To determine the fixation disparity and refractive error of first-year optometry students to ascertain any relationship between them and also identify any association between fixation disparity and visual symptoms at near.
MethodIt was an analytical cross-sectional study involving 85 participants aged 17 to 27 years (18.60 ± 1.37), 41% of whom were males. Subjective refraction was done at 3 m and fixation disparity was measured with and without spectacle correction using the Wesson Fixation Disparity Card. All analysis was set within a 95% confidence interval with a p-value ≤ 0.05 considered statistically significant.
ResultsRefractive error ranged from 0.25 SEQ (spherical equivalent) to 5.50 SEQ. Mean fixation disparity ranged from 2.9 ± 2.6 to 3.9 ± 2.8 min arc. There was no statistically significant correlation between refractive error and fixation disparity without correction (r = −0.180, p = 0.098) and with correction (r = 0.155, p = 0.157). For fixation disparity in the ortho and exo direction, mean fixation disparity with correction of participants who experienced headaches during or after reading (5.1 ± 2.6 min arc) was significantly higher (p = 0.032) than participants who did not (2.0 ± 2.6 min arc).
ConclusionMyopia is common among first-year optometry students. Refractive error has no significant effect on fixation disparity. Headache is significantly associated with exo fixation disparity at near.
During binocular fixation, each point on the retina of one eye corresponds to a point or area (Panum's area) on the retina of the other eye, and this point-to-point or point-to-area correspondence of the eyes allows images focused on the retina during binocular fixation to be fused into one single image.1 If the visual axes of both eyes are not properly aligned to the point of fixation during binocular vision, the point to point or point to area correspondence does not occur and images formed on the retina of each eye cannot be fused into a single image. Thus, two images are still perceived, a phenomenon known as diplopia.1 However, Panum's area makes room for some degree of imprecision in fixation during binocular vision without the occurrence of diplopia.2 It permits slight deviation of the eye from the point of fixation without diplopia, that is, the visual axes do not fall on corresponding retinal points but fall within corresponding Panum's areas; this small deviation from the point of fixation without diplopia is known as fixation disparity and is measured in minutes of arc (min arc).3 Associated phoria is a term used in close relation to fixation disparity. However, unlike actual fixation disparity, it is the amount of sphere or prism power that eliminates fixation disparity.4,5
The refractive status of the eye refers to the locus within the eye conjugate with optical infinity during minimal accommodation.6 Refractive status includes emmetropia or ametropia. Parallel rays of light focus sharply on the retina in emmetropia but focus at a point in the eye other than the retina in ametropia. Ametropia, also known as refractive error, may be myopia, hyperopia or astigmatism. In the myopic eye, with accommodation relaxed, the eye's refractive power is greater than needed for its axial length, thus, parallel rays of light are brought into focus in front of the retina. The hyperopic eye, on the other hand, has insufficient refractive power for its axial length and thus, with accommodation relaxed, parallel rays of light focus behind the retina. In astigmatism, the eye's refractive components are unable to form a point image for a point object at infinity.
Refractive error is the second leading cause of moderate to severe distance visual impairment.7 Unfortunately, studies show a high prevalence of refractive error among university students and optometry students.8–11 Hebbard showed an increase in fixation disparity in the horizontal meridian with increasing units of induced blur equivalent to +1 and +2 diopter sphere lenses in four subjects.12 This suggests that fixation disparity may be increased in the presence of uncorrected refractive error which also causes blur at distance or near. Nilsson et al., however, showed that monocular astigmatic blur up to 1.25 diopters had no significant effect on fixation disparity in the horizontal meridian and indicated that the focusing system of the eye requires more stress before any significant changes in fixation disparity.13 Spherical lenses known as aligning spheres have also been used in some instances to eliminate eso and exo fixation disparity and thus indicating a possible association between refractive errors and fixation disparity.4,5 In a study to measure distant and near readings of associated phoria, Pickwell found that 55% of people who experienced symptoms such as headaches, diplopia, blurred vision, eye strain and eye pain during near work had associated phoria in the exo direction.14 Yekta et al. also measured fixation disparity before and after the day's near work in young adults and found that increase in exo fixation disparity at the end of the day's near work was related with visual symptoms.15 These studies indicate that exo fixation disparity is associated with asthenopic symptoms.
