To compare contrast sensitivity function (CSF) with soft contact lens (SCL) and spectacles wear. To investigate the effect of a three-month period of SCL wear on CSF.
MethodsForty-seven myopic subjects with no history of contact lens (CL) wear were included in this longitudinal prospective study. CSF was measured with spectacles using the CSV-1000 (VectorVision, Greenvile, OH). Subsequently, subjects were fitted with a daily disposable lens (Nelfilcon-A, Stenofilcon-A or Nesofilcon-A) in one eye and a monthly disposable lens (Lotrafilcon-B, Comfilcon-A or Balafilcon-A) in the other eye and wore the same type of CLs for three months. CSF was measured again on the same day and after three months wearing CLs. Differences in CSF with spectacles and CLs on baseline and changes to CSF after three months of CLs wear were assessed. The effect of lens materials and wearing modality on CSF change was also investigated.
ResultsCSF was higher with CLs in comparison to the values with spectacles for spatial frequencies of 3, 6 and 12 cycles per degree (cpd) (p<0.05) while there was no difference for spatial frequency of 18 cpd (p=0.114). No significant difference was found in the CSF with CLs between baseline and after three months of lens wear (p>0.05). There was no difference in CSF between hydrogel and silicone CLs as well as when comparing daily with monthly wear CLs (p>0.05).
ConclusionCSF is better with CLs than with spectacles. CSF values with CL are similar between baseline and after 3 months of lens wear.
Comparar la función de sensibilidad al contraste (CSF) con el uso de lentillas blandas y gafas. Investigar el efecto en la CSF de un periodo de uso de lentillas blandas de tres meses.
MétodosEn este estudio longitudinal prospectivo incluimos a cuarenta y siete sujetos miopes sin antecedentes de uso de lentillas. La CSF se midió con gafas, utilizando el sistema CSV-1000 (VectorVision, Greenvile, OH). A continuación, se proporcionaron a los sujetos lentillas diarias desechables (Nelfilcon-A, Stenofilcon-A o Nesofilcon-A) en un ojo, y lentillas mensuales desechables (Lotrafilcon-B, Comfilcon-A or Balafilcon-A) en el otro ojo, utilizándose el mismo tipo de lentillas durante tres meses. Se volvió a medir la CSF el mismo día, y transcurridos tres meses de uso de lentillas. Se evaluaron las diferencias en cuanto a CSF con gafas y lentillas al inicio, y los cambios de CSF transcurridos tres meses de uso de lentillas. También se investigó el efecto en el cambio de CSF de las modalidades de las lentillas y la modalidad de uso.
ResultadosLa CSF fue más alta con el uso de lentillas, en comparación con el uso de gafas para las frecuencias espaciales de 3, 6 y 12 ciclos por grado (cpg) (p<0,05), mientras que no se produjo diferencia para la frecuencia espacial de 18 cpg (p=0,114). No se encontró diferencia significativa de CSF entre el valor basal y transcurridos tres meses de uso de lentillas (p>0,05). No se encontró diferencia de CSF entre las lentillas de hidrogel y silicona, ni al comparar el uso de lentillas diarias y mensuales (p>0,05).
ConclusiónLa CSF es mejor con lentillas que con gafas. Los valores de CSF con el uso de lentillas son similares entre el valor basal y transcurridos tres meses de uso de lentillas.
