To evaluate if fundus photography is useful to study the size of the optic disc in patients with optic nerve head drusen (ONHD).
MethodsCross-sectional study. Fifty-five patients with ONHD confirmed by B-scan echography and 52 patients’ normal controls were studied. Fundus photography was done in all the cases with a telecentric optical system FF450 IR plus from Zeiss with 20° magnification and Visupac measuring system. We measured total optic disc area, vertical and horizontal diameter.
ResultsPatients with ONHD had smaller optic disc area 2.6±0.55mm2 (mean±SD), horizontal diameter (1.68±0.18mm) and vertical diameter (1.94±0.28mm) than normal controls (2.93±0.43mm2, 1.86±0.14mm and 1.98±0.17mm, respectively). Significant differences were found in area (p=0.002) and horizontal diameter (p<0.001).
ConclusionsPatients with optic nerve head drusen had smaller optic disc size than normal controls, under digital fundus photography. Fundus photography could be helpful to differentiate optic nerve drusen from other ocular conditions.
Evaluar la utilidad de la fotografía del fondo de ojo para el estudio del tamaño del disco óptico en pacientes con drusas en la cabeza del nervio óptico (ONHD).
MétodosEstudio transversal. Se realizó un estudio de cincuenta y cinco pacientes con ONHD, confirmado mediante ecografía B-scan, y de 52 controles normales. La fotografía del fondo de ojo se realizó en todos los casos utilizando un sistema óptico telecéntrico FF450 IR plus de Zeiss con magnificación de 20°, y un sistema de medición Visupac. Medimos el área total del disco óptico, y los diámetros vertical y horizontal.
ResultadosLos pacientes con ONHD mostraban una menor área del disco óptico 2,6±0,55mm2 (media±DE), diámetro horizontal (1,68±0,18mm) y diámetro vertical (1,94±0,28mm) que los pacientes con controles normales (2,93±0,43 mm2, 1,86±0,14mm y 1,98±0,17mm, respectivamente). Hallamos diferencias significativas en cuanto al área (p=0,002) y al diámetro horizontal (p<0,001).
ConclusionesLos pacientes con drusas en la cabeza del nervio óptico muestran un tamaño menor del disco óptico en los controles normales, en comparación a la fotografía digital del fondo de ojo. Dicha fotografía del fondo podría ser útil para diferenciar las drusas del nervio óptico de otras alteraciones oculares.
Optic nerve head drusen (ONHD) were histologically described by Müller1 in 1858. In 1868 Liebrich2 described their clinical appearance, seventeen years after Helmhotz had invented the ophthalmoscope. Since then, different terms have been used to describe papillary drusen: optic disc drusen, optic nerve head drusen, colloid or hyaline bodies.3 In clinical practice, the incidence of ONHD is 0.34%4 while histological incidence is 2%.5
Drusen usually have an extracellular location, anterior to the lamina cribosa. In nine out of ten cases they are located behind the Bruch's membrane. Rarely, they grow posterior to the lamina cribosa or protruding into the vitreous (inside the glial tissue). Their pathogenesis is not clear. One of the main theories suggests that eyes with ONHD have smaller scleral canals that causing axoplasmic transport alteration, mitochondrial calcification and drusen formation.6–8
Superficial optic nerve head drusen are usually easily identifiable ophthalmoscopically. However, deep and hidden drusen can be difficult to differentiate from true papilledema. Among the different diagnostic methods, B-scan echography is considered the gold standard for diagnosing optic disc drusen.9
Different authors agree that optic discs are smaller in patients with pseudopapilledema or optic nerve drusen,10–12 than in patients with true papilledema.
Therefore, it would be helpful for clinical optometrist to have an alternative cheap, fast and accurate method for evaluating the optic disc size, when B-scan echography is not available or accessible.
The purpose of our study was to evaluate the optic disc size in patients with optic nerve head drusen using digital fundus photographs and comparing them with normal controls.
