This study aimed to evaluate the refractive error of the uncooperative infants and children with the new method of retinoscopy called the tele-lens (“Mirza”) retinoscopy.
MethodsIn the “Mirza” tele-lens retinoscopy, the examiner placed the trial lenses in 1/3 distance between the tested eye person and peephole of the retinoscope (22.2 cm far from the spectacle plane). First, the optical calculations were done to find the correction factors for this new method of retinoscopy. Second, the dry standard and “Mirza” tele-lens retinoscopy were performed in 78 eyes from 39 children aged 7–12 years with good cooperation and next, the procedure was repeated using cyclopentolate drops and then the results of the two methods were compared, and at the end, the dry “Mirza” tele-lens retinoscopy was done in the 60 eyes of 31 uncooperative infants with a mean age of 21.85 ± 8.79 months for evaluating the feasibility of the “Mirza” tele-lens retinoscopy procedure. The intraclass correlation coefficient (ICC) and Bland–Altman plot for assessment of agreement between the findings of two retinoscopic methods in dry and cyclo conditions were used.
ResultsThe comparison between the dry standard and “Mirza” tele-lens retinoscopic results with means of 1.39 ± 1.43 and1.36 ± 1.39, respectively were not statistically significant (p > 0.05). Besides, comparing the mean cycloplegic results of two methods (standard vs. “Mirza” tele-lens), the difference was not statistically significant (2.37 ± 1.44 vs. 2.41 ± 1.37) (p > 0.05). Moreover, Two-way repeated measures ANOVA revealed no significant retinoscopy method × use of drops interaction (P = 0.103) in comparing two methods of the standard and “Mirza” tele-lens retinoscopy. ICC results indicated high agreement between two methods in both dry (ICC = 0.993) and cyclo (ICC = 0.989) conditions.
ConclusionsThe “Mirza” tele-lens retinoscopy method can be performed with satisfactory results in infants and children who do not cooperate for the standard procedure of measuring the refractive errors.
Detection, assessment, and management of refractive errors in children are of great importance, as this ability is a fundamental clinical skill among optometrists.1 Being aware of the refractive status of the child timely and its appropriate correction are important to reduce the incidence of the amblyopia, the costs of visual rehabilitation and ultimately reduce the health and social costs of the community.2 Accordingly, children in the early years of life need comprehensive eye examinations due to the probable presence of amblyopia, strabismus, significant refractive error or other factors affecting the reduction of visual acuity.3
In most cases, evaluation of refractive error in infants and young children through routine adult procedures, such as standard retinoscopy and autorefraction, is associated with problems due to the excessive activity of the accommodative system, lack of long-term fixation at a particular point, and the failure to cooperate for various reasons,4,5 so applying these methods may not lead to optimal results. Accordingly, different researchers have proposed methods for better and more reliable results, such as, cycloplegic refraction in high hyperopia with greater accommodative efforts,6 and Mohindra’s method in children who look at the light of a retinoscope during refraction,7 each in turn eliminating some of the problems associated with the evaluation of children’s refraction, but the problem does not end with this kind of non-cooperation. Some young children, mentally retarded children, and infants may become anxious and frightened by approaching and placing the trial lens on the spectacle plane and may begin to develop inadequacy, crying, and inaction.8,9 Better cooperation between the examiner and child in the retinoscopic process will be formd due to the emotional relationship between parents and children. Infants and young children may feel less anxious when they are physically close to their parents and this brings the most comfort to children. In these cases, if a trial lens is placed farther away (the Tele-Lens) from the spectacle plane, the optical reflex can be seen through retinoscope as a reflection from the retina, and eventually, the child’s refractive status is evaluated without disturbing the child. Can the results of this Tele-Lens retinoscopy be trusted and applied?
This study aimed to introduce a new retinoscopy method called the “Mirza” tele-lens retinoscopy for evaluation of refractive error in uncooperative infants and children and to compare it with standard retinoscopy.
Materials and methodsThe introduction of the “Mirza” tele-lens retinoscopy as the topic of this study requires firstly to determine the correct location of the trial lens for retinoscopy. As the lens moves away from the patient’s faceplate, the problem of lens disturbance for the child is reduced and eliminated. The clinical experience of the authors has shown that an approximate distance of 20 cm far from the faceplate is sufficient enough to eliminate the reactive behaviors of child, which are relative to the object located near the face. On the other hand, given that the usual working distance in the standard retinoscopy procedure is often 66.6 cm10,11 if the child’s spectacle plane departs from as much as 1/3 of this distance, a point will be created that is 22.2 cm from the child’s spectacle plane and 44.4 cm away from the peephole of the retinoscope (Fig. 1).
The “Mirza” tele-lens and standard retinoscopy. In A, the child’s reaction to approaching the trial lens in standard retinoscopy procedure was showed. In B, the trial lens magnification from its position farther from the spectacle plate was illustrated. In C, the “Mirza” tele-lens retinoscopy was performed by placing the trial lens at 22.2 cm far from the child’s spectacle plane.
This point has two features that help to select the optimal distance for refraction. First, this point is sufficiently far from the patient’s spectacle plane to eliminate the child’s reactive behaviors to the trial lens. Secondly, given that the lens is about 1/3 the distance between the child’s eye and the peephole of the retinoscope, evaluation of a child’s refractive error is easily obtainable by a skilled optometrist during retinoscopy despite optical changes in retinoscopic reflex.
