The VX120 (Visionix Luneau, France) is a novel multi-diagnostic platform that combines Hartmann–Shack based autorefraction, Placido-disk based corneal-topography and anterior segment measurements made with a stationary-Scheimpflug camera. We investigate the agreement between different parameters measured by the VX120 with accepted or gold-standard techniques to test if they are interchangeable, as well as to evaluate the repeatability and reproducibility.
MethodsThe right-eyes of healthy subjects were included in the study. Autorefraction of the VX120 was compared to subjective refraction. Agreement of anterior segment parameters was compared to the Sirius (CSO, Italy) including autokeratometry, central corneal thickness (CCT), iridiocorneal angle (IA). Inter and intra-test repeatability of the above parameters was assessed. Results were analyzed using Bland and Altman analyses.
ResultsA total of 164 eyes were evaluated. The mean difference between VX120 autorefraction and subjective refraction for sphere, spherical equivalent (SE), and cylinder was 0.01±0.43D, 0.14±0.47D, and −0.26±0.30D, respectively and high correlation was found to all parameter (r>0.75) except for J45 (r=0.61). The mean difference between VX120 and the Sirius system for CCT, IA, and keratometry (k1 and k2) was −3.51±8.64μm, 7.6±4.2°, 0.003±0.06mm and 0.004±0.04mm, respectively and high correlation was found to all parameter (r>0.97) except for IA (r=0.67). Intrasession repeatability of VX120 refraction, CCT, IA and keratometry yielded low within-subject standard deviations. Inter-session repeatability showed no statistically significant difference for most of the parameters measured.
ConclusionsThe VX120 provides consistent refraction and most anterior segment measurements in normal healthy eyes, with high levels of intra and inter-session repeatability.
VX120 (Visionix Luneau, Francia) es una plataforma multi-diagnóstico novedosa que combina la auto-refracción basada en Hartmann–Shack, la topografía corneal mediante discos de Plácido, y las mediciones del segmento anterior realizadas mediante cámara de Scheimpflug. Analizamos la concordancia entre los diferentes parámetros medidos por VX120 con las técnicas aceptadas o de referencia, para probar si eran intercambiables, y evaluamos la repetibilidad y reproducibilidad.
MétodosSe incluyeron en el estudio los ojos derechos de sujetos sanos. Se comparó la auto-refracción de VX120 con la refracción subjetiva. La concordancia de los parámetros del segmento anterior se comparó con la del sistema Sirius (CSO, Italia), incluyendo autoqueratometría, espesor corneal central (ECC) y ángulo iridiocorneal (AI). Se valoró la repetibilidad inter e intra-prueba de los parámetros anteriores. Los resultados se analizaron mediante el método de Bland–Altman.
ResultadosSe evaluó un total de 164 ojos. La diferencia media entre la auto-refracción de VX120 y la refracción subjetiva para esfera, equivalente esférico (EE), y cilindro fue de 0,01±0,43D, 0,14±0,47D y −0,26±0,3D, respectivamente, encontrándose una elevada correlación entre todos los parámetros (r>0,75) excepto para J45 (r=0,61). La diferencia media entre VX120 y el sistema Sirius para ECC, AI, y queratometría (k1 y k2) fue de -3,51±8,64μm, 7,6±4,2°, 0,003±0,06mm y 0,004±0,04mm, respectivamente, encontrándose una elevada correlación entre todos los parámetros (r>0,97) excepto para AI (r=0,67). La repetibilidad intra-sesión de la refracción VX120, ECC, AI y queratometría reflejó desviaciones estándar bajas entre sujetos. La repetibilidad inter-sesión no reflejó una diferencia significativa para la mayoría de los parámetros medidos.
ConclusionesVX120 aporta medidas consistentes de refracción y de la mayoría de las mediciones del segmento anterior en ojos sanos normales, con elevados niveles de repetibilidad intra e inter-sesión.
