This study aimed to investigate the correlation between convergence insufficiency symptom survey (CISS) score and the signs of convergence insufficiency (CI) and to evaluate the sensitivity and specificity of the CISS to predict CI and ametropia among young adult university students.
MethodThis prospective cross-sectional clinic-based study included 300 first year university students (mean age = 21.58 (SD ± 2.2) years) who consecutively reported for eye examination. Participants were administered the CISS questionnaire and investigated for the signs of CI. Diagnosis of CI was based on presence of three or four signs. The correlation between the CISS score and the signs of CI were determined and Receiver Operation Characteristics (ROC) curves were used to evaluate sensitivity and specificity.
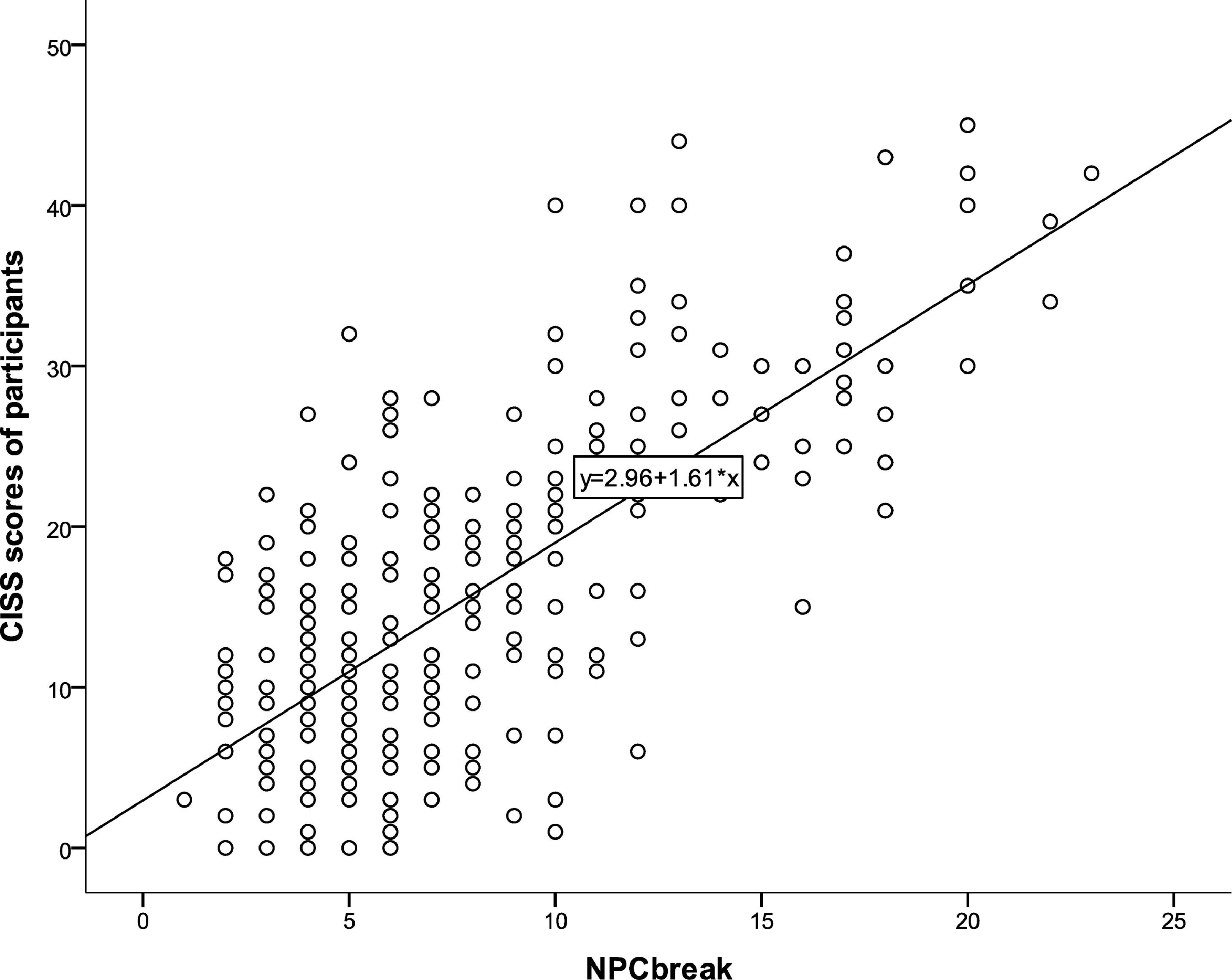
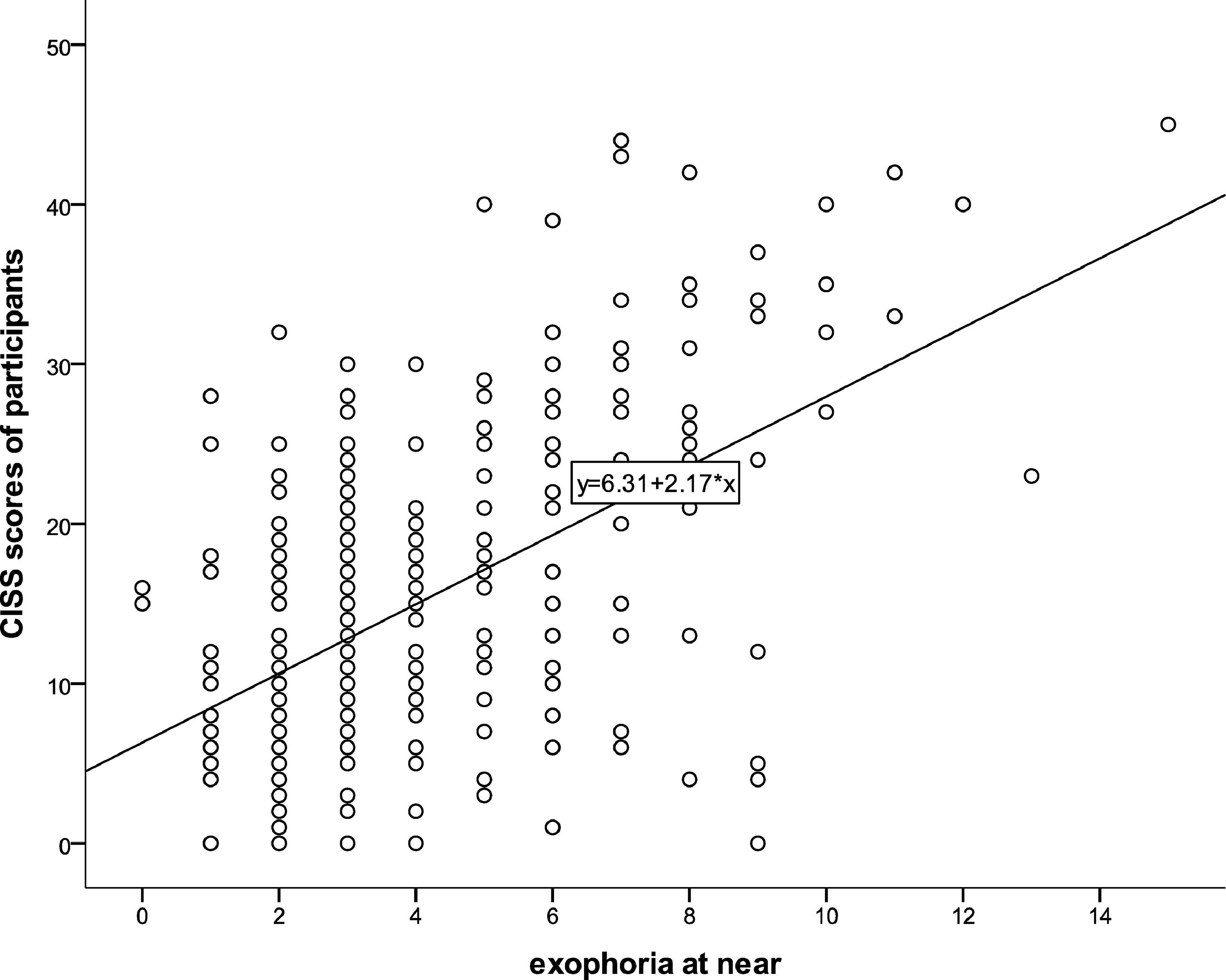
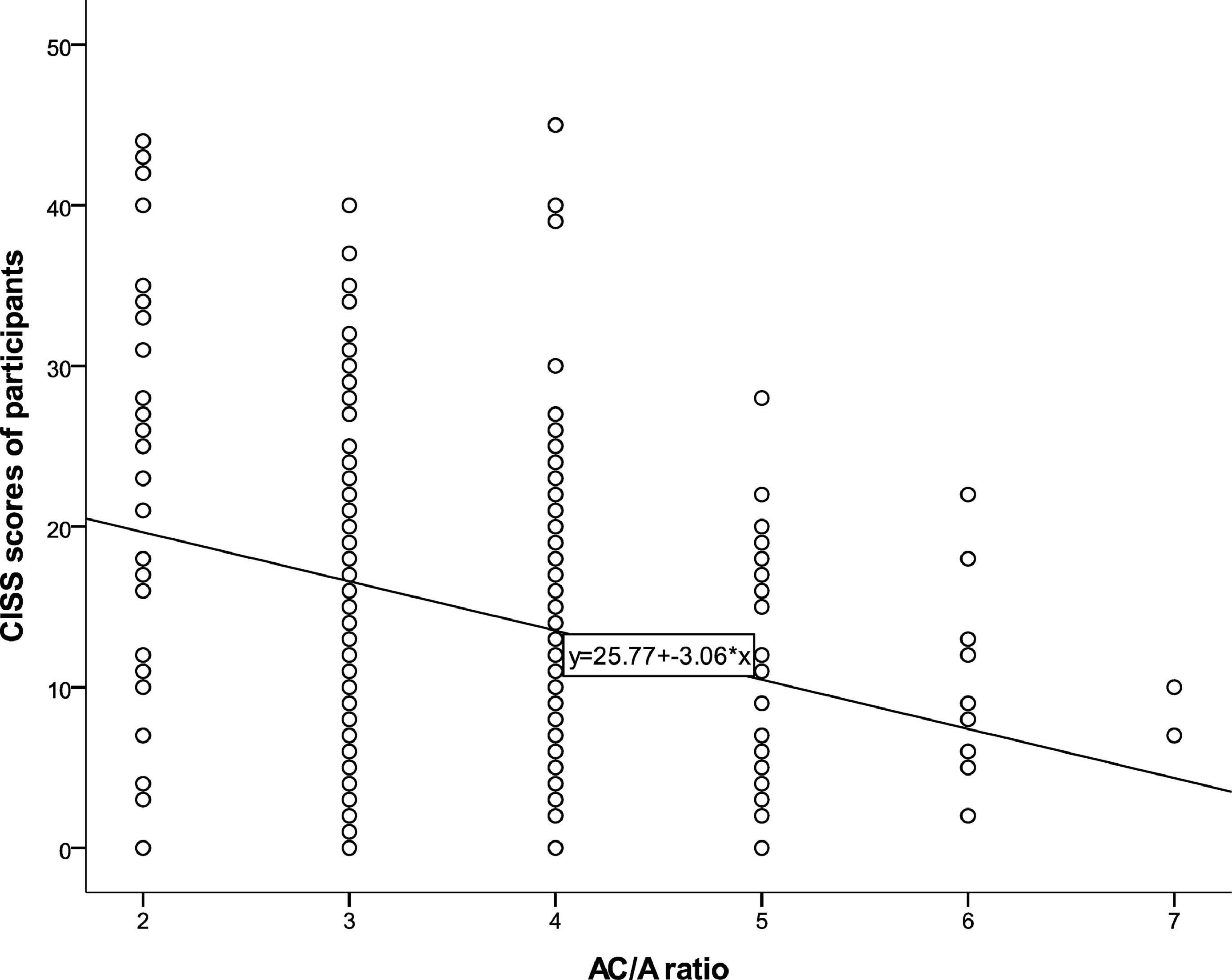
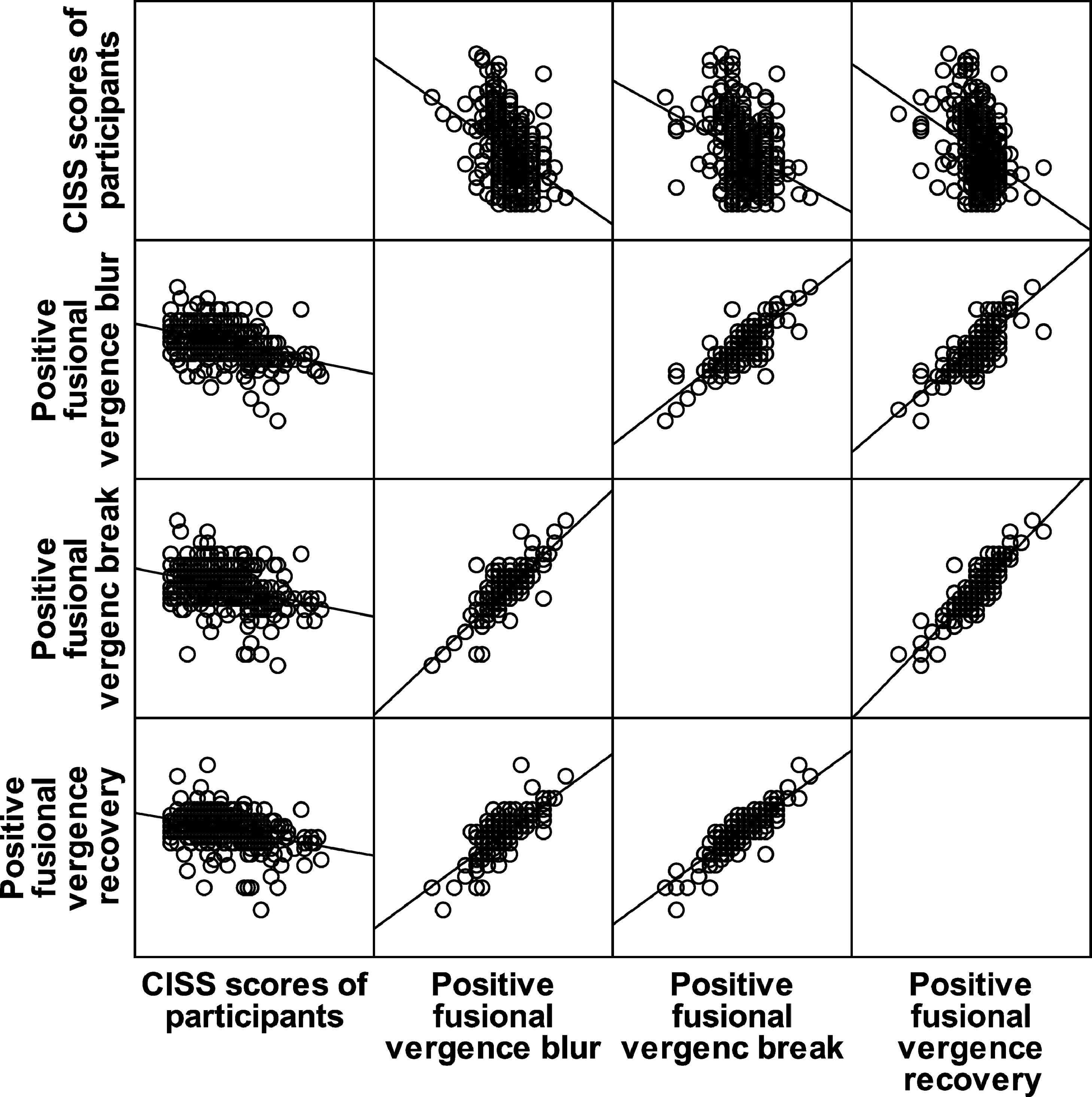
ResultsThere were significant correlations between CISS score and the clinical signs of CI namely NPC break (rs = 0.622, p = 0.0001), NPC recovery (rs = 0.620, p = 0.0001), near exophoria (rs = 0.434, p = 0.0001), near PFV blur (rs = -0.359, p = 0.0001), near PFV break (-0.306, p = 0.0001), near PFV recovery (rs = -0.326, p = 0.0001) and gradient AC/A ratio (rs = -0.290, p = 0.0001). There was a significant