University students have higher academic demands and are involved in a lot of near work; mainly reading. First-year students are usually engaged in four to six years of academic work and require single, clear, and comfortable vision for such work. For students, an increase in the amount of near work which occurs, especially weeks or days to examination, can cause stress on the visual system.16 This is confirmed in a study where ocular symptoms and associated phoria increased among students after examination alongside deterioration of other binocular vision functions.17 Another study reports that 10% of a random university student population complains of headaches associated with studying.18 Although studies have been conducted on the prevalence of refractive error among university students, to the best knowledge of the author, no study has been conducted to determine the presence or effect of fixation disparity on university students. The study, therefore, sought to determine the fixation disparity and refractive error of first-year optometry students to ascertain any relationship and also identify any association between fixation disparity and asthenopic symptoms in students during near work. This will enable clinicians to ascertain the role of fixation disparity in asthenopic symptoms at near, especially among students, and the effects of refractive error on fixation disparity.
Materials and methodsStudy designIt was an analytical cross-sectional study conducted at the Department of Optometry and Visual Science of the Kwame Nkrumah University of Science and Technology (KNUST), Ghana. Data was collected at the Optometry Clinic, at the College of Science building, KNUST from February to March 2020.
Data collectionThe study was conducted with adherence to the Declaration of Helsinki and received ethical approval from the Committee on Human Research, Publication, and Ethics of the School of Medical Sciences, KNUST. Written informed consent was obtained from the participants and every procedure was carefully explained to them during the examinations.
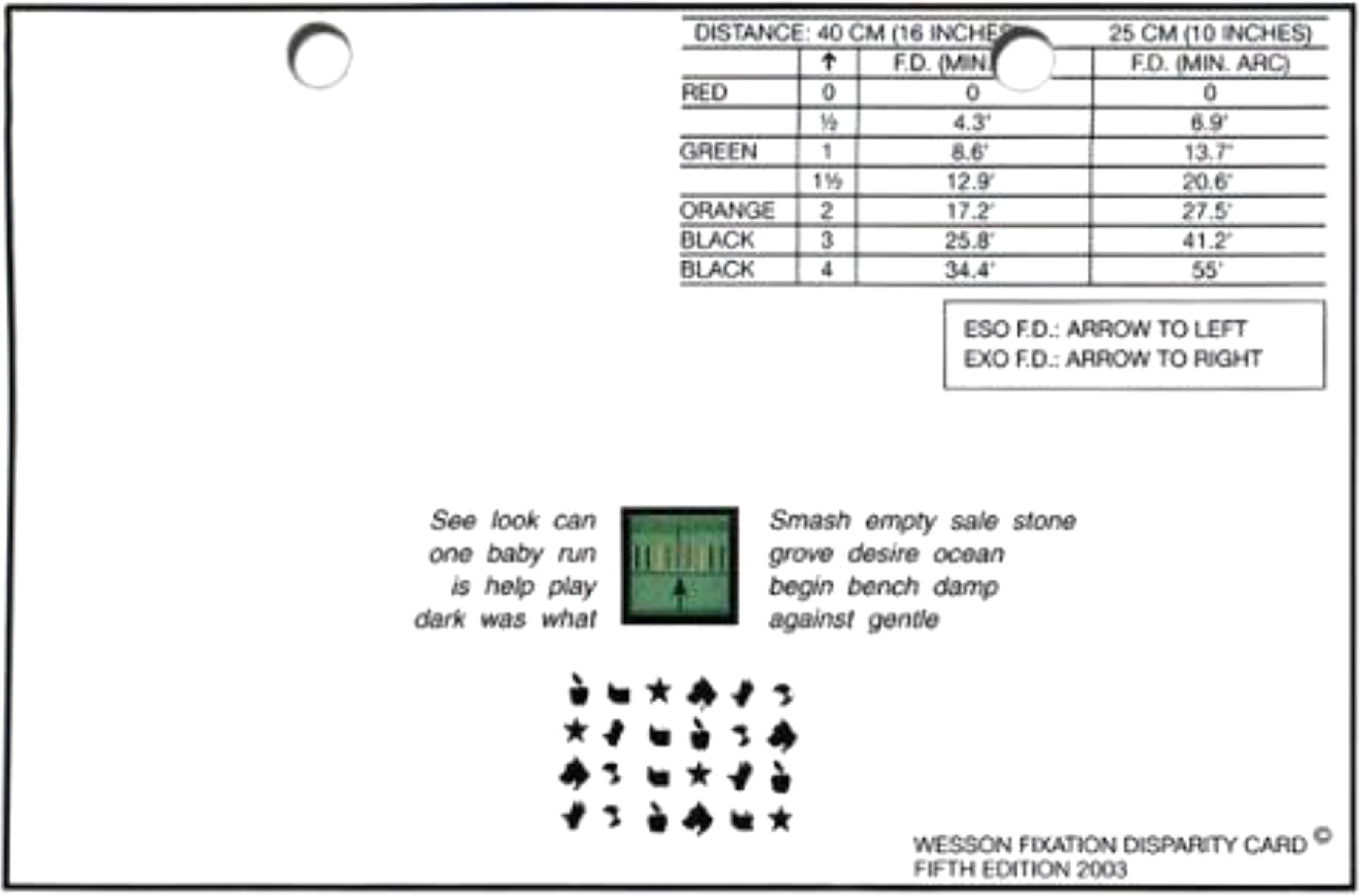
Participants with normal binocular vision were included in the study and those with strabismus and/or amblyopia were excluded. Cover test and refraction was done among participants to rule out strabismus and amblyopia, respectively. Participants indicated if they wore spectacles, experienced symptoms of headache or eyestrain during or after reading, and also recorded the hours they spent reading in a day. The reading distance, subjective refraction, and fixation disparity of participants were also measured. They read a text (font size 12) with their habitual spectacle prescription, and the distance from the eye or spectacle plane to the reading material was measured