Retinitis as a feature of syphilitic uveitis in immunocompromised individuals is a common finding. We present spectral domain OCT images of early syphilitic retinitis pre and post treatment with penicillin. This case suggests that the inner retinal layers may be selectively involved with early syphilitic retinitis. Early treatment is important to avoid outer layer retinal involvement and to decrease ocular morbidity.
Es frecuente el hallazgo de la retinitis como una característica de uveítis sifilítica en personas inmunodeprimidas. Presentamos imágenes de OCT Spectral Domain de retinitis sifilítica incipiente antes y después del tratamiento con penicilina. Este caso sugiere que las capas internas de la retina pueden estar afectadas selectivamente por retinitis sifilítica incipiente. Es importante llevar a cabo un tratamiento temprano para evitar la afectación de la capa externa de la retina y para reducir la morbilidad ocular.
The clinical manifestations of ocular syphilis have been extensively reported.1–7 Syphilitic uveitis involving the posterior segment may present with vitritis, retinal vasculitis, retinitis, chorioretinitis or papillitis.1–7 In immunocompromised patients, the infection may have an atypical appearance. However, recent case studies suggest that retinitis, in conjunction with posterior uveitis, may be the predominant clinical manifestation in HIV infected individuals.5,6 The ability to localize the infection to the inner retinal layers using spectral domain OCT analysis may aid the practitioner in the diagnosis and management of syphilitic retinitis. To the best of our knowledge, we present the first OCT images of pre- and post-treatment syphilitic retinitis utilizing new generation spectral domain technology. This may be a useful clinical diagnostic tool in predicting visual prognosis in these patients.