Modern optometry and ophthalmology require the data from several instruments to offer the patient a complete ocular exam, especially when refractive or cataract surgery or contact lens fitting are going to be planned.1 This clinical procedure can be simplified using multi-diagnostic platforms that integrate several technologies in the same device to measure different anatomical and optical parameters of the eye.1 These types of diagnostic platforms facilitate a complete characterization of the corneal structure, including the analysis of the shape and optical aberrations of the two corneal surfaces, distribution of thickness and even a volumetric analysis of the cornea.1
The VX120 (Visionix Luneau, Chartres, France) is new non-invasive multi-diagnostic platform that combines refraction (Hartmann–Shack based autorefractometer),2,3 simulated keratometry (based on Placido disk videokeratography),3,4 non-invasive stationary Scheimpflug based pachymetry and Hartmann–Shack wavefront aberrometry as well as other functions not investigated in this study.4,5
One common issue with new instrumentation is to test its accuracy. Accuracy may be described by two terms: trueness and precision.6 Trueness refers to the closeness between the mean of many results and the true value. For measurements of the eye, there are few true or accepted reference values.6 Therefore, new instruments should be assessed for agreement with other existing instruments or gold standard tests. This concept is also called validity.7
Precision refers to the closeness between repeated measurement that are influenced by five factors: (1) Observer, (2) Instrument used, (3) Instrument calibration, (4) Environment and (5) Time interval between measurements.6 The concept of precision has two components: repeatability and reproducibility. Repeatability is the variability in which the above five factors are kept constant.6 This is also known as intra-test repeatability.7 Reproducibility is the variability when one or more of the above five factors vary.6 When time is varied, this is called inter-test repeatability.7
Piñero et al. (2017)4 evaluated the intra-test repeatability of several functions of the VX120 system in 107 healthy subjects and found that the device provides consistent measurements of keratometric measurements, corneal eccentricity, and third- and fourth-order corneal aberrations. Likewise, the same research group has demonstrated recently that the VX120 system is also able to provide consistent measurements of anatomical parameters of the anterior segment, such as anterior chamber depth, central and peripheral pachymetry and iridocorneal angle.5 However, validity has yet to be assessed for this device.
This study investigated the agreement of refraction, central corneal thickness, iridicorneal angle and keratometry of the VX120 system with accepted or gold standard techniques to test if they are interchangeable, as well as the repeatability and reproducibility of the measurements provided by the device.
MethodsThis prospective user masked project took place at Hadassah Academic College, Jerusalem, Israel.
SubjectsSubjects above 18 years old were recruited from the student body and staff of Hadassah Academic College and Dept. of Optometry clinics from 2014–2015. All examinations took place in the refraction clinics at Hadassah Academic College. Due to compliance issues, not all subjects participated in all exams, yielding a different cohort for each validation procedure (Table 1). However, the same cohort was used in each type of experiment. The methods and the nature of the experiment were orally explained to the participants prior to their participation and they signed a statement of informed consent. This project was approved by the Ethics committee of Hadassah Academic College and followed the Declaration of Helsinki. Subjects were compensated for their time and travel to the clinic.
Description of the cohort demographics for each experiment.
| Parameter (experiment number) | N | Average age (years) | Age range (years) | SE (D) |
|---|---|---|---|---|
| 1. Agreement and intra-test repeatability of refraction | 61 | 24.4±7.3 | 18–50 | −1.05±1.80 |
| 2. Inter-test repeatability of Refraction of VX120 and (subjective refraction) | 37a (41a) | 22.6±4.1 (22.3±3.9) | 19–38 (18–38) | |
| 3. Agreement and intra-test repeatability of CCT, IR, Keratometry | 103 | 23.2±5.0 | 18–47 | −1.44±2.20 |
| 4. Inter-test repeatability of CCT | 31b | 23.6±5.9 | 18–46 |
Subjects with systematic pathology, pregnant women, subjects with nystagmus, and subjects with any other corneal or conjunctival pathology or infection were excluded from the study. Subjects with contact lenses removed the lenses at least 12h before the study for hard lenses and 30min for soft lenses or until there are no signs of corneal warpage. Subjects with known epileptic history were also excluded.