MethodsWe proposed a cross-sectional study to examine patients with optic nerve head drusen attended at Ophthalmology Unit, Alcorcon Foundation University Hospital, Madrid, Spain. The research was conducted under the approval of the Institutional Ethics Committee and according to the principles of the Declaration of Helsinki. All patients were given a written explanation of the study and then signed a consent form.
We estimated the sample size that gave a confidence level of 95%, a power of 80% and losses of 10%. Assuming a difference of 0.150mm based on the size differences found by Jonas,10 55 eyes with optic disc drusen and 55 normal control eyes were evaluated.
Inclusion criteria were patients with unilateral or bilateral, visible or buried optic disc drusen, confirmed by B-scan ultrasonography and refractive error lower than ±2 diopters. A comprehensive ophthalmic examination, including visual acuity, refraction, slit lamp examination, intraocular pressure, funduscopy, fundus photography and B-echography was conducted in all these patients.
The control group included patients with normal eye examination and refractive error lower than ±2 diopters, randomly selected between patients attending the Ophthalmology Unit.
Patients with low quality pictures, secondary to media opacity or lack of cooperation, were excluded in both groups.
Fundus photography was done with a fundus camera with a telecentric optical system (FF450 IR plus Zeiss) which incorporates a digital Visupac archiving and measuring system (version 3.2.1 Carl Zeiss Jena GmbH, Ophthalmic Instrument Division, Jena). We used a video camera color 3CCD (Sony Power HAD) (766×576pixels resolution), using the angles measured at 20° angle for the optic disc study.
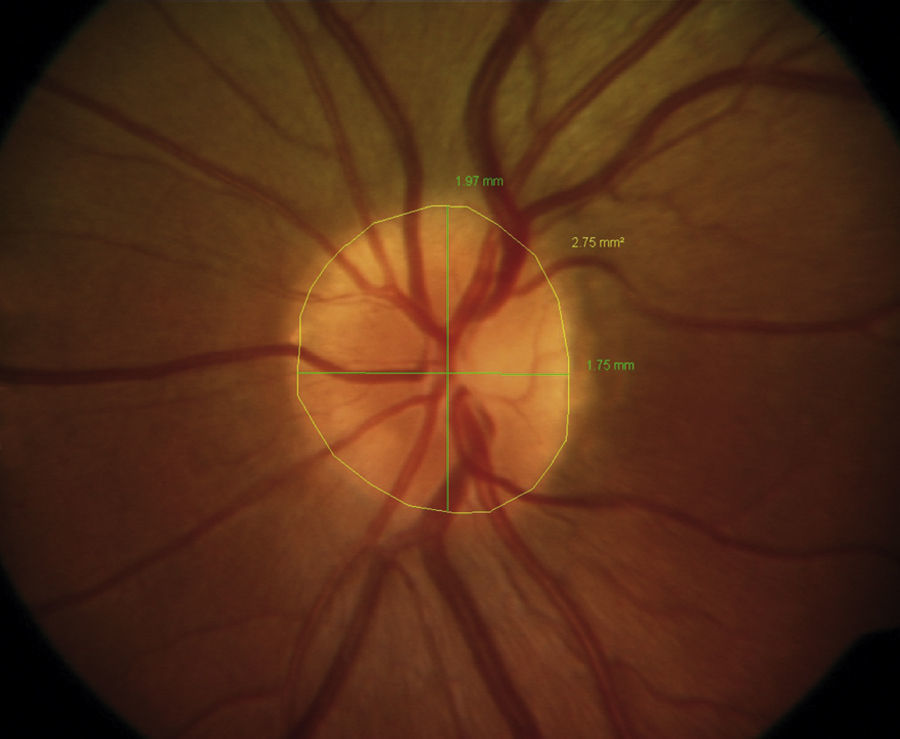
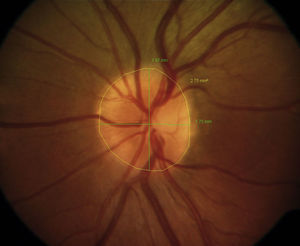
We measured the optic disc area (mm2) and the vertical (from 12 to 6h) and horizontal (from 3 to 9h) diameter (mm) with the Visupac digital analysis system (Fig. 1), as previously described.13 According to the measurement angle (20°) used, we considered the magnification factor for the telecentric optical system.14 To correct the magnification factor of each eye we chose the Bengstton and partners formula (BK-method) based on the best optic correction in each case.15 All cases were analyzed by the same observer (P.G.) in an observer–blind experiment.
