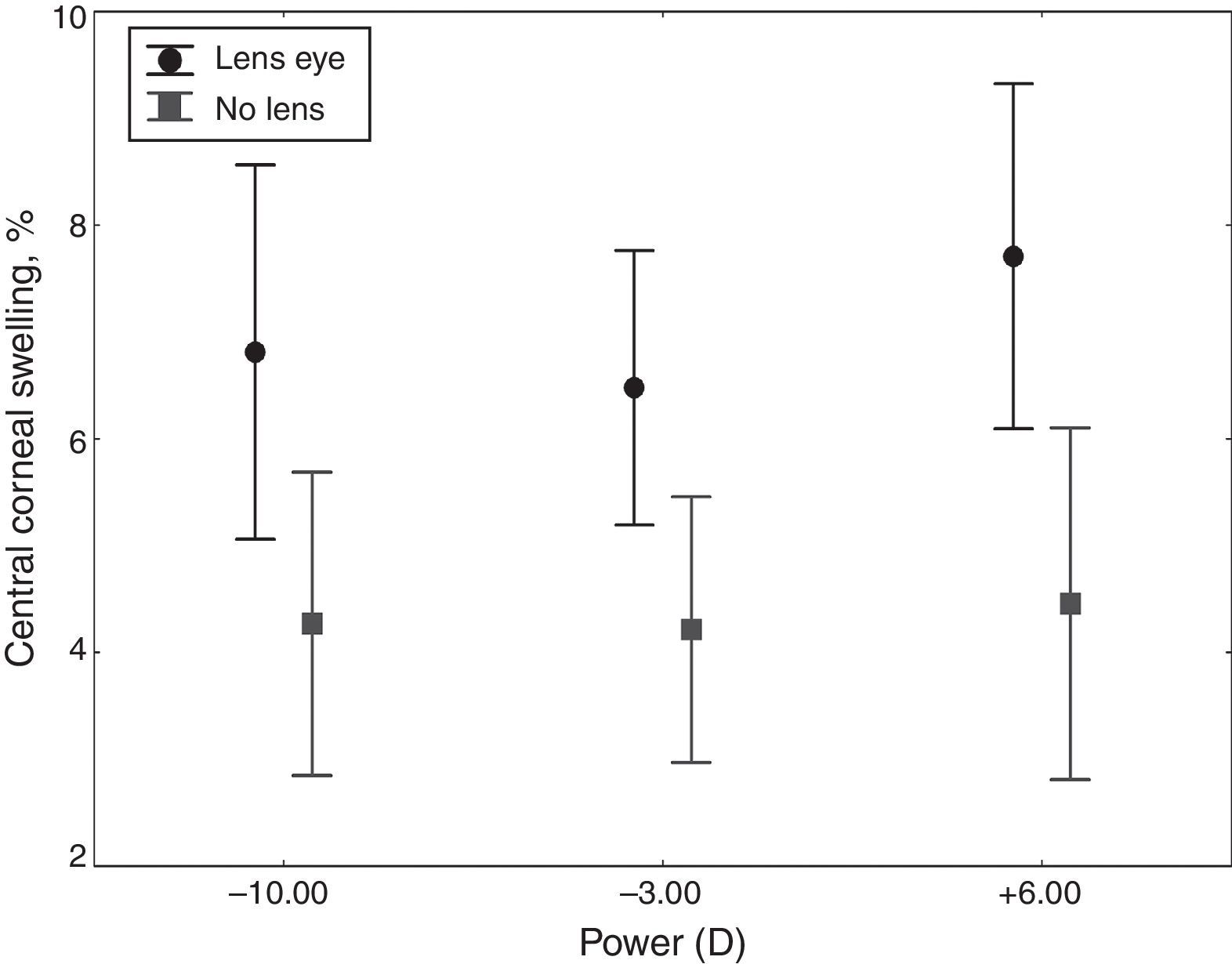
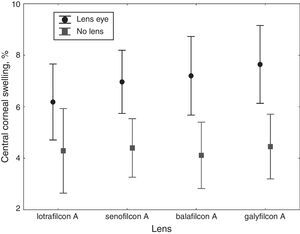
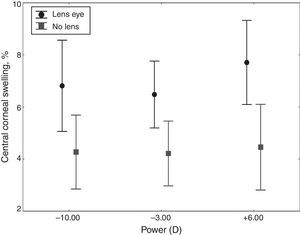
ResultsFor the +6.00 D and −10.00 D, lotrafilcon A induced the least swelling and galyfilcon A the most. The +6.00 D power, averaged across lens materials, induced significantly greater central swelling than the −10.00 and −3.00 D (Re-ANOVA, p<0.001), (7.7±2.9% vs. 6.8±2.8% and 6.5±2.5% respectively) but there was no difference between −10.00 and −3.00 D. Averaged for power, lotrafilcon A induced the least (6.2±2.8%) and galyfilcon A the most (7.6±3.0%) swelling at the center (Re-ANOVA, p<0.001). Central corneal swelling with +6.00 D was significantly greater than −10.00 D lens power despite similar levels of average lens transmissibility of these two lens powers.
