In 2019, an international survey was conducted to evaluate strategies and attitudes in the management of myopia in clinical practice worldwide. This study reports on the results found in Spain and how these results compare with those from other regions of the world.
MethodsA self-administrated, internet-based questionnaire was distributed to eye care professionals around the world through professional associations. The questions examined were based on the available strategies and their use.
ResultsA total of 173 Spanish optometrists, of the 1,336 practitioners from the five different continents who participated in the study, responded to the online survey. Spain, Asia and South America were found among the regions with the highest concern regarding the increased incidence of myopia (p ≤ 0.001). However, in these regions, the prescription of single-vision spectacles and single-vision contact lenses continues to be the main methods of visual correction prescribed to young myopic patients (p ≤ 0.001). Spanish practitioners, like those from other regions, considered orthokeratology to be the most effective treatment to control myopia progression (p ≤ 0.001). The major reasons why Spanish practitioners were not prescribing myopia control strategies were increased cost, inadequate information and unpredictable outcomes (p < 0.05).
ConclusionsThe uptake of myopia control methods by Spanish practitioners is relatively low, despite the increase in the prevalence of paediatric myopia as well as increased concern and perceived clinical activity in the area in recent years.
The prevalence of myopia has increased substantially over the last few decades. It currently affects around 34% of the global population and it has been estimated that its prevalence will continue to increase to affect 50% of the world population by the year 2050.1 In Spain, the prevalence of myopia in children has also increased substantially over the past two decades. In 2000, a cross-sectional study conducted in 7,621 Spanish subjects reported a prevalence of myopia of 2.5% for the age range of 3 to 8 years.2 More recently, an epidemiological study conducted between 2016 and 2019 in 7,497 Spanish children aged 5 to 7 years old found that the prevalence of myopia increased from 17% in 2016 to 19% in 2019.3
Several treatments options are currently being prescribed for the purposes of reducing myopia progression in children, including optical, pharmacological and behavioural interventions4–6 and recent guidelines have been proposed to inform eye care practitioners as to the expected level of efficacy of the different treatment options and on how to best implement these treatments in clinical practice.7,8
Nowadays, it is not clear how these treatments are being used in clinical practice. For this reason, in 2015 a questionnaire was distributed to eye care practitioners around the world through professional associations to obtain information with regards to practitioners' awareness in relation with the increase in the prevalence of myopia, the perceived efficacy of the different myopia control methods and the level of usage of these strategies, as well as the reasons why myopia control approaches may not be not prescribed.4 Due to the rapid changes and developments in this area, the same survey was distributed again to practitioners around the world in 2019.5 In this later study, in which 1,336 practitioners participated, it was found that despite growing concern about the increase in myopia in clinical practice as well as increased level of clinical activity in myopia control with respect to the previous questionnaire distributed in 2015, the vast majority of eye care practitioners continue to prescribe distance single-vision spectacles to young myopic patients.4,5 In the present study, an in-depth evaluation of the results obtained from the 173 Spanish practitioners that participated in the study are reported and compared with those obtained from other parts of the world.
MethodologyStudy design and data collectionThe methods used in this study have been previously explained in detail.4,5 Shortly, a questionnaire in eight languages (i.e., Chinese, English, French, German, Italian, Portuguese, Russian and Spanish) was distributed via the Internet using SurveyMonkey software (Palo Alto, California, USA), through various professional bodies to reach eye care professionals across the world (opticians, optometrists, ophthalmologists, and others). In Spain, the questionnaire was disseminated by email to all registered Optician-Optometrists in the country through the Spanish General Council of Spanish Optician-Optometrists. The questionnaire comprised the following nine questions:
- 1.
Level of concern about the increase in the incidence of paediatric myopia in clinical practice (quantified between “not at all” and “extremely” concerned on a 10-point scale).
- 2.
Perceived effectiveness, defined as the expected level of reduction in the progression of paediatric myopia of several clinical options for myopia control (quantified as a percentage from 0 to 100%).
- 3.
How activate they would consider their clinical practice in the area of myopia control (quantified between “not at all” and “completely” on a 10-point scale)
- 4.
Frequency with which different methods of myopia correction are prescribed to young/progressive myopic patients on an average month.
- 5.
Minimum patient age to consider the prescription of a myopia control method (assuming that the management skills and motivation of the child/parent are sufficient).
- 6.
