To describe the prevalence and severity of photosensitivity in patients with albinism, and to compare with ocular features and how this correlated with use and choice of optical filters.
MethodsCross-sectional study on 81 participants with ocular or oculocutaneous albinism. An ophthalmic evaluation including visual acuity, contrast sensitivity and evaluation of iris translucency and fundus hypopigmentation was performed. Participants were offered optical rehabilitation with testing of a wide panel of filters. The associations between ocular characteristics, subjective photosensitivity complaints, and filter choice were evaluated.
ResultsPhotosensitivity was rated as “some” to “worst imaginable” in 77.8% of participants. Severity of photosensitivity correlated significantly with fundus hypopigmentation (p = 0.04) but not with iris translucency (p = 0.14) and it was worse in those with poor visual acuity but there was no association between photosensitivity and contrast vision. Seventy-four new pairs of spectacles were prescribed in the study. All outdoor spectacles contained a filter, whereas 26.5% of new indoor spectacles did not. Relatively neutral filter colors (gray, brown or a combination of gray and brown with other colors) and low transmission were preferred.
DiscussionPhotosensitivity is common in albinism, but research targeting treatment is limited. Color and neutral filters with a low light transmission were preferred, with participants having a large number of spectacles, presumably to meet their needs in different situations.
Albinism is a genetic condition characterized by complete or partial absence of melanin in skin, hair and eyes giving affected individuals a fair complexion. It is a rare disorder with an estimated prevalence of 1:20.0001 but the prevalence may vary between countries with different genetic background.2 The condition can be divided into different types, depending on the genetic cause and phenotypic characteristics.2,3 Oculocutaneous albinism (OCA) is a non-syndromic type of albinism with 7 subtypes (OCA1-OCA7) depending on the involved gene but where the underlying cause is an error in the melanin synthesis that affects pigmentation of ectodermally derived tissues.3 Ocular albinism (OA1) has so far been characterized by only involving the eyes3 but a recent study was unable to demonstrate pigmentary differences in skin, hair and eyes between individuals with ocular and oculocutaneous albinism.4 Finally, syndromic forms of albinism exist where albinism is associated with additional pathologic features e.g., Hermansky-Pudlak syndrome, Chediak-Higashi syndrome or Griscelli syndrome.
The characteristic ocular findings of albinism include foveal hypoplasia, transillumination of the iris, fundus hypopigmentation, optic nerve hypoplasia, and increased decussation of retinal ganglion cell axons of the optic chiasm.5 High refractive errors, including high degrees of astigmatism, low visual acuity, nystagmus, strabismus, amblyopia, decreased depth perception, lowered contrast sensitivity and photosensitivity are also common features.5 There are no commonly approved diagnostic criteria but Kruijt et al.6 have recently suggested a set of major and minor diagnostic criteria to distinguish albinism from other conditions with similar features.
Photosensitivity can be very pronounced in patients with albinism and may have an impact on the ability to perform everyday activities such as work-related or educational tasks, participate in outdoor activities such as sports or cultural events. In this study, we used the term photosensitivity to comprise all the problems patients may have with light from visual disability (e.g. disability glare and hemeralopia) to discomfort and pain (e.g. discomfort glare and photophobia).7 Photosensitivity in albinism is thought to be related to the absence of melanin in pigmented intraocular tissues such as the iris and uveal tract leading to increased intraocular light scattering. Photosensitivity may be alleviated by filters but there is very little evidence as to which type of filter to use and their effects. In general, optical filters may work by reducing the overall amount of light that reaches the eye, e.g. neutral density filters that have a constant attenuation of light across the visible spectrum, or by reducing specific part of the visible spectrum, e.g. colored filters such as yellow filters that absorb more strongly in the short wavelength part of the visible spectrum. Light scattering is more pronounced the shorter the wavelength of the light. This is one explanation why colored filters may be used to enhance contrast vision which can be useful in many cases of low-vision rehabilitation. However, colored filters may introduce dyschromatopsia.