ConclusionsThe differences in corneal swelling of the lens wearing eyes are consistent with the differences in oxygen transmission of the silicone hydrogel lenses. In silicone hydrogel lenses central corneal swelling is mainly driven by central lens oxygen transmissibility.
Comparar el edema central de la córnea tras ocho horas de sueño, en ojos con cuatro lentes diferentes de hidrogel de silicona de tres potencias diferentes.
MétodosVeintinueve pacientes no usuarios de lentes de contacto llevaron lentes de lotrafilcon A (Dk, 140), balafilcon A (Dk, 91), galyfilcon A (Dk, 60) y senofilcon A (Dk, 103) con potencias de −3,00, −10,00 y +6.00 D durante noches diferentes, en orden aleatorio, y en un solo ojo. El ojo contra-lateral (sin lente) se utilizó como control. El espesor central de la córnea se midió utilizando un paquímetro óptico digital antes de la inserción e inmediatamente tras la retirada de la lente al despertar.
ResultadosPara +6,00 D y −10,00 D, lotrafilcon A produjo el menor edema, comparado con galyfilcon A. La potencia +6,00 D, promediada en los materiales de las lentes, produjo un edema central considerablemente mayor que las potencias −10,00 y −3,00 D (Re-ANOVA, p<0,001), (7,7±2,9% frente a 6,8±2,8% y 6,5±2,5% respectivamente), pero no existió diferencia entre −10,00 y −3,00 D. Promediando las potencias para cada lente, lotrafilcon A produjo el menor edema en el centro (6,2±2,8%) y galyfilcon A la mayor (7,6±3,0%) (Re-ANOVA, p<0,001). El edema corneal central con +6,00 D fue considerablemente superior que la de la potencia de lente −10,00 D, a pesar de los niveles similares de transmisibilidad media de la lente de estas dos potencias.
ConclusionesLas diferencias en cuanto a edema de la córnea de los ojos portadores de lentes son consistentes con las diferencias en cuanto a transmisión del oxígeno de las lentes de hidrogel de silicona. En las lentes de hidrogel de silicona, el edema corneal central es principalmente debido a la transmisibilidad del oxígeno central de la lente.
Hypoxia induced corneal swelling is a well known phenomenon and one of the primary indices of corneal physiological change during contact lens wear. Holden and Mertz1 hypothesized that the minimum oxygen transmissibility (Dk/t) of a lens should be 87±3.3×10−9 (cmmlO2)/(mlsmmHg) in order to prevent overnight lens induced corneal swelling. More recently, a value of 125×10−9 (cmmlO2)/(mlsmmHg) has been proposed as the critical Dk/t of a lens to prevent lens-induced overnight corneal anoxia.2 Studies have shown that silicone hydrogel lenses induce less corneal swelling compared to conventional hydrogel lenses when worn overnight (Bergenske P, Mueller N, Caroline P, Smythe J, Mai-Le K. Uniformity of overnight corneal swelling with extended wear contact lenses. Optom Vis Sci. 2001;78(12S):198; Bullimore MA, Nguyen M, Bozic J, Mitchell GL. Overnight corneal swelling with 7-day continuous wear of soft contact lenses. ARVO Meeting Abstracts. 2002;43:3100; Fonn D, Moezzi A, Simpson T, Situ P. Confirmation of a yoked corneal swelling response between the test and contralateral control eye. Optom Vis Sci. 2004;81(12S):30).3,4 Although all −3.00 D silicone hydrogel contact lenses meet the Holden and Mertz criterion of 87×10−9 (cmml O2)/(mlsmmHg) for the central lens transmissibility, no one has reported the effect of higher powered silicone hydrogel lenses (decreased Dk/t) on central corneal swelling. Previous corneal swelling studies with silicone hydrogel lenses including a previous study by the current authors5 used low powered silicone hydrogel lenses and compared between the lens types. Although Steffen et al.6 studied overnight swelling with silicone hydrogel lenses in a range of powers between −1.00 to −6.00 D to correct 25 adapted daily soft contact lens wearers it is unclear how many subjects wore higher powered lenses in this dispensing study and they did not compare corneal swelling across lens powers.
