The aim of this study was to assess and compare clinical characteristics of bilateral keratoconus patients with unilateral Vogt's striae.
MethodsIn this contralateral eye study, refractive status were evaluated in patients with bilateral keratoconus whose corneas had definite slit-lamp biomicroscopic evidence of unilateral Vogt's striae. All cases underwent a comprehensive ophthalmic examination. Some refractive errors components provided by autorefraction were converted to vectorial notation for power vector analysis. Finally, the outcomes were compared between keratoconus eyes with and without Vogt's striae.
ResultsFifty patients aged 20 to 38 years (27.43±5.5) were recruited in this study. The results showed a significant difference in uncorrected distance visual acuity (UDVA), corrected distance visual acuity (CDVA), non-cycloplegic and cycloplegic autorefraction including sphere, cylinder, spherical equivalent, and J0, between keratoconus eyes with and without Vogt's striae (all P<0.05), except for J45 (P=0.518 in non-cycloplegic autorefraction and P=0.574 in cycloplegic autorefraction). Comparison of cycloplegic and non-cycloplegic autorefraction in both study groups showed significant differences in the sphere and spherical equivalent (all P<0.001), but no significant difference was found in cylinder, J0, and J45 between the study groups (all P>0.05).
ConclusionsComparison of the cycloplegic and non-cycloplegic autorefraction in keratoconus eyes with and without Vogt's striae showed significant differences in UDVA, CDVA, and some refractive errors components provided by autorefraction between the two groups, with a worse condition in KCN eyes with Vogt's striae.
One of the typical biomicroscopic characteristic signs of keratoconus (KCN) is Vogt's striae, which can be unilateral or bilateral.1,2 Vogt's striae, also known as dark and light banding patterns and stress lines, are tiny vertical or rarely horizontal lines crossing the corneal depth.3–6 With progression of KCN, refractive errors including myopia and astigmatism increase through microstructural alterations in the cornea.7 Measurement of refractive errors using manifest and/or autorefraction is important to assess visual acuity and disease progression in eyes with KCN. Also, better visual acuity is achieved with subjective refraction compared to autorefraction in patients with KCN.8 Since KCN has an asymmetric entity, visual acuity and refractive error have been considered as the key indicators of KCN to determine the better eye and the worse eye.8,9 In addition, refractive error and Vogt's striae are two of the important parameters for classification, evaluation, monitoring, and rehabilitation of KCN10–13; therefore, characterization of KCN eyes with and without Vogt's striae by their refractive status is clinically important.6,10
Objective and subjective refraction techniques are considered as two procedures for determining the refractive status of the eye.14,15 In objective refraction, non-cycloplegic and cycloplegic autorefraction methods have been used widely in clinical practice; consequently, the difference between the autorefraction outcomes with and without cycloplegia has gained increasing attention over the past years.14,16 Bagheri and colleagues investigated the difference between these two methods in adults and reported a significant difference between non-cycloplegic and cycloplegic autorefraction.16 Another study reported that non-cycloplegic autorefraction overestimates myopia in adults.17
Although, a number of studies have assessed corneal characteristics with respect to the presence of Vogt‘s striae,3–6,18,19 only Mocan et al. compared the refractive errors between KCN eyes with and without Vogt's striae.19 To our knowledge, no study has compared cycloplegic and non-cycloplegic autorefraction in KCN eyes with and without Vogt's striae; therefore, this contralateral eye study was designed to assess and compare cycloplegic and non-cycloplegic autorefraction in patients with bilateral KCN with unilateral Vogt's striae.
MethodsThis cross-sectional contralateral eye study was conducted at Sedaghat Eye Clinic (Mashhad, Iran). Considering the cross-sectional nature of the study, the sampling was performed based on pilot study. Therefore, one hundred eyes of 50 patients with bilateral KCN and unilateral Vogt's striae were included in the study. The subjects had the same ethnicity (Caucasian). The study was conducted in accordance with the tenets of the Declaration of Helsinki, and written informed consent was obtained from all subjects. In addition, the study was approved by the Ethics Committee of Mashhad University of Medical Sciences. (Code number: 950806).