as their usual reading distance. Subjective refraction was performed using a Snellen 3-meters chart, trial lenses, and a trial frame at three meters. Fogging technique (with a + 3.00 DS lens) was employed during subjective refraction to control accommodation. Astigmatic errors were converted to their spherical equivalent (SEQ). Emmetropes were defined as participants with no refractive error (0.00 DS) and ametropes were defined as participants with refractive error greater than or equal to ±0.25 SEQ. The higher refractive error among the two eyes of each participant was used for analysis. Fixation disparity was measured at 25 cm in a well-illuminated room using a Wesson fixation disparity card (Fig. 1) and a polarizer. During fixation disparity measurement, the participants closed each eye and reported what the other open eye sees to ensure that one eye sees only the colored lines and the other eye sees only the black arrow on the card as they wore the polarizer. They read the words around the arrow and the colored lines to ensure fusion lock. As they read the words, they were interrupted and asked to report the position of the black arrow relative to the colored lines. This indicated the amount and direction of fixation disparity in minutes of arc as read from a chart on the card. Fixation disparity measurements were taken three times and the average used for analysis. Fixation disparity was measured with and without spectacle correction in ametropes.
Statistical analysesData was analyzed using the Statistical Package for the Social Sciences (SPSS) Version 25. Descriptive data was analyzed using percentages, means and standard deviations. Fixation disparity variables were positively skewed thus a logarithmic transformation was performed on variables and back-transformed after analyses. All analysis was set within 95% confidence interval with a p-value ≤ 0.05 considered statistically significant. Spearman's correlation was used to establish relationships between non-parametric fixation disparity and refractive error variables at two-tailed levels of significance.
ResultsParticipantsEighty-five (69.7%) out of 112 first-year optometry students aged 17 to 27 years (18.60 ± 1.37, mean ± SD) participated in the study, including 35 (41.2%) males and 50 (58.8%) females. All participants had normal binocular vision. Twenty-eight (32.9%) of the participants reported that they experienced headaches during or after reading and close to a third, 26 (30.6%), also reported that they experience eye strain during or after reading whiles wearing their usual spectacle prescription. The usual reading distance among the participants ranged from 19 to 59 cm with a mean reading distance of 42.09 ± 7.88 cm. The participants spent an average of 7.6 ± 2.9 h reading in a day.
