To determine the effect of residual stereopsis on vision-related abilities of low vision (LV) patients with age-related macular degeneration (AMD).
MethodsProspective non-randomized observational case series. Inclusion criteria included documented AMD, LV with best corrected visual acuity (BCVA) of 20/50–20/400 in the better eye, and ages between 50 and 90 years. Stereoacuity was measured using the near Frisby Stereotest. Vision related abilities were documented with the VA LV VFQ-48 questionnaire.
ResultsTwenty-seven subjects with mean age of 84±6 years old were recruited, of which 59.3% (16/27) were female. 59.3% (16/27) of the subjects were not able to see any stereoacuity plate, 25.9% (7/27) had stereoacuity of 340s of arc (SOA), 11.1% (3/27) had stereoacuity of 170 SOA and 3.7% (1/27) had stereoacuity of 85 SOA. The mean Overall Functional Visual Abilities (OFVA) score was significantly higher in those with stereopsis (2.25±0.99) than those without stereopsis (1.50±0.92) (P=0.028).
ConclusionsLV patients with stereopsis have better OFVA than those without. Stereopsis should be considered as a component of LV rehabilitation and considered as an outcome measure in research and clinical practice.
Determinar el efecto de la estereopsis residual sobre capacidades relacionadas con la visión de los pacientes con baja visión (BV) y degeneración macular asociada a la edad (DMAE).
MétodosEstudio observacional de serie de casos prospectivo y no aleatorizado. Los criterios de inclusión incluyeron DMAE documentada, BV con mejor agudeza visual corregida (MAVC) de 20/50 a 20/400 en el mejor ojo, y edades comprendidas entre 50 y 90 años. La estereoagudeza se midió utilizando el Frisby Stereotest de cerca. Las capacidades relacionadas con la visión se documentaron utilizando el cuestionario VA LV VFQ-48.
ResultadosSe reclutó a veintisiete sujetos con edad media de 84±6 años, de los cuales el 59,3% (16/27) eran mujeres. El 59,3% (16/27) de los sujetos no podían ver ninguna placa de estereoagudeza, el 25,9% (7/27) tenía estereoagudeza de 340 arcosegundos (arcseg), el 11,1% (3/27) tenía estereoagudeza de 170 arcseg y el 3,7% (1/27) tenía estereoagudeza de 85 arcseg. El índice de capacidad visual funcional general fue considerablemente superior en aquellos sujetos con estereopsis (2,25±0,99) que aquellos sin estereopsis (1,50±0,92) (p=0,028).
ConclusionesLos pacientes con BV y estereopsis tienen mejor índice de capacidad visual funcional general que los que no la tienen. Por tanto, la estereopsis deberá considerarse como un componente de la rehabilitación de la baja visión (RBV), y como una medición de los resultados en la investigación y práctica clínica.
Residual binocular visual functions can have a significant impact on routine activities of daily living (ADL); however; they are rarely assessed and documented in routine LV assessments.1 Loss of vision in one eye or both can have a profound effect on binocular visual functions. In most cases with LV, the fine balance of binocularity reached in the past is broken and emerging symptoms may disable many ADL as a result of binocular dysfunction.2
Stereopsis refers to our ability to appreciate depth, the ability to distinguish a relative physical distance between objects. It is possible to appreciate the relative location of objects using one eye (with monocular cues). However, it is the two slightly different views of a same object (disparate images) provided by each eye which allows stereoscopic depth discrimination.