Previous studies with conventional hydrogel lenses showed greater central corneal swelling with higher minus lens powers than lower minus powers with the same material, central thickness and central oxygen transmissibility (Dk/t).7–9 Tomlinson and Bibby10 showed that the central corneal swelling in minus powered hydrogel lenses was underestimated and in plus powered lenses was overestimated based on the central lens transmissibility. These findings led to the conclusion that the central lens transmissibility is a poor predictor of the magnitude of central corneal swelling and the response is influenced by the averaging of the lens oxygen transmission.7,10–14 To our knowledge no one appears to have investigated the influence of local central compared to average Dk/t of silicone hydrogel lenses to determine the primary driver of overnight central corneal swelling with these lenses.
The main aims of this study were to compare differences in central corneal swelling between different silicone hydrogel lens materials in high and low powered lenses and to determine if at high levels of oxygen transmissibility central corneal swelling with silicone hydrogel lenses can still be differentiated. In addition, this study aimed to investigate whether central corneal swelling is primarily driven by central or average lens transmissibility. Therefore, we compared central overnight corneal swelling induced by four different silicone hydrogel lenses with three different powers and tested the following null hypotheses:
- 1)
There are no statistically significant differences in central corneal swelling between the lens types for each lens power.
- 2)
There are no statistically significant differences in overall central corneal swelling between the 4 lens types.
- 3)
There are no statistically significant differences in overall central corneal swelling between the 3 lens powers.
- 4)
Average oxygen lens transmissibility is not the main driver of central corneal swelling in silicone hydrogel lenses.
Distribution of central corneal swelling across subjects from this study has been published15 showing that both the lens-wearing and control eyes followed a normal curve. This validates the use of parametric statistics for data analysis and the use of mean values to represent the central tendency of the data in this paper.
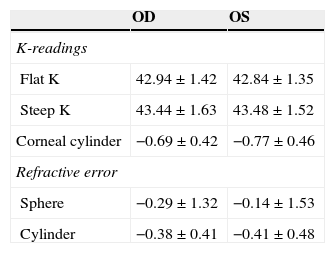
Materials and methodsSubjectsThis was a non-dispensing, randomized and double-masked study. Based on the data from previous corneal swelling studies at the Center for Contact Lens Research (CCLR), 26 subjects were required to detect a 0.8±1.2% difference in central corneal swelling with a power of 0.90 at ¿=0.05. In this study 37 neophytes were enrolled and 29 completed the study (14 female, 15 male). Eight subjects chose to discontinue from the study for personal reasons (relocation, finding a new job, etc.) before completing all follow-up visits. Only the data from the subjects who completed all study visits were included for data analysis. The mean age of the subjects was 27.1±7.9 years (median 25 years, ranging from 17 to 50 years). Every subject wore each of the 12 lenses according to a randomization table. Table 1 summarizes the refractive characteristics of the subjects enrolled in the study. Ethics approval was obtained from the Office of Human Research Ethics, University of Waterloo, and informed consent was obtained for each subject prior to enrolment in the study. All subjects were treated in accordance with the tenets of the Declaration of Helsinki.
Instrumentation and lensesCorneal thickness of each eye was measured using a computerized digital optical pachometer mounted on a Zeiss 30 SL-M biomicroscope. To enhance precision for obtaining the corneal thickness measurement at each time point, seven consecutive measurements were taken and the highest and the lowest readings were excluded by the instrument's custom software. The average of the remaining five measures was the recorded value of the corneal thickness provided that the standard deviation of these five measurements did not exceed 5¿m, otherwise the measurement of that time point was repeated.