Visual threshold to determine the smallest difference in contrast between the visible and invisible is the threshold contrast, the reciprocal of which provides contrast sensitivity.1 Generally, sinusoidal gratings, which contain a gradual change from highest luminance to lowest luminance and vice-versa, are used to determine the visual contrast threshold. This is measured with different spatial frequencies and contrasts, so it measures the real-world visual function unlike the visual acuity measurement. Visual acuity only indicates the visual performance on high contrast, and generally it is measured in a 100% contrast target. It does not stand as a complete tool to represent visual performance because contrast greatly varies in the real-world visual requirements and a wide range of targets have about 1% of contrast. In some conditions, contrast sensitivity may be significantly reduced even if visual acuity remains normal.1
Many researchers included contrast sensitivity tests to determine the visual performance with different types of contact lenses (CL). Some have assessed contrast sensitivity as the function of different spatial frequencies, which is contrast sensitivity function (CSF),2–4 while others have measured visual acuity with high and low contrast visual acuity charts.5,6 However, low contrast visual charts reflect the slope of higher spatial frequency level alone.7 Some of the previous studies found no difference in the CSF in subjects wearing spectacles and CL.6 However, Ortiz et al. found lower CSF with cosmetic as well as iris tinted soft CL when compared to no correction.8 Porish showed that the CSF can be improved in athletes with sport-tinted CL.9 However, the improvement was too small to affect the performance of these athletes.
Currently, with the high need to constantly perform tasks that require continuous observation of objects with varying degrees of contrast, and not only objects easily visible with high contrast, it becomes relevant to assess the CSF. As the CSF is positively correlated with vision-related quality of life, it is important to learn whether current CL affect contrast sensitivity.10,11 As far as the authors know, none of the previous studies determined the effect of contemporary CL wear on the CSF. The aim of this study was to investigate the effect of three months of soft CL wear on the CSF. The CSF with CL (baseline) was compared with spectacles and after three months of CL wear. The effect of lens materials, wearing modality, and gender on the CSF was also assessed.
Material and methodsNinety-four eyes of 47 healthy neophyte myopic subjects between 18 and 40 years of age with no ocular pathology were included in this longitudinal clinical trial. All the subjects had best corrected visual acuity equal or better than 6/6 in each eye. Subjects with astigmatism higher than 0.75 dioptre (D) and history of CL wear were excluded. A consent form was signed after detailed information was provided to the subjects. This study followed the tenets of the Declaration of Helsinki and was reviewed and approved by the University of Minho's Ethics Subcommittee for Life and Health Sciences. The sample size was calculated to warrant 80% statistical power with 0.05 significant level to detect the difference in LogCS by 0.15 between two conditions: with spectacles and CL at baseline; and with CL at baseline and after a period of three months of wear.
Preliminary examination including slit-lamp bio-microscopy and both objective and subjective refraction was performed on each subject. Visual acuity was measured with spectacles using Snellen self-illuminated chart. CSF was measured with CSV-1000 (VectorVision, Greenvile, OH).3,12,13 This is one of the commercially available contrast sensitivity measurement tools with good reliability which applied sinusoidal gratings.14 It uses an subjective method by forced-choice detection and measures the contrast sensitivity in four levels of spatial frequencies: 3, 6, 12 and 18 cycles per degree (cpd).1 Each set of spatial frequency contains 17 patches with a diameter of 3.8cm or 0.87 degrees. The first patch with highest contrast vertical sinusoidal gratings is used for explanation while the other 8 pairs of patches, numbered 1 to 8, are used for testing. The contrast of the 1st to 3rd patch decreases in 0.17 log unit steps while, from the 3rd to the 8th, it decreases in 0.15 log unit steps. The chart is retro-illuminated with an 85cd/m2 fluorescent light which can be controlled with a remote control. Subjects were seated two and a half meters away from the chart. CSF was measured in each eye separately with their habitual spectacles. Contrast sensitivity value of the last correct response was documented. As sensitivity is the inverse of contrast values, the log unit was used, and therefore, higher log values indicate better sensitivity.15 Each sinusoidal grating patch contains a bar with brightest luminance and darkest luminance, and the thickness of the bar depends on the spatial frequency of the gratings, e.g. for 3 cpd it is wider in comparison to that of 18 cpd. Thus,
Schirmer's test, keratometry and biomicroscopic examination were also performed on each subject. One eye was fitted with a daily disposable lens (Nelfilcon A or Stenofilcon A or Nesofilcon A) and the other was fitted with a monthly disposable lens (Lotrafilcon B or Comfilcon A or Balafilcon A) in a contralateral manner. Only monofocal spherical CL were used in this study. Details on the CL are presented in Table 1. Lens fitting was evaluated, and should any unacceptable fitting be found due to lens parameters, another lens was fitted from the study lens group. CSF was measured again after 30min of CL wear. OPTIFREE® Puremoist® multipurpose disinfecting solution (Polyquad 0.001% and Aldox 0.0006%, Alcon Laboratories, TX) was provided for the care of the monthly disposable lenses. Subjects were instructed to come after three months of CL wear for follow-up evaluation and subjects were again evaluated including the CSF assessment.