A consistent diagnosis of KCN was made by an expert corneal refractive surgeon (MRS) based on slit-lamp signs and the results of corneal topography/tomography. The inclusion criteria were clinical signs on slit-lamp biomicroscopy (Vogt's striae, Fleischer's ring, apical thinning, etc.),2,20 topographic signs of KCN (skewed asymmetric bow-tie, inferior steepening, etc.),21 and tomographic manifestations of KCN (abnormal elevation, pachymetry, and Belin/Ambrosio Enhanced Ectasia Display maps).22 Also, eyes with subclinical or forme fruste KCN were excluded from the study because this study focused on clinical KCN.
Subjects with a history of ocular surgery; corneal cross-linking, scar, inflammation, and opacity; and those with severe keratitis, severe dry eye, soft or hard contact lens use during the last three weeks before the examination, cataract, glaucoma, intraocular pressure – lowering drugs, pregnancy, lactation, KCN suspect, pellucid marginal corneal degeneration, and systemic diseases were excluded from the study.
The subjects underwent a complete ophthalmic examination, including a comprehensive case history, uncorrected and corrected distance visual acuity (UDVA & CDVA), noncycloplegic and cycloplegic autorefraction using cyclopentolate 1% by an auto kerato-refractometer (Topcon KR-1; Topcon Medical Systems, Inc., Tokyo, Japan), assessment of irregularity of the retinoscopic reflex or scissoring reflex in both eyes, slit-lamp biomicroscopy (Haag-StreitBM900 slitlamp, HAAG-STREIT Surgical GmbH, Koeniz, Switzerland), Scheimpflug-based anterior segment tomography (Pentacam HR, Oculus, Optikgerate GmbH, Wetzlar, Germany), and placido disc-based corneal topography (TMS4, Tomey, Enlargen, Germany). The spectacle CDVA was achieved using retinoscopy and subjective refraction before cycloplegia in both study groups. Visual acuity was recorded in decimal notation and converted to logarithm of the minimum angle of resolution (LogMAR) for statistical analysis.
In order to reduce probable errors related to the measuring time, all the measurements were done between 04:00 pm and 06:00 pm by one experienced optometrist. Based on the manufacturers’ instructions as well as the quality states and indices provided by the imaging instruments, measurements were accepted and erroneous measurements were repeated after 5min.
KCN eyes were divided into two groups: group with biomicroscopic evidence of Vogt's striae and group without Vogt's striae.
According to the staging scheme in the Collaborative Longitudinal Evaluation of Keratoconus (CLEK) study, KCN eyes were staged with respect to keratometry reading of the steepest corneal meridian measured by placido disc-based corneal topography into mild (<45 diopters [D]), moderate (45–52 D) and severe KCN (>52 D).12
Non-cycloplegic automated refraction was done using the Topcon KR-1 auto kerato-refractometer at a distance of about 5cm from the patient's eye.
Cycloplegia was achieved by instillation of cyclopentolate (CICLOPLEGICO, ALCON CUSI, S.A., El Masnou-Barcelona) into each eye twice at an interval of 10min. The participants were cautioned about subsequent symptoms of cyclopentolate use. Forty minutes after cyclopentolate instillation, measurements were repeated using the Topcon KR-1 auto kerato-refractometer.23 The mean of three readings was recorded as refraction in the conventional manner (sphere, cylinder, and axis) in both non-cycloplegic and cycloplegic states.
Power vector analysis described by Thibos and Horner was used to compare the refractive error components between the two study groups.24 Using the method, the conventional spherocylindrical refraction was converted to power vector coordinates and expressed by three dioptric powers: M, J0, and J45, where M is the spherical equivalent (SE) of the given refractive error, and J0 and J45 are the two Jackson cross cylinder equivalents to the conventional cylinder.
Statistical analysisStatistical analysis was performed using the SPSS version22 for Windows (IBM Inc., Chicago, Illinois, USA). The normal distribution of the parameters was assessed using the Kolmogorov–Smirnov test. The paired-sample t test or its non-parametric equivalent (the Wilcoxon signed rank test) was used to compare the mean of each refractive component before and after cycloplegia. Comparison of each refractive component between the eyes with and without Vogt's striae was done using the independent-sample t test or Mann–Whitney U test for both conditions.
Pearson correlation and intraclass correlation coefficients (ICC) with their 95% confidence intervals were used to assess the correlation between each refractive component. Poor, fair, moderate, strong and very strong agreements were defined base on ICC values of 0–0.2, 0.3–0.4, 0.5–0.6, 0.7–0.8 and more than 0.8, respectively.25P values less than 0.05 were considered statistically significant.