Corneal swelling was derived from the percentage difference in corneal thickness compared with the baseline measurements using the following formula
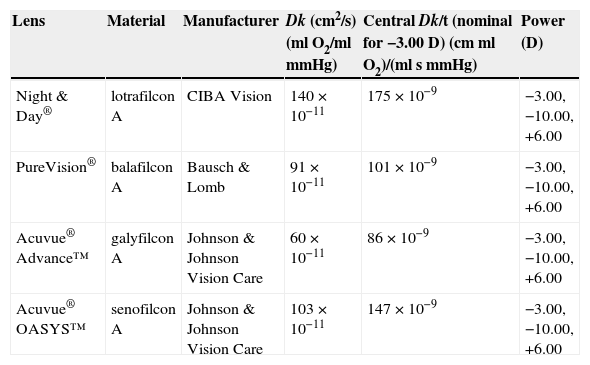
The parameters of the lenses used during the study are presented in Table 2.
Lens parameters.
| Lens | Material | Manufacturer | Dk (cm2/s) (mlO2/mlmmHg) | Central Dk/t (nominal for −3.00 D) (cm ml O2)/(ml s mmHg) | Power (D) |
|---|---|---|---|---|---|
| Night & Day® | lotrafilcon A | CIBA Vision | 140×10−11 | 175×10−9 | −3.00, −10.00, +6.00 |
| PureVision® | balafilcon A | Bausch & Lomb | 91×10−11 | 101×10−9 | −3.00, −10.00, +6.00 |
| Acuvue® Advance™ | galyfilcon A | Johnson & Johnson Vision Care | 60×10−11 | 86×10−9 | −3.00, −10.00, +6.00 |
| Acuvue® OASYS™ | senofilcon A | Johnson & Johnson Vision Care | 103×10−11 | 147×10−9 | −3.00, −10.00, +6.00 |
Central lens thickness was measured (masked for lens type and power) using a digital lens thickness gauge (Rehder Development Company, Castro Valley, CA, USA). This measurement was conducted on a random sample of the study contact lenses (i.e. 20% of lenses) worn by the subjects after lens removal. For each lens power central transmissibility was calculated using the following formula:
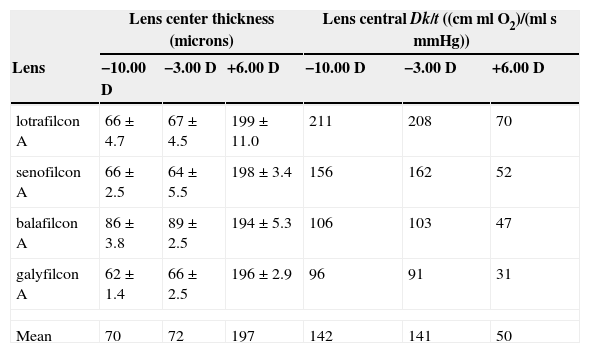
The measured central thickness and calculated Dk/t values are recorded in Table 3.
Central thickness (mean±SD) and transmissibility by lens and power.
| Lens center thickness (microns) | Lens central Dk/t ((cmml O2)/(mlsmmHg)) | |||||
|---|---|---|---|---|---|---|
| Lens | −10.00 D | −3.00 D | +6.00 D | −10.00 D | −3.00 D | +6.00 D |
| lotrafilcon A | 66±4.7 | 67±4.5 | 199±11.0 | 211 | 208 | 70 |
| senofilcon A | 66±2.5 | 64±5.5 | 198±3.4 | 156 | 162 | 52 |
| balafilcon A | 86±3.8 | 89±2.5 | 194±5.3 | 106 | 103 | 47 |
| galyfilcon A | 62±1.4 | 66±2.5 | 196±2.9 | 96 | 91 | 31 |
| Mean | 70 | 72 | 197 | 142 | 141 | 50 |
In this study harmonic average lens thickness over a cord diameter of 6.8mm10 for each lens was computed using the software by Douthwaite.16 Harmonic average lens transmissibility values were calculated by applying manufacturers’ quoted lens permeability values to these data using the following formula:
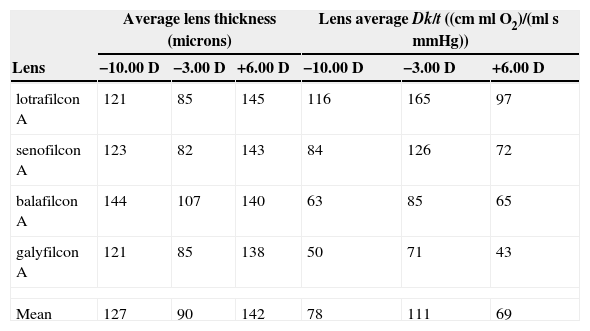
The computed harmonic average lens thickness and calculated harmonic average Dk/t values are recorded in Table 4.
