To determine the relationship between peripheral refraction at the horizontal retina, axial length and parental history of myopia between myopic adults who have positive parental myopia and those with negative parental myopia.
Methods69 males and 44 females in the age range of 18–25 years were assigned either a negative parental myopia (NPM) or positive parental myopia (PPM) group. In the corrected and uncorrected states, peripheral refractive error was measured up to 30° horizontally in 10° steps using an open field autorefractor. Axial length was measured using an Opto US1000 Fine A-Scan Ultrasonography (model US1000).
ResultsRelative peripheral refractive error showed more hyperopic defocus that was statistically significantly more increased in the positive parental myopia group than in the negative parental myopia group (P ≥ 0.02). The overall mean ± SD axial length of all subjects was 23.38 ± 0.32 mm (range 23.01–25.01 mm). The study showed a statistically significant difference (P = 0.005) in axial lengths of young adult myopes (23.45 ± 0.36 mm) with parental myopia compared to those with similar spherical equivalent refraction who have non-myopic parents (23.28 ± 0.19 mm).
ConclusionThere was significantly more hyperopic defocus at 30° N and 30° T retina in the corrected states of young adult myopes who had myopic parents compared to their counterparts with non-myopic parents.
The correlation between refraction and the eye’s axial length is as high as 0.89, therefore the axial length is regarded as the main component that determines the eye’s refractive state.1,2 In an eye with minimal refractive error (an emmetropic eye), the components, that is, its axial length matches the combined focal length of the cornea and crystalline lens. Earlier studies suggest that by age 13 years, the components of an emmetropic eye would have matched and reached its adults size.3 However, an eye with refractive error such as the hyperopic or myopic eye would show a mismatch between its components. In the myopic eye, the axial length exceeds the combined focal lengths of the cornea and crystalline lens. In a cross-sectional study,4 had determined the importance of the axial length to myopia onset in children aged 6–14 years who were enrolled in the Orinda Longitudinal Study of Myopia. The study had compared axial elongation between children with positive parental myopia (PPM) and those with negative parental myopia (NPM). Even before the myopia started,4 found that children with positive parental myopia had longer axial lengths compared to those with negative parental myopia. In addition, the study showed that, refractive error and axial lengths of parents and children were positively correlated.
Further, Mutti et al.5 showed a relationship between refractive error and axial length. The team had followed about 979 emmetropic children aged between 6–14 years and of diverse ethnicity for nine years in the Collaborative Longitudinal Evaluation of Ethnicity and Refractive Error (CLEERE) Study. Six hundred and five (605) of these children were found to have longer axial lengths at baseline and became myopic during follow up compared to three hundred and seventy-four (374) of them, whose axial lengths did not change and remained emmetropic. Children who became myopic had longer axial lengths before and after the onset of myopia compared to their counterparts who remained emmetropic.
Two myopic parents, one myopic parent and no myopic parent have 30–40 %, 20–25 % and 6–10 % of their children being myopic respectively.2,6,7 In addition, the odds ratio for children myopia is 2.05 when the child has one myopic parent and about 4.92 when there are 2 myopic parents compared to those without myopic parents.7,8
Whereas the contribution of genes (hereditary) to the progression of axial elongation is more consistent with previous studies, that of extensive reading to axial elongation seems less consistent.9,10 However, the rate of axial elongation seems to increase when a child is between ages 6 and 8 years.11 Once the rate of axial length starts, it could progress until the child turns 15–16 years when it may slow, but the that may still progress into the mid-20’s.12,13
On the contrary, Goss and Erikson14, found that juvenile myopia could continue to progress even after age 16 years. It is thus expected that when the 18 year old myopic student continues to perform extensive near work, his/her eyes axial length might continuously elongate and probably cause myopia to progress further.15–17 The basic rule is that for every 0.3 mm increase in axial length there is a corresponding progression of 1D in myopia.18
Due to increased axial length, myopic eyes have been found to be differently shaped compared to emmetropic and hyperopic eyes.19 While emmetropic and hyperopic eyes are found to be oblate in shape (longer equatorial diameter than the axial length), myopic eyes are said to be less oblate where the axial length is more elongated than the equatorial diameter.7 This implies that the relative peripheral refractive errors in the horizontal meridians (both temporal and nasal retina) of the myopic eye are relatively more hyperopic compared to the hyperopic and emmetropic eyes.20–22 It is thus expected that young adult myopes with similar spherical equivalent refraction would have similar peripheral refraction at the eccentricities.23 Our hypothesis for this study was; young adult myopes with or without parental myopia with similar axial lengths should have similar relative peripheral refractive errors in the uncorrected states, and similar conditions should prevail after optimum refractive correction. The purpose of this study therefore was to determine the relationship between axial lengths, peripheral refraction at the horizontal retina and parental history of myopia, between myopic adults who have positive parental myopia and those with negative parental myopia.
