In vivo study of retinal straylight in a patient before and after penetrating keratoplasty (PKP).
MethodsRetinal straylight was measured in a 65-year-old man suffering from a post-herpetic corneal scar, both before and after PKP using the compensation comparison method (C-Quant straylight meter, Oculus GmbH, Germany).
ResultsRetinal straylight values before surgery were high compared to those obtained for age-matched normals in previous studies, due to light scattering induced by the corneal scar. Mean and standard deviation straylight values before and 9 months after PKP were log(s)=1.71±0.09 and 1.05±0.08, respectively. Decrease in retinal straylight could be explained by an improved corneal transparency, resulting in a significant improvement in visual acuity.
ConclusionsRetinal straylight measurement provides objective and clinically valuable information about forward light scattering as the cause of visual disability. Improvement of the visual function after surgery is underestimated by visual acuity measures.
Estudio in vivo de la luz dispersa que alcanza la retina en un paciente antes y después de someterse a una queratoplastia penetrante (o sus siglas en inglés, PKP).
MétodosEn un paciente varón de 65 años con una úlcera corneal herpética se midió la proporción de luz dispersa que alcanza la retina tanto antes como después de una PKP, utilizando para ello un método psicométrico denominado “de comparación por compensación” («Compensation comparison method», C-Quant straylightmeter, Oculus GmbH, Alemania).
ResultadosLa cantidad de luz dispersa que alcanza la retina medida antes de la cirugía fue elevada en comparación con los valores obtenidos en estudios previos en sujetos normales de la misma edad, debido principalmente a la dispersión provocada por la úlcera corneal. La cantidad de luz dispersa que llega a la retina (media ± desviación típica), en las medidas preoperativas y en las realizadas 9 meses después de la intervención de PKP, fue igual a log(s)=1,71±0,09 y 1,05±0,08 respectivamente. La disminución de la cantidad de luz dispersa podría deberse a un aumento de la transparencia corneal, lo que también ocasionaría una mejora significativa de la agudeza visual.
ConclusionesLa medida de la luz dispersa que llega a la retina proporciona información clínicamente relevante sobre la dispersión de la luz hacia delante como causa de discapacidad visual. Las medidas de agudeza visual subestiman la mejora de la función visual obtenida tras la cirugía.
Retinal straylight measurement provides information about forward light scattering as well as direct information about optical imperfections related to disability glare.1 Disability glare, a factor in quality of vision, refers to a reduction in visual performance caused by a glare source, resulting in retinal contrast loss, secondary to intraocular straylight. It has been found that important causes of increased straylight are cataracts2,3 and refractive surgery.4-6 In addition, other corneal conditions such as corneal dystrophies or an infectious disease may also cause strong increase in straylight. We report a case of an eye with a post-herpetic corneal scar for which straylight was measured both before and after penetrating keratoplasty (PKP).
