The main objective of this study was to obtain percentile curves of refractive errors in a Spanish paediatric population aged between 3 and 12 years.
Materials and methodA descriptive, observational and cross-sectional study was conducted, including children aged between 3 and 12 years who did not present with any known ocular and/or systemic diseases. The convenience sampling method was used to select the sample from three schools and one hospital in the Community of Madrid. The refractive error was obtained using a Retinomax K-plus 3 autorefractometer (RTX; Right Mfg. Co. Ltd., Tokyo, Japan). The 5th, 10th, 25th, 50th, 75th, 90th and 95th percentiles were calculated using the IBM SPSS Statistics v.24 statistical software (IBM Corporation, Armonk, NY, United States).
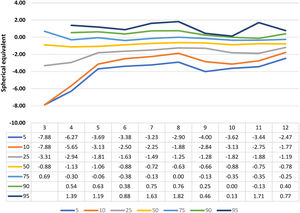
ResultsA total of 688 children with a mean age of 7.68 ± 2.17 years were analysed. In the 50th percentile curve, spherical equivalent values started to become myopic at 3 years (SE < –0.50 D) and the 75th percentile curve also turned myopic at 4 years. As a result, it was observed that the spherical equivalent value became more negative with time, starting from the ages indicated above. Therefore, the 90th percentile curve was negative at 11 years.
ConclusionPercentile curves of refractive errors in a Spanish paediatric population have been presented for the first time in order to help eyecare professionals detect children with refractive errors at an early age.
Emmetropisation is a developmental process in which the cornea and lens dioptric powers are balanced with the axial length, meaning that when the ocular accommodation is relaxed, the remote point is at optical infinity.1,2 As the eyeball grows, the refractive error tends towards emmetropy, a process which occurs more rapidly during the first two years of life.3,4
By measuring refractive error, it is possible to estimate the probability that a child will develop myopia in the future in the case in which they present with hyperopia lower than expected for their age.5 The emmetropization process is divided into two stages: before and after 6 years of age, since important changes occur up to 6 years of age.6 Three processes are observed from 3 months of age to 3.5 years: 1) a change in refraction from +2.00 D to approximately +0.75 D, 2) a decrease in refractive variability, and 3) refractive refractions. more positive than established (4.14). After this stage, around 6 years of age, hyperopia persists, in which the emmetropization process is almost complete.7 After 6 years of age, it is about to culminate, but it is still sensitive to factors that can lead to a refractive error, be it farsightedness, myopia or astigmatism; it is considered that this process ends at 7 years of age.7,8 On another note, early detection and adequate treatment of refractive errors could prevent amblyopia or the onset of strabismus.9-11
Traditionally the method used for identifying refractive errors in infants was cycloplegic and non-cycloplegic retinoscopy. This is a technique that requires extensive training and it is usually performed by experienced eyecare professionals.12 In recent years, different techniques and tools have been developed for detecting refractive errors which require minimal cooperation from the child. Autorefractometers are widely used amongst vision professionals because they allow them to perform a rapid and easy assessment.13 Handheld autorefractometers are particularly helpful when assessing refractive errors in children, babies and adults who are unable to lean on table-mounted devices, given that it is possible for measurements to be taken while the patient is in a supine position. Nonetheless, to date, very few studies have actually analysed the precision of these instruments.13
Percentile curves are used as a tool for assessing children's development and wellbeing.14 The study conducted by Chen et al.15 introduced the use of reference curves for refraction as a means of identifying children who were at high risk of myopia, in order to be able to advise parents on ways in which their children's lifestyles could be improved to lower this risk.
Nonetheless, percentile curves for refraction are specific to each population.16,17 Truckenbrod et al.18 analysed percentile curves in central Europe. Thus, they obtained that for all ethnic groups, a trend towards myopia with increasing age could be observed, but the progression of myopia is much greater in China and Korea than in Germany. The study carried out by Chen et al.15 in Guangzhou (China), concluded that further research must be conducted in order to generate percentile curves for refraction.
Therefore, the purpose of this study was to determine the percentile curves of refractive errors in a Spanish paediatric population aged between 3 and 12 years of age.
Materials and methodType of studyA descriptive, observational and cross-sectional study was conducted which included children who did not present with any known systemic and/or ocular diseases. The parents of all the participants signed the informed consent form, declaring that they had fully understood the study objectives. The study subjects were included during the third school quarter of the 2016–2017 academic years and the first quarter of 2017–2018. This research was conducted in accordance with the principles of the Declaration of Helsinki and it was approved by the Ethics Committee of the European University of Madrid.