Methods and materialsThe committee on Human Research, Publication and Ethics of the School of Medical Sciences, Kwame Nkrumah University of Science and Technology, reviewed and approved the study. Informed consent was received from the subjects. The study was conducted in accordance with the tenets of the Declaration of Helsinki.
Written and electronic advertisements were circulated among university students. Students who voluntarily responded to and submitted their informed consent forms were enrolled into the study. Eye examinations took place at the Optometry Teaching Clinic of the Department of Optometry and Visual Science, in Kwame Nkrumah University of Science and Technology, Kumasi. Students were selected based on the following inclusion criteria: normal ocular health, age between 18 and 25 years (inclusive), none of the students were undergoing orthok, visual acuity of 0.00 Log MAR or better in both eyes with habitual spectacles, spherical equivalent refraction (SER) of −1.00 to −4.00 D in each meridian when measured by cycloplegic refraction, astigmatism of ≤ 1.00, anisometropia of ≤ 1.00 D. Another inclusion criterion for students was that both parents had normal healthy eyes and had evidence of recent eye examination and/or spectacle/contact lens prescriptions and would submit their consent forms. Students excluded from the study were amblyopic, allergic to cycloplegic agents, undergoing treatment to manage myopia with multifocal optical lenses or pharmacological agents, had one myopic parent and one non-myopic parent, and /or had a history of contact lens wear. The study was conducted between April 14, 2017 and July 16, 2017.
ProceduresAfter joining the study, a subject was assigned to either the negative parental myopia (NPM) or positive parental myopia (PPM) group. The PPM group was defined as young adults who had both parents being myopic, and the NPM group was defined as young adults who had neither parent being myopic. Parents’ refractive status were obtained partly through forwarded emails from their optometrists and manual delivery of prescription forms by wards. In the NPM group, both parents were not myopic but were either emmetropic or hyperopic of SER ≤ 0. 50 D and ≥ 0.75 D respectively in each meridian, astigmatism ≤ 1.00 D and ≤ 1.00 D anisometropia. In the positive parental myopia group both parents were myopic with spherical equivalent refraction of myopia greater than or equal to -2.00 D in each meridian, astigmatism of 1.00 D and ≤ 1.00 D anisometropia and the parental myopia should have started before age 15 years.
Cycloplegic autorefractions was performed on subjects so that full myopic error was estimated at the central retina. Cycloplegic autorefraction was performed on both eyes, but only results in the right eye were used for analysis. Cycloplegia was achieved by instilling a drop each of cyclopentolate 1% and 0.5 % tropicamide eye drops into each eye. After five minutes, a second drop of each drop was instilled, and a period of 30 min allowed before pupil responses were examined to determine if cycloplegia had occurred for measurements to be taken. Cycloplegia was achieved if there was maximum pupillary dilatation ≥6 mm and unresponsiveness to light. The Shin Nippon NVsion K5001 autorefractor (marketed as Grand Seiko WR 5100K Japan) was used to measure cycloplegic refraction.
Non-cycloplegic objective and subjective refraction were performed before cycloplegic agents were instilled on each subject so that the distant prescription obtained was compared to their habitual prescriptions. The end-point of subjective refraction was reached using the minimum minus for best acuity principle.