Minimum level of myopia that would need to be present to consider prescribing a myopia control method (specified in 0.50D steps)
- 7.
Minimum level of myopia progression (dioptres/year) that would prompt a practitioner to specifically adopt a myopia control approach (specified in 0.25D steps).
- 8.
Frequency with which single-vison under-correction is being prescribed as a strategy to slow the progression of myopia (stated as “no”, “sometimes” or “always”).
- 9.
-If they had only ever fitted single-vision spectacles/contact lenses to myopic patients, what had prevented them from prescribing alternative refractive correction methods? The options (multiple options could be selected) consisted of:
- •
They don't believe that these are any more effective
- •
The outcome is not predictable
- •
Safety concerns
- •
Cost to the patient makes them uneconomical
- •
Additional chair time required
- •
Inadequate information/knowledge
- •
Benefit/risk ratio
- •
Other
- •
Although voluntary participation in the survey was anonymous, respondents were asked to provide basic demographic information about themselves, such as years of being qualified (grouped in six categories: 0, 0–5, 6–10, 11–20, 21–30, ≥31 years) and everyday working environment (i.e., clinical practice, academia, industry or other). The results obtained were grouped into five large regions (i.e., Asia, Australasia, Europe [without Spain], North America and South America) for analysis and comparison with Spain. The data was collected between October 2018 and April 2019.
Statistical analysisStatistical analyses were performed with SPSS 25.0 software (SPSS Inc., Chicago, Illinois, USA). The Shapiro Wilk normality test was used to assess whether the study variables were normally distributed. Subsequently, the Kruskal-Wallis and Mann–Whitney U tests were used for data analysis of non-normally distributed variables, whereas one-way analysis of variance and unpaired t-test were used for normally distributed data. To evaluate statistical significance, a threshold of p ≥ 0.05 was used.
ResultsDemographicsResponses were obtained from 1,336 eye care practitioners, of whom 13 were from Africa (not included in the analysis), 202 from Asia, 79 from Australasia, 717 from Europe, 5 from the Middle East (not included in the analysis), 147 from North America, and 173 from South America. Of the 717 questionnaires obtained from European practitioners, 173 provided data from Spain. Seventy-two percentage of all the questionnaires obtained globally were provided by optometrists, 20% by ophthalmologists, and the remaining 8% by other eye health professionals. All questionnaires obtained from Spain were completed by optician-optometrists (referred thereafter as “Spanish optometrists”, “Spanish practitioners” or the like). Most of the professionals who participated in this study overall as well as in Spain work in clinical practice - either in an optometry or refractive surgery setting (92% and 91%, respectively). Worldwide and Spanish practitioners reported being registered to practice for the 11−20 year and 21–30 year categories, respectively.
Concern about the increase in paediatric myopiaThe concern about the increase in paediatric myopia reported by eye care practitioners worldwide was very similar (8.5 ± 2.1) to that reported by Spanish practitioners (8.4 ± 1.9) (p > 0.05). Spanish practitioners were more concerned than Australasian (p = 0.025) and European practitioners (p = 0.007); and similarly concerned to Asian, South American and North American practitioners (p > 0.05). If European countries alone are taken into consideration,5 Spanish practitioners were more concerned than those from Germany (p = 0.000) and The Netherlands (p = 0.007), and similarly concerned than those from Italy, Portugal, Russia and the United Kingdom/EIRE (p > 0.05). In Spain, as in the other regions, no significant differences were found between the years of experience and the level of concern (p > 0.05).