ProceduresAll instrument measurements were performed per the manufacturer's guidelines. Instrument measurements were taken by qualified optometrists or optometry students trained in the use of each instrument. An examination including autorefraction, autokeratometry, central corneal thickness (CCT) and iridiocorneal angle (IR) measurements was performed using the VX120 system. The VX120 uses a very short flash of blue LED light with wavelength 450nm and with a constant power of approximately 50μW. It combines a Hartmann–Shack aberrometer, a Placido disk corneal topographer, a Scheimpflug imaging-based system and an air tonometer. The Placido disk system projects 24 rings on the corneal surface, measuring more than 100,000 points, and this information is used to provide all corneal topographic information. The Scheimpflug imaging-based system uses monochromatic blue light of 450nm to obtain pachymetric measurements with a resolution of ±10μm, and iridocorneal angle measurements with a resolution of ±1°. The Hartmann–Shack aberrometer of the VX120 system measures 1500 points in 0.2s in an area ranging from 2.0 to 7.0mm2 of diameter.
Besides measurements with the VX120 system, an examination was also performed with the Sirius system (Costruzioni Strumenti Oftalmici, CSO, Firenze, Italy). Subjects with abnormal findings were referred for further clinical evaluation and were excluded from the study.
Manifest refraction was performed by a single qualified optometrist (CK) who was masked to the results of autorefraction. In the agreement studies, exams were performed in a random order. Three measurements were obtained with the VX120 and Sirius systems, and the average was used in further analysis and for intra-test assessment of repeatability.
Only the right eye of each subject was used in all analyses.8 Inter-test (within 10 days after the initial objective measures) repeatability for each instrument (and for subjective refraction) was assessed on a subset of the original subjects, who were selected based on their willingness to comply with further testing. To avoid the effects of diurnal corneal thickness variations, these measurements were carried out at the same time of day, between 10am and 4pm.9
The different studies that were performed are summarized in Table 1. In each study, the same cohort of subjects was used.
Data analysisThe statistical analysis was performed using excel. Normality of all data distributions was confirmed by means of the Anderson–Darling test. Parametric statistics were used. Agreement and precision analyses were done using the Bland and Altman method10,11 which included calculation of the mean difference between the instruments, the standard deviation (SD) and the 95% limits of agreement (LoA=mean difference±1.96×standard deviation of the difference). Intra-test repeatability for different parameters was assessed by means of the following statistical variables: the within-subject standard deviation (Sw) of the 3 consecutive measurements, coefficient of repeatability (1.96×Sw×the square root of the number of measurements), and the intraclass correlation coefficient (ICC).
Sample size was calculated per the formulas recommended by McAlinden et al.6 For three repeated measurements (as in this study), sample sizes of 96, 43 and 24 subjects were required for a confidence in the estimate of 10%, 15% and 20%, respectively.
Student's t-test for paired data was used to assess the difference between variables and p-values of 0.05 or lower were considered as statistically significant.
Refraction notationThe spherocylindrical refractions obtained with the device as well as subjectively were converted to vectorial notation using the power vector method described by Thibos and Horner.12
ResultsOne hundred and sixty-four normal subjects (164 eyes) were enrolled in this study. Data from only the right eye was used in all analyses. In each part of the study, different samples of subjects were evaluated as summarized in Table 1.
Agreement of refractionA total of 61 subjects (19 men, mean age 24.4±7.3 years, range 18–50) participated in the refraction agreement study (VX120 autorefraction vs. subjective refraction). Their refractive error varied between −8.00D and +1.00D of sphere, and −1.75D and 0.00D of cylinder (mean spherical equivalent, −1.25±1.85D). Results from the VX120 for 3-mm pupils were used.