The aim of this study was to describe the prevalence and severity of photosensitivity in patients with albinism and to evaluate how subjective photosensitivity correlates with ocular features such as iris transillumination, retinal hypopigmentation, visual acuity, contrast sensitivity and not least, how these factors affect the choices made by patients during optical rehabilitation offering a broad range of optical filters.
MethodsStudy designA prospective, cross-sectional study on patients with ocular or oculocutaneous albinism was conducted. Details of the study population has been reported previously.4 Participants were identified among patients who had been seen at the Kennedy Center Eye Clinic (KCEC) in Copenhagen, Denmark. The KCEC is a tertiary referral center specializing in optical rehabilitation of patients with low vision from rare or inherited eye diseases. The services are freely available to patients across the country. Participants were invited by mail to participate in the study. Non-respondents were contacted by telephone.
ExaminationParticipants were evaluated by a low vision optometrist and an ophthalmologist. Binocular and monocular best corrected visual acuity at distance (measured in visual acuity letter score using the ETDRS chart at 4 or 1 meter distance depending on visual acuity) and near (measured in visual acuity letter score using the Colenbrander mixed contrast card) was measured. Contrast sensitivity was measured using the Pelli-Robson chart at 1 meter distance using room light and a direct day light that gave an even illuminance of approximately 280 lux (range 265–380 lux) both on the center and the four corners of the chart. Subjective and objective refraction was determined on non-dilated eyes and in pre-presbyopic participants, a cycloplegic refraction was conducted as well, using two drops of cyclopentolate 1% administered in five-minute intervals.
A detailed optometric history was taken and included evaluation of all current optical aids such as glasses, contact lenses, binoculars and magnifiers. The transmission properties of filters were measured using a Humphrey Lens Analyzer model 360, Humphrey Instruments, Carl Zeiss Inc., USA.
Iris transillumination was evaluated on retroilluminated slit-lamp images focused on the iris and were graded from 0 (no transillumination) to 8 (complete transillumination) based on Wang et al.8 by an ophthalmologist (LK). For the statistical analyses, iris transillumination was sub-grouped into no transillumination (grade 0), mild transillumination (grade 1–2), moderate transillumination (grade 3–5) and severe transillumination (grade 6–8).
Fundus hypopigmentation was graded using 45-degree fundus photographs centered on the macula according to the four-grade scale by Kruijt et al.6 by an ophthalmologist (LK). Grade 0 indicates a normal degree of pigmentation, grade 1: hypopigmentation outside the vascular arcades, grade 2: hypopigmentation inside the arcades and grade 3: total hypopigmentation including the macula and fovea.
Participants were asked to grade their photosensitivity in 3 grades: “no or few problems”, “some or moderate problems”, “severe or worst imaginable problems”.
Optical rehabilitationAs part of the study, participants were offered one or more optical rehabilitation aids (spectacles, contact lenses or/and magnifiers) according to their needs. The rehabilitation item(s) of choice was free of charge for the participants and there was no limit on the number of aids they could choose. A broad set of filters was presented to the participants and the subjective effect/comfort was tested both indoor and outdoor. A full list of filters used in the study is available in Supplementary Table 1. First, the participants were asked to determine the degree of light attenuation they preferred starting with neutral gray filters, then they were asked to compare with color filters. The transmission of the chosen filter was measured by the Humphrey Lens Analyzer and the color of the filter classified in one of the following color categories: no filter, gray, brown, yellow-brown, gray-green, green, blue, purple, plum, yellow, orange, or red. The final choice of optical rehabilitation (spectacles, contact lenses, magnifiers, binoculars) and the spectral characteristics and degree of transmission was made by the participants based on their subjective experience and preference
Ethics and approvalsNo medical ethics approval and no informed consent form signatures were required for this study, because no invasive procedures were performed (decision number H-18016363 by the Medical Ethics committee for the Capital Region of Denmark). Review of medical files were approved by the Danish Patient Safety Authority (approval number 3-3013-2458/1). The study was approved by the Danish Data Protection Agency under the Capital Region of Denmark (P-2020-274). The stud followed the tenets of the Helsinki Declaration.