Characteristics of the lenses used in the study. Nelfilcon A and nesofilcon A are hydrogel lenses while others are silicone hydrogel lenses.
| Lotrafilcon B | Comfilcon A | Balafilcon A | Stenofilcon A | Nelfilcon A | Nesofilcon A | |
|---|---|---|---|---|---|---|
| Company | Alcon | Cooper Vision | Bausch & Lomb | Cooper Vision | Alcon | Bausch & Lomb |
| Brand name | AirOptix® AquaTM | BiofinityTM | Purevision2TM | MyDayTM | Dailies® AquaComfort Plus® | BiotrueTM ONEday |
| Water content (%) | 34 | 48 | 36 | 54 | 69 | 78 |
| Thickness (mm) | 0.08 | 0.08 | 0.07 | 0.08 | 0.10 | 0.1 |
| Base curve/ diameter (mm) | 8.6/14.2 | 8.7/14.5 | 8.6/14 | 8.4/14.2 | 8.7/14 | 8.6/14.2 |
| Oxygen Permeability (barrer)m | 110 | 128 | 91 | 80 | 26 | 42 |
| Modulus (MPa) | 1.2 | 0.75 | 1.1-1.25 | 0.4 | 0.89 | 0.49 |
| Transmissibility (barrer/cm) | 137.5 | 160 | 130 | 100 | 26 | 42 |
Data were analysed with Statistical Software for Social Sciences (SPSS 22, IBM Corp., Armonk, NY). Kolmogorov-Smirnov test was applied to analyse the distribution of the variables; parametric tests were used to test normally distributed variables and non-parametric tests were applied to others. A repeated measures ANOVA was used to compare the CSF values in three different situations (with spectacles and with CL during baseline visit and with CL on final visit) as well as to detect the effect of gender on it. Association of changes in the CSF according to lens wearing modality (daily disposable vs monthly disposable) and type of lenses (hydrogel vs silicone hydrogel) was assessed by applying Mann-Whitney test. Correlation of the CSF with lens thickness, oxygen permeability and water content was determined by applying Spearman's rho test. P values less than 0.05 were considered as statistically significant.
ResultsNinety-four eyes of 47 subjects with a mean age of 24.3±4.1 years were included in this study. Among these, 66.0% (31) were women. The mean refractive error was −1.86±1.54D with a range of −0.75 to −5.50D. Lotrafilcon B was worn in 16 eyes, Nelfilcon A on 16 eyes, Comfilcon A on 15 eyes, Stenofilcon A on 15 eyes, Balafilcon A on 16 eyes and Nesofilcon A on 16 eyes. Subjects used the CL for 11.8±1.8h per day.
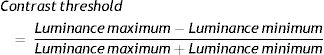
Table 2 shows the values of the CSF with their habitual spectacles (before starting to wear CL), after 30min of CL use on the first visit, and after a period of three months CL wear. Repeated measures of ANOVA shows that there is no difference in the CSF values with spatial frequency of 18 cpd (F(2, 174)=2–196, p=0.114) but there is a statistically significant difference in CSF with spatial frequencies of 3 cpd (F(1.754, 152.606)=12.729, p<0.001), 6 cpd (F(1.832, 159.419)=14.141, p<0.001) and 12 cpd (F(2, 174)=5.001, p=0.008). Pairwise comparison shows that baseline CSF with spectacles was less than that with baseline CSF with CL and final CSF with CL with spatial frequencies of 3, 6 and 12 cpd (p<0.05). However, there was no significant difference between baseline CSF values with CL and final CSF values with CL with spatial frequencies of 3, 6 and 12 cpd (p>0.05). In average, baseline CSF with CL was 0.07 higher than baseline CSF with spectacles.