The mean difference (value±std dev) and correlation between the VX120 autorefraction and subjective refraction for sphere, spherical equivalent (SE), cylinder and astigmatic vectors J0 and J45 described in Table 2 and Fig. 1. The 95% LoA between the two methods of obtaining the refraction were +1.06 to −0.77D (or ±0.92D), +0.86 to −0.83D (or ±0.85D) and +0.32 to −0.84D (or ±0.58D) for the spherical, spherical equivalent and cylinder component, and +0.46 to −0.26D (or ±0.36) and +0.38 to −0.29D (or ±0.34) for J0 and J45, respectively (Fig. 1).
Precision of refraction: Mean values of the parameters measured by the VX120 and subjective refraction (N=61).
| Parameter (mean±SD) | VX120 | Subjective refraction | Mean difference | p | r |
|---|---|---|---|---|---|
| Sphere (D) | −0.91±1.75 | −1.05±1.80 | 0.01±0.43 | 0.02 | 0.97 |
| Cyl (D) | −0.65±0.40 | −0.39±0.44 | −0.26±0.30 | <0.01 | 0.75 |
| SE (D) | −1.24±1.78 | −1.25±1.85 | 0.14±0.47 | 0.82 | 0.97 |
| J0 | 0.15±0.03 | 0.05±0.02 | 0.10±0.18 | <0.01 | 0.87 |
| J45 | 0.01±0.02 | −0.04±0.02 | −0.05±0.17 | 0.04 | 0.61 |
Difference in (A) spherical component, (B) spherical equivalent, (C) cylindrical component and (D) J0 and J45 vectors between the VX120 and subjective refraction/the Sirius, plotted against the mean refractive error/mean cylindrical Component/mean of the J0 and J45 components respectively. Mean bias is indicated by the solid lines and the 95% limits of agreement by the dashed lines.
Approximately, 38% of the VX120 results were within ±0.25D and 69% within ±0.50D of the spherical components of the prescription found subjectively (Fig. 2A). For the spherical equivalent, 54% of the autorefraction readings were within ±0.25D and 77% within ±0.50D of the subjective refraction (Fig. 2B). For the VX120 cylinder components, 43% were within ±0.25D and 80% within ±0.50D of the subjective results.
The agreement between the axes of the cylindrical components is shown in Table 3. For all cylindrical powers, 74.4% of VX120 axes were within ±20° of those found subjectively, and for cylindrical powers of 0.75D or greater, 78.6% of VX120 axes were within ±20° of those found subjectively.
Comparison of the axis of the cylindrical component measured with the VX120 system and by subjective refraction.
| All prescriptions with a cylindrical component, n=39 (%) | Prescriptions with a subjective cylindrical component ≥0.75D, n=14 (%) | |
|---|---|---|
| ±5° | 9 (23.1) | 5 (35.7) |
| ±10° | 20 (51.3) | 8 (57.1) |
| ±15° | 26 (66.7) | 10 (71.4) |
| ±20° | 29 (74.4) | 11 (78.6) |
Intra-test repeatability for the VX120 system in terms of refraction showed small within-subjects standard deviation (see Table 4).
Intra-test repeatability for subjective refraction (N=61).
| Sphere (D) | Cylinder (D) | SE (D) | J0 | J45 | |
|---|---|---|---|---|---|
| Mean (SD) | −0.91 | −0.65 | −1.24 | 0.14 | 0.01 |
| SD | 0.16 | 0.10 | 0.15 | 0.06 | 0.05 |
| Sw (D) | 0.40 | 0.32 | 0.39 | 0.24 | 0.21 |
| Coefficient of repeatability | 1.35 | 1.10 | 1.33 | 0.80 | 0.72 |
| ICC | 0.995 (0.992–0.997) | 0.95 (0.923–0.968) | 0.995 (0.993–0.997) | 0.972 (0.958–0.982) | 0.970 (0.954–0.981) |
Abbreviations: SE, spherical equivalent; Sw, within-subject standard deviation; SD, standard deviation; ICC, intraclass correlation coefficient; J0 and J45, power vector components.
