The presence of cataract causes reduction in visual acuity (VA) and contrast sensitivity (CS) and thus can affect individual's daily activities. The aim of this study was to investigate self-reported driving difficulty in patients with bilateral cataract.
MethodsA total of 99 participants aged 50 and above, with bilateral cataract, who possessed a valid driving license and drove regularly were chosen for this cross-sectional study that looked into their visual functions (VA and CS) and driving difficulty using the self-reported Driving Difficulty Questionnaire.
ResultsThe mean age of the participants was 65.04±7.22 years old. Results showed that the mean composite driving difficulty score was 83.18±11.74 and most of the participants were having difficulty for driving in the rain (73.7%) and at night (85.9%). Furthermore, the study found that there was a significant correlation between driving difficulty score and CS (rs = 0.40, p = 0.03). However, there was no significant correlation between driving difficulty score and VA (rs = -0.14, p = 0.17). A linear regression was calculated to predict driving difficulty score based on binocular CS and a significant regression equation was found (F (1,28) = 8.115, p = 0.008) with R² of 0.225. Drivers with bilateral cataract will most likely experience some forms of difficulty, especially when driving under low contrast conditions.
ConclusionThe findings of this study demand that a comprehensive eye examination should be made compulsory for older adult drivers when issuing or renewing their driving license for the safety of all road users.
Cataract is one of the leading cause of visual impairment globally.1,2 In Malaysia, latest reports also showed that cataract is the major cause of visual impairment among population above 50 years old.3,4 People with cataract experienced blurring of vision, reduced contrast sensitivity and excessive glare.5,6 Mehmet and Abuzer6 found that older adults with cataract rated their difficulty level in performing daily activities as poor to moderate. It is also reported that reduced visual functions due to the presence of cataract also affect driving skills and performance.7
Nischler et al.9 found a significant association between cataract severity and driving performance, as the more severe the cataract the worst the driving performance. Mantyjarvi and Tuppurainen10 added that older drivers with cataract had low contrast sensitivity and glare disability, as they needed extra illumination and took a longer time to adapt to a change in illumination. It could be difficult for them to see clearly, especially at dawn, dusk, and night. They were more sensitive to glare from headlights, streetlights, or the sun, causing them to have difficulty in seeing signages and other vehicles. This was supported by Owsley et al. ,11 who found that older drivers with cataract had significant driving difficulty during rain, rush hours, heavy traffic and night time. It was also reported that older adults with cataract had two times the risk of crashing compared to the older adults without cataract.11
Driving is a challenging task that requires good vision, psychomotor, and cognitive abilities.8 Previous study showed that good visual attention and motor function were the two crucial components in driving safety24 and driving performance.25 Studies showed that 50% of the older drivers react slower to dangerous driving situations than they used to (Yeoh, Benjamin and Sharifah Norazizan 2011). Good visual attention and fast reaction are crucial for being a safe driver (Yeoh, Benjamin & Sharifah Norazizan 2011). A simple test such as the Adult Developmental Eye Movement Test (ADEM) can be used to measure cognitive and visual attention parameters, which are important components in driving performance.25 This test may also help in the detection of impairments in the saccadic efficiency that could have a detrimental effect on the driving performance. According to Gené-Sampedro et al. ,25 difficulty in driving at night was found to be a potential predictor of driving performance. Therefore, scotopic vision assessment should be considered, not only photopic vision (Lijarcio et al. 2020). Lijarcio et al. in 2020 also suggested that the visual field should be considered as one of the assessments in issuing or renewing the driving licence.
It should be noted that most of the previous studies were conducted in Western countries with different weather and traffic conditions compared to Malaysia. To address the gap, this study aimed to determine the driving difficulty among drivers with bilateral cataract in specific driving situations using the Driving Difficulty Questionnaire, as no similar study was conducted in Malaysia to this date.
Materials and methodsThis cross-sectional study was conducted at a tertiary government hospital (Hospital Malacca). Convenience sampling method was chosen because of strict inclusion criterion among low prevalence of bilateral cataract (0.5%) in the southern region of Malaysia.3 This study protocol has been approved by Universiti Kebangsaan Malaysia Ethics Committee (UKM PPI/111/18/JEP-2017–684) and by the Ministry of Health Malaysia's Medical Research & Ethics Committee (KKM/NIHSEC/P17–1583(5)).