One of the most prominent characteristics of stereopsis is that it is robust. Many aspects of stereopsis remain functional at least through the eighties and probably beyond this age. This applies in equal measures to central as well as peripheral stereopsis. Past research has demonstrated that stereopsis persists in spite of differences between the two eyes in spatial frequency of content viewed, contrast levels and magnification.3
Stereopsis is a visual function which by definition is directly related to visual acuity.4 It is the level of visual acuity in the poorer eye which defines the level of stereopsis which can be achieved in a certain individual.5 Fine stereopsis can be achieved therefore only in those who have good visual acuity and therefore good macular function also in the poorer seeing eye. Hence in those with a loss of the macular function only gross stereopsis could be present.6
Patients with central visual disparities between the two eyes will preserve peripheral fusion.7 Since peripheral fusion is as potent as central fusion, peripheral stereopsis may be present in low vision cases, as evidenced by the excellent spatial orientation and mobility skills noticed in many of such patients. Studies show that binocular dysfunctions are prevalent in LV patients although stereopsis is present in about two thirds of tested subjects.8,9 All references in this paper relate to low vision subjects who lost macular function and hence relate to residual gross stereopsis.
Depth perception is an essential component of many ADL. It is required for better space as well as for accurate perception of distant, intermediate and near targets. Very few studies in the past addressed the issue of residual stereopsis and LV. None addressed the impact of loss of stereopsis on ADL relevant to LV patients. It is the intent of this paper to address this last issue.
MethodsThis is a prospective non-randomized observational case series. Consecutive cases were recruited from LV clinics and retina subspecialist offices in Toronto during 12 consecutive months. The study was performed in adherence to the guidelines of the Declaration of Helsinki. The study protocol was approved by the Research Ethics Committee of the University Health Network of Toronto and informed consent was obtained from each participant.
The study protocol included assessment of visual acuity and stereopsis with appropriate testing methods as well as an interview to obtain information on functional difficulties accordingly to a standard functional vision questionnaire. All was done in one single session.
Inclusion criteria include: documented AMD, LV with BCVA of 20/50–20/400 in the better eye, and study subjects between the ages of 50 and 90 years. Exclusion criteria include: apparent cognitive impairment, other retinal pathology, history of strabismus or strabismus surgery, amblyopia, significant ocular media opacity and uniocular patients.
Demographic details on age and sex were collected as well as details of refractive error.
Monocular best corrected visual acuity (BCVA) was measured with the Early Treatment Diabetic Retinopathy Study (ETDRS) charts. Normal indoor background illumination was supplemented with a 60W frosted incandescent bulb positioned behind the subject and 1m away from the testing sheet. All lighting provided a luminance of 133lx units at the level of the testing sheet. Testing was done at 1m distance and BCVA correction was provided to the subject for optimal viewing at the testing distance. All testing was done in a clinical setting.
Stereoacuity was measured using the near Frisby Stereotest (http://www.frisbystereotest.co.uk). Whereas in the Wirt test the stereoscopic effect is artificially produced by superimposing two dissimilar pictures and separating them by viewing them through a polarizing spectacle, the Frisby test presents targets which are actually ‘in depth’. The targets are actually ‘in depth’, because they are printed on the two sides of transparent plates of different thicknesses. There are three plates, 1mm, 3mm and 6mm thick, respectively. Each plate has four squares of random dot patterns, one square having the central portion printed on the opposite side of the plate from the surrounding portion. Viewed against a featureless background, for example a sheet of white paper, and with head and test held reasonably steady, the only clue to depth perception is binocular parallax. In this case it is the difference between the two levels, related to the distance from the observer, and the PD, which provides a measure of stereo acuity. As there are four patterns on each plate, they can be presented in any one of four positions and with either side facing the patient, so that the small area may appear in front of or behind the level of the surrounding pattern. The possibility of accurate guessing is thus practically eliminated, particularly as each plate maybe presented repeatedly in various positions without the patient being able to learn the correct response. The test can be held at any of six distances, from 30cm to 80cm. The six positions, combined with the three thicknesses of plates, provide 18 values of stereo acuity, from 880s of arc to 20s. These could be extended by increasing or decreasing the viewing distance.
