The United Kingdom (UK) National Health Service (NHS) currently provides sight tests at no cost to patients for all those aged <16 or ≥60. Some ‘at-risk’ patients and those in receipt of means-tested benefits are eligible for a NHS sight test between the ages of 16 and 60. In the UK, community optometrists typically either work in independent or national chain practices (multiples). The present study aims to explore whether practice type has any association with sight test outcome. As sight tests are essential in detecting early childhood visual problems, we also aim to explore children's first sight tests.
MethodData from 664,480 NHS sight test claims submitted in Essex from April 2015 to September 2016 were analysed using regression analysis. Practice type (multiple, independent) and children's first sight test were examined with respect to socio-economic status (SES, based on index of multiple deprivation rankings), age and sight test outcome.
ResultsThe median age for a first NHS sight test was 6 years old and was clinically independent of SES. Children's first sight tests typically resulted in neither a spectacle prescription being issued nor an onwards referral. Patients that attend multiples are significantly more likely to receive a new prescription, relative to no prescription, compared to a patient attending an independent (p<.001).
ConclusionsInequalities in sight test outcome appear to exist with differing type of practice (independent or multiple). Choice of practice type appears to be influenced by SES. Children have their first sight test at a later age than recommended.
Primary eye care in the UK is typically carried out by optometrists. This is generally in the form of a ‘sight test’ defined by the Opticians Act, which results in a prescription for refractive correction being issued (if required) and an ocular health check being performed.1 This is funded, either by the patient (i.e. private), or by the National Health Service (NHS) under the terms of the General Ophthalmic Services (GOS) contract.2 The sight test includes a refraction and basic ocular health check to determine whether or not the patient is required to be referred to an ophthalmologist or general practitioner. Accordingly, the outcome of a NHS sight test can be the issuing of: a new (or changed prescription), an unchanged prescription, a statement that no prescription is required or a referral to another health care professional. GOS in England provides sight tests for anyone under the age of 16 or above 60 at no cost to the patient usually every two years.3 Similarly, small groups of ‘at risk’ patients, students aged 16–18, and those in receipt of state-funded means tested benefits are eligible for an NHS funded sight test.4 A patient is free to change between optometry practices each visit, however, a practice may send a patient a reminder letter when they are due a routine sight test.
The National Screening Committee, a group that advises the UK government and NHS about population screening, recommends that all children should receive a sight check between the ages of 4 and 5 by orthoptic assessment, usually within schools.5 This is not as comprehensive as a sight test as it does not contain a check of ocular health. Unfortunately, this screening is only a recommendation and commissioning of school screening varies depending on the local authority. It has been reported that only 55% of local authorities commission this service and where this is not performed a NHS sight test is indicated.6 The age of children's first eye test, therefore, is an important metric to consider. The aim of testing children's eyesight is to detect common ocular abnormalities such as uncorrected refractive error or amblyopia (‘lazy eye’) that may hinder the child's progression either socially, or academically.7,8 As treatment aimed at correcting amblyopia is typically more successful when conducted before the age of 7,9,10 the earlier a child has his/her sight tested, the greater the probability that the condition will be detected, and managed effectively.
In the UK, there are national chain opticians (‘multiples’) that have numerous practices distributed across the country, and ‘independent’ opticians that have either one, or a small number of practices across a region. Previous research has reported that independents typically charge more for a private sight test and spent longer performing the eye test, relative to multiples.11 Shah and colleagues also reported that multiples delegated more tasks to auxiliary staff (e.g. trained optical assistants or dispensing opticians) and, moreover, patients felt independent opticians addressed their presenting symptom significantly better than multiples. These findings suggest that optometrists working in different practices may perform systematically different to each other despite both business types employing optometrists trained to the same standard.
The present study uses data from all NHS sight tests performed in Essex from April 2015 to September 2016. During this time, Essex was one of the few places within the UK to routinely capture this data electronically and it represents an area where it is possible to analyse large samples. Further details for the rationale of using Essex as a study area can be found in Shickle et al. (2017).12 The prerequisites to obtain a NHS sight testing contract are independent of the optometrist's place of work. Given this, it might be expected that there would be little difference in sight test outcome depending on which type of optometric practice a patient attends. However, given differences in business models, tests performed11 and false positive referrals13 it is expected that differences in NHS sight test outcomes will also exist.
The aim of the present study was to assess (a) whether NHS sight test outcome is related to practice type (independent or multiple), (b) whether socio-economic deprivation is associated with practice type, (c) what age patients’ have their first NHS sight test.