Optics of retinoscopy with a distant lens should now be assessed. It is worth mentioning that for some reasons, choosing a distance of 1/3 would be better:
First of all, it would be easier to consider this distance than other distances because it divides the usual distance for standard retinoscopy (66.6 cm) into three parts of equal size.
Secondly, based on the author’s experiences in using this method, it has been observed that by reducing the distance and getting closer to the patient, retinoscopy will be difficult due to the lack of necessary cooperation. Also, moving away from a distance of 1/3 will make it more difficult to see the retinoscopic reflex and increase optical errors.
The study protocol was approved by the institutional review board of the Iran University of Medical Sciences and the Steering Committees of the School of Rehabilitation Sciences and conformed with the tenets of the Declaration of Helsinki. The informed consent was obtained for experimentation with human subjects from All subject’s parents.
OpticsIn the emmetropic eye, the reflective light beams of the retina after exiting the pupil will be parallel (with no vergence power), so for observation of the focused beams on the peephole of the retinoscope and neutral point, a positive lens with a focal length equal to the distance between the peephole and the spectacle plane is needed to be placed in front of the patient’s eye on the spectacle plane. The lens should have a power of +1.50 D for this working distance of 66.7 cm.
According to the above explanation, the lens equation can be used to calculate the lens working distance required for the retinoscopic procedure.
According to the lens equation 1/f = (1/p) + (1/q) (Eq. (1)), p is the object distance, q is the image distance and f defines the focal length of the lens.
In myopia, the far point is at the front of the eye, and in hyperopia, this point is at the behind of the eye. So the p and q values in the “Mirza” tele-lens method were determined as follows (1) and (2):
(1) for hyperopia;
and
(2) for myopia;
where p1 is the distance of the far point from the spectacle plane, p2 is the distance of far point from the trial lens placement in the “Mirza” tele-lens retinoscopy (22.2 cm), q1 is the distance of spectacle plane from the peephole of the retinoscope, and q2 is the distance of the peephole of the retinoscope from the trial lens placement in the “Mirza” tele-lens retinoscopy (22.2 cm).Given that the trial lens distance to the peephole of the retinoscope (q) is equal to 66.7 cm (0.667 m) and the object distance (p) for the emmetropic eye is an infinite distance (∞), therefore 1/f can be calculated as follow;
In the “Mirza” tele-lens retinoscopy, it is assumed that the trial lens is 22.2 cm far from the spectacle plane, so its distance from the peephole of the retinoscope is 44.4 cm (66.7–22.2). Given that the 1/p is equal to 0 and q is equal to 44.4 cm, so according to equation 1, 1/f can be calculated as +2.25 D.
Here it is quite clear that if the eye is an emmetrope one, a working distance lens of +2.25 D is required to reach the neutral point, or in other words, if a neutral point is obtained with a +2.25 lens in the “Mirza” tele-lens retinoscopy (tele-lens power = +2.25D), the eye is emmetropic and will be a Plano refractive state (net retinoscopy = Plano).
When the tele-lens power is equal to +4.50 D, the standard net retinoscopy value will be the same power, i.e. + 4.50 D. This value is a key point in the “Mirza” tele-lens retinoscopy method so that the values of hypermetropia less than 4.50 D require a trial lens with power more than the amount of true hyperopia to achieve a neutral point in the “Mirza” tele-lens retinoscopy while in 4.50 D of hypermetropia, the tele-lens power is equal to the value of net retinoscopy and in the spectacle plane hyperopia greater than 4.50 D, the tele-lens power is lower than the net value of retinoscopy.
When the patient has 4.50 D of hyperopia, the vergence of light at the spectacle plane is −4.50 D, so we need a +4.50 D to make the vergence of light becomes zero at this point, and also we need a +1.50 D to focus the light at 66.6 cm in the peephole of retinoscope and see the neutral point. This will require a total of the trial lens value of +6.00 D for neutralization at the spectacle plane.
In “Mirza” tele-lens retinoscopy, because the trial lens is located at 22.2 cm far from the spectacle plane, the light vergence in spectacle plane will be −4.50 D and when it reaches to 22.2 cm far from the spectacle plane, the vergence of light will be −2.25 D, so we will require +2.25 D to make the vergence of light becomes zero at this point. On the other hand, to reach the peephole of retinoscope, which is 44.4 cm far from the trial lens, we will need another +2.25 D to focus the light at this point, so in total, the lens required for neutralization is +4.50 D same as in standard net retinoscopy.
The same procedure can be used to calculate the lens required to reach a neutral point for different values of refractive errors from myopia less than 1.50 D to Plano and then to different values of hypermetropia in this new method of retinoscopy. As it is clear from the description, this method requires conversion or correcting table to convert the tele-lens power to net standard retinoscopy (refractive error values) for different amounts of refraction as the table used in the conversion of the power of spectacle refraction to the initial contact lens.
ApplicationAfter performing the optical calculation as described in the preceding section and estimating the power of the lenses required to reach the neutral point in the “Mirza” tele-lens retinoscopy, to test the trial lens at neutrality during the retinoscopic procedure, the retinoscopic methods were firstly performed in the eyes of older children with good cooperation to reduce the possible procedure errors and finally in younger uncooperative children and infants to evaluate the applicability of this new method.