The choice of using the Frisby Stereotest was made having in mind the difficulties experienced by LV patients to perform tasks at near distance. This choice seems to be even more appropriate because of possible cognitive deficiencies experienced by many in this group of patients. The Frisby Stereotest pictures are random dot patterns. This is especially advantageous in LV patients. Random dot stereograms are usually printed on cards to be viewed in a stereoscope with some separating device. The Frisby test differs from the printed stereograms in that no spectacles or other separating device need to be worn by the patient which could add another degree of difficulty to the testing protocol.
The VA LV VFQ-4810 was used to test functional visual abilities. The VFQ-48 questionnaire is a validated evaluation tool that measures overall functional visual ability (OFVA) with four visual function subdomains (reading, mobility, visual motor skills, and visual information processing). The responses obtained with the VA LV VQF-48 questionnaire were entered into an excel spreadsheet quitar which calculated a score for visual ability based on a validated algorithm for each of the four subdomains as well a total representative abilities score.
Assessment of vision related abilities could be done using various tests and methods developed over the years. The VA LV VFQ-48 which we used in this study incorporates Rasch analysis which reflects in a comprehensive way the true ability of the individual on a certain task. Rasch analysis assumes that the attribute of interest can be ordered from less to more, it can be represented by a one-dimensional variable and the probability that the individual will give a certain response is solely a function of the difference between the magnitude of the attribute for that person and the magnitude of the attribute required to give that specific response.11
Primary outcome measures selected for this study were residual stereopsis estimates and ADL scores.
Data analysis was based on descriptive statistics that include frequency distributions, a measure of central tendency (mean) and a measure of dispersion (standard deviation). A statistical comparison of means between populations was made by t-test. Differences were considered to be statistically significant at a P-value of less than 0.05.
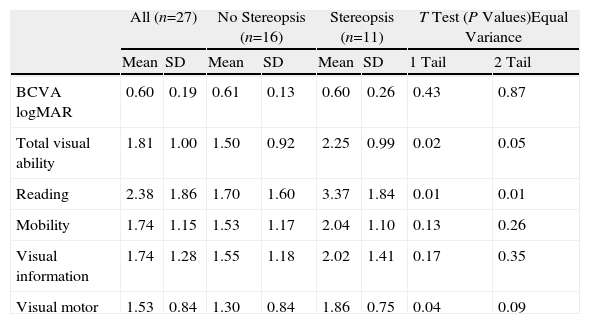
ResultsTwenty-seven subjects with mean age of 84±6 years old were recruited, of which 59.3% (16/27) were female. 59.3% (16/27) of the subjects were not able to see any stereoacuity plate, 25.9% (7/27) had stereoacuity of 340s of arc (SOA), 11.1% (3/27) had stereoacuity of 170 SOA and 3.7% (1/27) had stereoacuity of 85 SOA. Data are summarized in Table 1 with P values calculated for 1 and 2 tails T tests for equal variance. Mean BCVA was similar for those with stereopsis and those without stereopsis (P=0.437). Mean OFVA score was significantly higher in those with stereopsis than those without stereopsis (P=0.028). The stereopsis group had a significantly higher mean OFVA score than the no stereopsis group for reading (P=0.010) and visual motor skills (P=0.046). There was no significant difference between the two groups for the mean mobility score (P=0.133) and mean visual information processing score (P=0.177).
Impact of stereopsis on abilities.
| All (n=27) | No Stereopsis (n=16) | Stereopsis (n=11) | T Test (P Values)Equal Variance | |||||
| Mean | SD | Mean | SD | Mean | SD | 1 Tail | 2 Tail | |
| BCVA logMAR | 0.60 | 0.19 | 0.61 | 0.13 | 0.60 | 0.26 | 0.43 | 0.87 |
| Total visual ability | 1.81 | 1.00 | 1.50 | 0.92 | 2.25 | 0.99 | 0.02 | 0.05 |
| Reading | 2.38 | 1.86 | 1.70 | 1.60 | 3.37 | 1.84 | 0.01 | 0.01 |
| Mobility | 1.74 | 1.15 | 1.53 | 1.17 | 2.04 | 1.10 | 0.13 | 0.26 |
| Visual information | 1.74 | 1.28 | 1.55 | 1.18 | 2.02 | 1.41 | 0.17 | 0.35 |
| Visual motor | 1.53 | 0.84 | 1.30 | 0.84 | 1.86 | 0.75 | 0.04 | 0.09 |
SD: standard deviation.