Statistical methodsData were presented using descriptive statistics. Associations between categorical data were analyzed using Chi-square tests (when all variables were categorical) or ANOVA (associations between categorical and continuous data). A p-value of 0.05 was considered statistically significant.
ResultsWe invited 120 patients to participate and 81 (43 males, 38 females) provided data for this study. The median age was 31 years (range 14–84). Participants were of Danish/North European (n = 67), Middle Eastern (n = 12) or African ethnicity (n = 2).
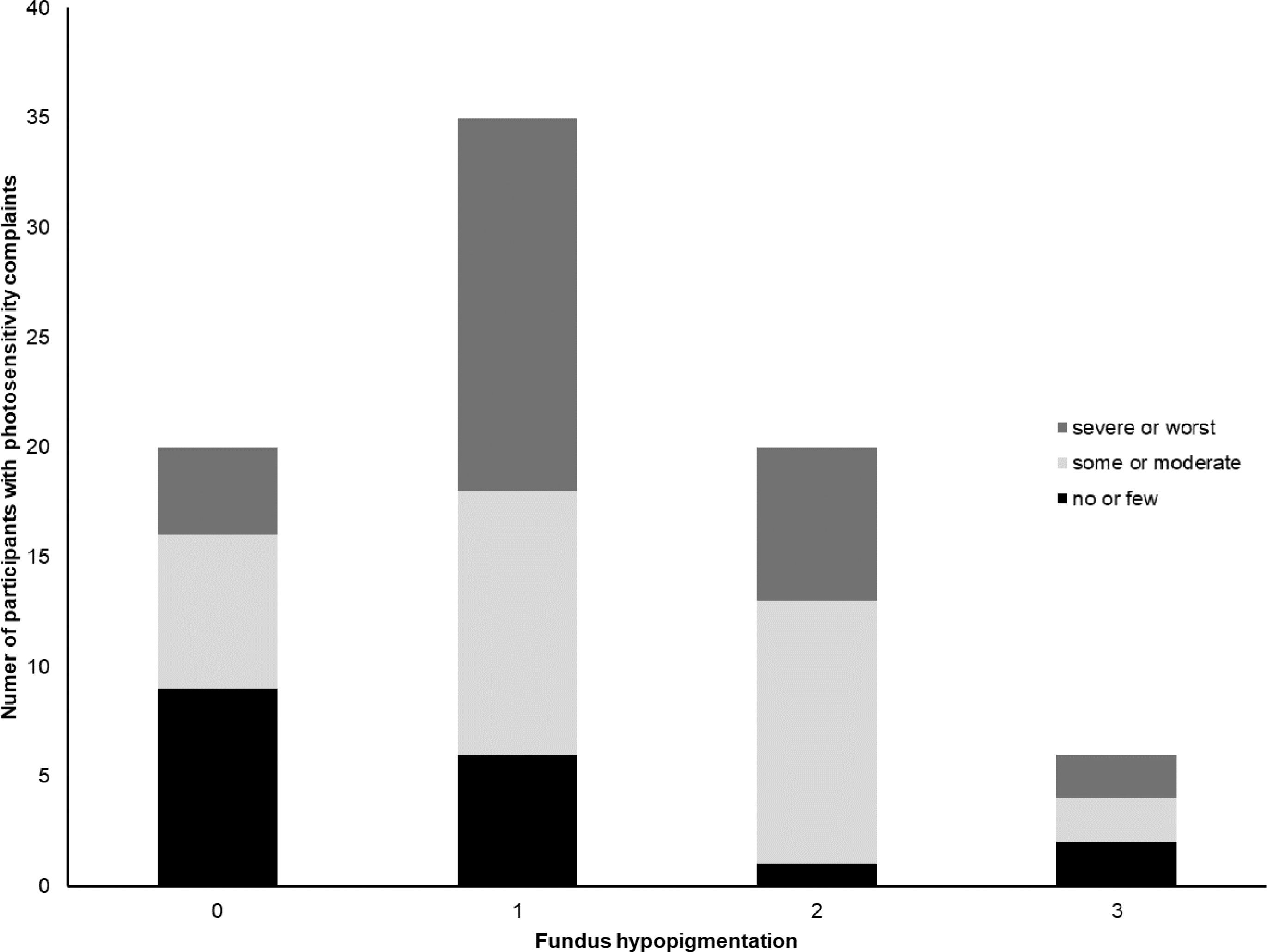
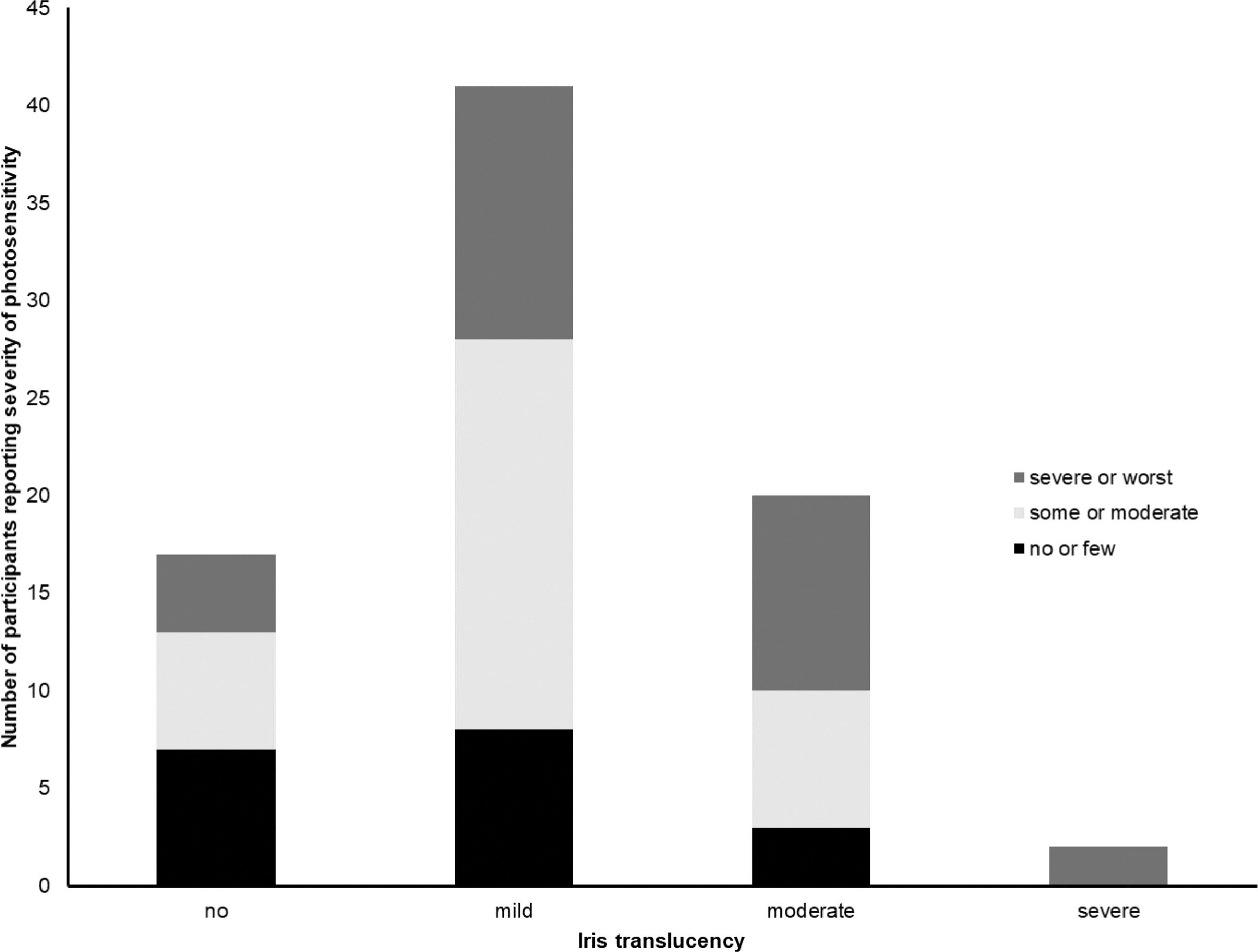
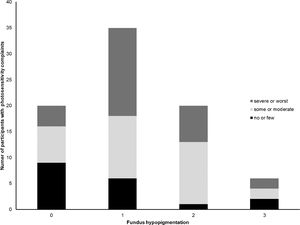
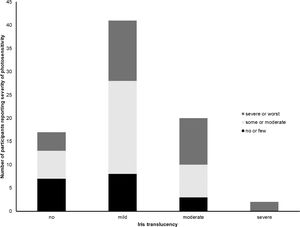
Severity of photosensitivity was graded subjectively by participants as “no or few problems” by 22.2% (n = 18), “some or moderate problems” by 