SampleThe sample was selected by means of a convenience sampling in three schools (Carmelo Teresiano School in Madrid, Dulce Chacón Public School in Fuenlabrada and Hermanos Torá Public School in Humanes) and one hospital (Rey Juan Carlos University Hospital of Mostoles); all of which were located in the Community of Madrid. The same inclusion criteria as used in the studies conducted by Navas-Navia et al.19,20 were followed with regards to visual acuity and stereopsis. As a result, the participants who were recruited from the school setting were children from pre-school through to sixth grade, and the participants who were recruited from the hospital were children who were attending their first ever routine ophthalmologic examination with no history of any ocular pathologies. A total of 688 children, of which 50.7% of which were male were analysed according to the frequency of the Spanish census population. The participants were aged between 3 and 12 years, and the mean age was 7.68±2.17 (3 years: 7: 4 years: 50; 5 years: 59; 6 years: 79; 7 years: 140; 8 years: 127; 9 years: 86; 10 years; 61; 11 years: 37; 12 years: 42). The children of the hospital facilities included in the study were those who attended a new first routine ophthalmology examination and who did not show any obvious eye pathology or symptoms of refractive errors. Children who presented with any systemic or eye pathologies were excluded from the study. Information regarding the existence of pathology was provided by the parents or guardians during the anamnesis that was performed previously.
Materials and procedureNon-cycloplegic refraction records were obtained using a Retinomax K-plus 3 autorefractometer (RTX; Right Mfg. Co. Ltd., Tokyo, Japan). This device has a repeatability of 0.902. This indicates that it presents a high concordance.21 Agreement and repeatability were demonstrated in various studies where their results were compared with other portable autorefractometers, retinoscopy and refraction under cycloplegia and without cycloplegia.21-26
Retinomax K-plus 3 is a wireless and portable device with a charging station. If no measurements are taken in six seconds, the unit automatically enters “quick mode” and a measurement is taken in 0.07 s.
To conduct a proper reading, both the instrument and the patient must be held in a stationary position and the patient must blink little or not at all during the test. The patients were shown a coloured image of a field with a Christmas tree in the middle. The tree appeared to be far away and initially it was blurry. When the instrument moved towards the eye, the image became much clearer to the patient and when the reading commenced, a faint beep was heard. After eight proper readings, the other eye was tested. The spherical range varied from –18 to +22 dioptres (D) increasing 0.25 D each time; and the cylinder range was 12 D.
Statistical analysisDescriptive statistical data and boxplot diagrams were obtained for the total sample, as well as for the 5th, 10th, 25th, 50th, 75th, 90th and 95th percentiles. To compare the results of the left and right eyes, JASP v.0.13.1 software (Jasp Team, Amsterdam University, Amsterdam, the Netherlands) was used to assess data normality. Likewise, a non-parametric or parametric test was conducted, depending on the results attained. All of the analysis was carried out with a significance level of 5% (p < 0.05), using the IBM SPSS Statistics v.24 software (IBM Corporation, Armonk, NY, United States).
ResultsSampleTable 1 shows the descriptive analysis of the refractive values and spherical equivalent obtained using the Retinomax K-plus 3 autorefractometer.
Descriptive analysis of refractive errors.
SE: spherical equivalent; RE: right eye; LE: left eye; BE: both eyes.
The Kolmogorov-Smirnov test rejected the normality of the data; as a result, the Wilcoxon signed-rank test was used for the comparison of means. No significant differences were found in either the sphere (Z = –0.476; p = 0.634) or cylinder (Z = –0.855; p = 0.393), nor in the RE and LE spherical equivalent (Z = –0.282; p = 0.778). In terms of age, no statistically significant differences were recorded between RE and LE for any age between 3 and 12 years (p > 0.05).
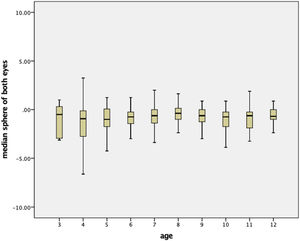
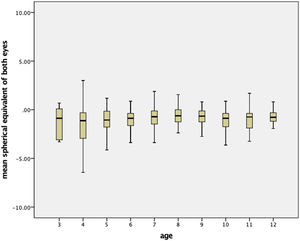
Percentile curvesFigs. 1 and 2 show the boxplot diagram of the mean spherical value and the mean spherical equivalent, respectively, by age for the total sample. No differences were found between RE and LE and, as a result, the mean value of both eyes was specified.
Figs. 3 and 4 show the curves for the mean spherical value and the mean spherical equivalent, respectively; alongside their mean numerical values for the 5th, 10th, 25th, 50th, 75th, 90th and 95th percentiles by age.