Materials and methodThe data captured was originally entered by optometry practices onto GOS sight test forms that were used to claim payment from the NHS. This form contains demographic information, reason why the patient qualifies for a NHS sight test and outcome of the sight test; for full details of the content: https://pcse.england.nhs.uk/media/1272/gos1-form_original.pdf.14 These forms were subsequently submitted to Evolutio Care Innovations Ltd, which is a private company employed by NHS England to process GOS sight test payments. These forms were electronically read using optical character recognition software, the data was captured in an Excel spreadsheet, and errors were subsequently checked. Data from 821,624 NHS sight tests performed in Essex were obtained across the time period examined (from April 2015 to September 2016). Data was anonymised (patient names removed and date of births changed to age in years) prior to the research team accessing this data. The data was transferred on a password protected memory stick. 157,144 entries were removed from analysis due to incomplete/missing data or patients living outside of the study area. In total, 664,480 results remained of which 39,392 (5.93%) were first eye tests. First eye tests are determined by ‘date of last eye test’ on the GOS form, typically, there will either be the date of the previous eye test or the word ‘first’ to indicate that the child's parents or guardian state that the child has never received an eye test (either privately or NHS) prior to that visit.
Statistical analysisData were analysed in Lower-Layer Super Output Areas (LSOAs) which are small areas of the UK controlled for population size. LSOAs in England have an average population size of 1500 and there are 1498 LSOA's in the county of Essex.15 Socioeconomic status (SES) was determined using the Index of Multiple Deprivation (IMD), which is the ranking of LSOAs in order from most to least deprived (i.e. one to ten), nationally based upon weights of various deprivation measurements. LSOAs in quintile one, therefore, are in the top 20% of socio-economically deprived LSOAs in the UK (i.e. most deprived).16 Regression analyses were performed using SPSS (IBM Corp. Released 2017. IBM SPSS Statistics for Windows, Version 25.0. Armonk, NY: IBM Corp). Unless otherwise indicated, statistical models included only the variables in question.
Due to differing eligibility of NHS sight tests to different ages, ages are grouped as follows: under 16s (free sight tests for all), those aged 16–59 (free sight tests only for those on means-tested benefits, or some at-risk groups) and 60 and above (free sight tests for all).
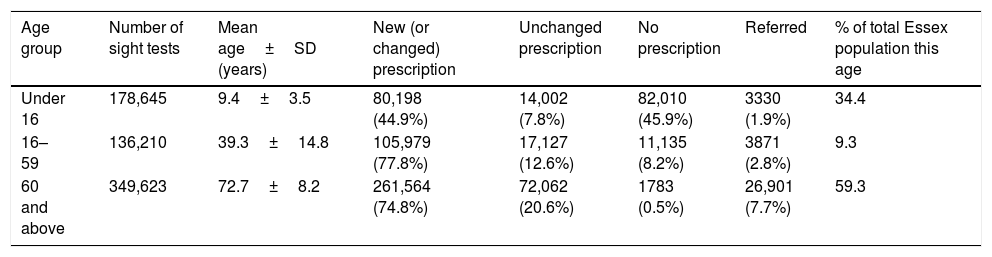
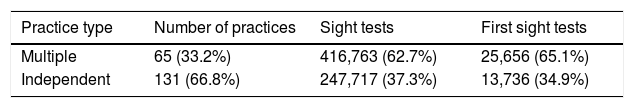
Results664,480 patient's attended for NHS funded sight tests. A breakdown of patients age and sight test outcome are given in Table 1 and a breakdown of sight tests by optical practice type (independent and multiple) are given in Table 2.
A breakdown of patient's ages and sight test outcome found in the present study. Percentages are greater than 100 as patients can be referred and given a prescription (refractive) outcome or referred and nor given a prescription outcome.
| Age group | Number of sight tests | Mean age±SD (years) | New (or changed) prescription | Unchanged prescription | No prescription | Referred | % of total Essex population this age |
|---|---|---|---|---|---|---|---|
| Under 16 | 178,645 | 9.4±3.5 | 80,198 (44.9%) | 14,002 (7.8%) | 82,010 (45.9%) | 3330 (1.9%) | 34.4 |
| 16–59 | 136,210 | 39.3±14.8 | 105,979 (77.8%) | 17,127 (12.6%) | 11,135 (8.2%) | 3871 (2.8%) | 9.3 |
| 60 and above | 349,623 | 72.7±8.2 | 261,564 (74.8%) | 72,062 (20.6%) | 1783 (0.5%) | 26,901 (7.7%) | 59.3 |
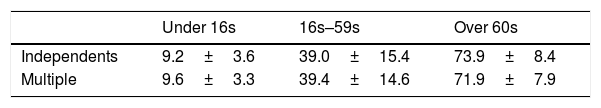
There was no clinically significant difference in ages that visited multiples, relative to independents. Specifically, means and SD's for each age group are detailed in Table 3.
