Evaluate the performance of a photochromic contact lens in various lighting conditions throughout the day, including those indoor and outdoor environments where the photochromic contact lens is in a less active or inactive state.
MethodsData from two clinical trials of a photochromic contact lens were analyzed to evaluate its performance in various light environments. Both studies involved a photochromic test lens (ACUVUE® OASYS with Transitions™ Light Intelligent Technology™) and a similar non-photochromic control lens (ACUVUE® OASYS 2-week with HYDRACLEAR® PLUS). The studies were both multi-visit, multi-site, 2-treatment by 3-period randomized crossover (i.e., Test/Control/Control or Control/Test/Test) dispensing studies, with follow-up visits after each 2-week dispensing period.
ResultsA total of 250 subjects were dispensed lenses across both studies, of which 237 total subjects completed. In situations where exposure to an activating light source is common (e.g., outdoors), the Test lens was preferred nearly 6:1 over the control lens. In situations where exposure to an activating light source is less common – indoors, driving at night, using digital devices –, the Test lens was still preferred over the control lens by margins of 4:1, nearly 4:1, and over 3:1 respectively. The Test lens was superior with respect to quality of vision, ability to see comfortably, clarity of vision, reduction of squinting while using computers and reduction of bright light while driving at night.
ConclusionThe photochromic test contact lens was rated superior to a non-photochromic control lens in environmental situations where the lens is in a less active or inactive state.
The glass photochromic variable light filter was invented in the 1960s,1 becoming commercially available as a plastic lens in 1991 when Essilor International introduced the Transitions® spectacle lens. This was widely adopted as both a visual performance-enhancing lens and protection against ultraviolet (UV) and high energy visible (HEV) light.2,3
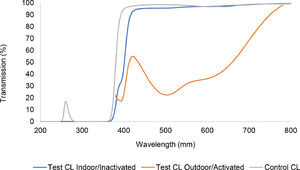
More recently, photochromic technology has been introduced to contact lenses by Johnson & Johnson as ACUVUE® OASYS with Transitions™ Light Intelligent Technology™ (AOwT), which uses the senofilcon A silicone hydrogel material. The lens on eye dynamically changes from ‘inactive’, as a pale blue-greyish tint with a minimum 85% visible light transmission (380–780 nm), to ‘active’, darkening to a minimum of 30% visible light transmission in response to the level of UV and HEV light exposure (Fig. 1).4
A range of psychometric studies has been undertaken with the AOwT lens to evaluate visual function under various conditions.5-8 These studies have been published elsewhere and will serve as the scientific foundation for the subjective responses presented here. As anticipated, the activated lens provides significant visual advantages in bright light conditions (e.g., disability glare, discomfort glare, photostress recovery). More surprisingly, improvements in visual function have also been noted in normal and low light conditions with inactivated AOwT lenses. In a contralateral study, measures of positive dysphotopsia (e.g., halo and starburst diameters) were significantly reduced with the photochromic lens, even in the inactivated state.6 The authors noted that, even when inactivated, the lens absorbs light in the short wavelength visible region – as much as 60% at 400 nm. Since high energy visible light is known to have an exaggerated effect on visual function,3,9-15 especially light scattering, effects of glare, retinal contrast, and visual discomfort, absorbance at these wavelengths are disproportionately important.
The question arises whether these measurable psychometric improvements under laboratory conditions translate to subjective improvement in normal usage. The purpose of this study, therefore, was to evaluate the subjective performance of the AOwT photochromic contact lens in varying light conditions, particularly normal and low light conditions. Data from two studies were reviewed and combined to analyze the performance of photochromic contact lenses not just in bright outdoor light but also indoors and under nighttime low-lighting conditions.