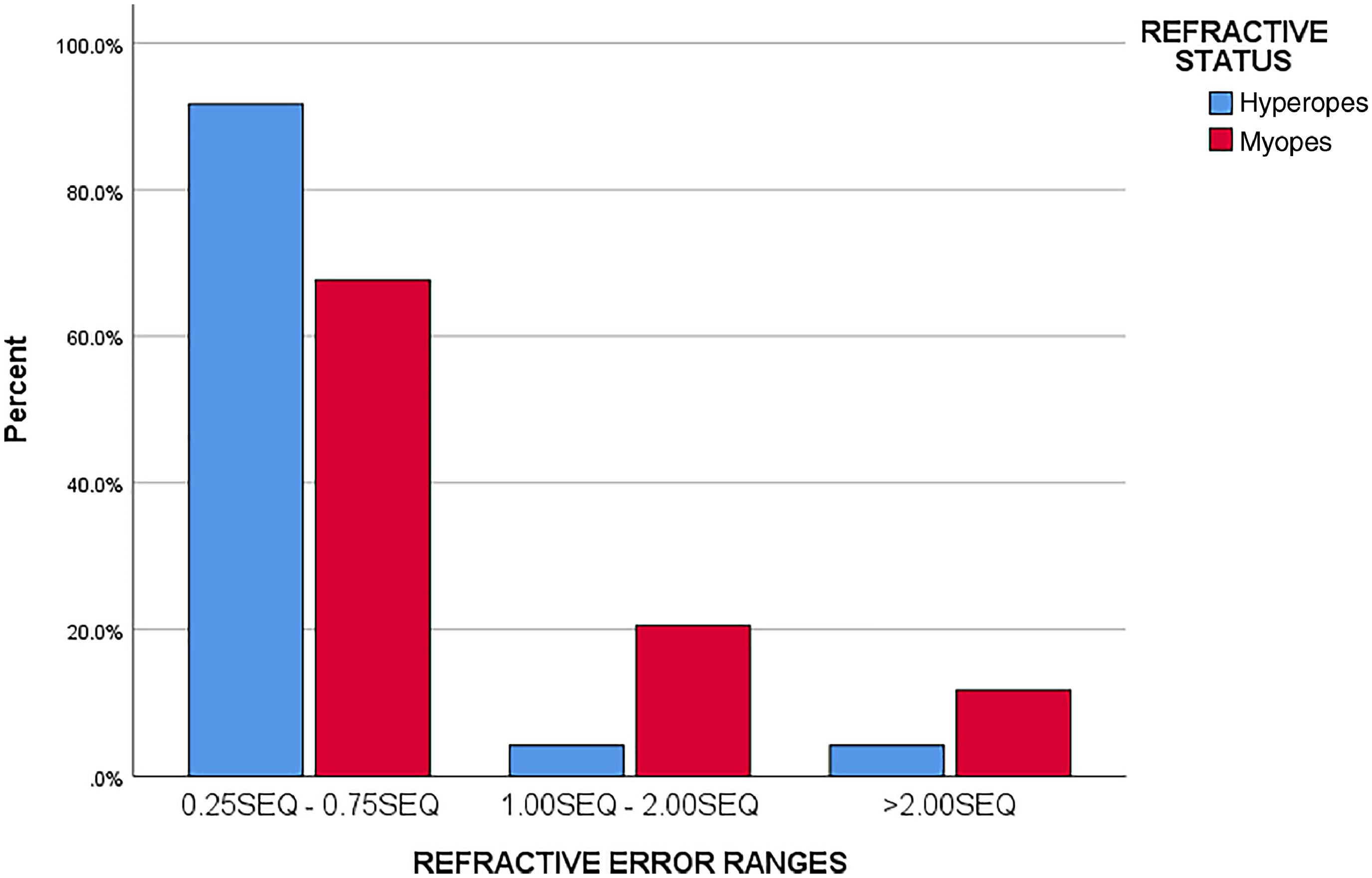
Refractive error of first-year optometry studentsThere were 27 (31.8%) emmetropes, 34 (40.0%) myopes and 24 (28.2%) hyperopes. The refractive error of myopes ranged from - 0.25 SEQ to −5.50 SEQ, with a median of −0.50 SEQ, whereas that of hyperopes ranged from +0.25 SEQ to +5.00 SEQ, with a median of +0.50 SEQ. Astigmatic errors ranged from −0.25DC to −1.00DC. Forty-five participants (52.9%) had refractive error of ± 0.75 SEQ or less and five participants (5.9%) had refractive error greater than ±2.00 SEQ. Fig. 2 shows the distribution and magnitude of refractive error among participants.