Ethical issuesThe Ethics Committee of Mashhad University of Medical Sciences approved the study protocol, which was conducted in accord with the tenets of the Helsinki Declaration. All participants signed a written informed consent.
ResultsFrom the 50 patients with bilateral KCN who had unilateral Vogt's striae, 34 were males (68%) and 16 were females (32%). The mean age of the participants was 27.4±5.5 years (range: 20 to 38 years).
In KCN eyes with Vogt's striae, 2 (4%), 10 (20%), and 38 (76%) eyes had mild, moderate, and severe KCN; while, in group without Vogt's striae, mild, moderate, and severe KCN was seen in 11 (22%), 28 (56%), and 11 (22%) eyes, respectively. Considering the low numbers of KCN eyes in subgroups, we only reported the numbers of KCN eyes in each subgroup and we did not compare the statistical differences between subgroups.
The mean and standard deviation of UDVA in KCN eyes with and without Vogt's striae were 0.63±0.41 and 0.31±0.35 LogMAR and mean CDVA for the two groups were 0.28±0.26 and 0.06±0.10 LogMAR, respectively. Paired-sample T test showed a significant difference in UDVA (P<0.001) and CDVA (P<0.001) between two groups.
Mean and standard deviation of non-cycloplegic and cycloplegic autorefraction in both study groups and their comparison between KCN eyes with and without Vogt's striae are presented in Table 1. KCN eyes with Vogt's striae had statistically higher absolute values of sphere, cylinder, spherical equivalent, and J0 compared to the eyes with no Vogt's striae on both noncycloplegic and cycloplegic states.
Non-cycloplegic and cycloplegic autorefraction outcomes of keratoconus eyes with and without Vogt's striae.
| Parameter | CR or NCR | Study group | Mean±SD | Range | Mean difference | P-value |
|---|---|---|---|---|---|---|
| Sph (D) | NCR | With VS | −3.62±2.53 | −8.75 to +0.50 | −1.82±2.10 | <0.001* |
| Without VS | −1.77±1.78 | −6.75 to +0.75 | ||||
| CR | With VS | −2.68±2.55 | −8.75 to +1.75 | −1.97±2.19 | <0.001* | |
| Without VS | −0.71±1.51 | −4.25 to +1.50 | ||||
| Cyl (D) | NCR | With VS | −5.10±2.27 | −9.75 to −1.50 | −2.84±2.66 | <0.001* |
| Without VS | −2.20±1.90 | −8.75 to 00.00 | ||||
| CR | With VS | −4.90±2.16 | −9.50 to −1.75 | −2.81±2.32 | <0.001* | |
| Without VS | −2.08±1.70 | −8.25 to 00.00 | ||||
| SE (D) | NCR | With VS | −6.20±2.91 | −13.00 to −0.50 | −3.20±2.31 | <0.001** |
| Without VS | −3.01±2.31 | −9.00 to +0.25 | ||||
| CR | With VS | −5.20±2.90 | −13.00 to −0.25 | −3.39±2.52 | <0.001* | |
| Without VS | −1.81±1.99 | −8.50 to +1.00 | ||||
| J0 | NCR | With VS | 1.24±1.58 | −2.92 to 4.37 | 0.94±1.30 | <0.001* |
| Without VS | 0.29±1.00 | −2.17 to 2.81 | ||||
| CR | With VS | 1.24±1.60 | −2.81 to 4.11 | 0.92±1.26 | <0.001* | |
| Without VS | 0.32±0.92 | −1.76 to 2.62 | ||||
| J45 | NCR | With VS | 0.28±1.91 | −4.04 to 3.35 | 0.17±2.61 | 0.518* |
| Without VS | 0.12±1.02 | −3.35 to 2.85 | ||||
| CR | With VS | 0.28±1.75 | −3.94 to 3.07 | 0.15±2.36 | 0.574* | |
| Without VS | 0.14±0.93 | −3.25 to 2.62 | ||||
VS: Vogt's striae, Sph: sphere, Cyl: cylinder, SE: spherical equivalent, J0: Jackson cross cylinder, axes at 0 and 90 degrees, J45: Jackson cross cylinder, axes at 45 and 135 degrees, SD: standard deviation, NCR: non-cycloplegic refraction, CR: cycloplegic refraction.