It should be noted that all retinoscopy procedures performed with the Heine Beta 200 streak retinoscope (HEINE Optotechnik, Herrsching, Germany) in the present study. In the early days of beginning the “Mirza” tele-lens retinoscopic procedure, to facilitate the maintenance of the correct working distance, a string with an effective length of 44.4 cm was used, one end of which was attached to the retinoscope handle at a distance of 66.6, and the other end was placed at a distance of 22.2 cm from the corneal plane that was hooked to the examiner’s finger. Also, room lighting is provided by three ceiling incandescent lamps that can be adjusted with the help of existing rheostats. To begin the retinoscopic process, room illumination is reduced to dim light conditions.
Retinoscopy in the eyes of older children with good cooperationAt first, the dry standard retinoscopy was performed in 78 eyes from 39 children aged 7–12 years with good cooperation. Then, the refractive errors of the same children were estimated through the dry “Mirza” tele-lens retinoscopy. The children were watching a cartoon at a distance of 6 m in chart projector (SC-2000 Nidek Instruments, Gamagori, Japan), or watching his parents standing in the same distance and talking to his or her, or a combination of the two during the implementation of any of the retinoscopic methods.
During the “Mirza” tele-lens retinoscopy, the optometrist held the corrective lens at a 1/3 of the standard distance of 66.7 cm (22.2 cm) and performed the neutralization procedure on two meridians using the sphere-sphere method and reported the obtained values as a tele-lens power result regardless of the correction factor or the working distance lens. It is worth mentioning that the data were collected from children over several sessions in several days so that 4–8 children were examined at each session on a specific day. Initially, the standard retinoscopy was performed on all children at a session on a specific day, and the results were recorded on an independent examination datasheet. Then, after completing the standard retinoscopy procedure for all the children over sessions, the “Mirza” tele-lens retinoscopy was performed on the children who were present on the same day and the results were recorded on another independent examination datasheet. For this reason, the children’s refractive errors resulting from the standard retinoscopy method don’t remain in the memory of the examiner. Also, unlike the Mohindra’s retinoscopy and standard method, there is no single fixed value to reduce the tele-lens power amounts for obtaining net retinoscopic values and even the authors of this article, who have been skilled in doing this new method for a long time, have to refer to the correction/conversion table to find the net values. In addition, reasons such as independent registration sheets of the “Mirza” tele-lens and standard retinoscopic results, the number and variety of children in terms of refractive error, the variety of results conversion factors between the two methods for different values of refractive errors and the urgent need for the results conversion table, eliminate the bias of refractive error values in the next stage of retinoscopy.
After completing the dry refraction, one drop of topical 1.0% cyclopentolate was administered to each eye twice with a 5-min interval to perform the standard and the “Mirza” tele-lens cycloplegic refraction 30 min after the last distillation. It is worth noting that in the presence of astigmatism, it is better to use the sphere-sphere method to neutralize any meridian to make easier the performance of this procedure at a distance of 22.2 cm.
The purpose of this session was to assess the method on the eyes of children who had good and appropriate cooperation to avoid or reduce the possible errors due to the non-cooperation of the child, then the applicability of the method was assessed in terms the lens placement at a distance of 22.2 cm, observation of the retinoscopic reflex and its motion, evaluation of the reflex motion in two different principal meridians (in cases of astigmatism) and so on in this situation.
To prevent and reduce the errors caused by daily changes in the ametropia in infants and young children, all refractive error measurements of one child were taken in one day and two methods of standard and “Mirza” tele-lens retinoscopy with and without cycloplegic agent were applied from one to three hours’ interval to prevent the optical and bias effects of one method on the results of the other. Due to the required time for the distillation of cyclopentolate drops and preparation of the child for the minimum necessary cooperation to perform the retinoscopic process, at least one-hour interval was applied between dry and cyclo retinoscopic procedures. In the time between the standard and “Mirza” tele-lens retinoscopy, the child was playing outside the examination environment in the kindergarten area next to the Rehabilitation School of Iran University of Medical Sciences to prevent the child from getting tired and prepare her/him for continuing retinoscopy procedures.
Retinoscopy in the eyes of younger uncooperative children and infantsThis time it was necessary to evaluate the ability of the method in the eyes of younger children and infants who did not cooperate well during the retinoscopy procedure and avoid having the trial lens approaching the eye. An attempt was made to perform the dry and cycloplegic “Mirza” tele-lens retinoscopy on the 68 eyes of 34 infants aged 8–37 months. 34 children participated in this section, and the “Mirza” tele-lens retinoscopy did not apply to three children due to the continuing lack of cooperation, so the new method was performed on only 31 children. Given the lack of cooperation of the infants in the standard retinoscopy procedure, the use of opportunities that these children were looking at the distance target to perform the retinoscopy and viewing its reflex was a priority for an expert optometrist to complete the neutralization procedure.
The procedure was performed in the same detail as previously described for retinoscopy in the eyes of cooperative older children with the “Mirza” tele-lens retinoscopy procedure and all other essentials of the “Mirza” tele-lens retinoscopy were considered.
The aim of the “Mirza” tele-lens retinoscopy method in younger uncooperative children and infants was to evaluate the feasibility of the method on the target age group only, and since the target group did not allow the standard retinoscopy, standard routine retinoscopy was not performed in this age group.