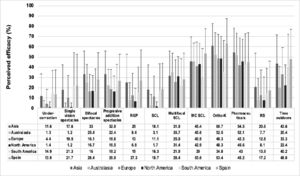
Perceived efficacy of the different methods of myopia controlOverall, eye care practitioners worldwide perceived orthokeratology as the most effective method of myopia control (51.3% [Confidence intervals {CI}: 49.7–52.8]), followed by pharmaceutical approaches (46.5% [CI: 45.0–48.1]) and approved myopia control soft contact lenses (42.7% [CI: 41.2–44.2]). In Spain, orthokeratology (63.5% [CI: 59.6–67.4]), followed by approved myopia control soft contact lenses (54.4% [CI: 50.2–58.4]) and time outdoors (48.5% [CI: 43.6–53.4]) were perceived as the most effective myopia control methods. This difference in perceived efficacy between the world's average and Spain was significant (p < 0.001) (Fig. 1). Significant differences were found between Spain and some of the other regions assessed in the efficacy of single-vision under-correction spectacles, single-vision (full correction) spectacles, bifocal spectacles, rigid gas-permeable contact lenses, single-vision soft contact lenses, specific myopia control soft contact lenses, orthokeratology, progressive addition spectacles and increased time spent outdoors (Table 1). However, no significant differences were found between Spain and the other regions assessed in the efficacy of standard multifocal soft contact lenses, pharmaceuticals and refractive surgery (p < 0.05). In Spain, practitioners reported higher levels of efficacy for orthokeratology, approved myopia control soft contact lenses and time spent outdoors the fewer the years of experience (p < 0.05). In contrast, in North America, the more years of practitioner experience the greater the perceived efficacy of orthokeratology (p < 0.05). If results from optometrists surveyed globally are considered alone (since Spanish optometrists cannot prescribe drugs like atropine), it was found that Asian optometrists (54.4 ± 23.6) reported a higher perceived efficacy of pharmaceutical approaches than Spanish optometrists (45.2 ± 28.5) (p < 0.05), but no significant differences were found between Spanish optometrists and optometrists from the other regions of the world (p < 0.05).
Mann–Whitney U test results (p-values) of the differences between Spain and the rest of the regions assessed in the perceived efficacy of myopia control methods.
RGP, rigid gas-permeable contact lenses; SCL, soft contact lenses; MC SCL, soft contact lens approved for myopia control; Ortho-K, overnight orthokeratology; =, Similar levels of efficacy reported by Spanish practitioners; >, Spanish practitioners reported significantly higher levels of efficacy; <, Spanish practitioners reported significantly lower levels of efficacy.
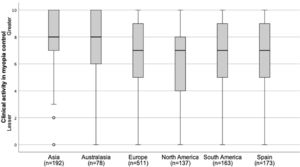
Perceived clinical activity in the field of myopia controlSpanish practitioners reported a similar level of perceived clinical activity in the field of myopia control (6.9 ± 2.6) in comparison with practitioners worldwide (7.0 ± 3.6) (p < 0.05) (Fig. 2). In Spain, as in North America and the rest of European countries, significant differences were found between the different age ranges of professional experience in the perceived level of clinical activity in the field of myopia control (p < 0.05), with increasing years of professional qualification typically showing an increase in the perceived level of clinical activity in the field of myopia control.
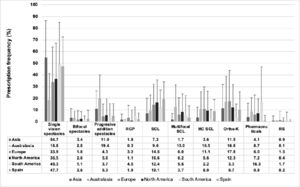
Frequency of prescribing different myopia correction options for progressing/young myopesSingle-vision (full correction) spectacles were, by far, the most widely prescribed option to progressing/young myopes, representing 31.2% (CI: 26.4–36.0) and 47.7% (CI: 43.7–51.6%) of all prescriptions reported overall in the world and in Spain, respectively (Fig. 3). In contrast, orthokeratology were prescribed to 13.2% (CI: 12.0–14.5) and 9.5% (CI: 7.2–12.4) of progressing/young myopes by practitioners worldwide and Spanish practitioners, respectively. Significant differences were found between Spain and the other regions assessed in the prescription frequency of single--vision spectacles, singlevision soft contact lenses, approved myopia control soft contact lenses and pharmaceuticals. However, no significant differences were found between Spain and the other regions in the prescription frequency of bifocal spectacles, progressive addition spectacles, rigid gas-permeable contact lenses, standard multifocal soft contact lenses, orthokeratology and refractive surgery (p < 0.005). Significant differences between the different age ranges of professional qualification were found in the prescription frequency of approved soft contact lenses for myopia control (p = 0.036), with increasing years of professional qualification typically showing a lower prescription frequency of such lenses. No significant differences were found between Spanish practitioners’ years of experience and the prescription frequency for the remaining myopia control strategies (p < 0.005).
Prescribing frequency of different myopia correction options to progressing/young myopes in a typical month. RGP, rigid gas-permeable contact lenses; SCL, soft contact lenses; MC SCL, soft contact lens approved for myopia control; Ortho-K, overnight orthokeratology; RS, refractive surgery. Error bars represent one standard deviation.