positive correlation between CISS score and the number of clinical signs of CI (rs = 0.575, p-value = 0.0001). The CISS had good sensitivity (AOC = 0.882) to predict CI and poor sensitivity (AOC = 0.642) to predict ametropia.
ConclusionThe CISS score is correlated with the severity and number of signs of CI in young adult Ghanaian university students. Its use in addition to clinical investigative testing may give a definitive diagnosis of symptomatic CI.
Convergence insufficiency
Convergence insufficiency symptom survey
Receiver Operating Characteristics
Area under the curve
Positive fusional vergence
Near point of convergence
Convergence insufficiency (CI) is the commonest vergence disorder in young adult African populations.1,2 It is typically characterized by symptoms of asthenopia mostly during reading or performing near work and clinical signs such as exophoria greater at near than distance, receded near point of convergence, decreased positive fusional vergence at near and other signs of low accommodative convergence over accommodation (AC/A) ratio.3 Recent reported prevalence's among African university students range from 1.6% among Optometry students in Ghana2 to 29.6% in first year University students in Benin City, Nigeria.1 A specialized questionnaire for CI (Convergence Insufficiency Symptom Survey, CISS) has been shown to have good construct validity and reliability and has been used to measure the type, severity and frequency of symptoms before and after treatment for patients with symptomatic CI.4,5 There is evidence of a case of CI in an African patient who was successfully treated using the CISS scores as guide to evaluate outcome.6 In a recent study, it has been confirmed that examiner bias in terms of CISS questionnaire administration does not affect CISS scores.7
Rouse et al.8 in their study among 8 to 12 year old children suggested a potential correlation between patient symptoms and the number of clinical signs of CI even though there was no statistically reported findings to support this assertion. Another study among symptomatic children with a CISS score greater than 16 and three clinical signs of CI, found no correlation between the severity of the clinical signs and their level of symptoms.9 One study, however, determined significant weak correlations between symptoms and clinical signs of CI among children 8 to 10 years of age.10 This latter study10, however, did not administer the CISS. Study by Horwood et al.11 on young adults showed that a high CISS score can be a good predictor of presence of one or more signs of CI. However, authors did not find any study that has investigated specific correlations between the clinical signs of CI and level of symptoms among young adults. With different CISS cut off points for symptomatic and asymptomatic young adults12 and children, 13 it is likely that the findings on relationship between signs and symptom levels might differ.
A study indicated that the CISS is not specific for CI;14 the originators of the revised CISS also acknowledge that it could be helpful in patients with other accommodative or vergence disorders13 because their symptoms are similar.3 Borsting et al.15 also found out that the CISS was able to discriminate between children with accommodative insufficiency and normal binocular vision. With ametropia been one of the major conditions encountered in the optometric clinic population,16 it was prudent to investigated possible associations between CISS score and ametropia. The symptoms of some types of ametropia and accommodative or binocular vision anomalies may overlap.17
The present study aimed to investigate the correlation between CISS score, and severity and number of clinical signs of CI among a young adult African University population. It also aimed to evaluate the sensitivity of the CISS to predict CI among these young adult African students. The present study also sought to explore possible associations between CISS scores and magnitudes of ametropia and to evaluate the sensitivity and specificity of the CISS to predict ametropia among these young adult African students.