The open field autorefractor allowed targets to be observed at different distances and angles. Subjects were instructed to fixate binocularly on targets placed at a distance of 6 m, hanged on a horizontal wooden structure at 0°, 10°, 20° and 30° in the nasal and temporal visual fields, with the reticle mark maintained over the center of a clear image of the pupil on the autorefractor’s LCD screen. Measurements were taken with and without subjects’ habitual spectacles. Five measurements of refraction were taken at each eccentricity of the right eye only. Subjects rotated their eyes to look at the targets. These targets were red LED that were lit so that subjects could maintain that focus with and without their habitual spectacles. These measurements were done using the Shin-Nippon (Grand Seiko) NVision-K5001 in a room with luminance range of 120 lux–130 lux. Measurements of axial lengths were also taken using an Opto US1000 Fine A-Scan Ultrasonography (model US1000). All measurements were done by the same examiner, and five readings were taken and the average was used. The measurements were taken between 3 pm and 6 pm.
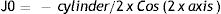
Statistical analysisData was analyzed using Microsoft Excel and Stata 11. The sphero-cylindrical refractive error of subjects was decomposed into power vector form according to the equation by Ref.24
S, C and axis are the spherical, cylindrical and cylindrical axis components of the sphero-cylindrical refractive error respectively. M is the mean spherical equivalent refractive error.
J0 represents with and against- the- rule astigmatism and J45 is for oblique angles from 45 to 135°.
To determine whether differences exist between the peripheral refraction at any eccentricity and that at the central retina, the relative peripheral refractive error (RPRE) was calculated as the difference between mean refraction at the fovea and periphery whether uncorrected or corrected
where Mi is the mean refraction at the eccentricities and M0 represents mean refraction at the fovea.Spherical equivalent refractions for parents were calculated using Eq. (i).
To determine whether there was difference in mean RPRE between PPM and NPM groups at 30 T and 30 N, the RPRE was calculated as in the uncorrected and corrected states respectively.
where u and c represent mean refraction in the uncorrected, and the corrected eye respectively at 30 T or 30 N.To determine whether there was a difference in axial length between subjects in the PPM and NPM groups an unpaired t-test was used.
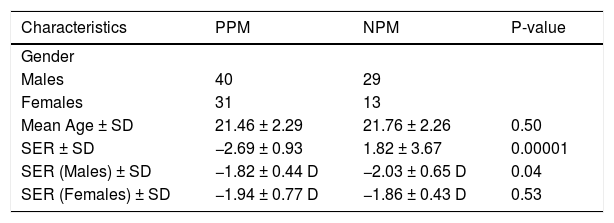
ResultsSubjects demographicsThis study included 69 males and 44 females. The overall mean age ± SD of subjects was 21.49 ± 2.23 years. The mean age for male and female subjects were 21.47 ± 2.24 years and 21.52 ± 2.23 years respectively (P = 0.89). There was no statistically significant difference in age between subjects in the positive parental myopia and negative parental myopia groups (P = 0.50). The overall mean spherical equivalent refraction (SER) on-axis for all subjects was −1.91 ± 0.60 D (range −1.22 to −4.44 D). The mean spherical equivalent refraction on-axis for female and male subjects was −1.94 ± 0.69 D (range −0.1.22 to −4.44 D) and −1.89 ± 0.54 D (−1.22 to −3.87 D) respectively (P = 0.66). There was no statistically significant difference in the SER between the PPM and NPM group. The gender distribution and mean spherical equivalent refraction ± SD for participants in positive parental myopia group and negative parental myopia groups are shown in Table 1.
Demographic distribution and mean SER for participants in PPM and NPM groups.
| Characteristics | PPM | NPM | P-value |
|---|---|---|---|
| Gender | |||
| Males | 40 | 29 | |
| Females | 31 | 13 | |
| Mean Age ± SD | 21.46 ± 2.29 | 21.76 ± 2.26 | 0.50 |
| SER ± SD | −2.69 ± 0.93 | 1.82 ± 3.67 | 0.00001 |
| SER (Males) ± SD | −1.82 ± 0.44 D | −2.03 ± 0.65 D | 0.04 |
| SER (Females) ± SD | −1.94 ± 0.77 D | −1.86 ± 0.43 D | 0.53 |
PPM = positive parental myopia; NPM = negative parental myopia; SER = spherical equivalent refraction.