40.8% (n = 33) and “severe or worst imaginable problems” by 37.0% (n = 30). Photosensitivity was greater in those with less pigmented fundi (chi-square, p = 0.04), see Fig. 1, whereas there was no significant association between subjective grading of photosensitivity and the degree of iris transillumination (chi-square=0.14), see Fig. 2.
Number of participants reporting severity of photosensitivity depending on the degree of fundus hypopigmentation according to a grading scheme by Kruijt et al.6 with grade 0 indicating a normal degree of pigmentation, grade 1: hypopigmentation outside the bending vessels, grade 2: hypopigmentation inside the bending vessels and grade 3: total hypopigmentation including the macula and fovea.
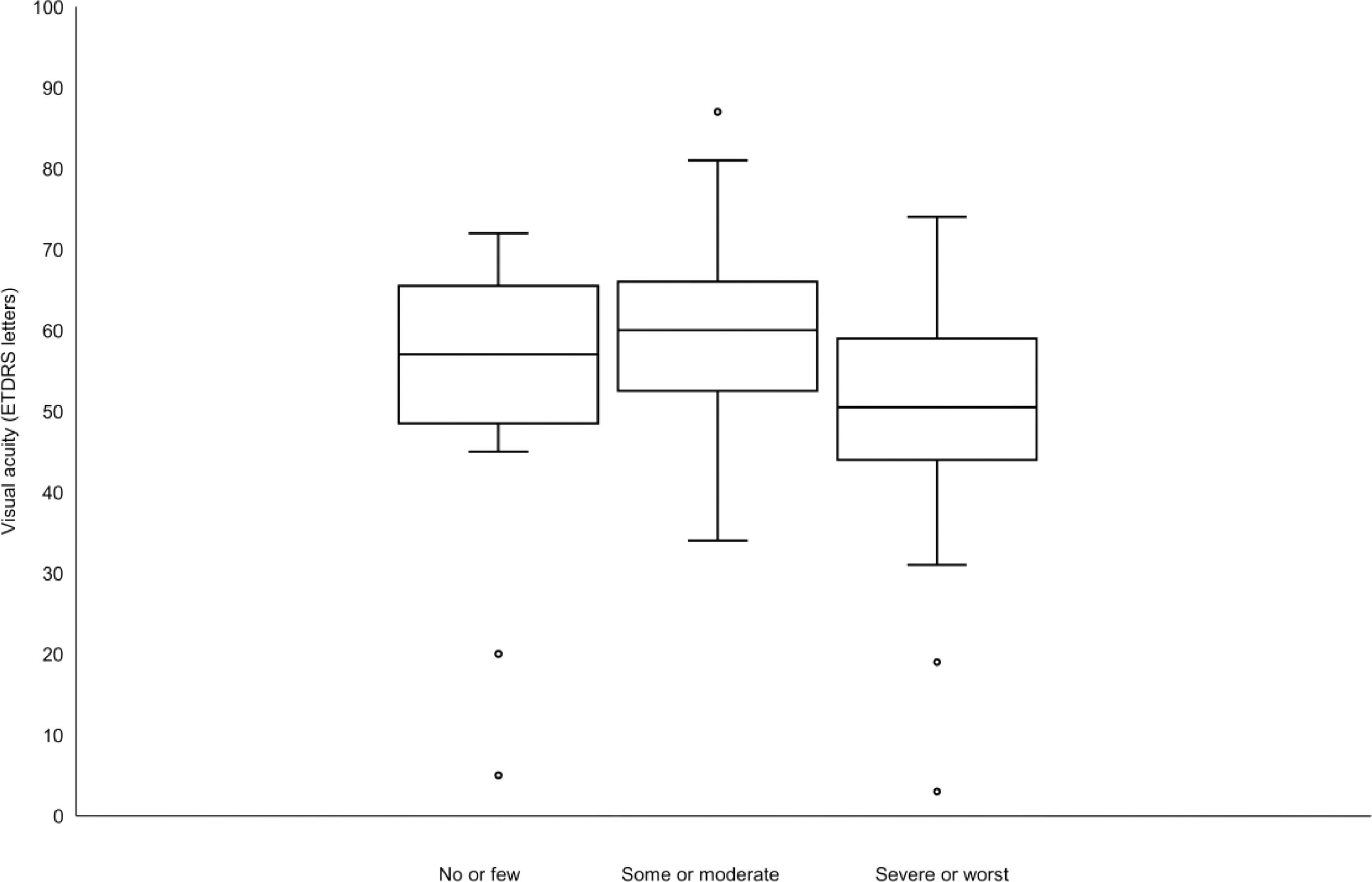