Materials and methodsSubjective data were combined from two clinical studies that compared a photochromic Test contact lens (AOwT) with a non-photochromic equivalent as the Control lens (ACUVUE® OASYS 2-week with HYDRACLEAR® PLUS, ACUVUE OASYS, AO). The studies were registered at ClinicalTrials.gov and received the identifiers NCT03228212 and NCT03679741. Both studies were randomized, controlled, multi-site, 2-treatment by 3-periods crossover studies conducted within a year of each other. In both studies, subjects wore lenses for a series of 2-week wearing periods, with follow-up visits for subjective questioning after each period. Subjects were masked to the control lens only and randomized bilaterally in blocks of two using permuted block randomization to one of two wearing sequences: Test/Control/Control or Control/Test/Test. Study-responsible biostatisticians generated the randomization schemes separately for each study using the PROC PLAN procedure from SAS Software Version 9.4 (SAS Institute, Cary, NC).16,17 To enable masking, all lens packages were over-labelled so that, apart from the randomization code, all packages were identical. Note that it is impossible to double-mask in this type of study since the subject quickly realizes which lens is photochromic and which lens is not. Masking the control lens, however, prevents potential bias if that lens happens to be their habitual brand.
All subjects were adapted wearers of spherical silicone hydrogel soft contact lenses and were in the age range of 18–49 years (inclusive). Subjects also had vertex-corrected spherical equivalent refraction in the range −1.00 D to −6.00 D and best corrected visual acuity of 20/25 or better in each eye.
Lens fit was checked prior to dispensing lenses for each period, and all dispensed lenses demonstrated a 0.00 D spherical over-refraction. Subjects were advised to wear the study lenses for at least five days per week and six hours per day over a period of 2 weeks. Presbyopic subjects were allowed to wear reading glasses over the contact lenses. Each of the three periods of lens wear involved a follow-up assessment visit approximately 2 weeks after lens dispensing. An electronic questionnaire (BioClinica, Princeton, NJ) was used to record subjective responses, and subjects responded to those questions privately and at their own pace.
The primary endpoints were subjective assessments of lens preference and ratings of visual performance indoors, outdoors, while using digital devices and while driving. The individual questionnaire items are detailed in Table 2. The preference response options were: Strongly prefer the first study contact lenses that I wore, Prefer the first study contact lenses that I wore, No preference, Prefer the second study contact lenses that I wore, Strongly prefer the second study contact lenses that I wore. The subjective assessment response options were: 1: Excellent, 2: Very good, 3: Good, 4: Fair, 5: Poor. A ‘not applicable’ option was also available. Each subject could select only one response option per question.
The studies were conducted in accordance with the Declaration of Helsinki and Good Clinical Practice Guidance. Enrolled subjects provided written informed consent before any study-related procedures and the studies were approved by the appropriate Ethics Committee (Sterling IRB; IDs: 5952C and 6435C).
Statistical analysisThe analysis population consisted of subjects that had data at the 2-week follow-up, and subjects were grouped by the treatment that they received. Subjective responses for each preference item were analyzed jointly using a Bayesian multinomial model for nominal data. Results were reported as posterior mean proportions and preference ratios of preferring the Test lens over the Control lens and 95% credible intervals. Other individual questions were analyzed jointly using a Bayesian random-effects multinomial model for ordinal data. However, due to the low incidence rate within the fair and poor response categories, these were collapsed into one response. Results were reported as posterior mean proportion estimates and odds ratios and 95% credible intervals. All statistical analyses were performed using SAS software version 9.4 (SAS Institute, Cary, NC).15,16
ResultsSubject accountability is shown in Fig. 2. The first study completed 127 subjects across five investigational sites, while the second completed 110 subjects across six sites. Of the 11 sites, two of them participated in both studies, resulting in nine unique sites that enrolled approximately 20 subjects each. All sites were the offices of eye care professionals in the United States. In total, 259 subjects were enrolled, but nine were not dispensed lenses; the remaining 250 were dispensed at least one study lens, but 11 such subjects were discontinued before data collection; a further two were later discontinued, but their data were used in the analysis of this report (n = 239); 237 subjects completed the study; and 229 were considered cohort.
Two-week enrolment periods followed by study visits were conducted during July 14 to September 18, 2017 and August 29 to October 31, 2018 for the two studies, respectively.
Table 1 summarizes baseline demographics and clinical characteristics of the overall sample population.
Demographics and clinical characteristics.
SD: Standard Deviation.