Data analysesThe dry and cycloplegic results of the two methods were compared by paired t-test. Also, the intraclass correlation coefficient (ICC) between the net results of the dry and cycloplegic “Mirza” tele-lens and standard retinoscopy was determined. To assess the agreement between the two methods of retinoscopy, the Bland–Altman plots were used. Differences between measurements were plotted against their mean and the 95% limits of agreement were determined as the mean difference ±1.96 *standard deviation of the differences. Besides, a two-way repeated-measures ANOVA with factors of retinoscopy method (standard vs. “Mirza” tele-lens) and use of cycloplegic drop (dry vs wet) was performed using the refractive error values. A single expert optometrist was considered to perform the standard and “Mirza” tele-lens retinoscopy to avoid the inter examiner’s errors.
ResultThe refractive errors of 78 eyes from 39 cooperative children with a mean age of 9.69 ± 1.91 years (range from 7 to 12 years) and mean dry refractive errors of +1.39 ± 1.43 D (range from −0.50 D to +5.75 D) were evaluated. Also, the refractive findings of 60 eyes of 31 uncooperative infants with mean age 21.85 ± 8.79 months (range from 8 to 37 months) and mean refraction of +2.23 ± 1.00 D (range from +0.50 D to +4.50 D) were evaluated. It should be noted that these children were related to the kindergarten that is next to the School of Rehabilitation Sciences of Iran University and many of whose parents were employees of the school and were available.
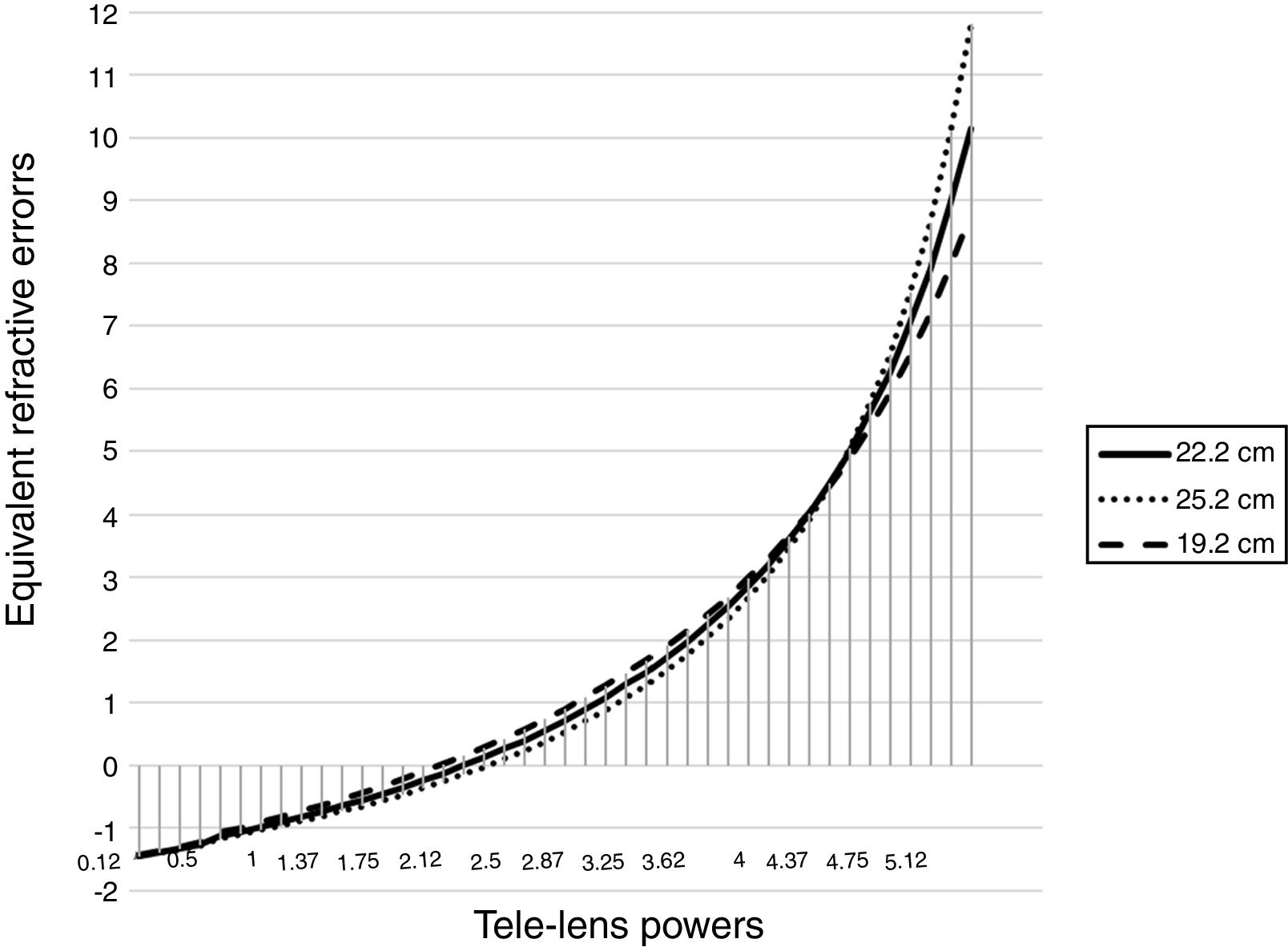
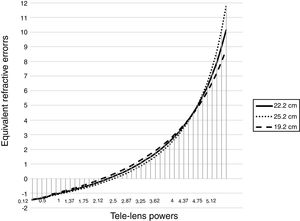
The results of the optical calculationIn this part of the present study, by applying the physical laws of lenses and by producing refractive errors of −1.50 D to +10.00 D, the amount of correction lens power was determined at a trial lens distance of 22 cm from spectacle plane and the results were recorded in Table 1.