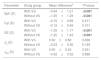
Conventional refractive components showed a statistically significant decrease in absolute values of sphere (P<0.001) and SE (P<0.001) after doing cyclopegia separately for eyes with and without Vogt's striae, while changes in cylinder (P>0.05) were not statistically significant. Similarly, there were no significant changes for the components J0 and J45. (P>0.05) (Table 2).
Refractive error changes between non-cycloplegic and cycloplegic autorefraction in keratoconus eyes with and without Vogt's striae.
| Parameter | Study group | Mean difference† | *P-value |
|---|---|---|---|
| Sph (D) | With VS | −0.94±1.01 | <0.001 |
| Without VS | −1.05±1.29 | <0.001 | |
| Cyl (D) | With VS | −0.15±0.89 | 0.211 |
| Without VS | −0.12±0.49 | 0.101 | |
| SE (D) | With VS | −1.00±1.17 | <0.001 |
| Without VS | −1.20±1.43 | <0.001 | |
| J0 (D) | With VS | 0.00±0.60 | 0.838 |
| Without VS | −0.03±0.36 | 0.149 | |
| J45 (D) | With VS | 0.00±0.40 | 0.931 |
| Without VS | −0.02±0.32 | 0.886 | |
VS: Vogt's striae, Sph: sphere, Cyl: cylinder, SE: spherical equivalent, SD: standard deviation, J0: Jackson cross cylinder, axes at 0 and 90 degrees, J45: Jackson cross cylinder, axes at 45 and 135 degrees.
As shown in Table 3, there were strong correlations between non-cycloplegic and cycloplegic refractive outcomes in both study groups. (P<0.0001, r=0.723 to 0.983) Also, there was a high agreement between two statuses in both study groups based on ICC values.
Correlation and agreement between non-cycloplegic and cycloplegic autorefraction in keratoconus eyes with and without Vogt's striae.
| With vogt's striae | Without vogt's striae | |||||||
|---|---|---|---|---|---|---|---|---|
| P* | r | ICC | 95% CI | P|| | r | ICC | 95% CI | |
| Sph (D) | <0.0001 | 0.981 | 0.929 | 0.583–0.976 | <0.0001 | 0.723 | 0.808 | 0.390–0.919 |
| Cyl (D) | <0.0001 | 0.912 | 0.953 | 0.917–0.973 | <0.0001 | 0.941 | 0.983 | 0.970–0.991 |
| SE (D) | <0.0001 | 0.919 | 0.926 | 0.628–0.973 | <0.0001 | 0.778 | 0.860 | 0.489–0.944 |
| J0 | <0.0001 | 0.930 | 0.964 | 0.937–0.980 | <0.0001 | 0.876 | 0.968 | 0.944–0.982 |
| J45 | <0.0001 | 0.977 | 0.986 | 0.976–0.992 | <0.0001 | 0.885 | 0.975 | 0.957–0.986 |
Sph: sphere, Cyl: cylinder, SE: spherical equivalent, J0: Jackson cross cylinder, axes at 0 and 90 degrees, J45: Jackson cross cylinder, axes at 45 and 135 degrees, D: diopter, ICC: intraclass correlation coefficient, CI: confidence interval.
Considering the importance of Vogt's striae as an indicator of KCN,6 KCN eyes with Vogt's striae had worse UDVA and CDVA. Moreover, KCN eyes with Vogt's striae had higher absolute values of sphere, cylinder, SE, and J0 compared to KCN eyes without Vogt's striae in both non-cycloplegic and cycloplegic conditions. The association of Vogt's striae with worse vision and higher refractive errors can be used to determine the better eye in KCN patients to estimate the impact of disease on quality of vision and vision related quality of life. It has been suggested that treatment decisions should be considered on the better-seeing eye rather than the worse-seeing eye.9
In both groups, sphere and SE values of non-cycloplegic autorefraction were more myopic than the corresponding values in cycloplegic refraction. These findings agree with the results of Jorge et al., who described that the differences between non-cycloplegic and cycloplegic refraction in normal eyes are only due to the accommodative response.26 Jorge and colleagues performed retinoscopy and autorefraction in normal eyes26 but the refractive results of the present study has been reported using autorefraction in KCN eyes.