Inter-test repeatability for the refraction parameters were assessed for the VX120 system and subjective refraction on a subset of the original cohort of 37 and 41 patients, respectively (Table 5). No statistically significant difference was observed between the first and the second session for sphere, cylinder and spherical equivalent parameters for the VX120 system and for all subjective refraction parameters (Table 5).
Inter-test repeatability for subjective refraction (N=41) and the VX120 (N=37).
| Intertest | Sphere (D) | Cylinder (D) | SE (D) | J0 | J45 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| VX120 | Subj | VX120 | Subj | VX120 | Subj | VX120 | Subj | VX120 | Subj | |
| Mean difference | −0.03 | −0.01 | −0.03 | −0.01 | −0.05 | −0.01 | 0.03 | 0.03 | 0.03 | 0.00 |
| SD of difference | 0.28 | 0.07 | 0.11 | 0.15 | 0.27 | 0.10 | 0.06 | 0.07 | 0.04 | 0.07 |
| p value | 0.47 | 0.57 | 0.09 | 0.60 | 0.26 | 0.44 | 0.01 | 0.36 | 0.00 | 0.84 |
Abbreviations: Subj, Subjective refraction; SE, spherical equivalent; Sw, within-subject standard deviation; SD, standard deviation; ICC, intraclass correlation coefficient; J0 and J45, power vector components. p value represents the difference between 1st and 2nd session.
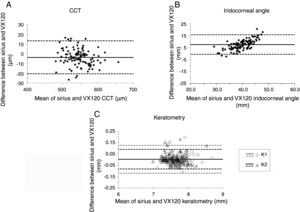
A total of 103 subjects (20 men, mean age 23.2±5.0 years, range 18–47) participated in the validation study comparing CCT, IR and keratometry between the VX120 and the Sirius systems (Table 6). Their refractive error varied between −9.13D and 4.51D of sphere, and −2.56D and −0.09D of cylinder (mean spherical equivalent, −1.44±2.20D). The results (Table 6, Fig. 3) show no statistically significant difference between the instruments for keratometry measurements.
Precision of central corneal thickness (CCT), Iridocorneal angle (IA) and K readings: Mean values of the parameters measured by the VX120 and the Sirius (N=103).
| Parameter (mean±SD) | Sirius | VX120 | Mean difference | p | r |
|---|---|---|---|---|---|
| Sim K1 (mm) | 7.73±0.02 | 7.73±0.04 | 0.003±0.06 | 0.60 | 0.97 |
| Sim K2 (mm) | 7.59±0.02 | 7.59±0.04 | 0.004±0.04 | 0.34 | 0.98 |
| Mean CCT (μm) | 543.9±2.7 | 547.5±6.5 | −3.51±8.64 | <0.01 | 0.99 |
| IA (°) | 43.5±1.0 | 36.0±0.7 | 7.6±4.2 | <0.01 | 0.67 |
The average thickness was 547.5±6.5μm and 543.9±2.7μm for VX120 and Sirius, respectively. The average difference between the two instruments (3.51±8.64) was statistically, but not clinically significant (p<0.01, see Table 6). For IR, the average difference for IR was both clinically and statistically significant (7.6±4.2, p<0.01). Fig. 3 shows the Bland–Altman comparative analysis of VX120 and Sirius measurements.
Intra-test repeatability for the VX120 system (n=103) showed relatively low within-subjects standard deviations (Sw) for all parameter measured (Table 7).