Equivalent refractive errors to the values obtained by the “Mirza” retinoscopy method.
| Trial lens power at neutrality | Spectacle plane refractive error(net values) |
|---|---|
| 0 | −1.50 |
| 0.12 | −1.45 |
| 0.25 | −1.38 |
| 0.37 | −1.33 |
| 0.5 | −1.25 |
| 0.62 | −1.20 |
| 0.75 | −1.12 |
| 0.87 | −1.06 |
| 1 | −0.97 |
| 1.12 | −0.91 |
| 1.25 | −0.82 |
| 1.37 | −0.74 |
| 1.5 | −0.65 |
| 1.62 | −0.55 |
| 1.75 | −0.45 |
| 1.87 | −0.35 |
| 2 | −0.24 |
| 2.12 | −0.13 |
| 2.25 | 0.00 |
| 2.37 | 0.12 |
| 2.5 | 0.26 |
| 2.62 | 0.40 |
| 2.75 | 0.56 |
| 2.87 | 0.72 |
| 3 | 0.89 |
| 3.12 | 1.07 |
| 3.25 | 1.28 |
| 3.5 | 1.72 |
| 3.62 | 1.96 |
| 3.75 | 2.25 |
| 3.87 | 2.53 |
| 4 | 2.86 |
| 4.12 | 3.20 |
| 4.25 | 3.59 |
| 4.37 | 4.00 |
| 4.5 | 4.50 |
| 4.62 | 5.01 |
| 4.75 | 5.63 |
| 4.87 | 6.27 |
| 5 | 7.07 |
| 5.12 | 7.93 |
| 5.25 | 9.00 |
| 5.37 | 10.18 |
Based on these results, with the change in hypermetropia from 0.00 to 10.00 D, the tele-lens power was changed from +2.25 D to +5.35 D. In other words, by changing 10 D in standard net retinoscopy values, the tele-lens power results change by 3.15 D.
Possible errors due to changes of ±3 cm in the placement of the trial lens in Fig. 2 with the range of refractive error of −1.50 D to +10.00 D are shown. As it turns out, the error first increases to a certain extent, then the changes progress to a decrease in the error, and again from +4.50 D onwards, an error-increasing trend occurs. the error rate of the 3 cm displacement of the lens in the −1.50 D of the tele-lens power is zero. This error gradually increases from zero in the range of −1.50 D to +4.50 D, and in +3.50 D (equivalent to +1.73 D hyperopic net refraction), the error rate reaches a maximum of 0.21 D and then the error rate decreases. At +4.50 D, this error reaches almost zero.
The error rate is again increased from the point of the +4.50 D by increasing the hypermetropic refractive error and in high hyperopic refractive errors, such that in +7.00 D reaches to about 0.50 D error, in +8.00 D to 0.75 D error and in the +9.00 D and +10.00 D reaches to 1.00 D error.
The retinoscopy results of the cooperative childrenThe mean and standard deviation of the net result of the dry and cycloplegic standard retinoscopy were +1.39 ± 1.43 D (range from −0.50 D to +5.75 D) and +2.37 ± 1.44 D (range from 0.00 D to +7.00 D) according to subtracting 1.50 D equivalent to working distance lens, respectively.
Also, the results of dry and cycloplegic “Mirza” tele-lens retinoscopy were +1.36 ± 1.39 D (range from −0.25 D to +5.95 D) and +2.41 ± 1.37 D (range from +0.50 D to +7.00 D) according to the optical “Mirza” tele-lens retinoscopy conversion Table 1, respectively.