Regression analysis showed that the highest correlation was present between stereopsis and mobility (R=0.424, P≤0.194 (t=1.404, DF=9)) abilities and to a lesser degree between stereopsis and BCVA (R=−0.1915, P≤0.573 (t=−0.5853, DF=9)) (Table 2).
Levels of stereopsis versus abilities.
| Stereo Sec | BCVA logMAR | Visual Ability | Reading | Mobility | Visual Information | Visual Motor |
| 170 | 0.50 | 2.33 | 2.49 | 1.67 | 3.04 | 1.83 |
| 85 | 0.80 | 1.04 | 0.18 | 1.68 | 0.73 | 1.10 |
| 340 | 0.50 | 2.15 | 3.66 | 0.69 | 2.81 | 2.22 |
| 340 | 0.40 | 2.98 | 3.07 | 2.79 | 3.04 | 2.65 |
| 170 | 0.30 | 3.27 | 5.82 | 2.89 | 2.81 | 2.43 |
| 340 | 0.70 | 2.56 | 5.82 | 2.79 | 1.21 | 2.22 |
| 340 | 1.10 | 0.58 | 1.63 | 0.24 | 0.25 | 0.23 |
| 170 | 1.00 | 0.91 | 2.06 | 1.03 | -0.77 | 1.07 |
| 340 | 0.50 | 2.36 | 3.05 | 1.84 | 2.60 | 2.02 |
| 340 | 0.50 | 3.22 | 3.57 | 3.48 | 3.29 | 2.65 |
| 340 | 0.30 | 3.39 | 5.82 | 3.40 | 3.29 | 2.04 |
| BCVA | R=−0.1915, P<=0.573 (t=−0.5853, DF=9) | |||||
| Visual ability | R=0.355, P<=0.284 (t=1.13, DF=9) | |||||
| Reading | R=0.424, P<=0.194 (t=1.404, DF=9) | |||||
| Mobility | R=0.17, P<=0.6175 (t=0.5175, DF=9) | |||||
| Visual info | R=0.3559, P<=0.2835 (t=1.142, DF=9) | |||||
| Visual motor | R=0.31, P<=0.34 (t=0.99, DF=9) | |||||
Binocular viewing is the most common viewing condition in daily life for all, either for those who are visually impaired or for those who are not. Whereas stereopsis may require binocular retinal correspondence, binocular viewing may not require such a prerequisite. Hence residual stereopsis in LV patients after macular function loss presents an intriguing proposition. Modern concepts of residual visual functions confirm that residual stereopsis as reported in this study is possible.