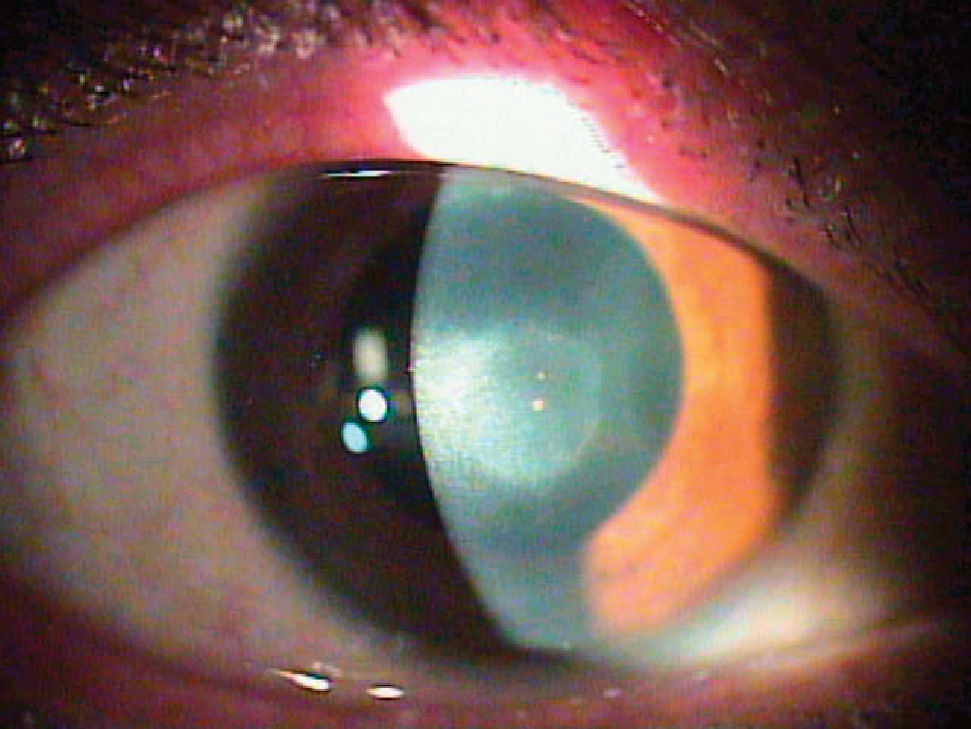
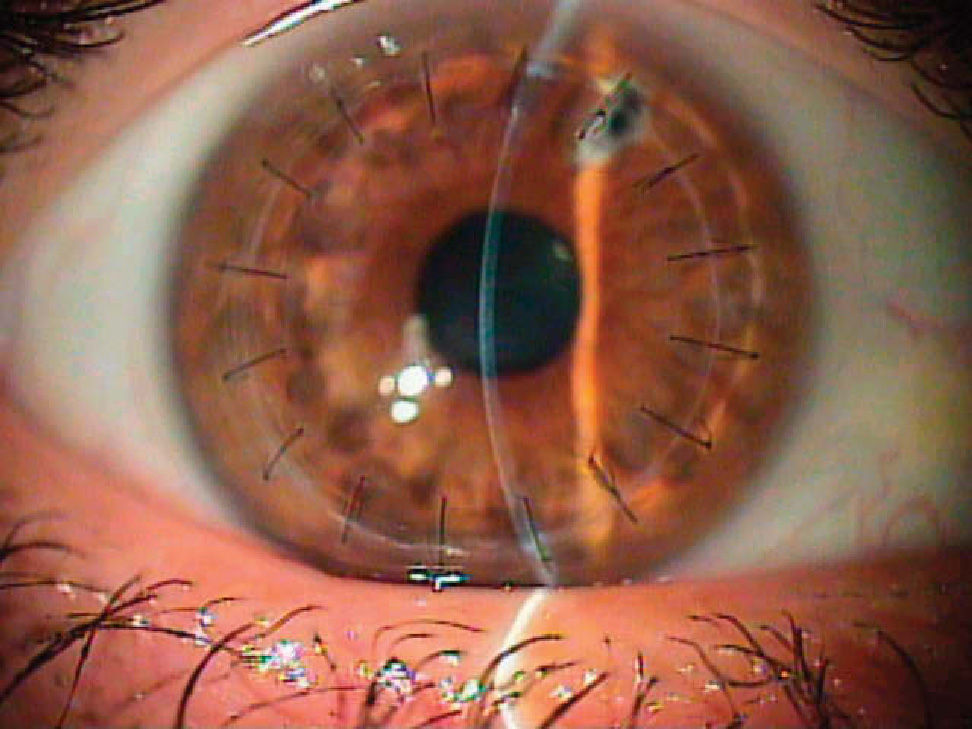
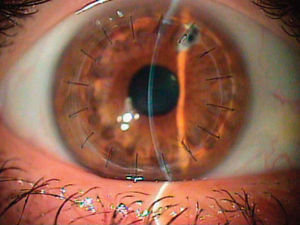
Case ReportA 65-year-old white man showed a preoperative postherpetic corneal scar on his left eye (Figure 1). The best spectacle-corrected visual acuity (BCVA) was 20/80 and the manifest refraction was -2.50 -1.50 × 120°. No other ocular abnormality was found (e.g., cataract). This eye underwent PKP to improve corneal transparency and visual acuity. A 0.25-0.50mm oversized donor cornea was punched out using the Barron donor punch (Katena Products, USA) and it was secured to the recipient's eye following excision of the cornea using the Hessbarg-Barron trephine (Katena Products Inc, Denville, NJ, USA). Figure 2 shows the postoperative picture of this eye, 9 months after PKP. Retinal straylight was measured using the commercially available clinical version of the compensation comparison method, the C-Quant straylight meter (Oculus GmbH, Germany), both before and 9 months after PKP (5 measurements each time). The system uses the abovementioned “compensation comparison” method, which is a modification of the original “direct comparison” method in order to make it more suitable for clinical use on a large scale. It consists of a series of concentric rings, the smallest of which is divided into two halves. The patient is asked to look at this central ring while a concentric one flickers with varying intensity and frequency. The patient is asked to compare both halves of the test field, one of which has some counter-phase flickering added, and to indicate which side flickers stronger by pressing a button. The pattern of right and wrong answers will define a psychometric function from which the straylight value is obtained.
The reliability of this instrument to estimate ocular straylight has been previously reported.7,8,9 Mean and standard deviation of the logarithmic straylight values before and 9 months after PKP were 1.71±0.09 and 1.05±0.08, respectively, which is in good agreement with previous reports of intrasession variance of 0.07 - 0.1.7,9 A significant reduction of straylight of more than 0.60 log units could be observed, which represents an improvement factor of 4.6. BCVA 9 months post-PKP was 20/30, with a manifest refraction of −1.50 −2.25×60°.