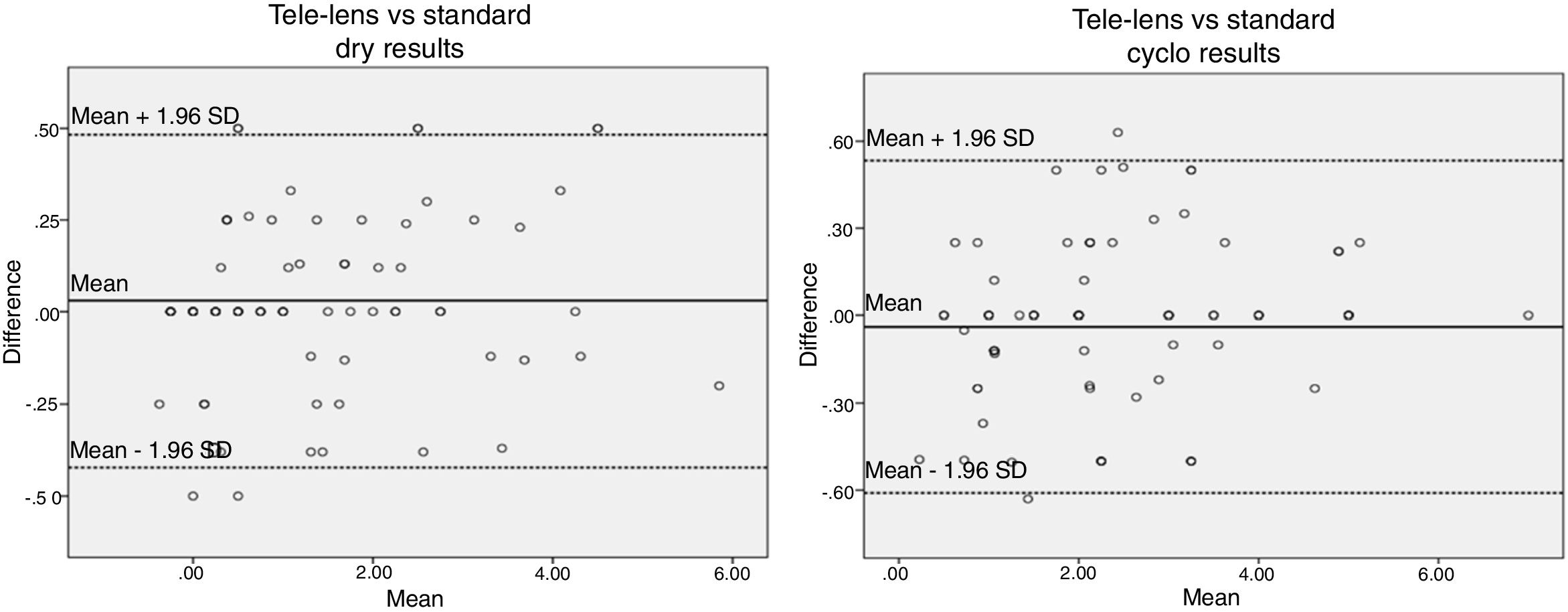
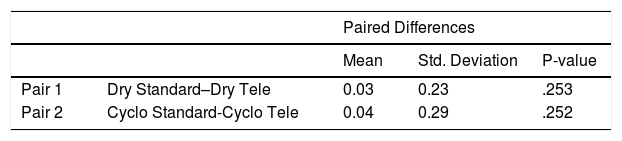
The mean difference between the dry and cycloplegic refraction of the two methods with their p-values are presented in Table 2.
As can be seen in Table 2, the comparison of net finding of dry standard retinoscopy (+1.39 D; 95% CI: +1.06 D to +1.71 D) with the dry “Mirza” tele-lens retinoscopy (+1.36 D; 95% CI: +1.04 D to +1.67 D) was not statistically significant (paired-sample t = 1.15; p = .253). Also, the comparison of mean cycloplegic value of the standard retinoscopy (+2.37 D; 95% CI: +2.04 D to +2.69 D) with the amount of the cycloplegic “Mirza” tele-lens retinoscopy (+2.41 D; 95% CI: +2.10 D to +2.72 D), was not statistically significant (paired-sample t = −1.15; p = .252). Besides, Two-way repeated measures ANOVA revealed no significant retinoscopy method × use of drops interaction (P = 0.103) in comparing two methods of standard and “Mirza” tele-lens retinoscopy.
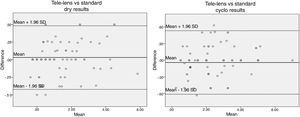
Also, the ICC between the findings of dry and cyclo mode of the “Mirza” tele-lens and standard retinoscopy showed a similar correlation for both methods, i.e. 0.993 (95% CI: 0.989, 0.996) for dry results and 0.989 (95% CI: 0.983, 0.993) for cyclo results. The calculated 95% limits of agreement for dry and cyclo findings are shown in Fig. 3A and B. The agreement and the obtained mean differences were not statistically different (p > 0.05).
The retinoscopy results of the younger uncooperative children and infantsThe “Mirza” tele-lens retinoscopy results of 60 eyes of 31 uncooperative infants with mean age 21.85 ± 8.79 months (range from 8 to 37 months) were evaluated. Three of the total numbers of infants were not at all willing to cooperate for manifestations such as crying, restlessness, fear, and hanging lens off even while the trial lens was placed in the 22.2 cm further away from the spectacle plane.
The mean refractive errors in these infants were +2.23 ± 1.00 D (range from +0.50 D to +4.50 D).
It is worth noting that all of these 31 infants were unwilling to cooperate for standard retinoscopy for the reasons previously described, so the results of this part only include the mean and standard deviation of the refractive errors obtained by the “Mirza” tele-lens retinoscopy and because of the lack of standard retinoscopic results, no comparisons could have been made. The purpose of this section was to investigate the feasibility of the “Mirza” tele-lens retinoscopy method in infants rather than comparison with the result of the standard retinoscopic procedure.
DiscussionThis study was conducted to introduce a new method of retinoscopy called the “Mirza tele-lens retinoscopy”. Based on the findings of this study and the high ICC between the net results of this new method and standard retinoscopy in cooperative older children, it can be said that this method is an alternative to standard retinoscopy with acceptable precision and accuracy and can be used in some young mentally retarded children and infants which are anxious and frightened by approaching and placing the trial lens on the spectacle plane. Using this new method, the refractive status of the eye can be assessed with minimal discomfort for the tested person. Since the evaluation of refractive error with standard retinoscopy method in non-cooperative children does not lead to accurate results and viewing the initial retinoscopic reflex may be with some difficulties and in the most case actually fails,9 this new method takes into account a solution such as increasing the distance of the correction lens from the child and the least contact with the child that is more optimal for assessment of refractive error.