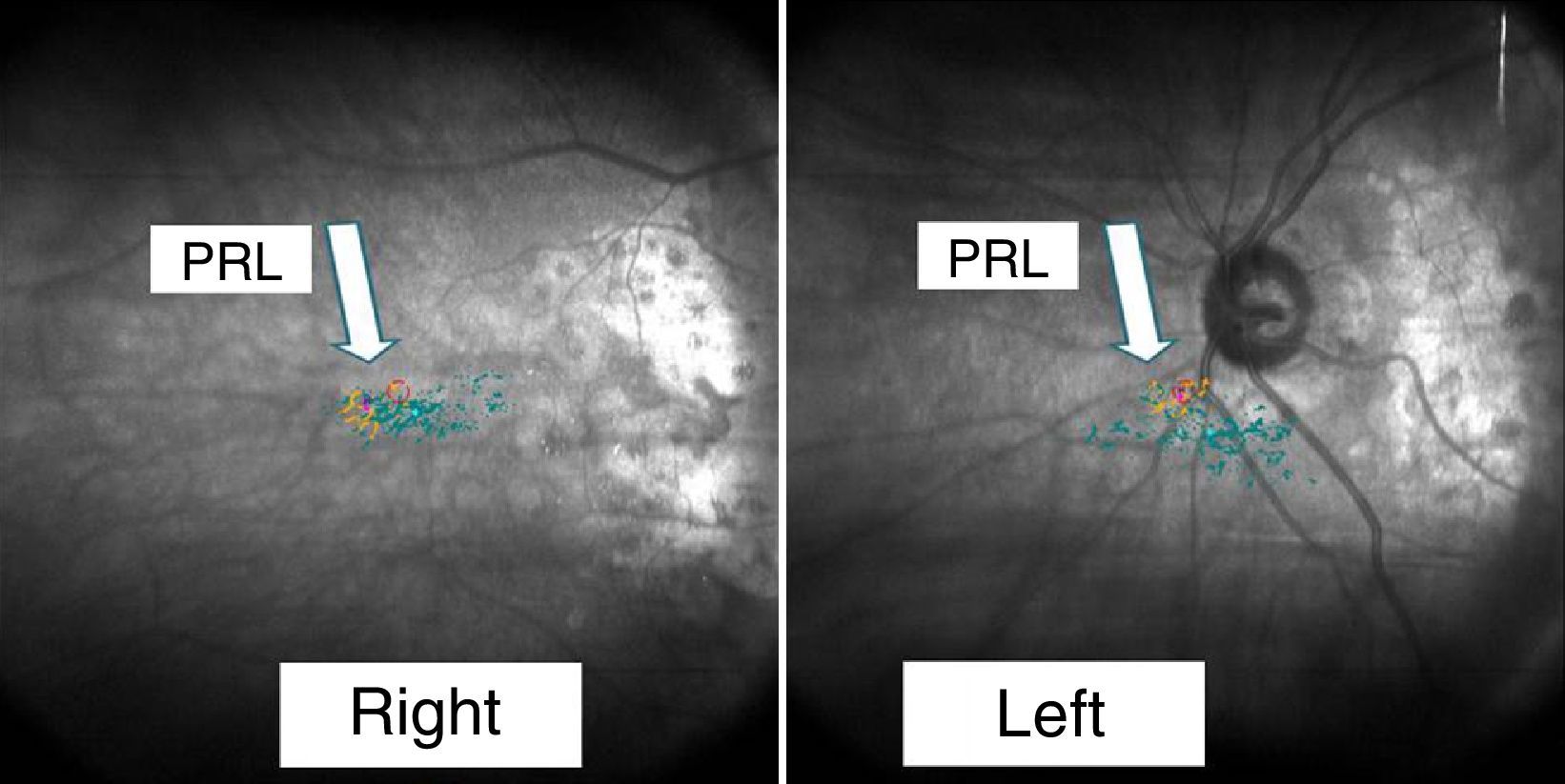
New observations show that following macular function loss a preferred retinal loci (PRLs) is developed and in turn assume partial macular functions.
The PRLs are topographical fixation areas on the retina which represent fixation attempts, central or eccentric, during viewing of targets. Development of PRLs occurs naturally in most cases when macular visual function is lost and exhibits dynamic performances. Such PRLs can be developed on any part of the residual retina, can be single or multiple, are apparently related to performance of specific tasks and offer superior visual function unmatched by any other locus on the retina.12 In those with macular function loss, like AMD cases, the majority of PRLs detected occur in the upper and the right quadrant of the retina which correspond to the inferior and left parts of the visual field.13 In Stargardt's disease and other macular dystrophies most PRLs tend to be localized on the upper retina.14
Today's instruments commonly known as microperimeters embody the technological abilities required to assess components of residual visual functions and functional vision. Most significantly microperimeters also extended our abilities to assess residual visual function in those with poor fixation stability and/or with eccentric fixation patterns. Microperimeters are the direct result of applications based on newer technologies based on Scanning Laser Ophthalmoscopy (SLO) as well as newer computing and eye tracking devices.15
In a recent study it was shown that in spite of large differences in visual acuity between the two eyes in low vision cases affected by AMD, in 51% of cases PRLs develop on corresponding retinal areas.16 (Fig. 1). This observation is very much in line with our findings in this current study. Among all subjects tested in our study 40.7% showed various levels of stereopsis.