There were six ocular adverse events in this study, two that occurred with the Test lens and four that occurred with the Control lens. The two occurring with the Test lens were classified by the investigator as non-significant and possibility related to the Test lens and included: corneal oedema in one eye and an infiltrative event in one eye. The four occurring with the Control lens were also classified by the investigator as non-significant and unlikely or possibility related to the Control lens, and included: bacterial conjunctivitis of three eyes, and an external hordeolum of one eye. All adverse events resolved without complication.
Subjective assessment questionnaireTo avoid confusion of outdoor light versus indoor light (both can be bright or dim luminance), the data are separated into those bright light conditions where the photochromic lens is likely to be activated and those normal or low light conditions where activation is less likely (Table 2). In each of the 14 subjective items, the proportion of subjects rating lenses ‘very good’ or ‘excellent’ was significantly higher with the test than the control lens, regardless of the lighting environment.
Odds ratio estimates for subjective responses to the test (AOwT) versus control (AO) lens under various lighting conditions.
For overall quality of vision, the proportion of subjects rating lenses ‘very good’ or ‘excellent’ was 85% for the test lens compared with 73% for the control lens. One of the largest differences was for ‘reduction of squinting while using digital devices’: 71% and 51% rated this ‘very good’ or ‘excellent’ for the test and control lenses, respectively. There was also a large difference for ‘ability to see comfortably in bright indoor light’: 83% and 69% rated this ‘very good’ or ‘excellent’ for the test and control lenses, respectively. The item relating to driving at night showed a large difference: 66% and 37% for the test and control lenses, respectively.
The odds ratios of having a more positive experience/rating of the Test lens over the Control lens are summarized in Table 2. Since the lower limits of each 95% credible intervals were above one, all ratios are significant. The largest odds ratio estimate was for ‘ability to see comfortably in bright sunlight’ at 5.24, meaning that subjects were over five times more likely to experience a benefit with the Test lens than with the Control lens.
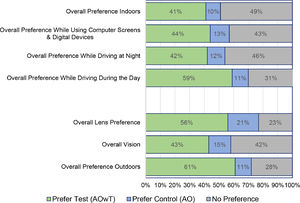
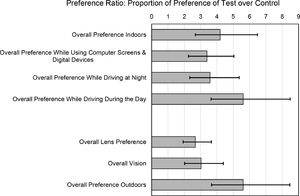
Lens preferenceThe preference data are summarized in Fig. 3 (‘strongly prefer’ and ‘prefer’ have been collapsed into ‘prefer’ for simplicity). A majority of subjects preferred the Test lens compared to the Control with respect to: overall lens preference (56.1%), overall preference outdoors (61.1%) and overall preference while driving during the day (58.6%). A large proportion of subjects (>40%) also preferred the test lens with respect to the other four items: overall vision, overall preference indoors, overall preference while driving at night, and overall preference while using computer screens and digital devices.
The preference ratios of the proportion of preference for Test over Control lenses (i.e., among those with a preference) are shown in Fig. 4. The Test lens demonstrated superiority relative to the Control with respect to all seven preference items since the lower limit of each 95% credible interval was above 1. The preference ratios ranged from 2.7 to 5.6. ‘Overall preference outdoors’ and ‘overall preference while driving during the day’ showed the strongest trends. Importantly, the preference ratios indicate significant benefits in normal and low light environments such as ‘overall preference indoors’ (4.2:1), ‘overall preference while driving at night’ (3.6:1), and ‘overall preference while using a computer’ (3.4:1). It is an interesting exercise whether to consider ‘overall preference while driving during the day’ an outdoor or indoor activity. Given that automobile windscreens block most of activating UV/HEV light entering the vehicle (although the side windows filter less),18 it is considered an indoor activity to the Test lens where it still provided a significant 5.6:1 preference ratio benefit for daytime driving.
DiscussionExpected bright light benefitsIt is natural to assume that filtering light in bright environments will provide a visual benefit given the common use of sunglasses. These benefits were evaluated using both psychometric and subjective clinical studies.
Psychometric evaluations of AOwT under bright light conditions have been published elsewhere and are not the focus of this paper.5 To summarize, the activated AOwT lens resulted in a 43% faster photostress recovery time, 39% less squinting, ability to handle 27% brighter light, 32% improved chromatic contrast, 48% reduction in halo diameter, 42% reduction in starburst diameter, and 37% reduction in two-point light threshold over the ACUVUE OASYS Control lens.