Case reportA 67-year-old African American male presented with a four day history of blurred vision, floaters and a red, throbbing, left eye (OS). He denied any systemic conditions and use of any medications. His last physical examination 25 years prior was unremarkable and he denied any history of previous red eye episodes. As a horse trainer he reported exposure to ticks, although he could not remember the last time he received a tick bite. He denied any rashes, recent weight loss or fatigue. He denied being at risk for infection of sexually transmitted diseases. He was a non-smoker and denied alcohol, intra-venous (IV) or illicit drug use.
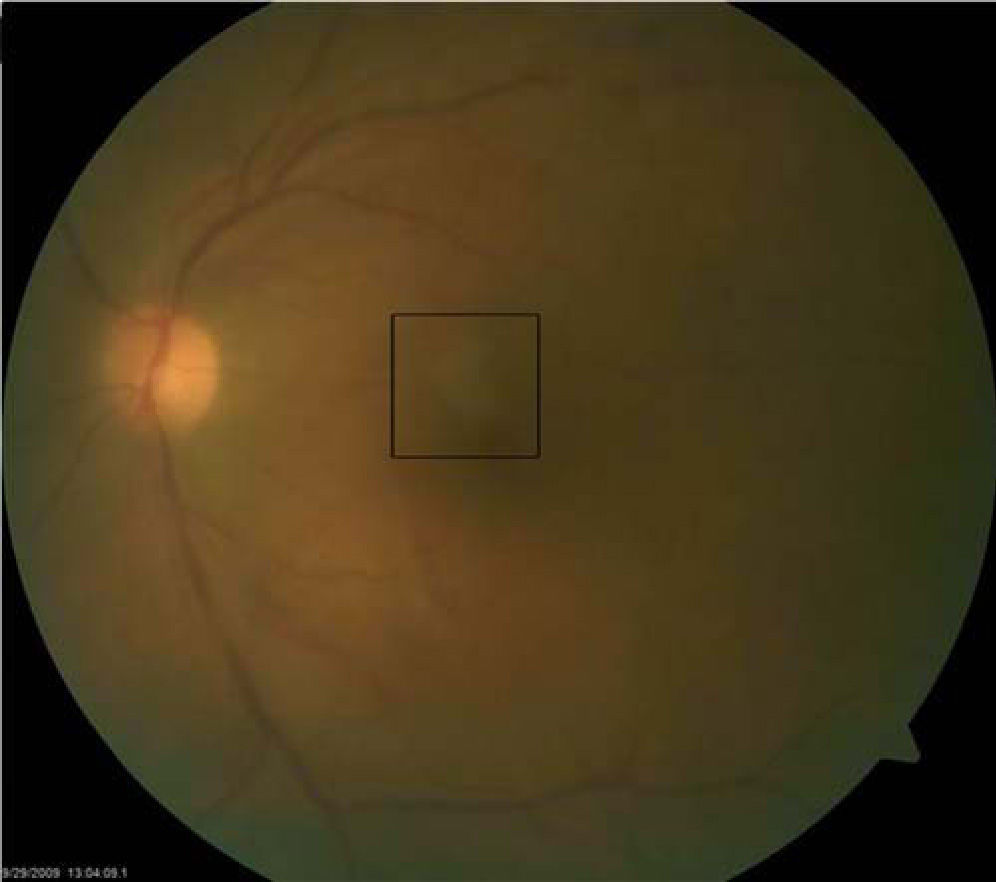
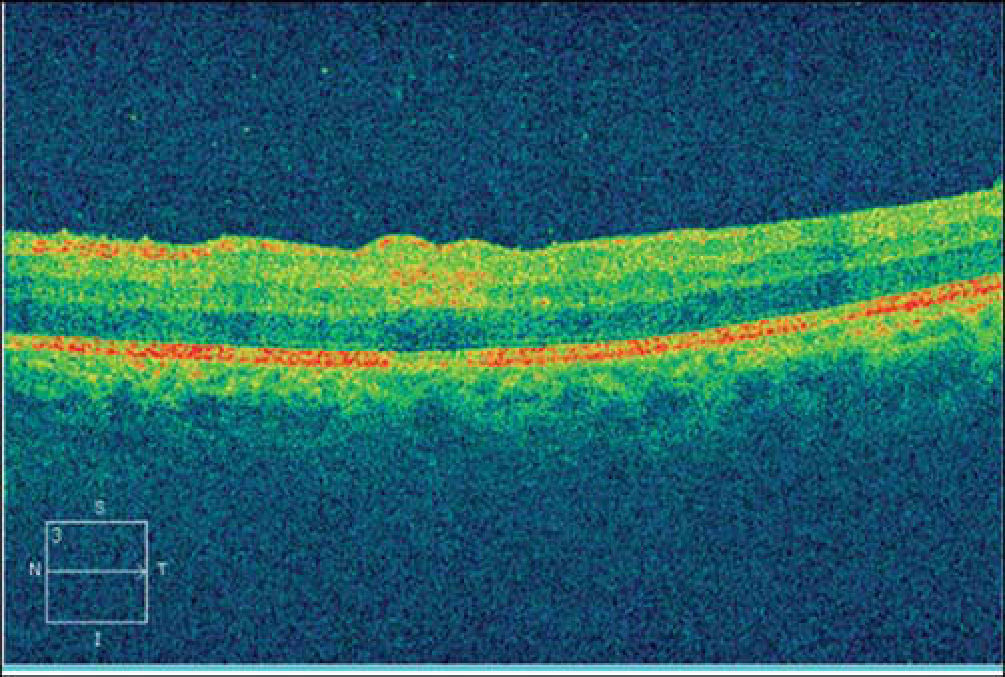
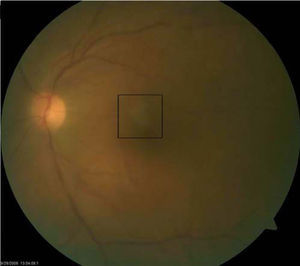
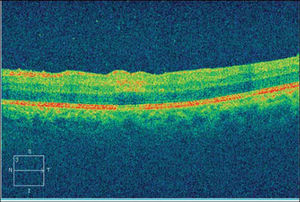
Best-corrected visual acuities were 20/20 right eye (OD) and 20/200 OS. Pupils were equal, round and reactive to light with no afferent pupillary defect. Anterior segment examination OD was unremarkable, while the OS showed 2+conjunctival peri-limbal injection, 3+cells and flare and 3+corneal edema with mutton fat keratic precipitates on the endothelium. Goldmann applanation tonometry readings were 12 mmHg OD and 10 mmHg OS. Dilated fundus examination revealed 2+vitreous cells with a placoid yellow retinal lesion in the superior para-foveal region OS (Figure 1). The right eye fundus was unremarkable and optic nerve appearance was normal in each eye. CirrusTM High Definition-Optical Coherence Tomography (HD-OCT) was performed and demonstrated an area of hyper-reflectivity involving the inner plexiform/ganglion cell layer corresponding to the para-foveal lesion OS. Optical shadowing of the underlying retinal pigment epithelium (RPE) was also noted (Figure 2).
Pre-treatment spectral domain OCT demonstrating hyper-reflectivity involving the inner plexiform/ganglion cell layer corresponding to the para-foveal lesion OS. There is also optical shadowing of the underlying retinal pigment epithelium (RPE). Outer retinal layers and photoreceptors are spared.
Owing to the panuveitis, blood work was ordered including: complete blood count (CBC) with differential; angiotensin converting enzyme (ACE) and chest-X-ray; purified protein derivative (PPD); rapid plasma reagin (RPR) and fluorescent treponemal antibody absorption (FTA-ABS); toxoplasmosis IgG and IgM titers and lyme titers. The patient was referred to a uveitis specialist for further evaluation and management.