It is clear that the “Mirza” tele-lens retinoscopy performance, like the standard retinoscopy method, needs to acquire skills with continuous practice to be done correctly, which means that at first, one may have difficulty viewing and assessing the retinoscopic reflex. Therefore, the “Mirza” tele-lens retinoscopy with practice and proficiency can be performed almost as quickly as the standard retinoscopy by a skilled optometrist in some cases that do not have the mentioned necessary cooperation for the relevant procedure. In the early days of beginning the “Mirza” tele-lens retinoscopic procedure, to facilitate the maintenance of the correct working distance, the tie a string to the head of the scope with knots at a distance of 66.6 and 22.2 cm from the spectacle plane was adjusted. After performing this procedure for a long time and increasing the skill and gaining experience by an optometrist in performing the “Mirza” tele-lens retinoscopic method, no string was used to maintain the working distance, although the authors of the article initially advised using this string to maintain the correct working distance. Besides, the lighting conditions of the room were changed to dim light in order to perform the “Mirza tele-lens retinoscopy” as required for the standard retinoscopy.
It is clear that most infants are hyperopic and the average cycloplegic refractive error is approximately +2.00 D with a standard deviation of approximately 2.00D.12 On the other hand, the refractive error value is equal to +4.50 D when the neutral point was observed with the trial lens of +4.50 D in the “Mirza” tele-lens retinoscopy, therefore this lens as a starting point in this retinoscopy procedure can be used with sufficient accuracy and speed to detect refractive errors and in turn, to manage the visual functions of infants with visual disorders such as strabismus, accommodative anomaly, and amblyopia because the hypermetropic values of more than 4.00 D in early life in infants can mostly cause such problems.13–15
According to the results of the present study, when the hyperopic changes are 4.50 D from 0.00 D to +4.50 D, the “Mirza” tele-lens retinoscopic changes occur within a range of 2.25 D from +2.25 to +4.50 D. When the net standard retinoscopic changes are 5.50 D from +4.50 D to +10 D, the equivalent spectacle plane hyperopia in the “Mirza” tele-lens retinoscopy will be only 0.85 D from +4.50 to +5.35 D, so the results are very close to each other in this method and the different amounts of hypermetropia in theses ranges are a bit difficult to distinguish, although the brightness and motion of the retinoscopic reflex will be very favorable due to the magnification caused by the trial lens at a distance of 22.2 cm of the spectacle plane. Therefore, applying this new method to evaluate the refraction of infants requires a great deal of precision, as in higher refractive error may require the use of trial lenses with steps of ±0.12 D for neutralization procedure. Although the “Mirza” tele-lens retinoscopy method can be a good alternative to the standard retinoscopy in uncooperative infants, given the low range changes of corrective lens and the high potential for a significant error to reach the neutralization endpoint in very high hyperopic values, it is recommended that firstly, at higher hypermetropic values, more precision should be used to detect the ‘with’ or ‘against’ movement of the retinoscopic reflex, secondly, it is important to note that the accuracy of this method is reduced in very high values of hypermetropia. For example, according to Table 1, it is clear that by changing the amount of hypermetropia from 9.00 D to 10.00 D, the results of the “Mirza” tele-lens retinoscopy change from +5.25 D to +5.35 D, which means that for 1.00 D change in this hyperopic range, only 0.10 of a change in the “Mirza” tele-lens retinoscopy is seen. Another important point that needs to be explained is to evaluate the myopic infants because the minification of the negative lens increases with increasing the distance from the spectacle plane, which in turn makes the evaluation of the refractive error difficult and inaccurate, especially in amounts more than 3.00 D of myopia. In this study, patients with the refraction of more than 1.50 D myopic were also present that their number was very limited. On the other hand, the myopia of 1.50 D could be neutralized without any lenses at a working distance of 66.6 cm. And also myopia of 2.00 D could be neutralized without any lenses at a working distance of 50 cm and myopia of 5 D at 20 cm, so we do not need to use “Mirza” tele-lens retinoscopy at myopia more than 1.50 D.
It is worth mentioning that due to other reasons such as the probability of increasing the surface scattering and optical aberration of the trial lens in high myopic refractive errors, and the need for trial lenses outside the available lenses in the clinic’s trial lens set, the values above 1.50 D myopia have not been reported. In fact, the “Mirza” tele-lens retinoscopy is not practical in myopic cases above 1.50 D myopia, and in these cases, the radical retinoscopy can be considered a more appropriate alternative because by reducing the distance, a more visible reflex can be seen, so retinoscopy will be easier and can be performed without any trial lens.
As mentioned previously, in this new method, the trial lens is placed at a distance of 22.2 cm instead of on the spectacle plane and near the eyes. Therefore, a novice refractionist may not observe the exact distance. If this distance is incorrectly considered, for example, 3 cm forward (19.2 cm) or backward (25.2 cm), changes will occur based on the optics of the method.
The error rate of the 3 cm displacement of the lens increases from zero to 0.21 D in the refractive error ranges of −1.50 D to +3.50 D, and then gradually decreases up to the refraction of +4.50 D that reaching almost zero in this point. After this point of +4.50 D, the error gradually increases and this error rate reaches 1.00 D in high hyperopic refractive errors about 10.00 D.