Contrast sensitivity function (in Log Units) with spectacles and with contact lenses on the first day and with contact lenses on the final day.
As shown in Fig. 1, the CSF was higher at medium level of spatial frequency when compared to lower or higher spatial frequencies with spectacles as well as with CL during baseline and after the three-month period.
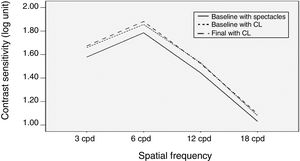
There were no statistically significant differences between CSF values obtained in men and women neither with spectacles nor with CL (p>0.05). Table 3 presents the changes in the CSF for each spatial frequency for the different lens materials after a period of three months of lens wear. There was no association of lens wearing modality with changes in the CSF values. It was similar with daily and monthly disposable lenses (p>0.05). The CSF values were similar with silicone hydrogel lenses and hydrogel lenses (p>0.05). Also, no significant correlation was obtained between the changes in the CSF with water content (r<0.121, p>0.05), oxygen permeability (r<0.145, p>0.05) or lens thickness (r<0.144, p>0.05).
Changes in contrast sensitivity function (in Log Units) by three months of soft contact lens wear with different lens materials.
| 3 cpd | 6 cpd | 12 cpd | 18 cpd | |
|---|---|---|---|---|
| Lotrafilcon B | 0.04±0.17 [0.464] | 0.08±0.22 [0.217] | 0.07±0.40 [0.608] | −0.02±0.31 [0.805] |
| Comfilcon A | 0.04±0.09 [0.052] | −0.01±0.18 [0.320] | 0.05±0.26 [0.506] | 0.003±0.24 [0.758] |
| Balafilcon A | −0.01±0.15 [0.464] | 0.001±0.17 [0.916] | −0.13±0.27 [0.053] | 0.02±0.27 [0.959] |
| Nelfilcon A | −0.02±0.19 [0.465] | 0.05±0.22 [0.422] | 0.03±0.33 [0.527] | 0.07±0.29 [0.318] |
| Stenofilcon A | 0.02±0.10 [0.330] | 0.03±0.17 [0.354] | 0.01±0.13 [0.892] | −0.04±0.18 [0.473] |
| Nesofilcon A | 0.03±0.18 [0.549] | −0.01±0.12 [0.863] | −0.07±0.33 [0.717] | 0.04±0.28 [0.474] |
Mean values±standard deviations are followed by p values in bracket.
Fig. 2 shows the CSF for the different lens materials at baseline and at the final follow up visit. It can be observed that different materials apparently behaved differently. For example, with lotrafilcon B lens wear, the CSF increased at 3, 6 and 12 cpd, but decreased at 18 cpd, while with comfilcon A lens wear, the CSF increased in 3, 12 and 18 cpd, but decreased at 6 cpd after three months of lens wear. However, all of these differences were considered not statistically significant (p>0.05). The difference in the CSF was not correlated with the refractive power of the lenses (r<0.164, p>0.05).