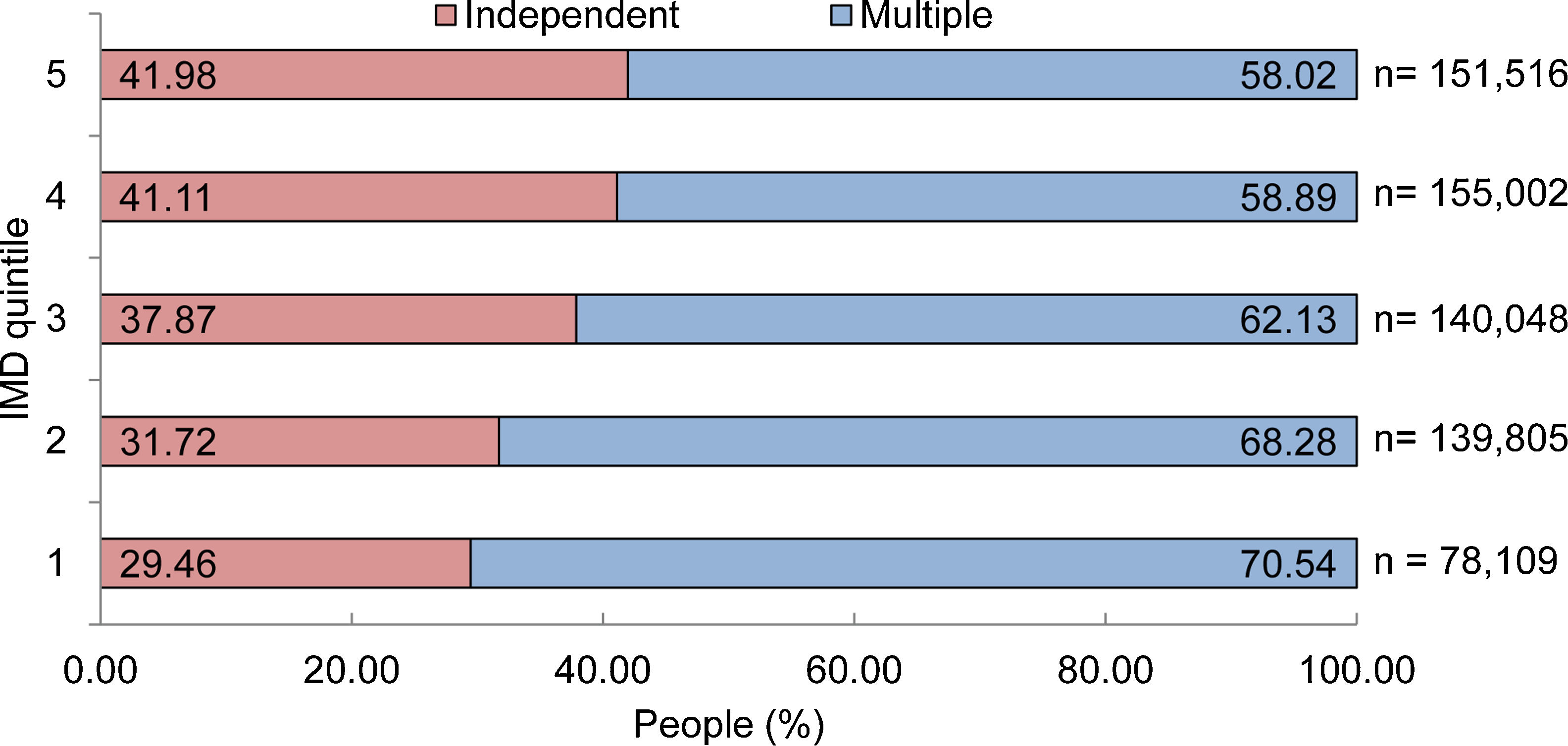
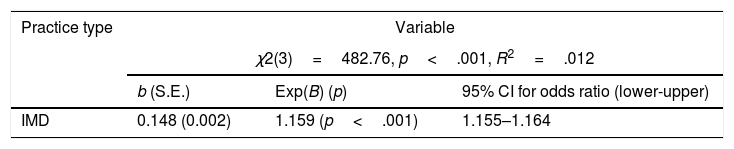
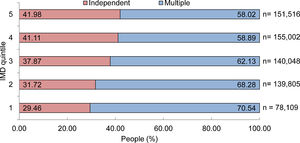
As IMD quintile increases from most to least deprived, the proportion of people presenting to independent, relative to multiple, increases (Fig. 1).