Categorical variables are expressed as % rates and measurable variables are expressed as mean (SD) and 95% confidence interval. Categorical variables were compared by the Pearson Chi square with continuity correction or Fisher exact test when at least 25% of values showed an expected cell frequency below 5.
Quantitative variables were compared by the Student t test after evaluation of normal distribution test (Kolmogorov–Smirnov) and equality of variances. Quantitative variables without normal distribution were analyzed by Mann–Whitney U test. All statistical analyses were performed with the use of SPSS software (version 17.0, SPSS, Inc., Chicago, IL), and all reported probability values were 2-sided. We assumed significance at the 5% level (p<0.05).
In patients with bilateral optic disc drusen, only one eye was randomly selected for statistical analysis.
ResultsA total of 107 eyes from 110 eligible subjects were included in this study. We included 55 eyes of 55 patients with optic nerve head drusen (ONHD) confirmed by B-scan ultrasonography. Forty-five patients (81.8%) had bilateral drusen. Age range 5–71 years (mean 37 years). 58.2% of the patients were women, but no statistically significant difference was found. Fifty-two percent of the drusen were visible or superficial and 48% were not visible under ophthalmoscopic examination.
Fifty-two control patients were also studied. Twenty-eight women and 24 men. Age range 5–84 years (mean 40 years).
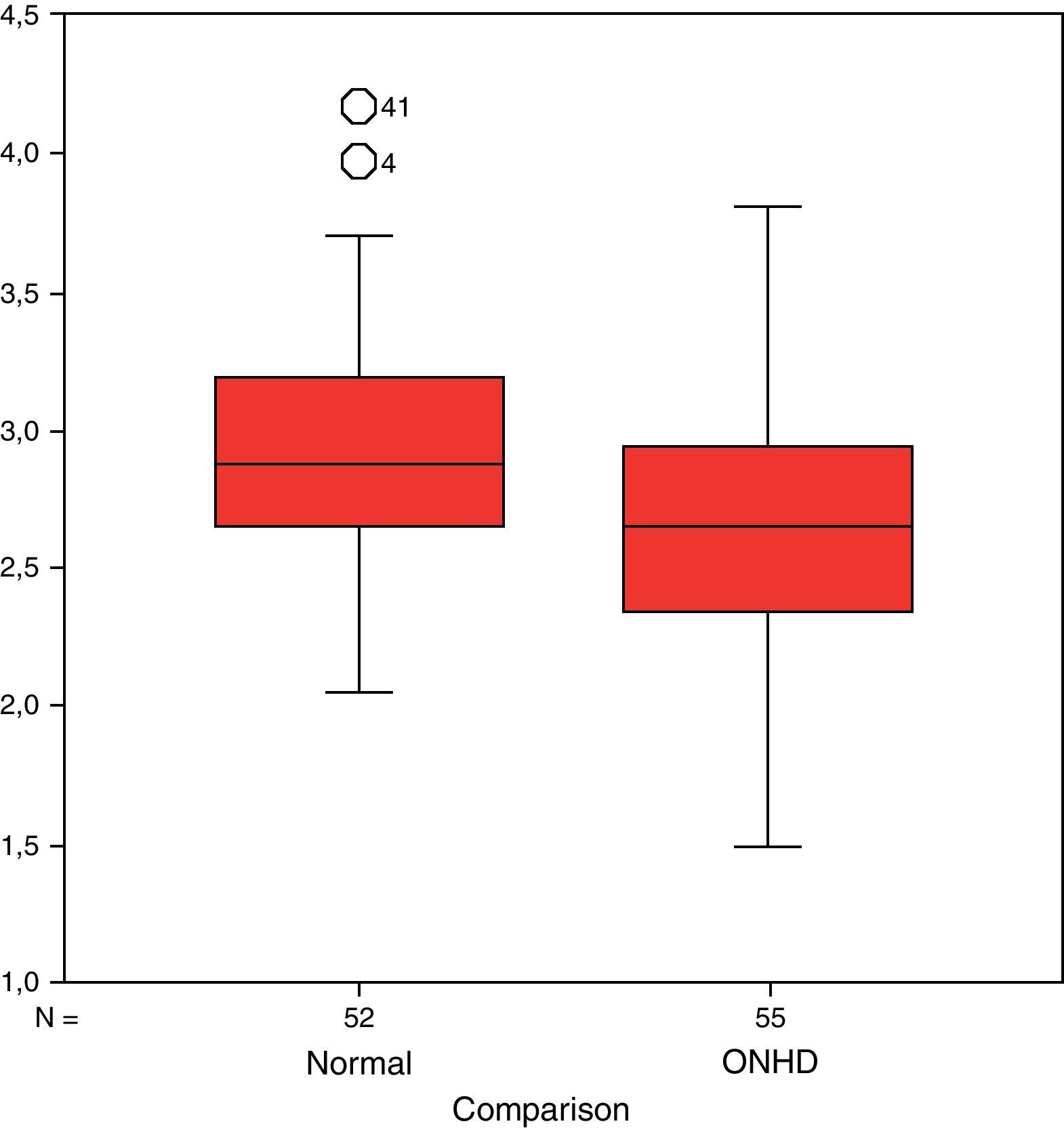
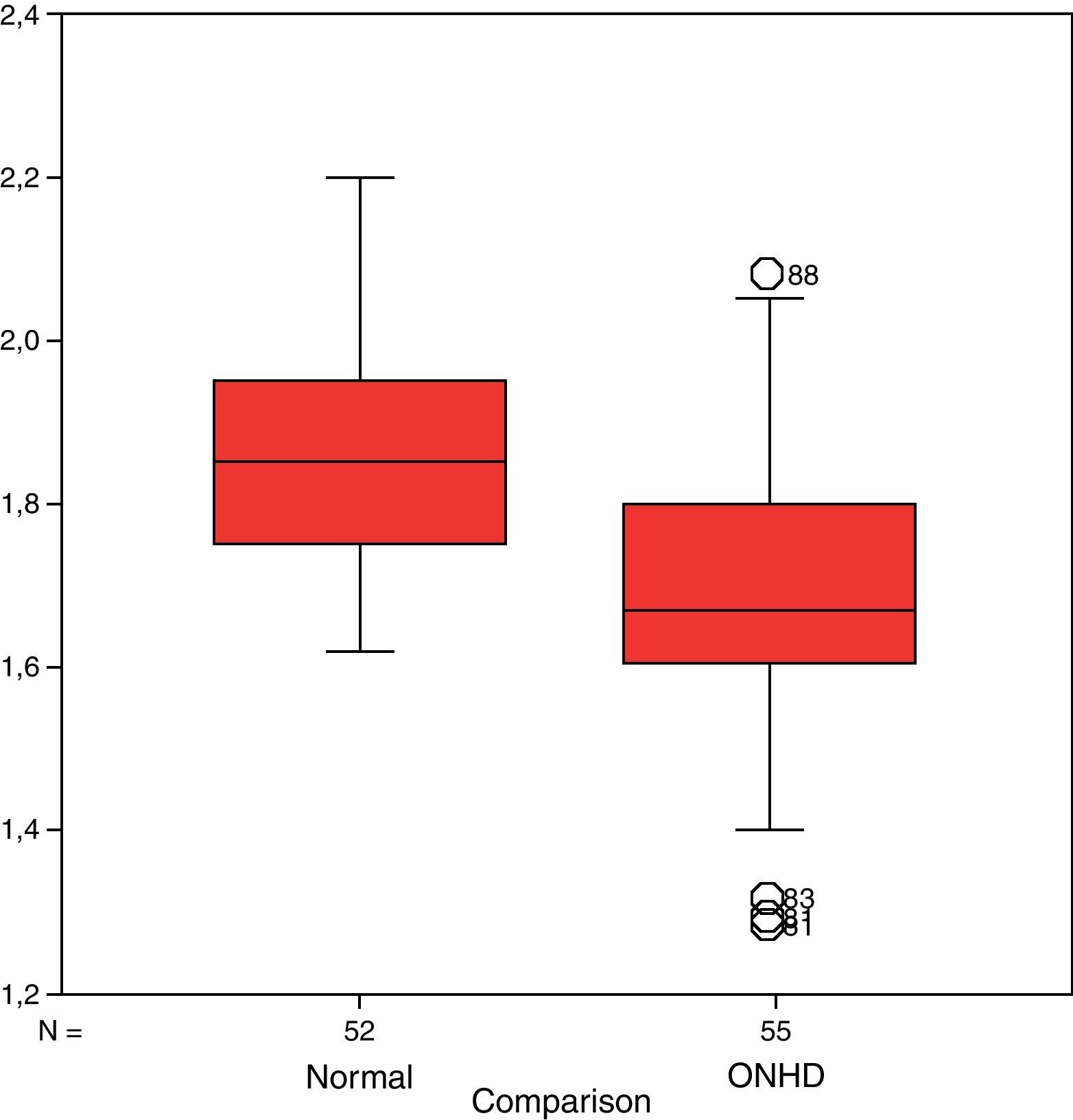
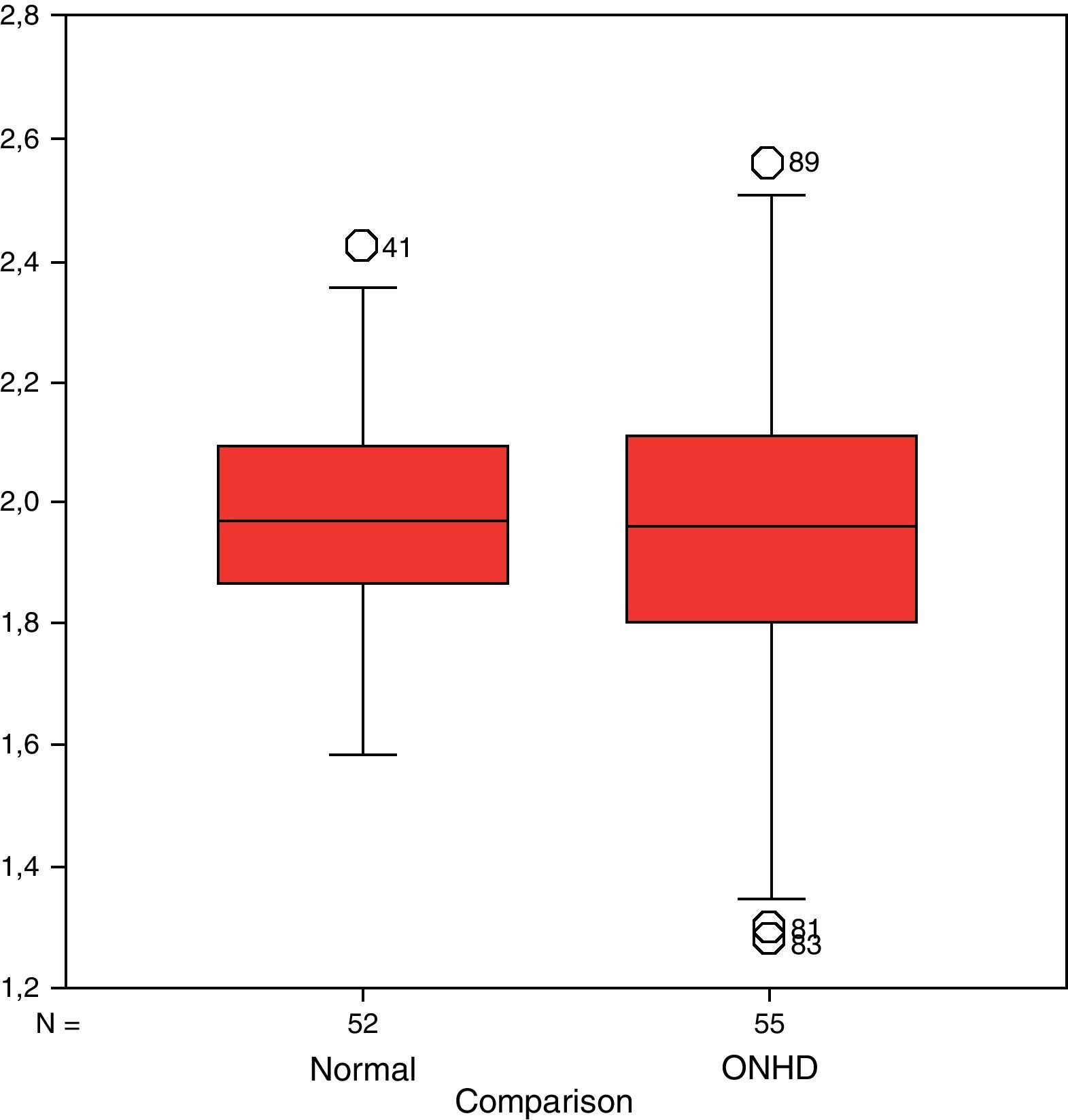
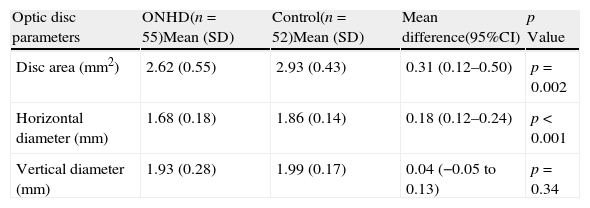
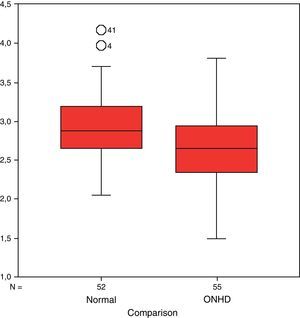