Our results also show that perhaps not all who develop PRLs on corresponding retinal areas have stereopsis. An explanation to impaired stereopsis in low vision cases is probably provided by a previous paper8 which reports a significant correlation between impaired depth perception and cognition, regardless of levels of visual acuity.
Binocular deficiencies which affect fusion of images from both eyes and impact summation, inhibition, and rivalry functions may offer another explanation for stereopsis impairment.17 Recent studies on cases with AMD found binocular contrast inhibition in almost half of the study cases, mostly in the low and medium spatial frequencies18 which suggests dominance of the poorer eye under binocular conditions. This could be responsible for metamorphopsia experienced by many low vision patients as well as for impaired stereopsis.
In daily life, it is argued that impairments rating should be considered and reported as the best-corrected binocular visual function, rather than the best-corrected visual function for the better eye. This can easily be documented and reported for visual acuity, for the contrast sensitivity function and for residual fields. Visual acuity abilities can be measured easily with ETDRS charts. One point is given for each letter read correctly, with scores calculated for each eye and for a binocular test. The 3 visual acuity score values are combined into a single personal functional acuity score (FAS), with 60% of the weight given to the binocular value and 20% to each of the monocular values. A similar method can be used for calculating binocular contrast sensitivity function scores for a selected spatial frequency and also for calculating functional field scores. Such estimates may be more adequate to show correlation with ADL scores.
As expected, our study indeed confirms that those who retained stereopsis demonstrated OFVA scores higher than those who did not. Also stereopsis was correlated with higher abilities scores for reading and visual motor skills. No such correlation could be found with BCVA. In fact mean BCVA was not significantly different (P=0.44) between those retaining stereopsis and those not retaining it (Table 1). In those who retained stereopsis, mobility skills abilities were found to present the higher correlation with stereopsis, as may be expected (Table 2).
There is sizable evidence published in the literature that those who are visually impaired perform poorer during their ADLs than normal sighted individuals. This was demonstrated for many ADL such as reading, writing, shopping, indoor and outdoor orientation and mobility.19
We believe that our paper makes a modest contribution by demonstrating that documenting residual stereopsis in low vision cases may offer additional understanding of residual functional abilities in low vision cases. However documentation of residual visual functions like stereopsis following devastating pathology is only one aspect of the vision rehabilitation process. Ultimately, a patient's QOL depends entirely on optimizing all residual vision related skills. One of the purposes for demonstration of predictor correlations between residual visual functions and ADL is to devise methods and devices which can ultimately improve ADL. Refraction is a first step in this aspect. A recent study showed that a significant improvement in visual acuity could be attained by refraction in low vision cases, in the better-seeing as well as in the worse-seeing eye.20 In clinical practice this can be achieved easily by refraction of both eyes and prescription of eye ware which restores BCVA to each eye, to the better one as well as to the poorer one.
Testing for stereopsis during routine assessments of low vision patients may provide additional clarification on residual functional visions. It may also offer clues on the suitability of binocular low vision devices in some cases and possibly predict the success rate with such devices.
Our study is limited by the small numbers enrolled and by the limited outcome measures selected. Hence it should be viewed as a pilot study. Our hope is that ideas presented in this paper will be followed and developed by further research by others for the benefit of our patients.
Conflicts of InterestThe authors have no conflicts of interest to declare.
Presented at Research Day, Department of Ophthalmology and Vision Sciences, University of Toronto, Ontario, Canada, May 9, 2010.