Computed harmonic average thickness and average lens transmissibility by lens and power for 6.8mm cord diameter.
| Average lens thickness (microns) | Lens average Dk/t ((cmmlO2)/(mlsmmHg)) | |||||
|---|---|---|---|---|---|---|
| Lens | −10.00 D | −3.00 D | +6.00 D | −10.00 D | −3.00 D | +6.00 D |
| lotrafilcon A | 121 | 85 | 145 | 116 | 165 | 97 |
| senofilcon A | 123 | 82 | 143 | 84 | 126 | 72 |
| balafilcon A | 144 | 107 | 140 | 63 | 85 | 65 |
| galyfilcon A | 121 | 85 | 138 | 50 | 71 | 43 |
| Mean | 127 | 90 | 142 | 78 | 111 | 69 |
For each overnight period one of the study lenses was placed on one eye (according to a randomization table) in the evening, prior to sleep. Subjects were then carefully examined to ensure that the lenses were fitting properly, such that there were no debris trapped between the lens and the cornea and the lens was comfortable. The following morning subjects were woken at 7am to remove the lens. Immediately after removal, subjects were escorted to the exam room with their eyes closed. Corneal thickness of each eye was measured immediately after eye opening, after the subjects were comfortably seated at the optical pachometer. Each measurement was then repeated on both eyes every 20min over the first hour after eye opening and every hour for the subsequent two hours.
Central corneal thickness in both lens wearing and control eyes was measured using a modified optical pachometer interfaced to a PC. The anterior segment was examined with a slit lamp biomicroscope (with and without the instillation of fluorescein) for safety purposes after the last measurement.
Data analysisDescriptive statistics were generated for all variables. The effects of lens type and lens power were examined. p-Values of less than 0.05 were considered to be statistically significant. Repeated measures analysis of variance (Re-ANOVA) was used to examine the effect of lens type (lotrafilcon A, senofilcon A, balafilcon A and galyfilcon A) and lens power (−3.00, −10.00 and +6.00 D). When appropriate the Huynh–Feldt (HF) correction was applied to adjust the p values and the HF corrected p values are reported in this paper. For each lens power, to compare the effect of lens type, a separate Re-ANOVA was conducted. Tukey HSD Post hoc tests were used to determine the significance of all pair-wise differences.
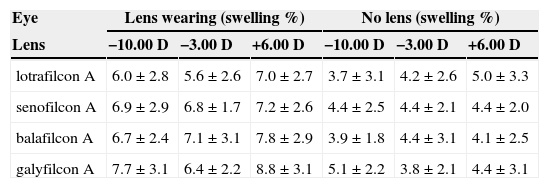
ResultsThe results of the central corneal swelling for all lens types and powers are shown in Table 5.
Mean (± SD) overnight central corneal swelling.
| Eye | Lens wearing (swelling %) | No lens (swelling %) | ||||
|---|---|---|---|---|---|---|
| Lens | −10.00 D | −3.00 D | +6.00 D | −10.00 D | −3.00 D | +6.00 D |
| lotrafilcon A | 6.0±2.8 | 5.6±2.6 | 7.0±2.7 | 3.7±3.1 | 4.2±2.6 | 5.0±3.3 |
| senofilcon A | 6.9±2.9 | 6.8±1.7 | 7.2±2.6 | 4.4±2.5 | 4.4±2.1 | 4.4±2.0 |
| balafilcon A | 6.7±2.4 | 7.1±3.1 | 7.8±2.9 | 3.9±1.8 | 4.4±3.1 | 4.1±2.5 |
| galyfilcon A | 7.7±3.1 | 6.4±2.2 | 8.8±3.1 | 5.1±2.2 | 3.8±2.1 | 4.4±3.1 |
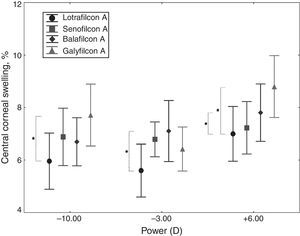
Overnight central corneal swelling for each lens type with each lens power is shown in Fig. 1. For each lens power in Fig. 1, there was a statistically significant effect of lens type (Re-ANOVA, pHF<0.05 for all). The +6.00 D galyfilcon A lens induced greater corneal swelling than lotrafilcon A and senofilcon A (post hoc tests; p<0.05 for both), but was not different than balafilcon A (post hoc test; p>0.05). The −10.00 D lens also induced greater swelling with the galyfilcon A than lotrafilcon A (post hoc test; p<0.05), but not than the other two lenses (post hoc tests; p>0.05 for both). With −3.00 D lens, swelling induced by balafilcon A was greater than lotrafilcon A (post hoc test; p<0.05), but was not different than the other two lenses (post hoc tests; p>0.05 for both).