MethodologyEthical considerationsThis clinic-based prospective cross sectional study adhered to the tenets of the declaration of Helsinki. Institutional ethical approval was obtained from Institutional Review Board of University of Cape Coast (Reference number: UCCIRB/CHAS/2015/057). The participants signed a written informed consent before enrolling each of them into the study.
Study participants, setting and sampling procedureThe study was conducted in the optometric clinic situated on the campus of the University of Cape Coast, Ghana. The study population were first year university students (admitted within the 2015/2016 academic year) who reported to the optometric clinic for the university's mandatory first year student's eye examination. All first year students who consecutively attended the clinic for eye examination within the study period of October, 2015 to April, 2016 were enrolled into the study if they gave informed consent.
Clinical proceduresVisual acuityDistance visual acuity (VA) at 6 m and near VA at 0.4 m was taken using a distance Snellen chart and a near N-notation visual acuity chart respectively.
External and internal eye examinationThe ocular adnexa and anterior segment of both eyes were examined under a slit lamp biomicroscope. (Topcon SL-2G); the posterior segments of both eyes were examined using Keeler professional direct ophthalmoscope.
Inclusion / eligibility criteriaFirst year students aged 18 to 30 years old were included in the study. Students with ocular diseases, strabismus, nystagmus, unilateral or bilateral blindness, or on medications or any form of medical treatment were excluded from the study.
Questionnaire administrationThe 15 item revised CISS questionnaire (with each item scored on a scale of 0 to 4, where 4 represents the highest frequency of occurrence of symptoms "always" and 0 represents no symptom)12 with a good internal consistency (Chronbach alpha = 0.880) among Ghanaian University students, was administered to selected participants. All 15 item scores for each participant were summed to obtain the total CISS score. A CISS score greater than or equal to 21 was considered symptomatic.12
RefractionObjective refraction was determined with static retinoscopy (Keeler Professional streak retinoscope) followed by subjective refraction with a manual phoropter (Topcon VT-10).18 Final refractive correction was determined as the highest plus lens or least minus lens for best corrected visual acuity (BCVA) for each eye. Myopia and hyperopia were defined as minus and plus spherical equivalent refractive errors of greater than or equal to 0.50 DS respectively; astigmatism was defined as cylindrical correction of greater than or equal to 0.50 DC.
Binocular vision examination for CIBinocular vision investigation for CI included: measurement of near point of convergence (NPC) break and recovery using push-up method with RAF rule, measurement of distance and near lateral phoria using von Graefe phoria technique, smooth vergence testing to determine distance and near horizontal positive fusional vergence (PFV) amplitudes, and accommodative convergence over accommodation (AC/A) ratio using gradient method.12 Binocular vision testing was done over BCVA refraction results.
Criteria for diagnosing CI and ametropiaCI was diagnosed if three or more of the following clinical signs were present: a receded NPC (break point >8 cm),3,12,19 near decompensated exophoria greater than far exophoria (difference ≥ 6Δ), 9,19 low AC/A ratio (less than 3:1),3 reduced PFV at near (<15Δ Sheard's criteria).9,19 Ametropia was diagnosed if with BCVA refractive correction in place, participants presented normal results in binocular vision testing.20
Statistical methodsData was analyzed using IBM SPSS version 21 (SPSS, Inc., Chicago, IL, USA). Descriptive statistics such as frequencies, means with standard deviations, percentiles and 95% confidence intervals were computed for outcome variables. Normality of data was determined using the Shapiro Wilk p- values. Independent Sample Man Whitney U test was used to determine significant differences in age and CISS score among gender. Correlation between CISS score and clinical signs of CI were determined using Spearman's rho correlations. Welch ANOVA was used to test difference in CISS score between different ametropia. The sensitivity and specificity of the CISS to predict CI and ametropia were evaluated using Receiver Operating Characteristics (ROC) curves. With analysis done within 95% confidence interval, a two-tailed p-value ≤ 0.05 was considered statistically significant.
ResultsThe study enrolled 322 first year students out of which 22 were excluded with external ocular diseases (n = 9), internal ocular diseases (n = 5), strabismus (n = 3), nystagmus (n = 1), and on medical treatment (n = 4). A total of 300 first year students comprising 167(55.7%) males and 133 (44.3%) females aged 18 to 27 years (mean = 21.58 (SD ±2.2) years) were included in the study. Table 1 represents a descriptive data of all the parameters measured; some parameters were approximately normally distributed whilst others were not (Table 1). The minimum CISS score was 1 and the maximum was 42. The mean rank age for males (171.71) was significantly different from that (123.86) for the females (Mann–Whitney U test; p = 0.0001). The mean rank CISS score for males (152.61) was not significantly different from that (147) for females (Mann–Whitney U test; p = 0.637) Table 2 indicates the frequencies of refractive status, CI status and the number of clinical signs of convergence insufficiency observed among participants. The mean rank CISS score of participants with convergence insufficiency (254.02) was significantly higher than that (139.42) for those without convergence insufficiency (Mann–Whitney U test; p = 0.0001). The descriptive measures for parameters of binocular vision for participants diagnosed with CI are indicated (Table 3). The NPC break and recovery of symptomatic CI participants were significantly higher than that for asymptomatic CI participants (Table 3). There were no significant differences in near exophoria, positive fusional vergence and AC/A ratio between symptomatic CI participants and asymptomatic CI participants (Table 3).