The main findings of this study were that as the years increase, the spherical equivalent becomes more negative. In turn, as age increases, the values of the spherical equivalent in each percentile are closer. In recent decades there has been an unprecedented increase in the prevalence of myopia in practically the entire world, but with very significant regional differences, its frequency being much higher in East and Southeast Asia, followed by Europe. In Latin America, with the exception of Mexico, and in Africa, the rates of myopia have been reported in lower values. Amongst the factors that have triggered this epidemic, both hereditary and environmental have been identified, with the latter apparently having a greater impact.27-31
Retinomax is a handheld autorefractometer which enables a rapid estimation of the refractive state. Since its introduction in 1995, this device has been widely used, specifically to assess children's refractive states, both in a practical setting and for the purpose of research. Thanks to characteristics such as its portability and good sensitivity and specificity (0.90 and 0.94 respectively, in children ranging between 36 and 72 months), it is considered a useful device for attaining definitive measurements of the refractive error in cycloplegic conditions, particularly, in research studies. Likewise, it is useful for detecting high refractive errors in young children in non-cycloplegic conditions.24,32,33 In terms of cycloplegia, Retinomax has been used to compare and measure the refractive error in epidemiological studies considering ocular diseases in paediatric populations.34,35 Therefore, previous visual screening studies have shown it to be a useful tool for the diagnosis of refractive errors.24,36 A study conducted by Tuncer et al.12 compared the use of Retinomax under cycloplegic conditions to the use of a retinoscopy in 127 patients with a mean age of 96.7 months, and no significant differences were found between the two devices in terms of the sphere, cylinder and spherical equivalent. This therefore highlights the fact that Retinomax can be used successfully as a screening tool. A similar study conducted by Ying et al.37 compared the non-cycloplegic retinoscopy to Retinomax and to SureSight Vision Screener (Welch Allyn Medical Products, Skaneateles Falls, NY) under cycloplegic conditions in pre-school children. All of the devices offered a similarly high accuracy for detecting visual impairments in all types of assessments.
When undertaking exams with Retinomax under non-cycloplegic conditions, Liang et al.38 found that the values were 0.59 D more negative than those attained when using cycloplegia in the sphere. However, no differences were found in the cylinder and in the axis. In addition to the sphere data obtained under non-cycloplegic conditions, in general, 90% of the differences of the sphere and cylinder were within 0.5 D, and more than 97% of the differences in the low axis under cycloplegic conditions, and 68% of those under no-cycloplegic conditions were within 20°. These results were in line with those obtained in the studies by Tuncer et al.12 and Truckenbrod et al.,18 in which the difference between the values obtained under cycloplegic and non-cycloplegic conditions was –0.80 D and –0.75 D, respectively. As a result, the reviewed literature confirmed that Retinomax can be successfully employed as a detection tool, nonetheless, it may not provide the accuracy required for prescribing glasses.
Data about percentile curves in children was first presented in a RESC (Refractive Error Study in Children) study, which was conducted in the city of Guangzhou in China.15 In this study performed in China, unlike in this study, percentile curves were reported by gender and age, and only the 3rd, 50th and 97th percentiles were obtained. Nonetheless, when comparing results, Spain shows a more myopic environment in children between 5 and 9 years; and it is important to note the difference between the results for the 3rd percentile obtained in China and those of the 5th percentile obtained in Spain at 5 years. Likewise, in China, the 3rd percentile for girls and boys was –0.25; and in Spain, the 5th percentile was –3.69. In contrast, this situation evolves from 10 years, with China becoming a more negative environment.
This may be due to the fact that in China the preschool stage starts at 5 years, whereas in Spain it commences at 3 years. Likewise, in China, the school timetable for children within that age group is from 7:30 a.m. to 4:00 p.m., and children have more homework and spend more hours performing near-vision activities.39 This directly relates to the idea that the more hours spent undertaking near-vision activities, the higher the risk of developing myopia.40,41
Subsequently, a study conducted in Korea in 2018, with children aged 5 years, reported +0.72 D and +0.04 D values for the 10th and 50th percentile, respectively.42 Despite the fact that the spherical equivalent was more negative amongst Spanish children, the spherical equivalent values were more similar. This confirms the upward trend in terms of the prevalence of myopia in children in recent years.
In Europe, only one study on percentile curves of refractive errors has been published, and this study was conducted in Germany in 2020.18 This study followed the same methodology as used in the one conducted by Chen et al.15 Our results once again showed a more myopic environment until 10 years. As previously mentioned, this difference might be related to the year in which the sample was collected, and whether it was prior to the lockdown provoked by the pandemic. Nonetheless, the prevalence of myopia in German children was lower than it was in Spanish children, with a prevalence of 20.1% amongst Spanish children aged between 5 and 7 years43 and of 13.3% amongst German children aged between 3 and 17 years.17
One of the main strengths of this study was that the normative values presented are the only ones that have been recorded in Spain. On the other hand, the main limitation of this study was that convenience sampling was used, which explains why these results are not directly translatable to the entire population; additionally, these curves can be understood as indicative. This aspect must be considered in future studies. In turn, it should be considered that the instrument used (Retinomax) is more precise when used under cycloplegic conditions, and in this study the refraction was performed without cycloplegic. It should also be emphasized that the sample all comes from hospitals in the Community of Madrid, so it would also be interesting to carry it out in other autonomous communities.
ConclusionsA percentile curve was presented for the first time in a Spanish paediatric population. By comparing this study with similar studies conducted in Asia and Germany, it is evident that there are more cases of myopia in Spain. Nonetheless, as in the other studies, the myopia progression rate increases with age.
The percentile curves obtained in this study show the distribution of the refractive error by age, clearly showing that the prevalence of myopia is gradually increasing. These curves may serve as the basis for detecting children with refractive impairments at an early age.
This research was funded by the project CAT0001305 of Cátedra Fundación Salud Visual - European University of Madrid.