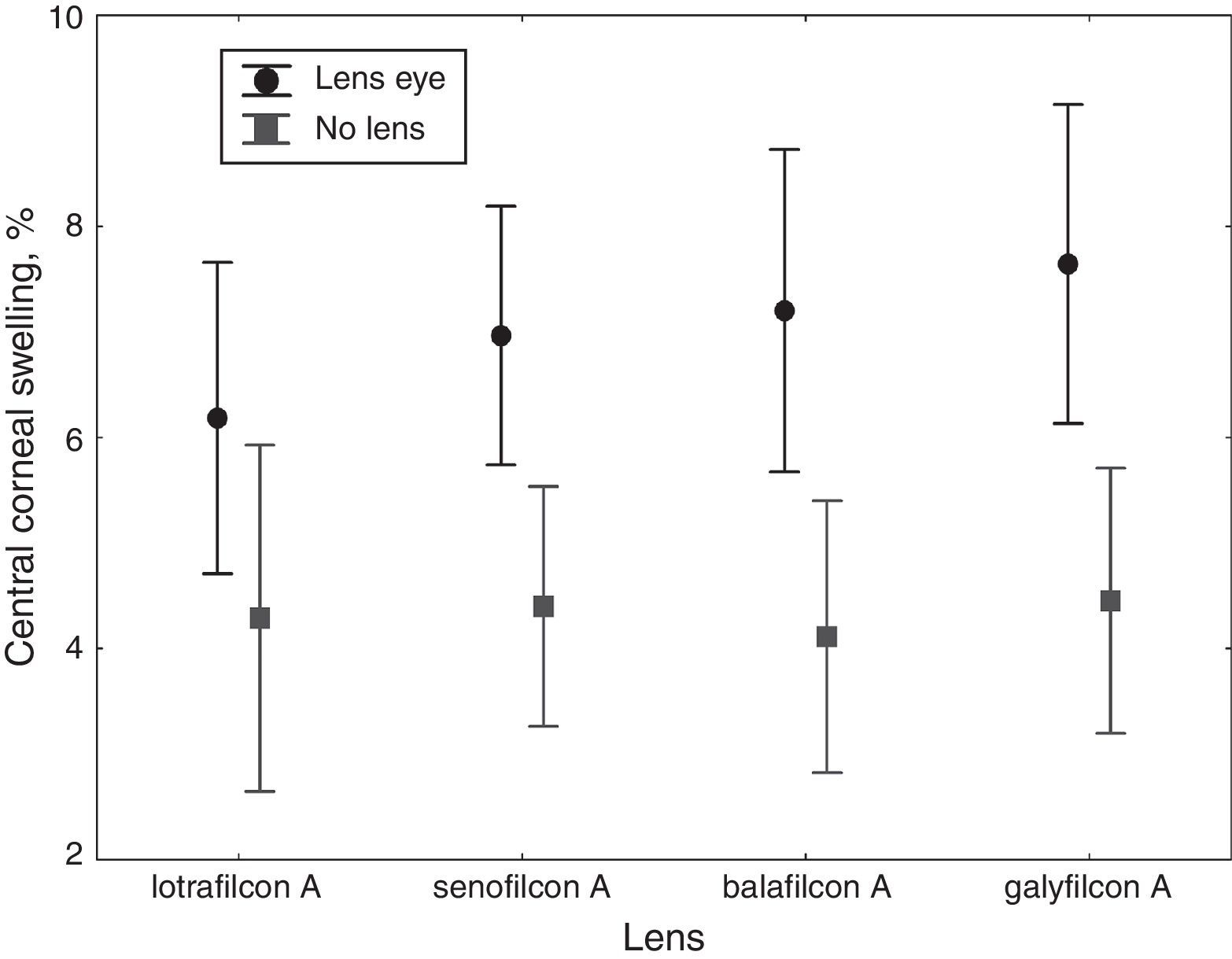
Effect of lens type on central corneal swellingAveraged for power, there was a significant effect of lens type (Re-ANOVA, pH-F<0.001) lotrafilcon A induced the least (6.2±2.8%) and galyfilcon A the most central corneal swelling (7.6±3.0%) (post hoc tests; p<0.05). There was no difference between galyfilcon A, balafilcon A and senofilcon A, and between lotrafilcon A and senofilcon A (post hoc tests; p>0.05). Immediately after lens removal, all lenses induced significantly more central corneal swelling than their respective controls (all post hoc tests; p<0.05) (Fig. 2).