Intra-test (N=103) and inter-test (N=31) repeatability for central corneal thickness (CCT), Iridocorneal angle (IA) and K readings.
| CCT (μm) | IA (°) | Sim K1 (mm) | Sim K2 (mm) | |||||
|---|---|---|---|---|---|---|---|---|
| VX120 | Sirius | VX120 | Sirius | VX120 | Sirius | VX120 | Sirius | |
| Intratest | ||||||||
| Mean (SD) | 547.5 | 543.9 | 35.97 | 43.54 | 7.73 | 7.73 | 7.59 | 7.59 |
| SD | 6.45 | 2.70 | 0.72 | 0.98 | 0.04 | 0.02 | 0.04 | 0.02 |
| Sw (D) | 2.54 | 1.64 | 0.85 | 0.99 | 0.19 | 0.15 | 0.20 | 0.14 |
| Coefficient of repeatability | 8.62 | 5.57 | 2.88 | 3.36 | 0.64 | 0.50 | 0.68 | 0.48 |
| ICC | 0.983 (0.976–0.988) | 0.997 (0.995–0.998) | 0.939 (0.916–0.957) | 0.973 (0.963–0.981) | 0.988 (0.983–0.991) | 0.992 (0.989–0.994) | 0.984 (0.978–0.989) | 0.997 (0.995–0.998) |
| Intertest | ||||||||
| Mean difference | 0.04 | 1.24 | 0.07 | −0.26 | −0.005 | 0.021 | −0.014 | −0.002 |
| SD of difference | 7.90 | 6.49 | 1.19 | 2.08 | 0.04 | 0.07 | 0.04 | 0.03 |
| p value | 0.98 | 0.29 | 0.74 | 0.49 | 0.46 | 0.11 | 0.05 | 0.77 |
Abbreviations: Sw, within-subject standard deviation; SD, standard deviation; ICC, intraclass correlation coefficient. p value represents the difference between 1st and 2nd session.
A subset of the original cohort, 31 subjects (31 eyes, 9 men, 22 women) repeated measurements of both the VX120 and Sirius. Subjects’ mean age (±SD) was 23.6±5.9 years (range 18–46). Refractive error for these normal subjects varied between −9.13D and 3.10D of sphere, and between −2.07D and −0.14D of cylinder (mean spherical equivalent, −1.52±2.70D). High inter-test repeatability was demonstrated for most parameters measured (see Table 5).
DiscussionThis is the first validation study of the VX120. In terms of the agreement between objective refraction measurements provided by the VX120 system and subjective refraction, there was no clinically significant bias between the results of the VX120 and subjective refraction for either the spherical component or the spherical equivalent of the prescription (0.01D, p=0.02; 0.14D, p=0.82, respectively). These results are consistent with those reported in other previous studies comparing subjective and objective refraction using different devices.2,18–24 In this study, there was good agreement between objective and subjective refraction technique, with 38% and 54% of eyes with sphere and SE within ±0.25D of that found by non-cycloplegic subjective refraction, and 69% and 77% within ±0.50D. These results are consistent with those obtained in previous studies evaluating other devices providing objective refraction.2,19 The bias for the cylindrical component was also small (−0.26D) and consistent with the results of other previous studies.21,24 A statistical significant difference was found for astigmatic power vectors J0 and J45 (p<0.01 and 0.04, respectively), but the mean difference compared to subjective refraction values was very low and not clinically relevant (0.10 and −0.05D, respectively).
The VX120 system provides consistent measurements of refraction, with SW values for intra-test repeatability analysis below 0.40D and ICC of 0.970 or higher. These results are similar to those reported in other studies evaluating intra-test repeatability of other devices providing automatic refraction.13–23 Segura and coauthors15 evaluated in healthy eyes the intra-test repeatability of refractive measurements provided by an autorefractometer (WAM-5500, Grand Seiko Co.) and a ray tracing aberrometer (iTrace, Tracey Technologies) and found ICC values of 0.999 and 0.904 for sphere and cylinder with the autorefractometer, and values of 0.998 and 0.939 with the aberrometer. Prakash and coauthors14 evaluated the consistency of refractive measurements provided by a new generation Hartmann–Shack aberrometer (iDesign, Abbott Medical Optics), finding Sw values of 0.25 and 0.08D, respectively. Besides the good intra-test repeatability of refractive measurements obtained with the VX120 system, the inter-test performance was also shown to be good in our study, with standard deviation of differences between measurements of 0.28D or below. Therefore, our results confirm that the VX120 system is able to provide consistent measurements of refraction.