A binary logistic regression indicated that there was a significant association between IMD quintile (one to five) and choice of optometric practice (independent or multiple) (χ2(3)=482.76, p<.001). Specifically, as IMD increased by one quintile, patients were 1.159 times more likely to visit an independent practice (Table 4).
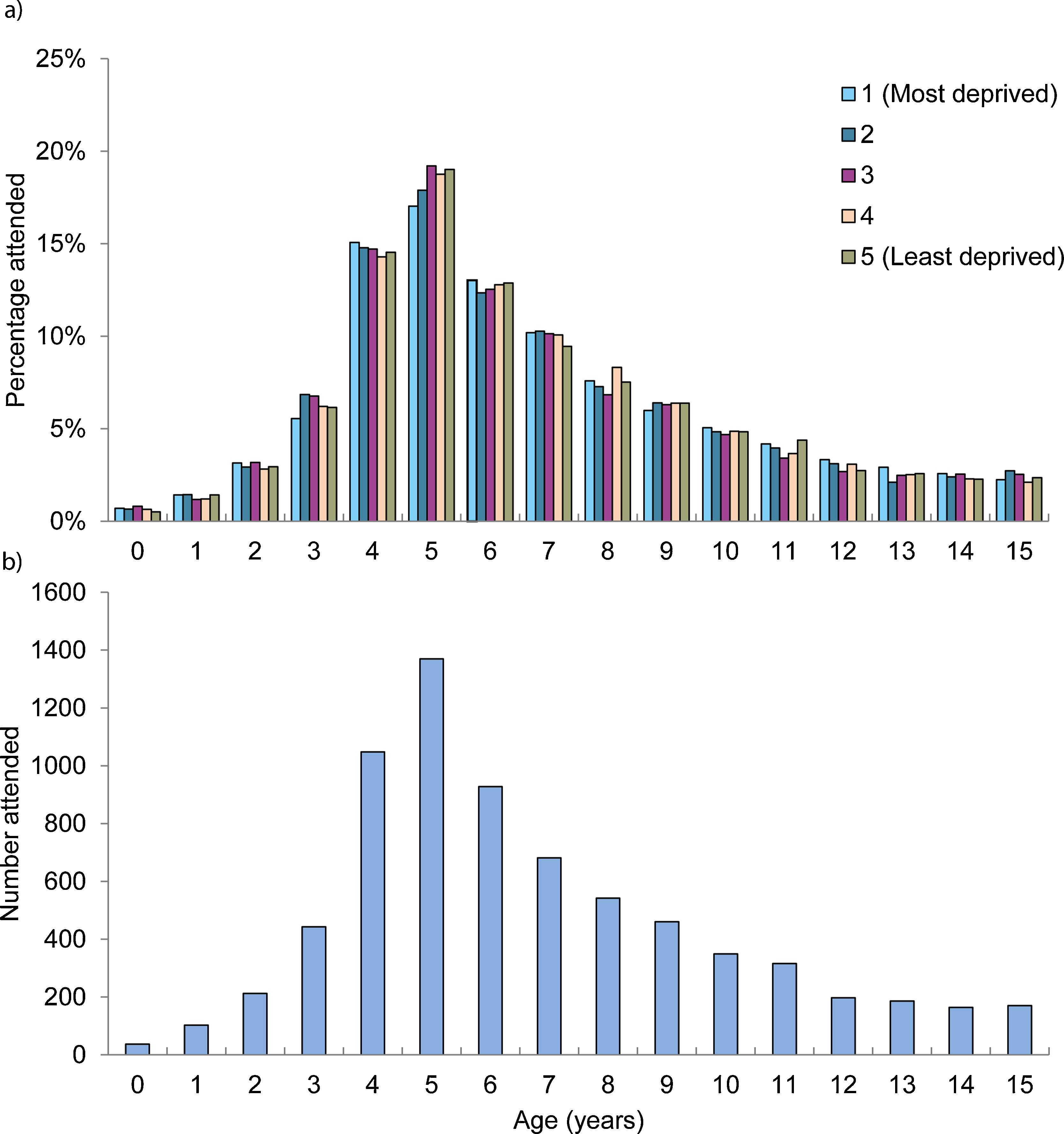
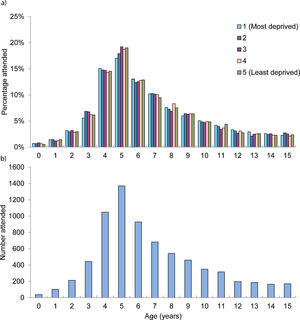
First eye test39,392 patients presented for their first eye test. Due to varying eligibility criteria of differing age groups, only those under 16 (n=30,777) were included for these analyses (Fig. 2).