Out of 58 participants with ametropia, 36 (62.1%) had no spectacle correction. These included 16 (44.4%) myopes and 20 (55.6%) hyperopes.
Fixation disparity among first-year optometry studentsTable 1 shows the amount and direction of fixation disparity of participants. Fixation disparity ranged from 0 to 41.2 min arc among ametropes and 0 to 13.7 min arc among emmetropes. Mean fixation disparity was 3.5 ± 2.3 min arc in emmetropes, 3.9 ± 2.8 min arc in myopes, and 3.9 ± 2.8 min arc in hyperopes when tested without spectacle correction and reduced to 2.9 ± 2.6 min arc and 2.9 ± 2.8 min arc in myopes and hyperopes, respectively, when tested with spectacle correction.
Amount and Direction of fixation disparity of participants.
There was a reduction in mean fixation disparity of myopes from 3.9 ± 2.8 min arc when tested without spectacle correction to 2.9 ± 2.6 min arc when tested with spectacle correction. This reduction, however, was not statistically significant (p = 0.497). There was also a reduction in mean fixation disparity of hyperopes from 3.9 ± 2.8 min arc when tested without spectacle correction to 2.9 ± 2.9 min arc when tested with spectacle correction, but this was also not statistically significant (p = 0.566). Differences in mean fixation disparity between emmetropes and myopes (p = 0.809) and emmetropes and hyperopes (p = 0.848) when tested without spectacle correction was not significant. There was no statistically significant correlation between refractive error and fixation disparity without spectacle correction (r = 0.025, p = 0.822) and with spectacle correction (r = 0.030, p = 0.787).
The number of myopes with fixation disparity in the exo-direction reduced by 20.6% when tested over spectacle correction., and the number of hyperopes with fixation disparity in the exo-direction increased by 4.1% when tested over spectacle correction. There was also a 14.7% increase in the number of myopes and a 12.5% decrease in the number of hyperopes with fixation disparity in the eso-direction when tested over spectacle correction. (Table 1)
Effects of fixation disparity on studentsFor fixation disparity in the ortho and exo direction, mean fixation disparity with correction of participants who experienced headaches during or after reading (5.1 ± 2.6 min arc) was significantly higher (p = 0.032) than participants who did not experience headaches during or after reading (2.0 ± 2.6 min arc). Difference between mean fixation disparity with correction of participants who experienced eye strain during or after reading (3.3 ± 2.4 min arc) and those who did not (2.6 ± 2.9 min arc) was, however, not statistically significant (p = 0.577). For fixation disparity in the ortho and eso direction, mean fixation disparity with correction showed no statistically significant difference (p = 0.077) between participants who experienced headaches during or after reading (1.3 ± 2.1 min arc) and participants who did not (0.3 ± 1.1 min arc). There was also no statistically significant difference (p = 0.507) between participants who experienced eyestrain during or after reading (0.8 ± 1.8 min arc) and those who did not (0.4 ± 1.3 min arc).
DiscussionSeveral studies have found similar results on refractive error among optometry students. Goss et al. found 65.3% myopes, 30.1% emmetropes and 4.5% hyperopes among a first-year optometry class at Northeastern State University, USA.10 Septon (1984) in a study among 447 second-year optometry students at Pacific University also found 74.3% myopes, 17% emmetropes and 8.7% hyperopes.19 Similarly, Bullimore et al. found 55.6% myopes and 6.3% hyperopes among 189 Aston University optometric undergraduates.20 All these studies had myopia as the highest prevalence and hyperopia the least prevalence among optometry students. However, in a study conducted by Darko-Takyi et al. among optometry students in Ghana, 17.1% had myopia, 19.0% had hyperopia, and 22.9% had astigmatism showing myopia as the least present condition.11 Unlike the present study, Darko-Takyi et al. did not convert astigmatic errors into spherical equivalents and thus may be the cause for the variation in results.
Majority of participants with refractive error had no spectacle correction. A cohort study by Megbelayin among medical students revealed similar findings.21 Although there was a high prevalence of ametropia (79.5%), 90.4% of ametropes were not wearing glasses at the time of the study, and 80.7% had never worn glasses. In another study on school children, 30.29% had refractive error with the commonest type being myopia (22.6%).22 However, only 4 (6.3%) of these ametropes wore spectacle correction.