Regarding the analysis of corneal curvature, the results of agreement and repeatability are similar to other studies which compared autokeratometer to the gold standard (Bausch and Lomb keratometer).3 In this study, there were no significant differences in keratometry between the VX120 and Sirius systems. The LoAs found were also acceptable, with values from −0.12 to 0.13mm (or ±0.12) and from −0.08 to 0.09mm (or ±0.09) mm for K1 and K2, respectively, which are similar and even smaller than those reported in other studies comparing technologies of measurement of corneal curvature.3,22,25–28 Piñero et al. (2017)4 found similar results when they evaluated the intrasession repeatability of keratometry measurements for the VX120. These authors obtained Sw below 0.26D for keratometric measurements, with ICC above 0.982.
This study evaluated whether the CCT and IA measurements obtained with the VX120 system can be used interchangeably with those obtained with another Scheimpflug imaging system (Sirius). For CCT, the average difference between the two instruments (3.51±8.64μm) was statistically, but not clinically significant (p<0.01, see Table 6). For IR, the average difference for IR was both clinically and statistically significant (7.6±4.2, p<0.01). Furthermore, the consistency of CCT and IA measurements was good, with Sw values of 2.54μm and 0.85°, respectively. The same level of consistency was found with the Sirius system for both parameters, confirming that both instruments provide consistent measurements of CCT and IA, with similar level of accuracy. The results of this study confirm previous results on the consistency of pachymetric and IA measurements obtained with the VX120 system.5
Several studies evaluating have obtained similar or even worse Sw values for CCT with the Sirius system (Prakash et al.29 Sw: 5μm; Montalbán et al.30 Sw: 2.80μm; Chen et al.31 Sw: 3.10μm) and optical biometry systems (Zhao et al.32 Sw: 14.24μm; Kunert et al.33 Sw: 19.5μm). Likewise, the level of intra-session repeatability obtained for IA with the VX120 was consistent with that reported for other devices.34,35 The LoAs between Sirius and VX120 systems for CCT were clinically acceptable, confirming that these two devices can be used interchangeably for the measurement of such parameter. In contrast, the difference between instruments in IA was statistically significant and LoAs can be considered as clinically relevant, with the presence of differences up to 15°. Possibly, the VX120 and Sirius systems use different algorithms and graphical approaches for defining and estimating numerically the IA.
There are some limitations in the current study. The same cohort of subjects was not used for each experiment. However, this does not impinge on the results since each experiment in itself used the same cohort of subjects. The confidence in the estimation was higher (15–20%) for some of the experiment, due to a smaller sample size.
In conclusion, the VX120 provides consistent measurements of refraction, keratometry, CCT and IA in normal healthy eyes, with high levels of intra and inter-session repeatability. The measurements of objective refraction are in agreement with those obtained by subjective refraction in most of cases. The VX120 and Sirius systems can be used interchangeably to measure CCT and keratometry, but the measurement of IA can differ significantly between both instruments.
Conflicts of interestThe Dept. of Optometry at Hadassah Academic College received a grant from Visionix (Luneaux, Fr) to compensate participants for their time and travel. In addition, Visionix provided the Dept. of Optometry with a long term loan of a VX120 instrument.
David P Piñero received a grant from Visionix (Luneaux, Fr) for the performance of a study with the VX120 system at the University of Alicante.
Tzadok Parnas received a salary from Visionix for logistic administration of some of the experiments.
We would like to thank Dr. Gary Roth, Dr. Rachel Eichler, Dr. Rema Shabany-Khayat, Dr. Kenneth Koslow as well as Ravid Doron, Haim Wertzer, Hadas Eichenstein, Noga Bromberger Reut Ifrah and Meron Tepara and Yishai Gordon for data acquisition. The Dept. of Optometry at Hadassah Academic College received a grant from Visionix (Luneaux, Fr) to compensate participants for their time and travel. In addition, Visionix provided the Dept. of Optometry with a long-term loan of a VX120 instrument.