Optic disc area in eyes with ONHD was 2.6mm2 and 2.93mm2 in the controls (p=0.002) (Fig. 2). Horizontal diameter in eyes with drusen was 1.68mm and 1.86mm in the controls (p<0.001) (Fig. 3). Vertical diameter in eyes with drusen was 1.94mm and 1.98mm in the controls (p=0.34) (Fig. 4, Table 1).
Optic disc size: ONHD vs controls.
| Optic disc parameters | ONHD(n=55)Mean (SD) | Control(n=52)Mean (SD) | Mean difference(95%CI) | p Value |
| Disc area (mm2) | 2.62 (0.55) | 2.93 (0.43) | 0.31 (0.12–0.50) | p=0.002 |
| Horizontal diameter (mm) | 1.68 (0.18) | 1.86 (0.14) | 0.18 (0.12–0.24) | p<0.001 |
| Vertical diameter (mm) | 1.93 (0.28) | 1.99 (0.17) | 0.04 (−0.05 to 0.13) | p=0.34 |
ONHD=Optic nerve head drusen. p Value calculated using t Student.
Optic nerve head drusen (ONHD) are usually bilateral and asymptomatic. The loss of visual acuity is rare and usually associated with complications such as ischemic optic neuropathy, neovascular membranes and vascular occlusions.6
The optician optometrist should know the difference between a pseudopapilledema secondary to ONHD, usually with a good prognosis, from true papilledema, a potentially serious pathology.
Ophthalmoscopy was the main method for diagnosing ONHD until more advanced techniques such as autofluorescence, CT or ultrasound appeared.9 Superficial drusen are easy to identify. However, these only represent 47% of all ONHD.6 Other opthalmoscopic characteristics of the optic nerve, such as elevation, blurred edges and the absence of excavation, vascular abnormalities and papillary small size can make us suspect their presence.16 Recent studies have shown that optical coherence tomography (COT) is useful in differentiating ONHD from true papilledema using qualitative and quantitative criteria.17,18
There are three main theories to explain the pathogenesis of optic nerve drusen:
- (1)
Degenerative axonal death.