(a) The number of patients presenting for their first eye test at each age in each IMD quintile. (b) The number of first eye tests at each age after combining all IMD quintiles together. In both graphs each age represents the whole year. For example, an age of 1 represents all people from one year to less than two years.
The mean age for those presenting for their first eye was 6 years and 254 days. This ranged from 6 years and 285 days (IMD quintile 1) to 6 years and 229 days (IMD quintile 3). The median age for a first sight test was 6 in all five IMD quintiles.
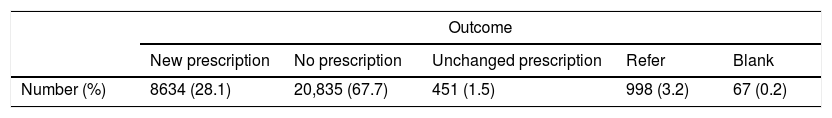
Table 5 details the outcomes of first sight tests. The majority of first sight tests resulted in neither a referral, nor issuing of a spectacle prescription (67.7%).
The number and percentage of each sight test outcome for patients under 16 attending their first sight test (numbers add up to greater than 100% as patients who are referred may or may not additionally receive an outcome for their prescription).
| Outcome | |||||
|---|---|---|---|---|---|
| New prescription | No prescription | Unchanged prescription | Refer | Blank | |
| Number (%) | 8634 (28.1) | 20,835 (67.7) | 451 (1.5) | 998 (3.2) | 67 (0.2) |
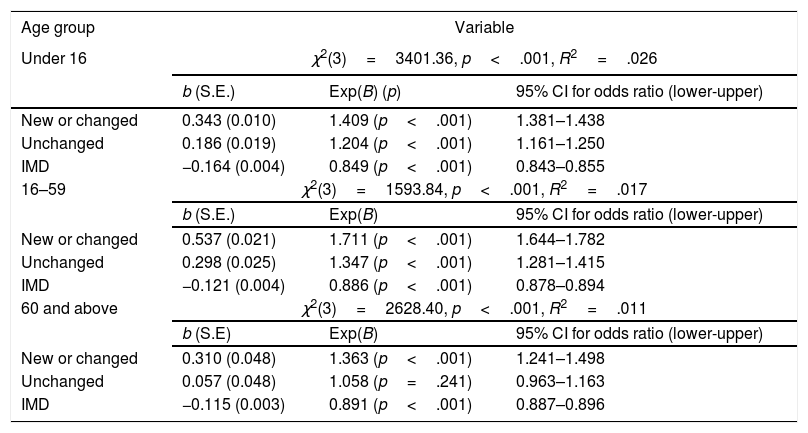
To examine whether the practice type (multiple or independent) had any effect on sight test outcome (new prescription, unchanged prescription or no prescription), separate multinomial logistic regression analyses were performed for each age group. IMD quintile (one to five) in which the patient lives was used as a co-variate to account for the effects of SES on sight test outcome (Table 6).
The effect of practice type on sight test outcome. All outcomes are relative to a patient being issued with no prescription at a multiple, relative to an independent.