Effect of lens power on central corneal swellingThere was a significant effect of lens power on central corneal swelling (Re-ANOVA; pH-F<0.001) as illustrated in Fig. 3. The +6.00 D power, averaged across lens materials, induced significantly greater central swelling than the −10.00 and −3.00 D (post hoc tests; p<0.05 for both), (7.7±2.9 vs. 6.8±2.8 and 6.5±2.5% respectively) but there was no difference between −10.00 and −3.00 D (post hoc test; p>0.05) (Fig. 3).
Computed central and harmonic average lens transmissibilityThe central lens thickness measurements and respective calculated central oxygen transmissibility values (from the permeability values provided by the lens manufacturers) of each lens type and computed values of harmonic average lens thickness and average lens transmissibility over 6.8mm cord diameter are shown in Tables 3 and 4 respectively. For each lens type as expected and can be seen from these tables the central lens transmissibility of high and low minus powered lenses were similar and both were markedly different than the central Dk/t in plus lens power (Table 3). In contrast, harmonic average lens transmissibility values in high powered plus and minus lenses were similar and notably different than harmonic average Dk/t in −3.00 D lens (Table 4).
DiscussionIn this study we used 12 different silicone hydrogel lenses with central oxygen transmissibility values ranging from 31 to 211×10−9 (cmml O2)/(mlsmmHg). Central corneal swelling differences between the lens types were particularly pronounced in high powered lenses and are clearly seen in both +6.00 D and −10.00 D lens powers in Fig. 1, suggesting that the corneal swelling response especially in the higher lens powers may be minimized by using silicone hydrogel lenses in the higher transmission end. These results are consistent with the difference in the calculated central oxygen transmission values between the silicone hydrogel lenses shown in Table 3 and show that at high levels of Dk/t, central corneal swelling with silicone hydrogel lenses can still be differentiated based on the lens oxygen transmissibility. The exception to this statement was galyfilcon A which did not induce the most swelling among lenses in −3.00 D power (Fig. 1) as would be predicted from the other lens power results in this study and other published work (Moezzi AM, Fonn D, Simpson TL. Comparison of overnight corneal swelling induced by prototype lotrafilcon A toric versus balafilcon A toric. American Academy of Optometry Meeting Abstract. 2006:060095).17,18 This can be attributed to sampling or perhaps other possible uncontrolled lens specific or ocular surface related factors which may have influenced the corneal swelling response in addition to lens Dk/t warranting further investigation in future studies. The small but significant differences in central corneal swelling between the study lenses in each high powered group (i.e. −10.00 or +6.00) (Fig. 1) are probably not clinically relevant. However, some subjects exhibited high levels of corneal swelling as we reported previously15 and for those it would seem sensible to use the lenses that cause the least amount of swelling.