There was an inverse relationship between subjective rating of photosensitivity and visual acuity with worse grades of photosensitivity associated with lower visual acuities (ANOVA, p = 0.009, see Fig. 3) whereas there was no significant association between degree of photosensitivity and contrast sensitivity (ANOVA, p = 0.07).
Box-and-whiskers diagram showing visual acuity in relation to subjective rating of photophobia as “no or few problems”, “some or moderate problems” or “severe or worst imaginable problems”. The box represents the 25% and 75% percentiles with the median given as a horizontal line within the box. Whiskers represent minimum and maximum values, except when extreme outliers are present (circles). Then whiskers present 1.5 times the interquartile range of the first or third quartile.
The majority of participants (96.3%, n = 78) had one or more pair of spectacles before they entered the study, 46 participants (56.7%) had two pairs of spectacles or less, 21 (25.9%) had three pairs of spectacles, 7 (8.6%) had four pairs of spectacles and 4 (4.9%) had five pairs of spectacles. None used contact lenses. Those with more severe forms of photosensitivity had more spectacles, see Table 1.
All but five (6.2%) participants had one or more pair of spectacles with a filter. Among those who did not have a filter, three had no or few problems with photosensitivity and two had severe problems with photosensitivity. Thirty-four (42.0%) participants had spectacles specifically for indoor use – all with a filter. Sixty-two (76.5%) participants had spectacles specifically for outdoor use and all with a filter. Forty-six (56.8%) had spectacles that were used both indoor and outdoor of which 3 did not have a filter. Thirteen (16.0%) had a specific set of reading spectacles of which 3 did not have filter.