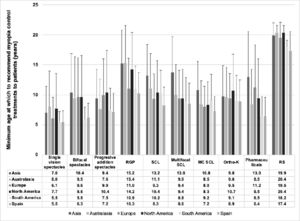
Significant differences between regions were found in the minimum age at which a myopia control method would be prescribed (p < 0.001) (Fig. 4). Overall, eye care practitioners from all regions recommend prescribing a myopia control treatment at an older age (10.1 ± 5.8 years [CI:10.0–10.2]) than Spanish practitioners (7.8 ± 3.5 years [CI: 7.6–8.0]) (p < 0.001). Spanish practitioners recommend the prescription of single-vision spectacles, rigid gas-permeable contact lenses and pharmaceutical agents at a younger age in comparison with the other regions assessed (p < 0.001). No significant differences were found between regions in the age at which a patient would be prescribed any of the other myopia control options assessed (p < 0.05). Of interest is that Spanish practitioners recommend the prescription of approved myopia control soft contact lenses at a younger age than soft contact lenses (p < 0.001). No significant differences between the different age ranges of professional experience were found in the mean minimum age at which a patient would be prescribed a myopia control method for any of the regions assessed (all p > 0.05).
Minimum age (years) at which practitioners from the different regions would recommend myopia control treatments to patients. RGP, rigid gas-permeable contact lenses; SCL, soft contact lenses; MC SCL, soft contact lens approved for myopia control; Ortho-K, overnight orthokeratology; RS, refractive surgery. Error bars represent one standard deviation.
Spanish eye care practitioners recommend prescribing a myopia control method to patients with a slightly higher level of myopia (-1.6 ± 1.4D [CI: -1.7 to -1.5]) than that of the average of all the other regions (-1.5 ± 1.3D [CI: -1.6 to -1.5]) (p = 0.03). Significant differences between regions were found in the minimum degree at which the different myopia control methods would be prescribed (p < 0.001) (Table 2-). Spanish practitioners, as it was typically the case for practitioners from the other regions as well, reported prescribing single-vision spectacles and single-vision soft contact lenses for lower levels of myopia (mean -1.2 ± 0.4D and -1.40±0.8D, respectively), whereas rigid gas-permeable contact lenses and refractive surgery would be prescribed for higher levels of myopia (mean -2.7 ± 2.0D and -3.8 ± 2.1D, respectively). No significant differences between the different age ranges of professional experience were found in the minimum degree of myopia at which a myopia control method would be prescribed for any of the regions assessed (all p > 0.05).
Mann–Whitney U test results (p-values) of the differences between Spain and the rest of the regions in the minimum degree of myopia at which a myopia control method would be prescribed.
SCL, soft contact lenses; RGP, rigid gas-permeable contact lenses; MC SCL, soft contact lens approved for myopia control; Ortho-K, overnight orthokeratology; RS, refractive surgery; =, Similar rates; >, Spanish practitioners reported significantly higher degree of myopia to consider myopia control options; <, Spanish practitioners reported significantly lower degree of myopia to consider myopia control options.
Minimum annual amount of patient myopia progression that would prompt a practitioner to specifically adopt a myopia control approachSpanish as well as Australasian and European practitioners would recommend a myopia control intervention to patients with a lower annual myopia progression (0.50–0.75D/year) than those from the other regions (p < 0.001) (Table 3). If European countries alone are taken into consideration, practitioners in Spain recommend a myopia control intervention for patients with a higher annual progression of myopia than those from Germany, Ireland, Italy, Norway, Portugal, Switzerland and the United Kingdom (p < 0.001); and for patients with a lower annual progression of myopia than those from Austria, France and The Netherlands (p < 0.001). No significant differences were found overall for all regions in the minimum range of annual myopia progression to offer a myopia control option based on the number of years of professional experience (p > 0.05).
Use of single-vision distance under-correction as a method to slow myopia progressionGlobally, 78.2% of all eye care practitioners that participated in this survey did not consider distance, single-vision under-correction to be an effective strategy for slowing myopia; 17.4% practitioners reported prescribing it sometimes; and 4.1% reported always recommending this strategy (Table 4). These figures were slightly different in Spain (p < 0.001), where single-vision under-correction was never, sometimes or always recommended by 69.4%, 30.2% and 0.6% of practitioners, respectively. Spain and South America are the regions where practitioners most commonly prescribe single-vision under-correction as a method for slowing myopia progression (p < 0.05), whereas Australasian practitioners the least (p < 0.001). No significant differences between the different age ranges of professional qualification were found in the prescription of single-vision under-correction neither for Spanish practitioners (p > 0.05) nor overall for practitioners globally (p > 0.05) .