Due to the most children with binocular anomaly such as accommodative esotropia that often have the average cycloplegic refractive error of +4.75 D with ranges between +1.50 and +7.00 D,16 the probability of error by changing the distance will reach its lowest level in these ranges (0.12 D to 0.50 D). Therefore, the maximum error of the 0.50 D is completely negligible and could not cause any problems in the course of clinical practice comparing to the facilities it provides for us.
In fact, this method is recommended when the standard method is not applicable, and therefore, methods such as Hirschberg test for measuring the angle of strabismus that is used in the ophthalmic clinic however is not very accurate, it is very helpful when the practitioner is forced to use.
Another way to reduce errors in high refractive hyperopic values is to instantly and for a moment placing the lens on the spectacle plane and neutralizing the retinoscopic reflex in the standard method. Although the child does not allow the lens to be close to his eyes, a skilled refractionist can capture this moment.
Despite all these ways of error reduction, the authors accept that this method requires the acquisition of skills to keep the working distance lens in its correct position to increase retinoscopic accuracy and reduce the error rate.
As a report of new technique that explores the possibility of doing the refraction by this technique and not validating the technique, it may be overlooked.
To determine the validity of the new technique of retinoscopy, the non cycloplegic and cycloplegic “Mirza” tele-lens retinoscopy findings were compared with the gold standard retinoscopy findings by using two methods of the intraclass correlation coefficient (ICC), and Bland–Altman plots. As the results of the present study showed, there were high agreement values (ICC higher than 0.98) between results provided from standard and the “Mirza” tele-lens retinoscopy in both situations of dry and cycloplegic refraction. These values between the results of these two retinoscopic methods indicate a strong relationship between them, which means that the results of the “Mirza” tele-lens retinoscopy are sufficiently accurate and valid, so this method of retinoscopy is useful in evaluating the refractive errors especially in poorly or un-cooperated children instead of the standard dry and cycloplegic retinoscopy method. Two-way repeated measure ANOVA showed a lack of interaction between the two factors, so the “Mirza” tele-lens retinoscopy results in both cyclo and dry mode were consistent with the standard retinoscopic results. In addition, the Bland–Altman analysis for the agreement of dry and cyclo findings of the “Mirza” tele-lens retinoscopy with standard retinoscopy showed no significant differences in the 95% limits of agreement with shorter range for dry than the cyclo results of the “Mirza” tele-lens retinoscopy (Table 2 and Fig. 3), suggesting that the data obtained from these measurements from the two different methods of retinoscopy can be interchanged. In fact, this way can be used to examine validity by assessing the level of agreement by visualizing the data with Bland–Altman plots. According to the mentioned results, a good argument between the data of the two retinoscopic methods indicates the optimal validation of the “Mirza” tele-lens retinoscopy method.
It is essential to pay attention to some tips:
First, the distance of 22.2 cm (1/3 of the standard retinoscopic distance) was considered in the present study to make the optical calculations as easily as possible.
Second, careful observance of the distance of 22.2 to perform in the present study is necessary because the change of this distance can cause mistakes in the evaluation of the high refractive errors and optical calculations.
Third, the optometrists and ophthalmologists who work in the field of pediatric visual assessment can consider distances other than 22.2 cm, in fact, any distance that leads to the child’s cooperation in the retinoscopy procedure can be considered for this purpose.
Fourth, the conversion optical calculations should be made out according to any distance provided for lens placement (more or less than 22.2 cm) based on the items mentioned in the present study.
The notable limitations of the present study are:
- 1
To perform this new method for assessing the refraction in children with non-cooperation, it is necessary to acquire the incumbent skills, so the examiner must be an expert. there are challenges at beginning the standard retinoscopy, that over time by repeating the procedure and gaining skills, the procedure will be easier to perform and the refraction will be evaluated more accurately.
- 2
It is necessary to observe the distance of the trial lens in order to reduce the measurement error during the retinoscopy process. However, the errors made by changing the distance of 3 cm to the desired position of the trial lens (22.2 cm) are discussed in the article.
- 3
In high amounts of hyperopia, it is very important to use the trial lens with power steps of 0.12 D to neutralize the refractive errors, and in high myopia, as mentioned, it is better to use alternative methods such as radical retinoscopy, and the tele-lens method will not be accurate enough in such these cases, and better not to be used.
It should be noted that, when the standard retinoscopy procedure does not apply to uncooperative infants and children, some articles recommend the use of sedative agents and ocular examination under more invasive conditions. In this situation, if the distance of the trial lens to the spectacle plane increases which, in turn, most often causes the child to cooperate in the retinoscopy process, then the “Mirza” tele-lens retinoscopic method becomes applicable, meaning this new method may prevent the need to examine under anesthesia because this situation can be associated with risks.17,18
ConclusionGiven that most infants and children are hypermetropic and that 4.50 D of hyperopia in the “Mirza” tele-lens retinoscopic method is equivalent to this amount and starting point of the most of the accommodative problems and anomalies will begin from these values so this method can be used in the evaluation of refraction of infants and children who do not have the necessary cooperation for the standard retinoscopic procedure.
FundingNone declared.
Conflict of interestThe authors have no conflicts of interest to declare.
This study was supported by the Iran University of Medical Sciences. We would like to thank all staff of the optometry clinic of the School of Rehabilitation Sciences in this study.