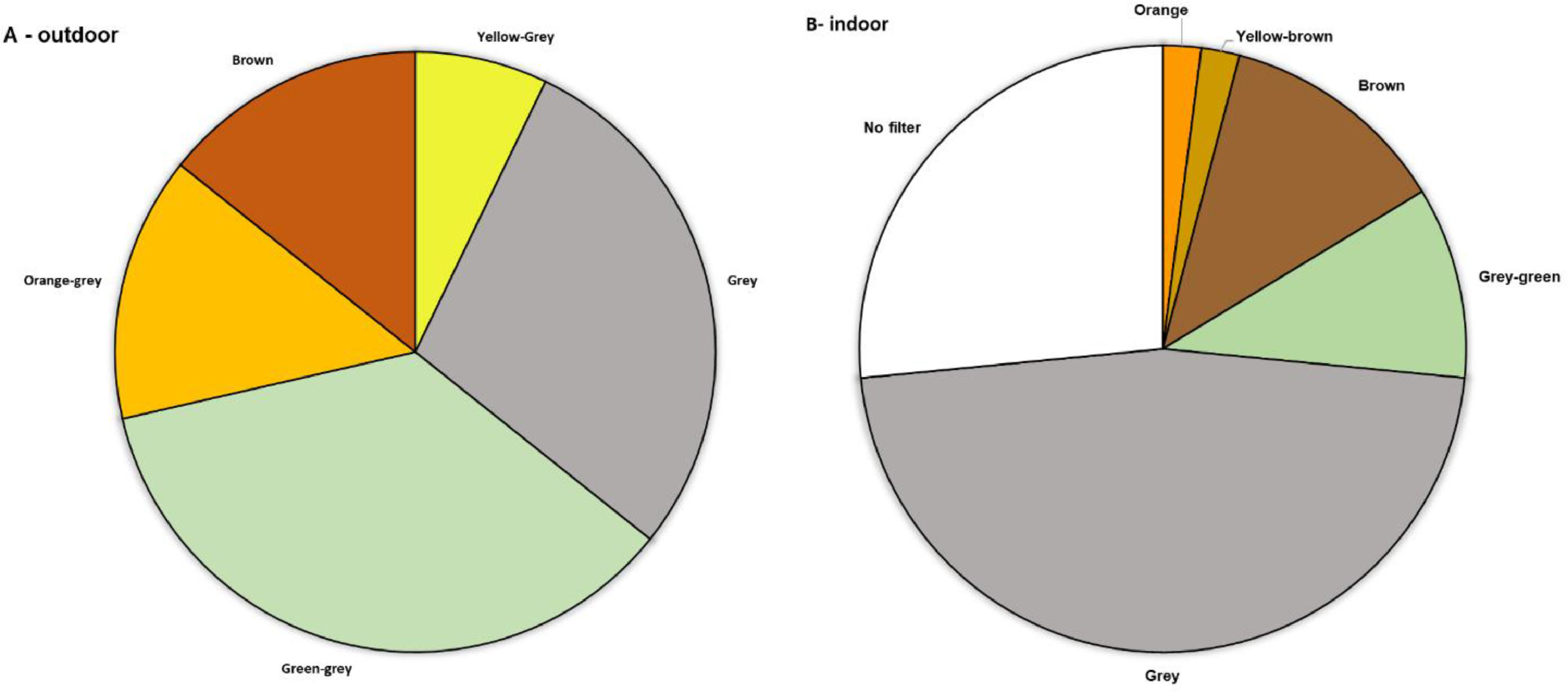
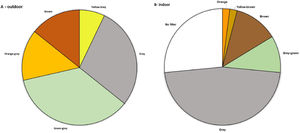
Seventy-four new pairs of spectacles were prescribed as a consequence of the study and 4 participants received a contact lens with a gray filter. Fourteen participants received a new set of spectacles specifically for outdoor use, filter choice of these spectacles can be seen in Fig. 4a and Supplementary Table 1. Forty-nine participants received a new set of spectacles specifically for indoor use, filter choices can be seen in Fig 4b and Supplementary Table 1. The remaining spectacles were prescribed for combination purposes.
DiscussionPhotosensitivity was very common in our cohort of participants and it correlated with the degree of fundus hypopigmentation but not significantly with the degree of iris transillumination. Thus, it seems that fundus pigmentation has a higher impact on photosensitivity in those with albinism than iris translucency. It should, however, be noted that our study population only included a few with a very translucent iris and that the majority had less severe forms of iris transillumination. Previously, iris print contact lenses have been shown to reduce straylight in albinism.9 Surprisingly few participants chose a contact lens in our study even though they were all given the choice.