- (2)
Proteins transudation from congenital abnormal disc vasculature.
- (3)
Axonal flow alteration.
Seitz19 postulated that optic nerve drusen originates from the material extruded after the rupture of the axons in a slow degenerative process. Sacks et al.11 published – as an alternative hypothesis – that congenitally abnormal disc vasculature may allow transudation of plasma proteins. That could act as a nidus for the deposition of extracellular materials with the result of drusen formation. Spencer7 proposed that drusen were the consequence of an axonal flow alteration. Tso,8 from his studies with electronic microscopy, pointed out that an abnormal axonal metabolism leads to drusen formation.
Different authors suggest that the chronic axoplasmic flow obstruction, that leads to optic nerve drusen, is probably caused by a small scleral canal.11,12,20
This is also supported by the fact that optic nerve drusen are rare in African-Americans21 who usually have larger scleral canals than Caucasians.22,23
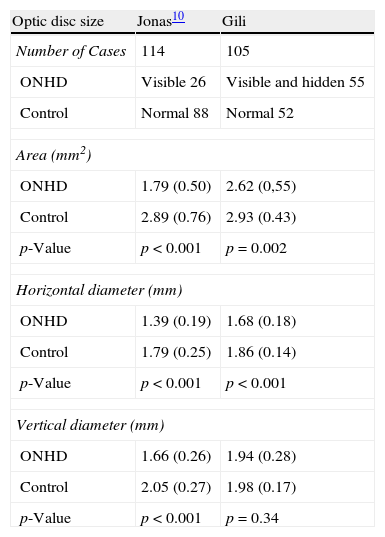
Some authors have previously described small optic discs in patients with optic nerve drusen.10–12Compared with our findings, Jonas10 has reported similar papillary measures in his control group, but lower measures in his ONHD group. These can be explained by differences in the population analyzed, the equipment used and the types of ONHD studied (Jonas studied only visible ONHD and we studied both visible and hidden).Jonas finds significant differences between ONHD and normal optic discs in all the parameters. We only found significant differences in the area and the horizontal diameter (Table 2).However, Floyd,24 found equal or even larger papillary sizes in patients with papillary ONHD than in controls, after measuring the scleral canal with optical coherence tomography. The author suggests that the presence of calcium accumulation could mask the pigment epithelial layer, simulating an apparent larger size of area and disk diameter. In future studies we plan to analyze ONHD with spectral domain tomography and fundus photography simultaneously.
Optic disc size in patients with optic nerve head drusen (ONHD) and controls by different authors: median (SD) and p-value.
| Optic disc size | Jonas10 | Gili |
| Number of Cases | 114 | 105 |
| ONHD | Visible 26 | Visible and hidden 55 |
| Control | Normal 88 | Normal 52 |
| Area (mm2) | ||
| ONHD | 1.79 (0.50) | 2.62 (0,55) |
| Control | 2.89 (0.76) | 2.93 (0.43) |
| p-Value | p<0.001 | p=0.002 |
| Horizontal diameter (mm) | ||
| ONHD | 1.39 (0.19) | 1.68 (0.18) |
| Control | 1.79 (0.25) | 1.86 (0.14) |
| p-Value | p<0.001 | p<0.001 |
| Vertical diameter (mm) | ||
| ONHD | 1.66 (0.26) | 1.94 (0.28) |
| Control | 2.05 (0.27) | 1.98 (0.17) |
| p-Value | p<0.001 | p=0.34 |
In conclusion, patients with optic nerve head drusen have smaller optic disc size, under digital fundus photography. This finding, together with what has been previously reported by other authors10–12 supports the pathogenically theory that a small scleral canal leading to an axoplasmic flow alteration, could be the cause of optic disc drusen formation.
Fundus photography to study the papillary size could be helpful to differentiate optic nerve head drusen from other ocular conditions. Although echography is the best way to study optic nerve drusen, fundus photography – harmless, fast and easy to perform – may be useful when other tests are not available.
Conflict of interestThe authors have no conflicts of interest to declare.