DiscussionThis study measured the effect of soft CL wear in the CSF, by comparing the scores obtained with spectacles and after a period of three months of lens wear. The effect of lens materials, wearing modality, and gender was also assessed. Significantly higher CSF was found with CL in comparison to the CSF with spectacles on the first examination for all the spatial frequencies except for the spatial frequency of 18 cpd. The lower the spatial frequency, the greater was the difference. Similar to our findings, Dalcoll et al. found an increase in the CSF with soft CL.16 The CSF is a product of both neural and optical factors.1 Aberration and glare affect the quality of the image, so the higher CSF with CL when compared to spectacles, may be due to the smaller asymmetric aberrations with soft CL.17 Charman reported that incorrect refractive error correction reduces the CSF in high spatial frequency.18 So, in the current study, no difference in the CSF with spectacles and CL in high spatial frequency of 18 cpd may be due to uncorrected astigmatism with spherical CL. Furthermore, the difference in the CSF with spectacles and with CL during the baseline visit was inferior to 0.14 Log units in all the spatial frequencies, so this difference may not be clinically significant.19
Contrary to the current study, a couple of previous studies found no difference in the CSF with spectacles and with soft CL wear.20,21 Gray suggested that changes in corneal physiology due to CL wear may reduce the CSF.22,23 However, in the current study, the baseline CSF was measured with CL within half an hour of lens wear. So, within this short period, no changes in corneal physiology are expected.
Another important finding of this study is that three months of soft CL wear did not change the CSF. Soni et al. suggested that CL with higher thicknesses and low oxygen transmissibility may reduce the CSF by inducing corneal edema.7 However, in the current study, CL were worn in a daily wear modality and the central thickness of the lenses was not more than 0.10mm. The oxygen transmissibility of the CL used in this study was enough to avoid corneal edema on open eye condition.24 Lira et al. found that CL power impacts oxygen transmissibility as the central thickness and the peripheral thickness of the CL differ significantly, especially in high power lenses.25 However, low power CL (mean −1.86±1.54D) were used in this work, so, it is not expected to find lower Dk/t values than those recommended for daily wear. Supporting our findings, Grey found no changes in the CSF with six months of soft CL wear.23 In his six-sample size study, he concluded that the CSF initially decreases with soft CL wear but it rapidly recovers to a normal state within few hours. In another study, he found a reduction in the CSF with soft CL after few hours of wear when compared to the initial CSF with no correction.22
As shown in Table 3 and Fig. 2, CSF seems to vary with lens materials. There was a smaller difference in CSF on lower spatial frequency when compared to the CSF on higher spatial frequencies, and this variation was highly perceivable after three months of CL wear. However, this variation was not statistically significant. Moreover, in this study, the CSF was similar with daily disposable versus monthly disposable lenses and silicone lenses versus hydrogel lenses. Contrary to the present findings, Belda-Salmeron found that the CSF depends on the lens materials as well as lens design and manufacturing methods.6 They reported severe reduction in the CSF with thicker lenses than thinner lenses and a better CSF with lathe-cut lenses as opposed to spectacles or cast-moulded lenses was found. However, in the current study, there was no significant correlation between changes in the CSF and centre thickness. This may be due to the fact that, a small range of centre thickness of the CL was used in the current study. Gupta et al. compared the CSF with two types of CLs, Purevision multifocal and Purevision single vision lenses, and found no differences in the CSF.26 Similarly, Fernandes et al. found no significant difference in the CSF with multifocal and monovision CL in presbyopic subjects.5
This study used the CSV-1000 for contrast sensitivity measurement. Some of the studies found lower reliability of the CSV-1000 in CS measurement.27 However, the same test was used during all the visits in this longitudinal study and the same examiner measured all the data. It was reported that reliability increases if performed by the same examiner.27 One limitation of the study is that the CSF was measured with habitual spectacles of the subjects on the first day, and the power of the spectacles in some of the subjects might not be accurate at that time.
Thus, from this study, it can be concluded that CSF is higher with soft CL when compared to the CSF with spectacles. No significant difference was found in the CSF with CL between baseline and after 3 months of lens wear. The CSF with CL does not relate to the lens materials, wearing modality and gender of the subjects. In the future, it would be interesting to explore the effect of toric and multifocal CL wear on the CSF.
Conflict of interestThe authors have no conflicts of interest to declare.
Financial supportThis work was supported by the Portuguese Foundation for Science and Technology (FCT) within the framework of the Strategic Funding UID/FIS/04650/2019.