| Age group | Variable | ||
|---|---|---|---|
| Under 16 | χ2(3)=3401.36, p<.001, R2=.026 | ||
| b (S.E.) | Exp(B) (p) | 95% CI for odds ratio (lower-upper) | |
| New or changed | 0.343 (0.010) | 1.409 (p<.001) | 1.381–1.438 |
| Unchanged | 0.186 (0.019) | 1.204 (p<.001) | 1.161–1.250 |
| IMD | −0.164 (0.004) | 0.849 (p<.001) | 0.843–0.855 |
| 16–59 | χ2(3)=1593.84, p<.001, R2=.017 | ||
| b (S.E.) | Exp(B) | 95% CI for odds ratio (lower-upper) | |
| New or changed | 0.537 (0.021) | 1.711 (p<.001) | 1.644–1.782 |
| Unchanged | 0.298 (0.025) | 1.347 (p<.001) | 1.281–1.415 |
| IMD | −0.121 (0.004) | 0.886 (p<.001) | 0.878–0.894 |
| 60 and above | χ2(3)=2628.40, p<.001, R2=.011 | ||
| b (S.E) | Exp(B) | 95% CI for odds ratio (lower-upper) | |
| New or changed | 0.310 (0.048) | 1.363 (p<.001) | 1.241–1.498 |
| Unchanged | 0.057 (0.048) | 1.058 (p=.241) | 0.963–1.163 |
| IMD | −0.115 (0.003) | 0.891 (p<.001) | 0.887–0.896 |
For the under 16 category, there was a significant effect of practice type on NHS sight test outcome (χ2(3)=3401.36, p<.001, R2=.026). Specifically, the odds of a patient who attended a multiple receiving a ‘new or changed prescription’ rather than ‘no prescription’ was 1.409 times more likely than the odds for a patient who attended an independent practice. Similarly, the odds of a patient receiving an ‘unchanged’ prescription, rather than ‘no prescription’ at a multiple was 1.204 times that of the odds of a patient attending who attended an independent (p's<.001).
For the 16–59 category, there was a significant effect of practice type on NHS sight test outcome (χ2(3)=1593.84, p<.001, R2=.017). Specifically, the odds of a patient who attended a multiple receiving a ‘new or changed prescription’ rather than ‘no prescription’ was 1.711 times more likely than the odds for a patient who attended an independent practice. Similarly, the odds of a patient receiving an ‘unchanged’ prescription, rather than ‘no prescription’ at a multiple was 1.347 times that of the odds of a patient who attended an independent (p's<.001).
For the 60 and older category, there was a significant effect of practice type on NHS sight test outcome (χ2(3)=2628.40, p<.001, R2=.011). Specifically, the odds of a patient who attended a multiple receiving a ‘new or changed prescription’ rather than ‘no prescription’ was 1.363 times more likely than the odds for a patient who attended an independent practice (p<.001). The odds of a patient receiving an ‘unchanged’ prescription, rather than ‘no prescription’ at a multiple was 1.058 times that of the odds of a patient attending an independent and was not significant (p=.24).
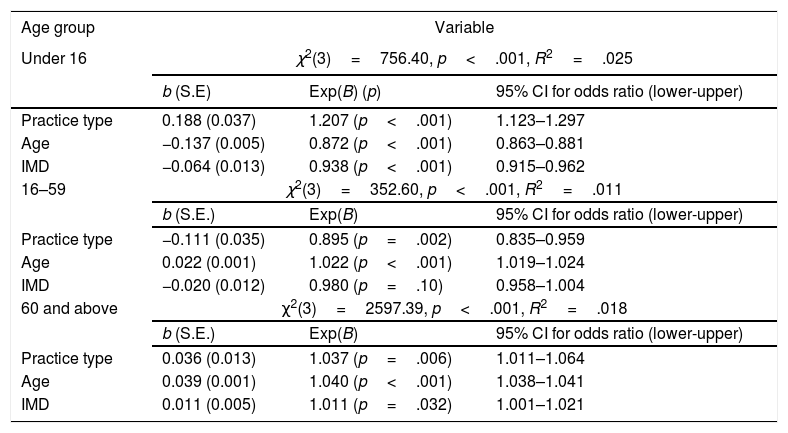
As an alternative, or addition, to patients being given a refractive outcome, the patient may be referred. Separate binary logistic regressions were used for each age group (under 16, 16–59 and 60 and above) to examine the effect of practice type (multiple and independent) on whether the patient is referred. For each age group, age, deprivation quintile (one to five) and referral outcome (referred or not) were used as predictor variables for practice type (Table 7).
The results of the binomial logistic regression analysis with practice type, age and level of socio-economic deprivation (IMD).