The overall mean spherical equivalent refraction of the right eyes of both parents was −0.93 ± 3.25 D (range −5.00 to 2.62 D). The difference in mean central spherical equivalent refraction between positive parental myopia (−2.69 ± 0.93 D) and negative parental myopia (1.82 ± 3.67 D) groups was statistically significant (P = 0.00001)
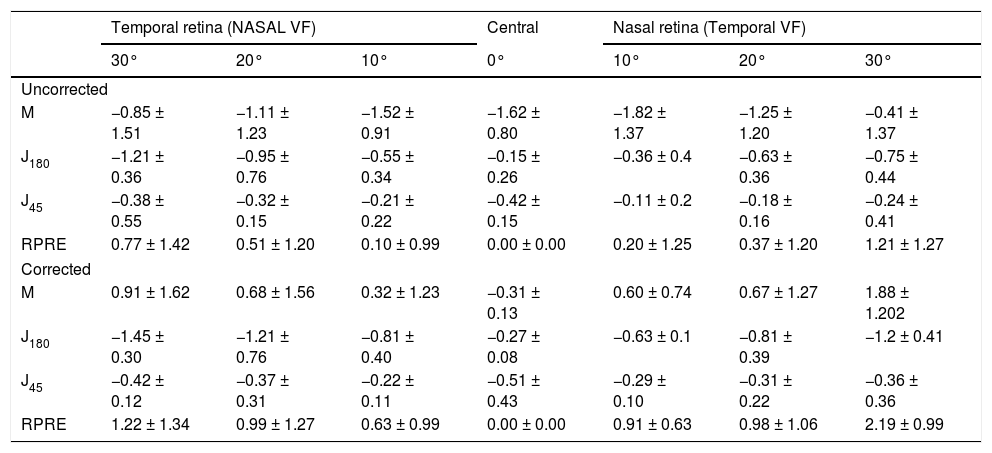
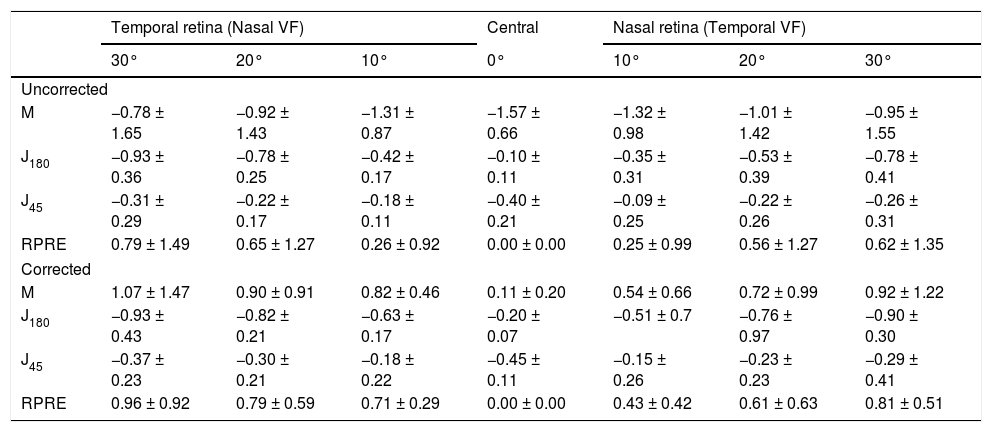
Spherical equivalent refraction (M) in the uncorrected statesIn the uncorrected state, negative values were seen at all horizontally eccentric locations in both positive parental myopia (Table 2) and negative parental myopia (Table 3) groups. However, these negative values were relatively more hyperopic at the eccentricities than at the fovea. In the uncorrected state, M at 30 °N and 30° T were not statistically significantly different (P-value ≥ 0.07) between the positive parental myopia and negative parental myopia groups (Tables 2 and 3).