Descriptive measures of parameters investigated.
IQR – interquartile range, CISS- convergence insufficiency symptom survey, Exo- exophoria, N- near, PFV- Positive fusional vergence, rec – recovery, Eso- esophoria, D- distance, CI- convergence insufficiency, Ame- Ametropia, Emm- Emmetropia.
Frequencies of various conditions investigated.
Descriptive parameters of participants with convergence insufficiency.
NPC – near point of convergence, IQR – interquartile range, Exo- exophoria, N- near, PFV- Positive fusional vergence, rec – recovery, D- distance, CI – convergence insufficiency
There were significant correlations between CISS score and the clinical signs of CI (Table 4). Figs. 1, 2, 3 and 4 represent scatterplots of the association between specific parameters.
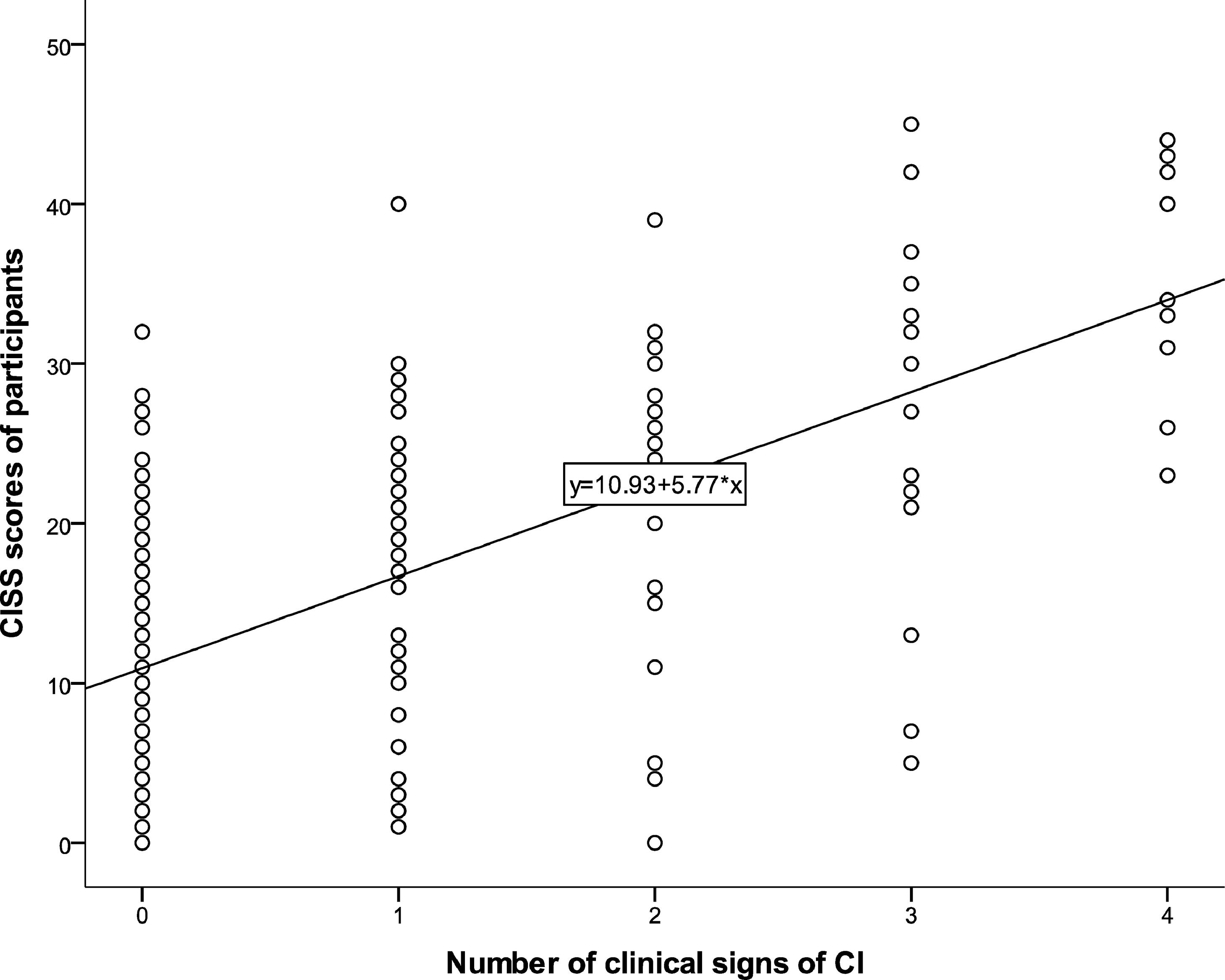
Association between CISS score and number of clinical signs of CIThere was significant positive correlation between CISS score and the number of clinical signs of CI (rs = 0.575, p-value = 0.0001) as indicated (Fig. 5).