Fixation disparity measurements were predominantly in the exo-direction among all the refractive status of participants (and when tested with and without spectacle correction in ametropes). This is not surprising as subjective fixation disparity at near tends to be larger in the exo-direction and suggests that the eyes are under-converging.15,2324 Other studies have reported similar mean fixation disparity among participants, with fixation disparity being largely in the exo direction. Jaschinski reported in a study that mean fixation disparity increased from 0 to 3.5 min arc exo as the distance between the eyes and visual display unit was shortened from 85 cm to 25 cm.25 He further reported a change in mean fixation disparity from 1 min arc (eso) to 3 min arc (exo) as the viewing distance was reduced from 100 cm to 20 cm.26 In a more recent study, Jaschinski found mean subjective fixation disparity to be in the exo-direction and reported that it increases in the exo-direction as the viewing distance is further shortened.27
No significant relationship was found between fixation disparity and refractive error. These findings, which may be attributed to the low refractive error (0.25 SEQ–0.75 SEQ) found in most (52.9%) study participants, support claims of researchers that spectacles do not aid in the compensation of phorias and as such do not improve binocular function,28 even though Dywer and Wick argue otherwise and suggest that the correction of even minute refractive errors eliminates slight blur, and improves binocularity.29 They also support the claim of Nilsson that the focusing system of the eye requires more stress before any significant changes in fixation disparity.13 Again, the findings suggest that the spherical equivalent lens power that corrects refractive error may not necessarily eliminate or reduce fixation disparity.
The 20.6% decrease in exo-direction of fixation disparity and 14.7% increase in eso-direction for myopes when tested over spectacle correction can be explained by the accommodation-convergence relationship of the eyes associated with lenses. Minus lenses are known to stimulate accommodation which in turn stimulates convergence based on this relationship. As such, exo-deviation is expected to reduce and eso-deviation is expected to increase when minus lenses are introduced to correct myopia. This same phenomenon can be used to explain the 4.1% increase in exo fixation disparity and 12.5% decrease in eso fixation disparity for hyperopes when tested over spectacle correction. Hyperopes are corrected with plus lenses which relaxes accommodation and causes divergence of the eyes, thus the increase in exo-deviation and decrease in eso-deviation.
Headache was found to be associated with exo fixation disparity in the present study. This is expected as a study found a slightly higher than usual associated phoria in individuals suffering from migraine.30 Participants with more exo fixation disparity at near in a study by Jaschinski also had more near vision fatigue and preferred longer viewing distance.31 In a more recent study, Jaschinski again reported that individuals with stronger complaints of asthenopia tend to have larger exo subjective fixation disparity in near vision (40 cm) but not in distance vision (5 m).27 Yekta also found the magnitude of fixation disparity and associated phoria for near vision to be associated with symptoms.32 These studies confirm the association of fixation disparity and asthenopic symptoms such as headaches as found in the present study. Admittedly, refractive error can be a confounding factor in the association between fixation disparity and asthenopic symptoms.33,34 However, considering the low median refractive error among participants (±0.50 SEQ), it is highly unlikely for it to cause such symptoms at near.
Refractive error and its correction may not have significant effect on fixation disparity. However, fixation disparity may be associated with symptoms among students during near work and thus fixation disparity tests should be adopted as a routine clinical exam for students. Studies should be conducted to ascertain possible reasons for uncorrected refractive errors among first year students and also determine the most effective means to eliminate or reduce fixation disparity.
The study unlike other studies measured fixation disparity with and without spectacle correction in ametropes to highlight the effect of spectacle correction on fixation disparity. The study also made use of the Wesson fixation disparity card; a simple tool that can be adopted in routine optometric exams to test for fixation disparity. However, as a limitation, it was unable to capture a fair distribution and wider range of refractive errors among participants.
ConclusionThe study shows that majority of first-year optometry students are myopes, and a high percentage of ametropes among them are uncorrected. Mean fixation disparity among students ranged from 2.9 to 3.9 min arc. Refractive error and spectacle correction was found to have no significant effect on fixation disparity. However, headache was found to be associated with exo fixation disparity at near.
It is recommended that measures be adopted to promote spectacle correction among students. Also, routine clinical examinations among students should include fixation disparity tests to detect and reduce or eliminate fixation disparity and prevent associated headaches during near work.
DisclosureThis research did not receive any grant from funding agencies in the public, commercial, or not-for-profit sectors.