Mean ± SD of M, J180, J45, and RPRE for Myopes with Positive Parental Myopia (PPM).
| Temporal retina (NASAL VF) | Central | Nasal retina (Temporal VF) | |||||
|---|---|---|---|---|---|---|---|
| 30° | 20° | 10° | 0° | 10° | 20° | 30° | |
| Uncorrected | |||||||
| M | −0.85 ± 1.51 | −1.11 ± 1.23 | −1.52 ± 0.91 | −1.62 ± 0.80 | −1.82 ± 1.37 | −1.25 ± 1.20 | −0.41 ± 1.37 |
| J180 | −1.21 ± 0.36 | −0.95 ± 0.76 | −0.55 ± 0.34 | −0.15 ± 0.26 | −0.36 ± 0.4 | −0.63 ± 0.36 | −0.75 ± 0.44 |
| J45 | −0.38 ± 0.55 | −0.32 ± 0.15 | −0.21 ± 0.22 | −0.42 ± 0.15 | −0.11 ± 0.2 | −0.18 ± 0.16 | −0.24 ± 0.41 |
| RPRE | 0.77 ± 1.42 | 0.51 ± 1.20 | 0.10 ± 0.99 | 0.00 ± 0.00 | 0.20 ± 1.25 | 0.37 ± 1.20 | 1.21 ± 1.27 |
| Corrected | |||||||
| M | 0.91 ± 1.62 | 0.68 ± 1.56 | 0.32 ± 1.23 | −0.31 ± 0.13 | 0.60 ± 0.74 | 0.67 ± 1.27 | 1.88 ± 1.202 |
| J180 | −1.45 ± 0.30 | −1.21 ± 0.76 | −0.81 ± 0.40 | −0.27 ± 0.08 | −0.63 ± 0.1 | −0.81 ± 0.39 | −1.2 ± 0.41 |
| J45 | −0.42 ± 0.12 | −0.37 ± 0.31 | −0.22 ± 0.11 | −0.51 ± 0.43 | −0.29 ± 0.10 | −0.31 ± 0.22 | −0.36 ± 0.36 |
| RPRE | 1.22 ± 1.34 | 0.99 ± 1.27 | 0.63 ± 0.99 | 0.00 ± 0.00 | 0.91 ± 0.63 | 0.98 ± 1.06 | 2.19 ± 0.99 |
VF = visual field; RPRE = relative peripheral refractive error.
Mean ± SD of M, J180, J45, and RPRE for Myopes with Negative Parental Myopia (NPM).
| Temporal retina (Nasal VF) | Central | Nasal retina (Temporal VF) | |||||
|---|---|---|---|---|---|---|---|
| 30° | 20° | 10° | 0° | 10° | 20° | 30° | |
| Uncorrected | |||||||
| M | −0.78 ± 1.65 | −0.92 ± 1.43 | −1.31 ± 0.87 | −1.57 ± 0.66 | −1.32 ± 0.98 | −1.01 ± 1.42 | −0.95 ± 1.55 |
| J180 | −0.93 ± 0.36 | −0.78 ± 0.25 | −0.42 ± 0.17 | −0.10 ± 0.11 | −0.35 ± 0.31 | −0.53 ± 0.39 | −0.78 ± 0.41 |
| J45 | −0.31 ± 0.29 | −0.22 ± 0.17 | −0.18 ± 0.11 | −0.40 ± 0.21 | −0.09 ± 0.25 | −0.22 ± 0.26 | −0.26 ± 0.31 |
| RPRE | 0.79 ± 1.49 | 0.65 ± 1.27 | 0.26 ± 0.92 | 0.00 ± 0.00 | 0.25 ± 0.99 | 0.56 ± 1.27 | 0.62 ± 1.35 |
| Corrected | |||||||
| M | 1.07 ± 1.47 | 0.90 ± 0.91 | 0.82 ± 0.46 | 0.11 ± 0.20 | 0.54 ± 0.66 | 0.72 ± 0.99 | 0.92 ± 1.22 |
| J180 | −0.93 ± 0.43 | −0.82 ± 0.21 | −0.63 ± 0.17 | −0.20 ± 0.07 | −0.51 ± 0.7 | −0.76 ± 0.97 | −0.90 ± 0.30 |
| J45 | −0.37 ± 0.23 | −0.30 ± 0.21 | −0.18 ± 0.22 | −0.45 ± 0.11 | −0.15 ± 0.26 | −0.23 ± 0.23 | −0.29 ± 0.41 |
| RPRE | 0.96 ± 0.92 | 0.79 ± 0.59 | 0.71 ± 0.29 | 0.00 ± 0.00 | 0.43 ± 0.42 | 0.61 ± 0.63 | 0.81 ± 0.51 |
VF = visual field; RPRE = relative peripheral refractive error.