Photosensitivity was evaluated by simply asking participants how they would rate their photosensitivity from “no or few problems”, “some or moderate problems” to “severe or worst imaginable problems”. More elaborate questionnaires such as the Visual Light Sensitivity Questionnaire10 exists but there is no consensus on which approach provides the best assessment of photosensitivity. Photosensitivity adversely affects quality of life in patients with albinism11 and it is important to alleviate the symptoms of photosensitivity to improve quality of life and quality of functional vision.12 Photosensitivity is a frequent symptom in many different eye diseases and as the underlying conditions affect vision, e.g. visual acuity, contrast and color vision, differently, choice of filter may differ between different pathologies although one review was unable to demonstrate a clear tendency between type of disease and filter choices but all included studies gave participants a very limited number of filter choices.13
Photosensitivity may be alleviated by optical filters. Filters may work by reducing the overall amount of light that reaches the retina or may reduce specific parts of the visible spectrum. Lights of shorter wavelengths are scattered to a higher degree than longer wavelengths. Thus, reducing short wavelengths may be beneficial in reducing photosensitivity from scattered light. In addition, yellow and orange filters are often used to enhance contrast and may be beneficial in low vision patients with poor contrast vision but colored filters may affect color vision.14 Few studies have evaluated the effect and choice of filters in patients with albinism. One study on 42 participants with albinism used a filter with low transmission at all visible wavelengths but more so for shorter wavelengths and concluded that it improved contrast sensitivity but only one type of filter was evaluated.12 In a different study 8 participants with albinism were given the choice of 5 different filters and were reported to prefer amber or dark amber filters.15
In our study, participants were given the choice of a very broad range of filters and filter densities and were allowed to choose differently for indoor and outdoor use. We found that most participants preferred a relatively color neutral filter such as gray or brown or gray and very few preferred a filter with a distinct color such as orange. Color vision is expected to be normal in patients with albinism1 but mild color vision defects have been demonstrated in patients with Hermansky-Pudlak syndrome16 and in patients with tyrosinase-positive albinism.17 Colored filters may be considered beneficial in ocular conditions with a cone dysfunction where the dyschromatopsia induced by colored filters may be less noticeable to the patient whereas dyschromatopsia may disturbing to patients with albinism and normal color vision.
Around ¼ of participants choose an indoor spectacle without filter whereas all new outdoor spectacles contained a filter. Patients with albinism are often withdrawn from society compared to the general population, partly explained by social discrimination caused by their appearance, and they tend to be more emotionally unstable and with less of an assertive personality.18,19 For individuals affected by albinism, the social stigma can be a greater burden than the medical aspects. The request for indoor spectacles without filter can either reflect participants trying not to stand out in social surroundings, that in Denmark are largely indoor, or may reflect that light intensities indoor are not high enough to trigger the photosensitivity. If the choice was caused by social considerations, it was a surprise finding that only 4 participants chose contact lenses.
Prior to the study, the participants had a large number of glasses and as we demonstrated, the request of filter choices differed for indoor and outdoor glasses. In addition, most patients with albinism have low vision and may require special optical solutions for reading and other near work – thus it was rarely possible to find one set of spectacles that fulfilled every need. This emphasizes the need for individual guidance and for a flexible system that allow patients to choose more than one solution.
ConclusionPhotosensitivity was found to be very common in patients with albinism, especially those with fundus hypopigmentation and poor visual acuity, and that neutral filters were preferred to alleviate the complaint and that most participants needed different spectacles for indoor and outdoor with an increased need for filters in outdoor spectacles. As the present study demonstrates, participants with albinism each prefer their own combination of filter color and filter attenuation when given a free choice. Thus, optical rehabilitation of photosensitivity in patients with albinism should be tailored to the individual patient and patients should be given a wide choice of filters to choose the most comfortable solution for each given task at hand.
Conflicts of InterestThe authors have no conflicts of interests to disclose.
The authors are grateful for the participants' engagement in the study. The study did not receive any funding.