Reasons why myopia control methods are not prescribedSignificant differences were found between Spain and the rest of the world's average in factors preventing the prescription of a myopia control approach (p < 0.05). Worldwide, as well as in Spain, the main reasons why myopia control methods are not prescribed are their high cost followed by inadequate information (p < 0.05). Additionally, in Spain, South America and Asia, unpredictable results and lack of efficacy are also important factors preventing practitioners the prescription of myopia control approaches (p < 0.05). Other reasons commented in the free text section preventing Spanish practitioners the prescription of myopia control approaches included the need for dissemination of better scientific information on these methods to improve practitioner training. In contrast, practitioners globally identified other factors preventing the prescription of myopia control approaches, which included lack of availability of treatments and instruments required to prescribe them, as well as the need for informative material and consistent regulation for the approval and prescription of these methods.
DiscussionThis study evaluated trends in myopia management in clinical practice in Spain and compared these trends with those from other regions of the world. Of interest is that worldwide and Spanish practitioners reported being registered to practice for the 11−20 year and 21–30-year categories, respectively; the latter might explain some of the differences found in the variables assessed in this study between Spain and the other regions of the world.
That Spain is one of the regions of the world where there is a greater concern about the increase of myopia in children is consistent with the rise in the prevalence of paediatric myopia reported over the last couple of decades.2,3 The perceived level of clinical activity in the field of myopia control was reported relatively high overall by practitioners worldwide as well as by Spanish practitioners, which might be also related to increasing prevalence rates of myopia and available treatment options and guidelines to best use them in clinical practice.7,8 Although there are differences in the prevalence of myopia between regions around the world, the prevalence of myopia has been found to increase in all regions around the world over the last few decades, and it has been forecasted to experience significant increases over the next three decades.1 The latter might explain why practitioners from different regions all share similar levels of concern about the increasing prevalence of myopia.
Orthokeratology is considered the most effective method for slowing myopia progression both in Spain and in the other regions, which is attributed to the numerous studies demonstrating the efficacy of this myopia control method.9–12 Furthermore, unlike other myopia control interventions, orthokeratology appears to be effective in reducing the progression of myopia in children for long periods of time ranging from 5 to 10 years.13–17 Pharmaceutical agents are also among the treatment options perceived as most effective. However, of interest is that 0.01% atropine has not demonstrated to be efficacious in slowing the axial elongation of the eye,18 despite widespread use in ophthalmology at this concentration.19 Despite no contact lenses were specifically approved for myopia control neither in Spain nor in most parts of the world at the time when this study was conducted (October 2018 and April 2019), the perceived efficacy of soft contact lenses specially approved for myopia control by practitioners worldwide has increased by 20% compared to our previous report4 and this might be attributed to efforts from industry to obtain regulatory approval of contact lenses specifically approved for this particular intended use in different parts of the world as well as by practitioners recognition that regulatory approval grants increased safety and efficacy for contact lenses approved for myopia control in comparison to off-label prescribing.20 Furthermore, of interest is that a survey found that Spain is the country in the world reporting the highest proportion of myopia control fits to minors – close to 35% of all contact lenses fitted to patients aged 6 to 17 years from 2018 to 2020 were classified as “myopia control”21 - which, again, might be attributed to increasing numbers of both soft and orthokeratology specifically approved for myopia control becoming available to Spanish practitioners. In 2021, Spain has been found again as the market with the highest rate of soft contact lens prescribing for myopia control.22
Although outdoor activity was also perceived as an effective strategy for slowing myopia progression, its efficacy in slowing myopia onset, and possibly as a result lower end-point myopia, is well established, but its effect on reducing myopia progression in pre-existing myopes remains controversial.8,23–25 Differences in the perceived myopia control efficacy of outdoor activities between regions might be attributed to differences in lifestyle and population density. Despite studies published about two decades ago26,27 and recent clinical guidelines7,8 reporting that spectacle distance, single-vision, under-correction could increase rather than decrease the rate of myopia progression in comparison to full single-vision spectacle correction in children, it is surprising that some practitioners still perceive this as an effective myopia control approach, with over 30% and 20% of practitioners recommending this approach “sometimes” in Spain and overall worldwide, respectively. It is also surprising that despite Spanish practitioners, as well as those from the other regions, perceived certain myopia control options efficacious (Fig. 1), such myopia control options were not frequently prescribed in clinical practice (Fig. 3). Furthermore, although single-vision distance spectacles were perceived as an ineffective myopia control approach, it was the most widely prescribed correction for young/progressive myopes, accounting for approximately 50% of all myopia control options being prescribed (Fig. 3). It should also be noted that at the time when this survey was conducted (October 2018 and April 2019) no such spectacle lens designs approved for myopia control were available neither in Spain nor in other parts of the world.