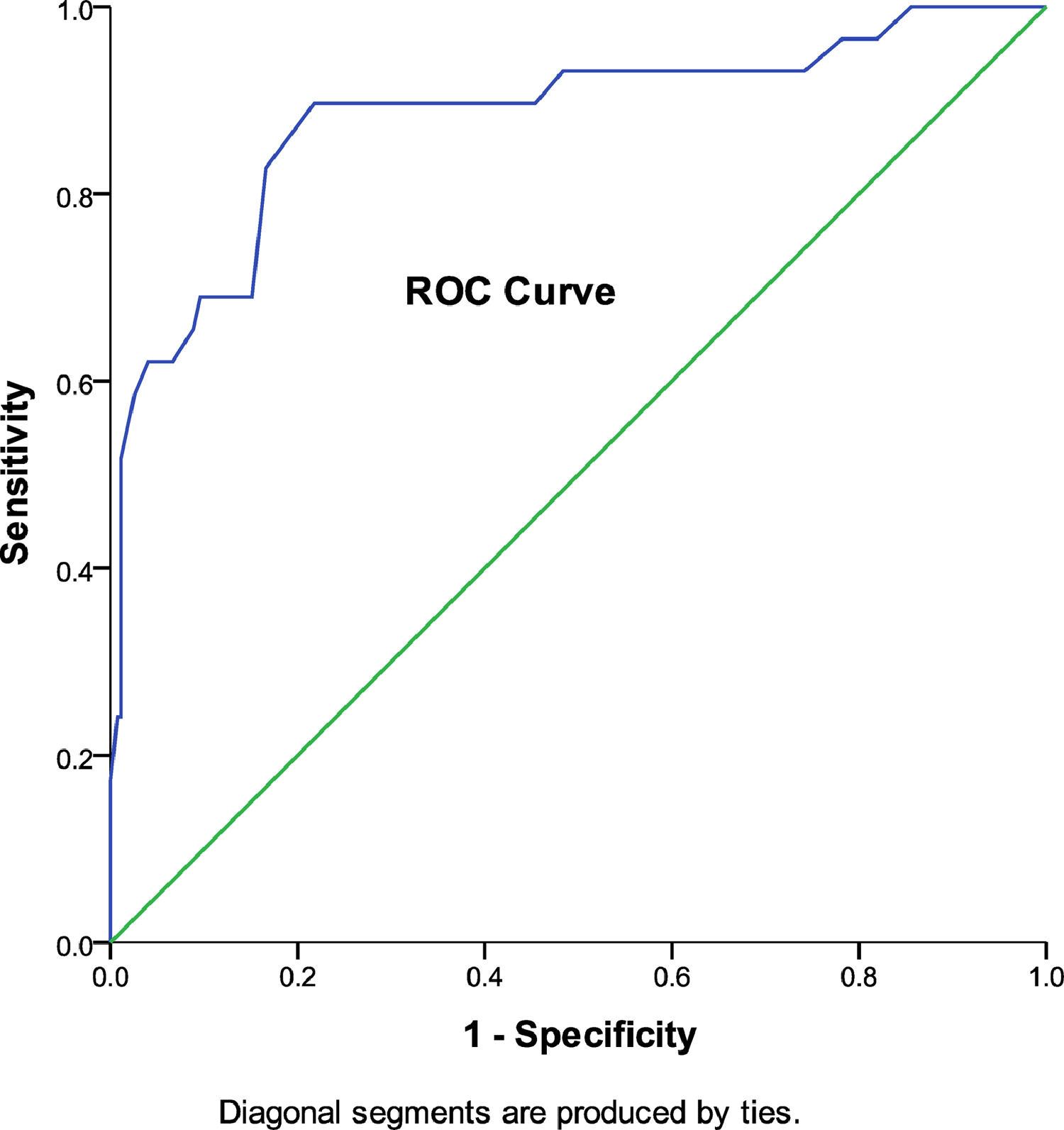
The association between CI and SymptomsOut of the 29 participants with convergence insufficiency, 26 were symptomatic and 3 were asymptomatic. Holding gender constant, symptomatic participants were more likely to experience convergence insufficiency (OR = 34.508, 95% CI = 9.945–119.688, p = 0.0001) compared to asymptomatic participants (OR = 0.029, 95% CI = 0.01–0.101, p = 0.0001). There was a statistically significant ROC curve (p = 0.0001, AOC = 0.882, 95% CI = 0.804–0.960) with AOC indicating a good sensitivity and specificity of the CISS to predict CI (Fig. 6).