DiscussionPKP for corneal disease has a long history, and has proven a high success rate.10,11 In the present case, BCVA after surgery is good and comparable with that found in previous studies.11 Focusing on straylight results, which are the main purpose of this report, high values were found prior to surgery, compared to those obtained in previous studies for age-matched normals without any ocular abnormality (around 1.20±0.20 log(s) units).6 On average, retinal straylight remains relatively unchanged up to 40 years of age, but then it doubles by the age of 65 and triples by the age of 77,12 primarily because of cataract. It should be born in mind that any pathological condition affecting hydration and/or transparency of the cornea may induce increased light scatter depending on the type of disease.13 Thus, the increase of retinal straylight is correlated with the reduction of corneal transparency caused by corneal scars (Figure 1). It is important to note that, due to the logarithmic nature of the straylight metrics used, an increase of 0.3 log units implies a doubling of the amount of straylight. Nine months after PKP a significant reduction of retinal straylight—by a factor of 4.6— was obtained, indicating how the donor cornea has improved corneal transparency (Figure 2). This fact also resulted in a better BCVA but, interestingly, only by a factor of 2.7, which is equivalent to 4 lines. Straylight values obtained after the surgery were similar to those found in age-matched normal subjects.6 Direct slit-lamp examination provides information regarding the success of the surgery in terms of corneal transparency. However, slit-lamp examination alone is not a good predictor of intraocular straylight changes and the presence of disability glare.5 Visual acuity has been recently shown to vary rather independently from retinal straylight.6 Equally, contrast sensitivity in post-surgical patients may be different between subjects showing similar straylight values.14 In this sense, retinal straylight measurement provides valuable additional information regarding visual performance, complementary to slit lamp examination and visual acuity measurements.
This report describes how retinal straylight values provide objective information about the reduction in internal straylight after PKP in an eye with a post-herpetic corneal scar and shows how the visual function is underestimated by visual acuity measures compared to retinal straylight values. Straylight measurement at different times post-surgery would give valuable information about the changes occurring at different treatment stages or during the healing process, better than visual acuity measures.