ParticipantsRecruited participants included those above 50 years old, diagnosed with bilateral cataract, that were legally licensed to drive and were actively driving (at least once a week). A sample size of 30 was calculated based on the formula by Cochran (1963), considering α = 0.05, delta = 0.10 and a proportion of 0.0459.12 The proportion was based on the prevalence of cataract among the 50 years old and above in Southern Malaysia, which is 4.59%.3 Other inclusion criteria were: (i) physically fit based on the Medical Examination Standards for Vocational Driver's Licensing guideline13; (ii) cognitive score of >17 as measures by Mini-Mental State Examination (MMSE)15 ; (iii) habitual bilateral VA of 0.3 to 1.0 logMAR as the minimum required standard when driving in Malaysia is 0.3 logMAR.13 The exclusion criteria were (i) other ocular diseases such as ARMD or diabetic retinopathy; (ii) failed MMSE and (iii) no longer driving.
MaterialsThe logarithm of the minimum angle resolution (LogMAR) ETDRS chart was used to measure visual acuity (VA), and the Pelli Robson chart was used to measure contrast sensitivity (CS).14 The Mini-Mental State Examination (MMSE) was used in this study to determine the status of cognitive function. Only participants who scored 17 and above were eligible as subjects.15
Driving difficulty status was identified using the Driving Difficulty Questionnaire which is a subset of Driving Habits Questionnaire.11 Participants were asked to rate the degree of visual difficulty that they experienced from 0 to 5-point scale. A composite score of driving difficulty was computed based on the responses to all 8 items and scaled on a 100-point scale.
ProcedureA written consent was obtained from all participants prior to the enrolment. Demographic data on gender, age, working status, driving characteristics (duration and frequency) and type of vehicle transmission were identified from the interviews. All participants were then screened for cognitive function using the MMSE.
Habitual monocular and binocular VAs of all participants were determined using LogMAR chart at 4 m and recorded in logMAR units. Only those with a VA of 0.3 logMAR or worse were accepted in this study. The Pelli Robson contrast sensitivity chart was used to measure habitual monocular and binocular CS at 1 m and recorded in Log Contrast Sensitivity units.
The driving difficulty status of all participants was then identified using the Driving Difficulty Questionnaire. Participants were required to answer all the questions on their own. If the participants could not read due to vision problems, the examiner read out the questions to them. Participants were asked to rate the degree of visual difficulty experienced in specific driving situations. Ratings were made on a 5-point scale (5 = no difficulty, 4 = a little difficulty, 3 = moderate difficulty, 2 = extreme difficulty, 1 = no longer drive in that situation due to visual problems). A composite score of driving difficulty was computed based on a 100-point scale [(mean score - 1) X 25]. Participants with a score of less than 90 were identified as having a driving difficulty.11