Serology was positive for only the RPR (1:128) and FTA-ABS. The patient was admitted to the hospital for intravenous (IV) penicillin administration. Lumbar puncture was performed to rule out neuro-syphilis and cerebro-spinal fluid analysis was negative for treponemal spirochetes. The patient was co-managed with an infectious disease specialist and human immunodeficiency virus (HIV) testing was ordered, which yielded positive results. The CD4 count was 250 cells/mm3 and viral load was 120,215 copies/mL. Highly active anti-retroviral therapy (HAART) was also initiated during hospitalization.
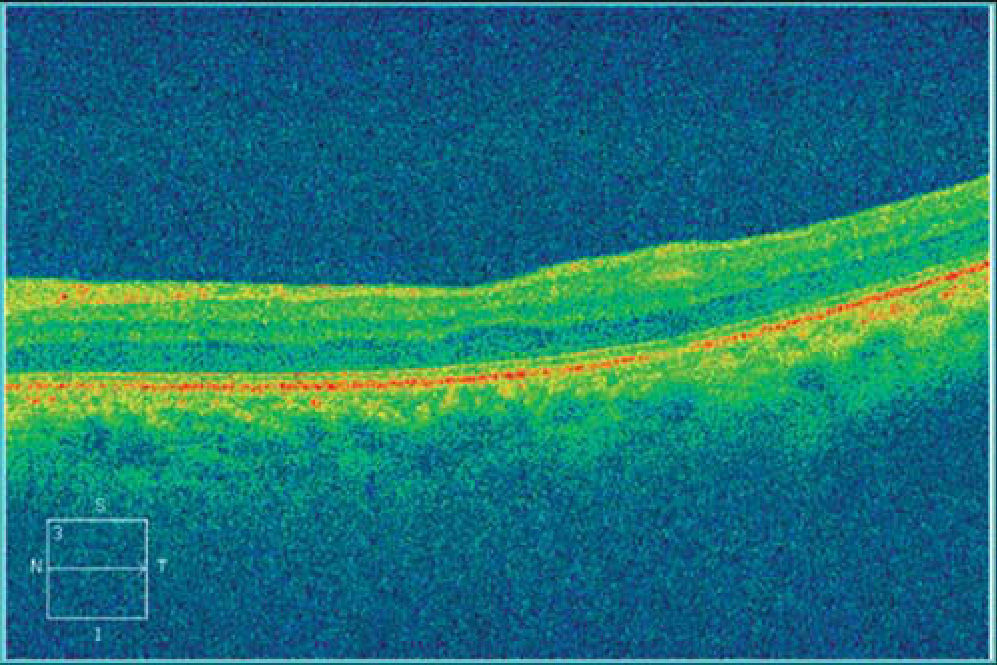
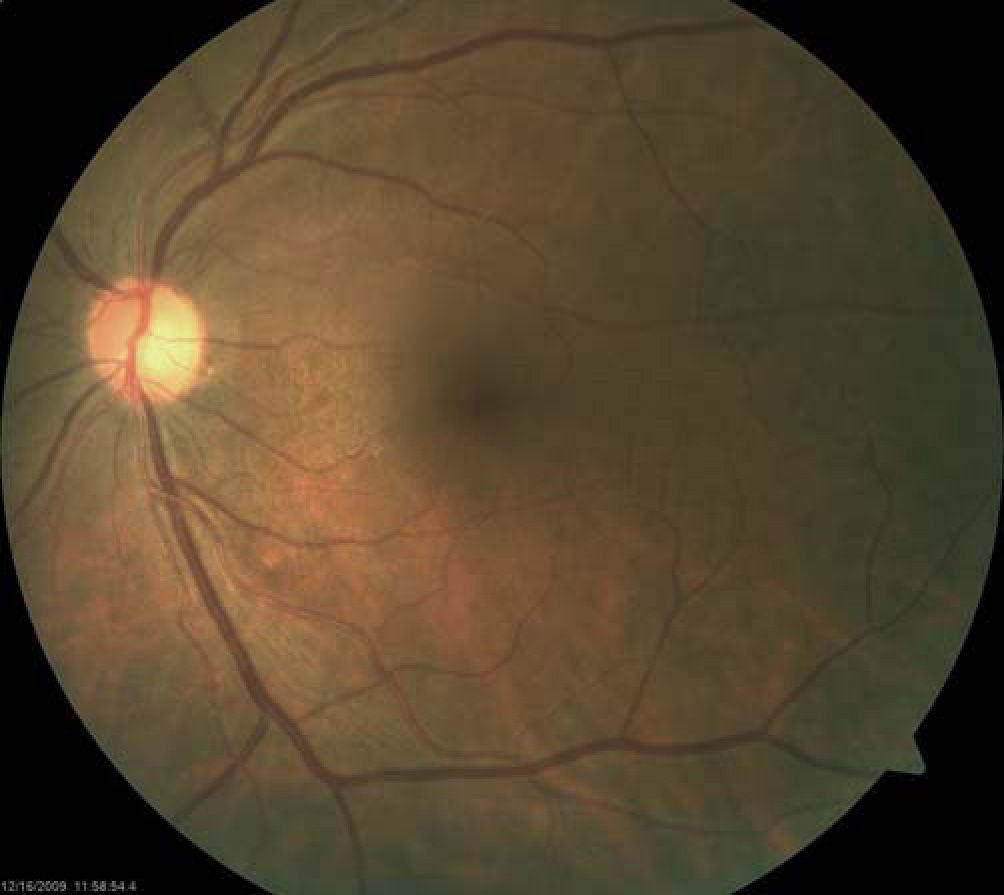
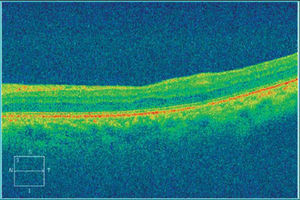
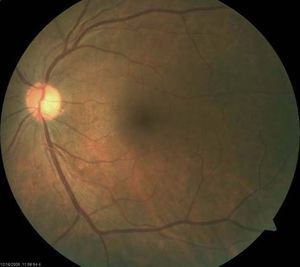
The patient returned two months after initial presentation. Best-correct visual acuity was 20/20 OD and 20/25+OS. Dilated fundus exam was normal in each eye, with no signs of vitreous cell or retinitis OU. CirrusTM HD-OCT OS was repeated and demonstrated resolved retinitis as evidenced by the decreased thickness of the inner retinal segments (Figures 3 and 4). The patient has remained stable over one year.
The clinical presentation of this patient appears typical of syphilitic ocular disease. Known as the “Great Imposter,” syphilitic ocular manifestations present a diagnostic dilemma by mimicking any type of inflammatory process.8 Several forms of syphilitic chorioretinitis have been reported: confluent, placoid and punctate. The confluent form presents with large confluent areas of retinal whitening.6 In 1990, Gass described the placoid type and coined the term “Syphilitic Posterior Placoid Chorioretinitis,” as a rare manifestation of ocular syphilis which causes acute vision loss in one or both eyes due to large placoid areas of chorioretinitis in the juxtapapillary or macular areas. These lesions are at the level of the retinal pigment epithelium and accompanied by vitritis.7 Punctate retinitis with inner retinal and pre-retinal white dots have also been described.6,10 Occasionally, serous retinal detachments have been found in association with retinitis.6
The pathogenesis of retinitis and chorioretinitis due to syphilis is unclear. One theory suggests that it reflects widespread dissemination, direct invasion and secondary obstruction of the choriocapillaris by spirochetes9,11 and that it involves the area adjacent to the retinal pigment epithelium.11 Another theory suggests it is due to deposition of soluble immune complexes in the tissues.11