The fact that practitioners from different regions considered a relatively higher patient age to recommend a myopia control approach in comparison to Spanish practitioners might be related to perceptions associated with decreased capacity for younger children to care for contact lenses, more fitting and training time required, and inferior risk-to-benefit ratio compared to older children.28 Similarly, differences between regions were also found in the minimum annual amount of patient myopia progression that would prompt practitioners to specifically adopt a myopia control approach, with Spain, Europe and Australasia reporting the same range of annual myopia progression (i.e., 0.50 to 0.75 D); Asian and North American practitioners a higher range (0.75 to 1.00 D); and South American practitioners reporting the highest amount of myopia progression (>1.00 D). Although there are no clear guidelines as to when to start prescribing myopia control methods based on progression rate,7 a global survey undertaken by paediatric ophthalmologists found that the most common indication for myopia control treatment was the rate of myopia progression, with a progression rate of 1.1 ± 0.6 D/year chosen overall as the cut-off for initiation of treatment with minor deviations across world regions (range 0.90–1.25D).19 Differences between regions in the patient's age and myopia progression rate at which to recommend a myopia control option might be also influenced by the region's predominant ethnicity, with higher rates of myopia progression typically found in Asian compared to European children,29 practitioners scope of practice as well as cultural and regional preferences. Nevertheless, there appears to be insufficient evidence to suggest that faster progressors, or younger myopes, derive greater benefit from treatment; however, the decreased risk of complications later in life provided by even modest reductions in progression suggest treatment is advised for all young myopes.16
The main reason reported as to why myopia control methods were not prescribed by practitioners is high economic cost. However, uncorrected myopia has been reported to produce an overall loss of productivity of over 202 billion dollars annually worldwide.26 Furthermore, myopia incurs substantial expenditure such that in the USA alone, the annual cost for eye examinations and corrections by spectacles and contact lenses has been estimated to be between $2 and $5 billion.27 It is well established that the higher the myopia and the longer axial length becomes, the higher the lifetime risk of developing ocular complications, such as myopic macular degeneration, retinal detachment, posterior subcapsular cataract, nuclear cataract, open angle glaucoma, and blindness.30 Although high myopia carries the highest risk of complications and visual impairment, low and moderate myopia also have considerable risks. Without wide adoption of myopia control methods, the burden of illness of myopia will increase substantially with the projected increase in the prevalence of myopia worldwide.31 Thus, in the long term, prescribing myopia control methods to reduce myopia progression are expected to reduce the rate of ocular pathologies associated with myopia and consequently the costs of treating myopia-related complications. Future studies are needed, however, to generate more homogeneous cost data and provide a complete picture of the global economic cost of myopia.32 Inadequate information, unpredictable results and current myopia control methods being ineffective were also common reasons preventing practitioners the prescription of a myopia control approach. However, since this survey was conducted abundant information regarding myopia control has become available, including guidelines summarizing current knowledge in the field that should help in promoting best clinical practice.8,33
In conclusion, this questionnaire on attitudes and strategies for the management of myopia in clinical practice has found that the uptake of myopia control methods by Spanish practitioners, as well as practitioners from other parts of the world, is relatively low, despite the increase in the prevalence of paediatric myopia, as well as increased concern and perceived clinical activity in the area. Spanish practitioners, like those from other regions, considered orthokeratology to be the most effective treatment for myopia control. However, in Spain together with Asia and South America, the prescription of single-vision spectacles and single-vision contact lenses continues to be the main methods of visual correction prescribed to myopic children. The major reasons why Spanish practitioners were not prescribing myopia control strategies, as in the rest of the regions, were increased cost, inadequate information and unpredictable outcomes. Further actions are needed to increase public and professional awareness and to educate and train eye care practitioners about myopia control interventions.
This project was supported by many eye care organisations across the globe. Special thanks are given to the Spanish General Council of Spanish Optician-Optometrists for dissemination of the survey to all registered Optician-Optometrists in Spain.