Subjective responses relating to outdoor activities during the day, understandably, favored the photochromic lens. Indeed, the Test lens dynamically reduces the amount of visible light entering the eye in all conditions, while the Control lens constantly has high light transmission. AOwT was preferred and rated higher than the control with respect to its performance: outdoors, in bright sunlight, while driving during the day, and its overall visual performance. The measured psychometric items help explain the strong subjective performance.
Normal or low light benefitsVisual benefits were also evident in less obvious lighting situations, where the photochromic molecules in the AOwT lens would be in an inactivated or less active state but still providing a useful visual filter. Even in the inactivated state, AOwT filters a significant amount of HEV below 420 nm (Fig. 1). It is well known that light scatters more readily at the violet end of the visible spectrum than at the red end of the spectrum.19 This creates a natural skewness in deleterious visual effects towards the violet end of the spectrum, and filtering light in this region, therefore, has a disproportionate benefit over filtering at the red end of the spectrum. Beyond the reduction of light scattering, the benefits of HEV-filtering have been extended to a decrease in the effects of glare, an increase in retinal contrast, and an increase in visual comfort.3,9-15
As noted earlier, psychometric evaluations of AOwT under low light conditions have been presented elsewhere,7,8 and the results are summarized in Table 3. There are several key benefits: first, there are significant improvements in visual performance metrics, even when the lens is not in the presence of an activating light source. For example, the diameter of halos and starburst are reduced by about 20% on average in dim lighting, which is important to night driving. The favorable result with respect to night driving was unexpected but consistent with a previous study of driving performance with AOwT.20 When compared to a non-photochromic contact lens in controlled driving conditions, the AOwT was non-inferior to the control lens for a wide range of driving tasks in low as well as high illumination. Interestingly, the AOwT lens performance was superior for nighttime sign recognition, and the sign recognition distance was improved by 19%. Consistent with previous reports,21 the authors speculated that mild improvements in low illuminance visual acuity and contrast sensitivity may have contributed to this finding.
Another finding was the apparent improvement in aspects of visual comfort when using digital devices. Glare and discomfort associated with digital devices is an increasingly common problem and has a significant economic and productivity cost.22,23 While using computers and digital devices (typically in the inactivated state), the AOwT lens was rated statistically superior to the ACUVUE OASYS Control lens for the ability to see comfortably, clarity of vision, and reduction of squinting. This was corroborated with a 3:1 preference for the AOwT lens over the ACUVUE OASYS lens for use with digital devices. To emphasize, these bright/normal/low light findings are clinical and statistical advantages over ACUVUE OASYS, which is the leading reusable spherical lens fit for all-day everyday use.24
The main limitation of the current studies is that the questionnaire has not been tested for validity; however, the results of subjective performance are consistent with previous objective visual performance studies. An additional limitation was that investigators were not masked to the lens types, which introduces a risk of bias. Similarly, the studies masked subjects to the control lens but were unable to mask the Test lens since subjects quickly realize whether or not they are wearing a photochromic contact lens. Nonetheless, masking the control lens prevents bias among any subjects who use that lens as their habitual lens. As for future studies, investigators could examine the lens among subjects who are particularly sensitive to bright lights.
ConclusionsIn summary, the photochromic Test contact lens was compared to a similar non-photochromic lens and showed visual benefits in lighting situations where such results are not obvious, such as: indoors, while using digital devices, and when driving at night. These benefits may provide a useful visual enhancement in varying lighting conditions experienced throughout the day and night.
FundingThis work was supported by Johnson and JohnsonVision Care, Inc. JJVC was involved in the study design, analysis, interpretation, and report. Data collection was performed entirely external by independent eye care professionals.
The authors would like to thank Hongzhi Guo for management of the clinical studies in this paper. The authors would also like to thank Nathan Greenaway of Visioncare Research Ltd for helping with manuscript preparation.
Journal: Journal of Optometry
ClinicalTrials.gov Identifiers: NCT03228212 and NCT03679741.