In the corrected states, positive values of M were seen at all eccentricities in both the positive parental myopia and negative parental myopia groups and the values were relatively more hyperopic than that at the fovea. When subjects wore their habitual spectacles, there was asymmetry seen in M between 30° T and 30° N and the difference was statistically significant in positive parental myopia group (P = 0.001). However, in the negative parental myopia group, the difference was not statistically significant (P = 0.61). At 30° T and 30° N, the difference in M between the corrected and uncorrected myopic eye was statistically significant in both the positive parental myopia and negative parental myopia groups (P ≤ 0.003)
Relative peripheral refractive error (RPRE) in the uncorrected statesIn the uncorrected state, there was asymmetry seen in relative peripheral refractive error between the temporal and nasal retina in both groups, however the asymmetry was not statistically significantly different between 30° T and 30° N in both groups (P ≥ 0.58)
Relative peripheral refractive error (RPRE) in the corrected statesIn the corrected state, asymmetry was seen between the temporal and nasal eccentricities in the relative peripheral refractive error at 30° T and 30° N retina locations. The difference in value was statistically significantly different in the positive parental myopia group (P = 0.0001) but not in the negative parental myopia group (P = 0.35). Relative peripheral refractive error showed more hyperopic defocus that was statistically significantly more increased in the positive parental myopia group than in the negative parental myopia group (P ≥ 0.02).
Astigmatism (J180 and J45)The mean amount of J180 and J45 in the uncorrected eyes of subjects in the positive parental myopia and negative parental myopia groups are shown in Tables 2 and 3. At 30° temporal retina in the uncorrected eye, the value of J180 was statistically significantly higher in the positive parental myopia than in the negative parental myopia group, however at 30° nasal retina the amount of J180 did not differ between the two groups. In both groups, the amount of J180 was significantly lower in the central retina than in all off-axis retinal locations (all P = 0.001). As shown in Table 2, the presence of the spectacle lens caused significant difference at 30° temporal and nasal retina (P ≤ 0.001) in the positive parental myopia group. However, as shown in Table 3 the spectacle lens did not cause a statistically significant difference at 30° temporal and nasal retina the negative parental myopia group. The spectacle lens caused significantly higher astigmatism in J180 in the positive parental myopia than in the negative parental myopia group (P = 0.0001).
The mean amount of J45 at 30° temporal and nasal retina in the uncorrected eye of subjects in the positive parental myopia and negative parental myopia groups did not differ statistically significant1y (P ≥ 0.44) In both groups, spectacles lenses did not cause a statistically significant difference in J45 at 30° temporal or 30° nasal retina (P ≥ 0.29). Between the positive parental myopia and negative parental myopia groups, the difference caused in J45 by the subjects’ habitual spectacle lens was not statistically significantly different (P ≥ 0.13)
Axial length (AL)The overall mean ± SD of all subjects was 23.38 ± 0.32 mm (range 23.01–25.01 mm). The correlation between mean axial length and mean myopia of the overall group was 0.73. There was a statistically significant difference found between the axial lengths of the two groups (P = 0.005). In the PPM group, the mean ± SD axial length in males was statistically significantly more elongated than the females (P = 0.03). However, there was no statistically significant difference between the mean ± SD axial length in males and females in the NPM group (P = 0.38).
DiscussionThe unique finding of this study is that, in this young myopic adult population, the mean relative peripheral refractive error at 30° nasal retina for uncorrected subjects in the positive parental myopia group and negative parental myopia group was 1.21 ± 1.27 and 0.62 ± 1.35 respectively, which were statistically significantly different (P-value = 0.02). Those with myopic parents showed statistically significantly higher relative hyperopic refraction at 30° T and 30° N than their counterparts whose parents were not myopic (P ≤ 0.02). Although, the difference in mean on-axis refraction between those in the positive parental myopia and negative parental myopia groups was not statistically significantly different (P = 0.50), the mean axial length of subjects in the positive parental myopia group was statistically significantly longer than those in the negative parental myopia group (P = 0.0001). In addition, the mean axial length of males in the positive parental myopia groups is statistically significantly longer than their counterparts in negative parental myopia group (P = 0.00001). Further, the spherical equivalent refraction of males in the negative parental myopia group (−2.03 ± 0.65 D) was statistically significantly more myopic than their counterparts in the positive parental myopia group (P = 0.04). In addition, the difference in mean on-axis refraction of parents of subjects in the positive parental myopia group was statistically significantly more myopic than their counterparts in the negative parental myopia group (P = 0.00001).