Data analysisData were analysed using IBM SPSS Statistics for Windows, Version 20.0. Armonk, NY: IBM Corp. Frequencies, mean, standard deviation (SD), and percentages were used for descriptive statistics. The driving difficulty score was correlated to bilateral VA and CS using Spearman's Rho. Simple linear regression was calculated to predict driving difficulty score based on binocular contrast sensitivity.
ResultsDemographic dataDetails on the demographic, VA, CS and driving characteristics of the participants are displayed in Table 1. The mean age of the participants was 65.04±7.22. Majority of the participants were males, Malay and not working. Driving characteristics revealed that 84.9% of the participants had driving experience of more than 30 years, actively driving and most of them were driving with an automatic transmission.
Demographic and driving characteristic of the participants.
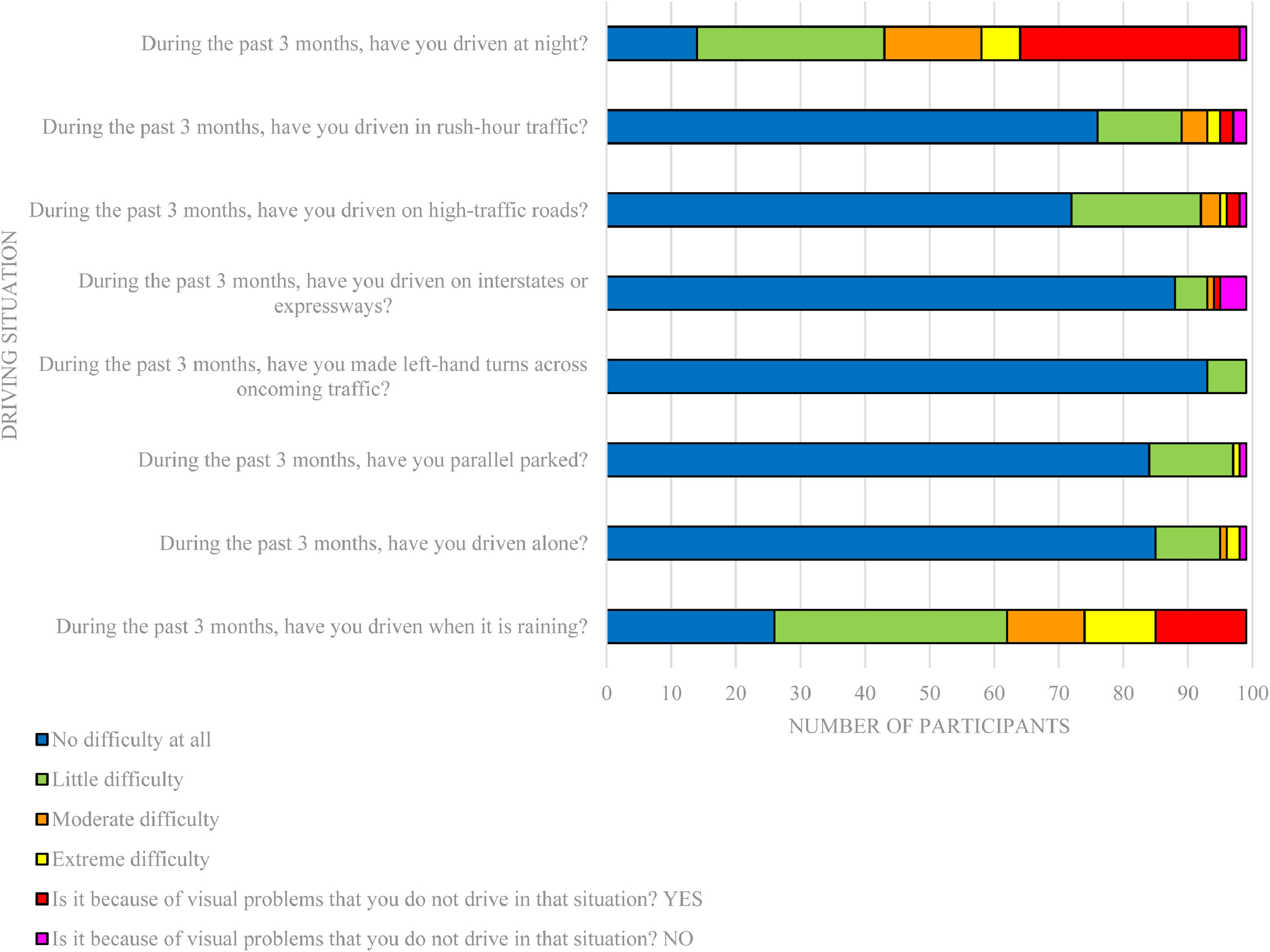
The mean composite driving difficulty score for all participants was 83.18±11.74. Fig. 1 shows the distribution of the answers to each item in the Driving Difficulty Questionnaire.
The results showed that 63.6% of the participants were having difficulties in driving. Majority of the participants had difficulty for driving in the rain (73.7%) and at night (85.9%). The percentage of driving difficulty in different situations is shown in Table 2. It is interesting to note that some of the participants also decided not to drive under these situations. Most of them did not drive at night (34.3%), in the rain (14.1%), in rush-hour traffic (2.0%), on high-traffic roads (2.0%), and on interstates or expressways (1.0%).
Driving difficulty status for different driving situations among the participants.
The VA was measured on all participants (N = 99), however the CS values were only available for 30 participants. Table 3 shows the mean and median values of VA and CS of the participants. Spearman's Rho indicated that there was a significant positive moderate correlation between driving difficulty and binocular CS (rs = 0.404, p = 0.03). However, there was no correlation between driving difficulty score and binocular VA (rs = −0.140, p = 0.17).
A simple linear regression was calculated to test if binocular contrast sensitivity significantly predicted the driving difficulty score. The results of the regression analysis indicated that the model explained 22.5% of the variance and that the model was significant, F(1,28) = 8.115, p = 0.008. It was found that binocular contrast sensitivity significantly predicted driving difficulty score (β1 = 25.58, p<0.05). The final predictive model was:
Driving difficulty score = 40.11+25.58 (CS), where CS is measured binocularly in Log Contrast Sensitivity units. Participant's driving difficulty score increased by 25.58 for each Log Contrast Sensitivity unit of CS.