| Age group | Variable | ||
|---|---|---|---|
| Under 16 | χ2(3)=756.40, p<.001, R2=.025 | ||
| b (S.E) | Exp(B) (p) | 95% CI for odds ratio (lower-upper) | |
| Practice type | 0.188 (0.037) | 1.207 (p<.001) | 1.123–1.297 |
| Age | −0.137 (0.005) | 0.872 (p<.001) | 0.863–0.881 |
| IMD | −0.064 (0.013) | 0.938 (p<.001) | 0.915–0.962 |
| 16–59 | χ2(3)=352.60, p<.001, R2=.011 | ||
| b (S.E.) | Exp(B) | 95% CI for odds ratio (lower-upper) | |
| Practice type | −0.111 (0.035) | 0.895 (p=.002) | 0.835–0.959 |
| Age | 0.022 (0.001) | 1.022 (p<.001) | 1.019–1.024 |
| IMD | −0.020 (0.012) | 0.980 (p=.10) | 0.958–1.004 |
| 60 and above | χ2(3)=2597.39, p<.001, R2=.018 | ||
| b (S.E.) | Exp(B) | 95% CI for odds ratio (lower-upper) | |
| Practice type | 0.036 (0.013) | 1.037 (p=.006) | 1.011–1.064 |
| Age | 0.039 (0.001) | 1.040 (p<.001) | 1.038–1.041 |
| IMD | 0.011 (0.005) | 1.011 (p=.032) | 1.001–1.021 |
Specifically, patients that attended multiples who were aged under 16 (1.207 times) and 60 and above (1.037 times) were more likely to be referred, relative to patients that attended independent. In contrast, those aged 16–59 who attended multiples were less likely to be referred (0.895 times), relative to those in the same age group that attended independent practices.
DiscussionThe present study found that NHS sight test outcome varies with practice type (multiple or independent) and patient choice of practice is dependent on the deprivation level of the area in which the patient lives. The present study also finds that the age at which a child presents for their first eye test is clinically independent of the deprivation level of the area that they live. Together these findings support the view that there are differences in sight tests between optometrists working in different practices. Importantly, this is not intended to suggest one practice type is superior to the other rather, simply, that differences do exist. Further work is required to explain the reasons for these differences. Indeed, Shah and colleagues11 conducted a study assessing how optometrists performed a sight test on a young myopic patient who presented with headaches. The authors reported that although there may be some differences between optometrists in multiples, relative to independents, there were no significant differences between the two groups when comparing which of the required tests (as judged by a ‘gold-standard’ reference group) were performed.
Practice type and routine NHS sight test outcomeAcross all age groups, patients attending multiples were significantly more likely to receive a ‘new or changed prescription’ relative to ‘no prescription’ compared to those patients that attended independent opticians. Although the exact reasoning's for this are unclear, it could that patients who think that they might require new spectacles choose to visit a multiple, or, alternatively, optometrists may be systematically performing differently. For example, the optometrists working in a multiple may have a smaller threshold for what they consider a ‘new prescription’, relative to an independent optometrist. Further work, therefore, is required to examine this. The finding that patients presenting to multiples are also more likely to receive an unchanged prescription, relative to no prescription, in both the under 16s and 16–59 age groups points to the conclusion that those attending multiples are more likely to wear spectacles, relative to patients visiting an independent. An alternative explanation could be due to differing commercial pressures between the two practice types; optometrists working in multiples may be under more pressure to recommend spectacles, thus, accounting for the differences found in the present study. It is possible that independent opticians are less likely to exist in deprived areas and thus, may influence patient's choice of practice; however this has yet to be studied. There is currently a paucity of research examining sight test outcome, and the large amount of electronically captured data that was analysed in the present study offered us the opportunity to examine this. However, given the retrospective design of this study, we are unable to draw definite reasoning for the differences found between practice types.
There was also a significant effect of practice type on whether patients were referred. The reasons for this are unclear. It has been reported that optometrists who are recently qualified may tend to refer more than their more experienced colleagues.13,17 It could, therefore, be that multiples tend to employ more newly qualified optometrists. Furthermore, it has been reported that multiples tend to produce a greater number of false positive referrals, even when accounting for the effects of optometrist experience.13 There is a paucity of published evidence examining this and it is unclear why this effect would be the opposite for those aged under 16 compared those aged 16–59. For those aged 60 or older, the effect is small (3.7%) and is unlikely to be clinically significant. It could also be that multiples and independent practices have significant differences in price of spectacles. There is, however, a lack of published evidence examining this.