Spherical equivalent refraction (M) in the uncorrected eyes of both groups showed negative values in the central and horizontal visual fields. However, relative to the central retina, M showed increased relative hyperopia as eccentricity increased. The result seen in this study is in agreement with that reported in previous studies.25,26–29
In the uncorrected eye, the relative peripheral refractive error (RPRE) of both groups increased from the central retina to the periphery within the horizontal visual field. This finding is in agreement with other studies that also worked on adults.25,30 At 30° nasal retina, RPRE in the uncorrected eye of the positive parental myopia group showed more relative hyperopia than the negative parental myopia group (P = 0.02). Although, refraction at the central retina for the two groups were not statistically significantly different, the difference at the nasal peripheral retina suggests that the eyes of subjects in either groups with similar central refraction could differ in shape.
When subjects wore their single vision spectacle correction, hyperopic refraction was seen at all eccentricities and peripheral hyperopia relative to the central retina increased as eccentricity increased in the positive parental myopia group but not in the negative parental myopia group. Increase in hyperopic defocus in the peripheral retina is probably related to axial length which was more pronounced in the positive parental myopia group than in the negative parental myopia group. Axial growth of the eye reaches its emmetropic size by age 13 years,3 however for a few children, the eye continues to elongate even beyond age 16 years until they become adults.13 It is thus difficult to determine whether the elongation of the eye beyond 16 years is as a result of heredity only or environmental factors only or an interaction between heredity and the environment.16,31,32 Nevertheless, a few studies have failed to associate education with myopia onset and its progression.33,34
Axial elongation is closely related to myopia onset and its progression.2,35 In this study, the axial length of those in positive parental myopia group was significantly (P = 0.005) more elongated compared to their counterparts in the negative parental myopia group. Although this study was conducted among adults, it could be that the findings in the studies from previous studies4,9 could be extrapolated to adults because their subjects would eventually become adults. This finding is supported by the previous studies4,9, who evaluated children and found that those with two myopic parents had more elongated axial lengths compared to those with one parent or those without myopic parent before myopia starts. Further, Saw et al.36, who also worked on children found that those who had myopic parents showed about −0.63 D myopia progression in a year while those without myopic children showed about −0.42 D yearly progression. In this study males in the PPM group showed significantly elongated axial length compared to the females in the same group. This finding is in agreement with that found in previous studies37,38 who worked on children aged 7–15 years. However, another study that explored the relationship between intra ocular pressure, myopia or its progression and axial length found no difference in baseline axial length between males and females with mean age 15.94 ± 4.16 years.39
Previous results showed myopes to have predominantly prolate-shaped eyes.40 In this study, the J180 at 30° temporal in the uncorrected positive parental myopia was found to be significantly higher than that at the corresponding angle in the negative parental myopia group. This finding indicates that the geometric shape of individuals with myopic parents against individuals without myopic parents is not the same even with similar spherical equivalent refractive errors. These findings were similar to that found in a cohort study using participants of a similar age range.40
ConclusionOur study suggests young myopic adults with positive parental myopia had both increasing axial length and increasing peripheral hyperopic defocus as compared to their counterpart with negative parental myopia.
There was significantly more hyperopic defocus at 30° N and 30° T retina in the corrected states of young adult myopes who had myopic parents compared to their counterparts with non-myopic parents. The study showed a statistically significant difference (P = 0.001) in axial lengths of young adult myopes (23.45 ± 0.56 mm) with parental myopia compared to those with similar spherical equivalent refraction (SER) who have non-myopic parents (23.28 ± 0.32 mm).