DiscussionDemographic data showed that most of the participants were still driving actively (more than 4 times per week), even with reduced VA and CS due to cataract. This group of participants also failed the VA criteria for driving set by the authority. The system of renewing the driving license in Malaysia does not require drivers to undergo general and ocular health assessments, except for the initial Vocational Driving Licence (VDL) or Commercial Driving Licence, and that has enabled the participants to continue driving even with reduced VA and CS.16,17
The driving performance of the participants with bilateral cataract was declined. This is in line with a previous study in Malaysia reporting that almost 50% of the drivers aged between 60 and 74 years old were having difficulty in driving.18 However, the study did not take into account the factor of vision status among the participants in detail, as compared to the current study. Findings from the current study were also in agreement with those from Owsley et al.11 and Abd Rahman et al.19 in which cataract was found to be significantly related to the driving difficulties and performance. Hence, the poor visibility due to eye problems could be the reason why the older drivers in Malaysia were having difficulties in reading signage, driving at night and in the rain.18
The current study agreed with Nischler et al.9 and Shandiz et al.20 that cataract with VA between 6/12 and 6/60 posed difficulties in driving. CS was another visual function that could be affected by cataract.5,7 Normal CS function for older population (age 50 and above) monocular and binocular was 1.65 log and 1.80 log, respectively.14 Leat et al.21 stated that a CS score of less than 1.50 reflected visual impairment, and they estimated that a score of less than 1.05 would result in disability. The current study showed that the mean binocular contrast sensitivity was 1.25±0.30, which was lower than 1.80 and could be significantly affecting driving performance. Mantyjarvi and Tuppurainen10 supported this finding and mentioned that the loss of contrast sensitivity function as in older drivers with cataract would affect their ability to drive significantly at dawn, dusk and night. Currently, CS is not a criterion in obtaining and renewing the driving licence. Thus, the local authorities should consider to include CS as one of the criteria other than just VA and colour vision for both new and renewal of driving licences application.22 A previous study also found that cataract also affected colour vision due to the yellowing of the crystalline lens, suggesting the need of a thorough assessment of colour vision among older adult drivers with cataract.23
The cataract sufferers in this study were found to have difficulty in driving in all situations (Table 2), and these findings were similar to a study conducted by Owsley et al. .11 However, the cataract sufferers in this study reported a higher percentage of difficulty driving in the rain and at night as compared to other situations which we looked into. Owsley et al.11 found that 67% of older drivers with cataract had difficulties for driving in the rain and 77% had difficulties in driving at night. The percentage was slightly lower than the current study due to the different levels of VA and CS in the previous study, which were better compared to the current study. It is worth to note that the different percentage could be attributed to the difference in traffic conditions or driving behaviour in Malaysia. The most prominent one is the left- or right-hand side driving in both countries in which these researches were carried out. This finding was supported by Nischler et al.9 who found that driving during bad weather or at night caused difficulties among drivers with cataract at all levels of severity of visual impairment. Previous studies also mentioned that cataract causes reduction in VA and CS.5,7 This problem could affect driving-related tasks, such as reading signage, seeing objects under low contrast condition, and seeing vehicles in adjacent lanes.7 Indirectly, these problems would affect the driving performance among cataract drivers.9,11
To the best our knowledge, there was no prior study that looked into the relationship between driving difficulties and VA and CS, specifically in cataract patients. The current study found that there was no correlation between driving difficulty and VA. The correlation of the driving difficulty and VA could not be seen among cataract patients in this study might be due to the fact that the current study was focused on moderate visual impairment only, instead of severe visual impairment. The current study used levels of VA to classify the severity of cataract whereas the previous one by Nischler et al.9 classified the severity of cataract based on a morphological criterion (intensity of opacification) and noted a significant association between cataract severity and the driving performance. Increase in cataract intensity resulted in significantly reduced driving performance.9 In contrast to VA, the CS analysis showed a significant moderate positive correlation with driving difficulty. This objective finding reflected current subjective finding (self-reported driving difficulty) that our respondents with bilateral cataract have difficulties driving under low contrast situations (Table 2). In additional, the current study showed that the driving difficulty score among bilateral cataract patients can be predicted based on value of binocular CS.
The results of this study provided important information on the driving difficulty status among drivers with bilateral cataract in Malaysia. It showed that drivers with cataract regardless of VA level, would have difficulties in driving due to the reduction in CS. Since cataract is a reversible visual impairment, it is interesting to find out if there is an improvement in the driving difficulty level among people with post-cataract operation compared to pre-cataract operation. Future study was suggested to include other ocular diseases such as glaucoma and diabetic retinopathy, which are irreversible visual impairments, as they might pose different situations of driving difficulties.
Cataract can reduce VA until do not meet the standard of visual requirement to drive. Furthermore, CS also can be affected for individuals with cataract. The older drivers with bilateral cataract would experience driving difficulties, especiallyunder low contrast situations. Currently, only distance VA and colour vision are considered when issuing a driving license. It is suggested that CS should be considered by the authority as one of the criteria when issuing or renewing a driving license. It is also suggested that the older adult drivers undergo regular and comprehensive eye examinations before renewing their driving licenses.
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.