Fig. 2 demonstrates an inverse relationship between oxygen transmissibility and mean overnight central corneal swelling induced by the silicone hydrogel study lenses. Also, this figure illustrates that with all study lenses, the lens wearing eye showed significantly more swelling than in the contralateral non-lens wearing eye as shown previously,4,5 (Fonn D, Moezzi A, Simpson T, Situ P. Confirmation of a yoked corneal swelling response between the test and contralateral control eye. Optom Vis Sci. 2004;81(12S):30) suggesting that even lenses that exceed the Holden and Mertz 87×10−9 (cmml O2)/(mlsmmHg)1 will not avoid overnight lens induced edema (Table 5). The additional swelling produced by the lens compared to the same closed eye condition without the lens has been partially attributed to lens-related corneal swelling factors other than hypoxia.19–25
Despite differences in thickness of the central and peripheral cornea there are similar oxygen demands across the cornea, independent of corneal location.26 Even after blinking, the effect of tear mixing to equilibrate the oxygen tension under a soft lens is insignificant.27 To maintain normal corneal physiology and health, it is important that high powered soft contact lenses provide sufficient local oxygen transmissibility through the thickest part of the lens.2,28–30 Bruce29 compared local Dk/t measurements of spherical lotrafilcon A and balafilcon A lenses of various powers and found that lotrafilcon A exceeded the Holden and Mertz criterion of 87×10−9(cmml O2)/(mlsmmHg) at all lens locations in the range of +3.00 to −6.00 powers, however only balafilcon A of +1.00 D power met this criterion across the lens. In our study none of the plus powered lenses met the minimum Dk/t of 87×10−9 (cmml O2)/(mlsmmHg) at the center as the highest central Dk/t was 70×10−9 (cmml O2)/(mlsmmHg) with +6.00 D lotrafilcon A (Table 3). All minus powered lenses in this study meet or exceed the Holden and Mertz criterion for extended wear at the center (Table 3).
Previous studies with conventional hydrogel lenses under closed eye conditions showed greater central corneal swelling with higher minus lens power but the same center thickness as the lower power lenses, and similar levels of central corneal swelling with minus compared to plus hydrogel lenses. This was despite greater central thickness and therefore lower central Dk/t of plus lens powers. These findings were explained by assuming that average of the central area of the lens instead of local central lens transmissibility was responsible.7,10–14 However, findings from these previous studies with hydrogel lenses are at odds with results from our study with silicone hydrogel lenses (Fig. 3).
For the ease of illustration, the mean values of central and average lens transmissibility for each lens power are shown in the right side of the last rows in Tables 3 and 4 respectively. Central corneal swelling with +6.00 D was significantly greater than −10.00 D lens power (Fig. 3) despite similar levels of average lens transmissibility of these two lens powers (Table 4, last row). However, central oxygen transmissibility in +6.00 D was significantly lower than −10.00 D lens power as shown in Table 3 and this is in line with the higher central corneal swelling induced by +6.00 D lenses in this study. Therefore, the greater central swelling induced by +6.00 D compared to the −10.00 D and −3.00 D in Fig. 3 can be explained by the lower central oxygen transmission of the plus lens power. Also central corneal swelling induced by −10.00 and −3.00 D lens powers in Fig. 3 were not significantly different despite obvious differences in average lens transmissibility between high and low minus lens powers (Table 4, last row). In contrast, the similar level of central corneal swelling induced by −10.00 D and −3.00 D lens powers (Fig. 3) can be easily predicted from the similarity in central lens transmissibility between these two lens powers as shown in Table 3 (last row). A correlation analysis (that was not statistically significant as only three pairs of data were compared) showed a very strong linear association between central corneal swelling and central lens Dk/t (r2=0.94) and a weaker association between the central corneal swelling and average lens transmissibility (r2=0.68). Therefore, these findings from our study suggest that in silicone hydrogel lenses central corneal swelling is mainly driven by central lens oxygen transmissibility. Average oxygen transmissibility is less likely to primarily affect the outcome here and a likely reason was that these lenses were in the high transmissibility range. These results are in agreement with a suggestion from at least one previous study which predicted a more prominent role for the effect of local oxygen transmissibility, rather than the averaging effect in higher transmissible hydrogel lenses.14
FundingThis study was supported by a grant from CIBA Vision USA, Duluth, GA, and in part by a COETF grant.
Conflicts of interestProfessor Desmond Fonn is a consultant for Alcon Laboratories and CooperVision Inc. None of the other authors of this manuscript have any potential financial interest in a product reported in the manuscript.
We thank Dr. Craig Woods, Dr John McNally and Ms. Alisa Sivak for their helpful comments. We also thank Dr. Sarah Guthrie for providing lens thickness measurements.
A summary of this work was presented as two posters at the American Academy of Optometry annual meeting, October 2008, Anaheim, CA.