Very few cases of syphilitic retinitis or chorioretinitis OCT findings are reported in the literature, and all use time domain OCT technology. Each case describes the preand post-treatment OCT findings of immunocompetent patients. The first were reported in 2007 by Joseph et al,12 and demonstrated increased thickening of the neuroretina and underlying layers with one case also having associated subretinal fluid. In both of these cases the chorioretinal architecture returned to normal after treatment with penicillin.12 Song and associates11 reported two cases of acute syphilitic posterior placoid chorioretinits following intra-vitreal injection of triamcinolone in patients treated for ocular inflammation without ruling out infectious causes prior to treatment.11 OCT showed subretinal fluid in both patients, with superficial retinal infiltrates in one patient. Despite appropriate treatment for syphilis, approximately six weeks after initial vision loss, the fundus became atrophic which resulted in poor visual outcomes.11 In 2009, Meira-Frietas et al13 reported OCT findings in an immunocompetent patient described as thickening of the foveal RPE-choriocapillaris band. This patient's OCT findings and vision returned to normal after treatment.13
Our case represents early syphilitic retinitis in an immunocompromised patient. In this instance, spectral domain OCT in the setting of early syphilitic retinitis shows inner layer involvement with sparing of the outer layers and photoreceptors, as evidenced by pre and post-treatment OCT findings. Early diagnosis and treatment is important to avoid outer layer involvement and decrease visual morbidity.
ConclusionsRetinitis as a feature of syphilitic uveitis in HIV infected individuals has been identified as a common clinical finding.5,6 Localizing the infection to the inner retinal layers utilizing spectral domain OCT technology may aid in determining potential visual outcome following prompt intravenous penicillin therapy. This case suggests that the inner retinal layers may be selectively involved with early syphilitic retinitis. Future investigation of similar cases should be performed to see if this is a reproducible finding.