Additionally, the current study did not show any significant difference in cylinder, J0, and J45 between non-cycloplegic and cycloplegic autorefraction in either study group. Indeed, neither vertical and horizontal components (J0 power vector) nor oblique components (J45 power vector) of refractive astigmatism changed with cycloplegia in KCN eyes with and without Vogt's striae. These findings are not consistent with the result of previous studies in terms of J0 which revealed a significant difference between the J0 component of non-cycloplegic and cycloplegic refraction in normal subjects.26,27 This difference may be attributed to the eyes assessed; the present study was conducted in KCN eyes, while the above studies were performed in a large number of normal eyes.
No significant difference in the non-cycloplegic and cycloplegic autorefraction outcomes between the two groups may point to a similar accommodative response and consensual accommodation between the two eyes.28
In association between the presence of Vogt's striae and other microstructural corneal alterations in KCN patients using in vivo confocal microscopy, Mocan et al. reported considerable differences in refractive error components such as SE and cylinder between patients with and without Vogt's striae.19Their results are consistent with the current study, although they did not use power vector analysis. Another most important difference is the study design. The current work is a contralateral eye study to avoid any bias. In addition, it was not mentioned whether they performed manifest or cycloplegic refraction. As far as the theoretical level is concerned, astigmatism is a vector variable composed of the magnitude of power and axis; therefore, the vectorial property of astigmatism should be considered in comprehensive analysis of corneal astigmatism due to KCN.29
The evidence collected in the present study has made a number of contributions to the ongoing debate on the clinical importance of Vogt's striae for staging10,11 and treatment13 of KCN. There are numerous staging systems for the assessment and evaluation of KCN severity based on the presence or absence of Vogt's striae,10,11 but there is no evidence to show the association of Vogt's striae with worse refractive status in patients with KCN. Zadnik et al. stated high probability of Vogt's striae in more advanced KCN based on the association between the presence of Vogt's striae with steeper keratometric reading.12 They did not consider the visual acuity and refractive outcomes for their conclusion.
The aim of this study was not to explain the “causal relationship” between corneal Vogt's striae and refractive presentations, but to show the “association” of Vogt's striae with worse clinical refractive status in KCN eyes. This also accords with the earlier observations showing that Vogt's striae are associated with corneal tomographic and biomechanical deterioration.30,31
From the treatment viewpoint, Wisse et al. stated that UDVA was the most sensitive factor used to assess the effect of the intervention. Indeed, this factor was suggested in the Dutch Crosslinking for Keratoconus (DUCK) score for both defining and documentation of KCN progression to perform corneal cross-linking.13 Notably, the current contralateral comparative eye study showed worse UDVA in KCN eyes with Vogt's striae.
One of the limitation of this study was related to the asymmetric nature of KCN. Despite substantial advantages of contralateral eye-to-eye comparative studies, there are limitations in matching the grade of KCN between two study groups. In addition, although there are a number of KCN classification based on clinical findings such as corneal pachymetry,10,11 we only used the staging scheme in the CLEK study.12 Also, we did perform subjective refraction to achieve reliable CDVA but we did not report the subjective refractive components in the present study. The reason is that we aimed to compare the autorefraction outcomes between two study groups. Future research can compare the subjective refraction between both study groups.
It should be emphasized that the present study did not aim to describe the significance of Vogt's striae in KCN diagnosis. It has been shown that stress lines were not just associated with KCN. Grieve et al. reported these lines in the normal and edematous corneas; however, these lines were significantly more numerous in KCN eyes.6
A future study investigating the association of Vogt's striae with refractive, tomographic, and biomechanical corneal alterations in normal corneas would be very interesting.
In summary, comparison of the cycloplegic and non-cycloplegic autorefraction in KCN eyes with and without Vogt's striae showed significant differences in UDVA, CDVA, and refractive errors components between the two groups associated with a worse condition in KCN eyes with Vogt's striae. These findings propose that in clinical practice, when the vision and refractive characteristics of KCN eyes are evaluated, attention should be paid to the presence of Vogt's striae in the cornea. These results can be used in clinical evaluation, monitoring, and treatment of KCN patients with Vogt's striae.
Conflicts of interestThe authors have no conflicts of interest to declare.