Practice type and first eye testAcross all levels of deprivation, multiple practices conduct the majority of sight tests, however the present study found that as IMD quintile increases by 1, a patient is 15.9% (odds ratio 1.159) more likely to visit an independent optometrist compared to a multiple. One possible explanation for this finding could be that more multiples could be established in deprived areas. A study examining areas of deprivation and optometry practices in Leeds, UK, however, showed that it is rare for any practice (multiple or independent) to be within a LSOA that is from the most deprived IMD decile. Moreover, when these practices are situated within a deprived area, they are typically on the border with a less deprived area.18 Mapping of practice type and IMD quintile was beyond the scope of the present study, but given the business requirements of the optometric business model,19 it is likely that optometrists (multiple and independent) in Essex are also predominately situated in less deprived areas.20
The age at which a child presented for their first eye test ranged by 56 days from 6.63 to 6.78 years depending on IMD quintile (median 6 years in all quintiles). This difference is unlikely to be clinically significant. This average age of first eye test, however, is conservative as all those that received their first eye test at 16 years or older (n=8615) were removed from analysis. Our finding that children are over six and a half years old before their first eye test could be cause for concern. Firstly, this age is considerably later than the 4 or 5 years of age that the NHS recommends for a first vision test.6 This leaves children with potential eyesight issues such as amblyopia going undetected close to the level at which treating becomes significantly more difficult (7 years).9,10 Moreover, in the UK schooling system, children will have typically had two or three years of education before their first sight test. If children are unable to see through this period, it would be expected that this could have an impact on their engagement and ability with education.8 Although, at present, a recent freedom of information request (July 2019) has revealed 96% of children in Essex aged 4–5 now attend school vision screening.21 This school screening scheme existed in a different format in the years that the present study examined (2015–2016) and the proportion of children receiving school screenings at that time is unknown to the local optical committee (Essex LOC, personal communication). All patients aged under 16, regardless of their socio-economic status are entitled to a NHS sight test at no cost to the patient.4 The finding, however, that only 34.3% of patients aged under 16 received a NHS sight test over the 18 month period of the present study supports the view that further work is required to promote the importance of children's sight tests across all socio-economic classes. Reduced visual acuity, that could be detected as part of a sight test, has been shown to be associated with reduced proficiency of reading and writing.22 Accordingly, lack of access to sight tests could be affecting more than just the child's ocular health. As part of a school vision screening, the child's parents receive a letter detailing the outcome; this may be a good opportunity to educate patient's families about the importance of regular eye examinations with optometrists.
Interestingly, the majority (67.7%) of children presenting for their first eye test neither required spectacles nor a referral to a doctor (General Practitioner or hospital eye department). This indicates that of the children in Essex that did attend their first sight test, the majority do so despite having no ocular problems. This could be in part, due to parent's awareness of the importance of sight tests despite no apparent symptoms.6 Although this is positive, the finding that only 34.4% of the Essex population aged under 16 received a NHS sight test, within the county in the 18 months the present study examined, suggests that more work is needed to promote the importance of sight tests.
Limitations of this studyThe present study uses the IMD of the area where an individual lives as a proxy for SES. However, given the way of calculating IMD rankings and the large sample used in the study, it is likely to be a good approximation of the SES for the majority of residents in each area.
Age of sight test on the data set we used was given as a whole number. For example, patients aged 6 years and 11 months were recorded as 6 years old. Therefore, the exact ages for mean age of first eye test can only be used as an approximation.
The metrics recorded: for example, age and whether it is the patient's first eye test relied on patient's information. This is not verified before the practice submits the GOS claim form. Accordingly, there may be some potential of patient's parents or guardians inaccurately recalling if the patient has had a prior eye test. This is unlikely to be an issue in the under 16 age-group as the time between the last eye test to the present visit would be relatively small. However, for those patients attending for their ‘first’ eye test in their 40s and 50s, it could be that they had an eye test as a child and simply could not remember back to that time. Patients 16 and over, however, were not included in the analyses of first eye tests and therefore, the effect on the results should be minimal.
Furthermore, the present study utilised a large sample size (n=664,480) and, as detailed by a recent editorial by Armstrong,23 the small R2 values questions the clinical significance of some of these findings, despite the highly statistical significant p values.
ConclusionThis study demonstrates that SES is associated with the type of optometrist (independent or multiple) a patient visits. Moreover, we demonstrate that the type of practice that a patient visits is associated with the likelihood of being prescribed glasses. We also find that patients in Essex typically present for a sight test at a late age, relative to what is recommended.
EthicsEthical approval had been granted by the Chair of the Biomedical, Natural, Physical and Health Sciences Research Ethics Panel at the University of Bradford on 07/05/19. Reference number EC25621.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interestASs is the interim Chair of Calderdale and Kirklees Local Optical Committee and is an Optometrist. CD is Chair of Bradford Local Optical Committee and is an Optometrist.
The authors would like to thank Prof. David Elliott and Dr William McIlhagga for their helpful discussions and comments. Thanks also to Evolutio Ltd for allowing access to the anonymised data.