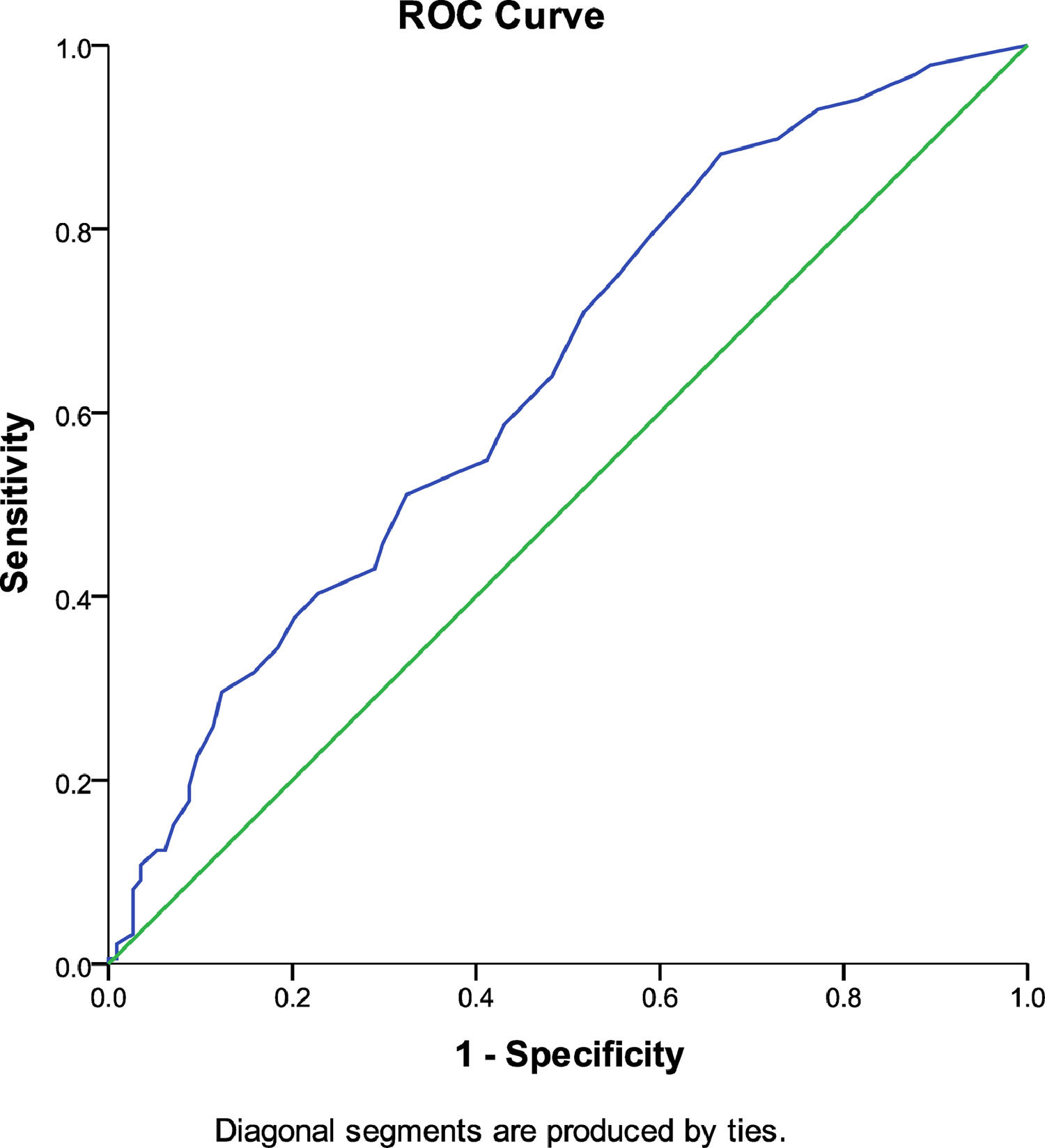
The CISS score and ametropiaThere was no significant correlation between CISS score, and magnitude of myopia (rs = 0.002, p- value = 0.992), magnitude of hyperopia (rs = 0.170, p-value = 0.188) and magnitude of astigmatism (rs = -0.069, p-value = 0.521). The mean rank CISS score for participants with ametropia (166.64) was significantly different from that (124.16) for those with emmetropia (Mann–Whitney U test; p = 0.0001). Using Welch ANOVA, there was no significant difference in CISS score (Fig. 6) between the different types of ametropia (F (2,183) = 1.489, p = 0.228). There was a statistically significant ROC curve (p = 0.0001, AOC = 0.642, 95% CI = 0.577–0.706) with AOC indicating a poor sensitivity and specificity of the CISS to predict ametropia (Fig. 7).
DiscussionThe CISS score was found to be associated with the severity of specific CI signs and number of classic signs of CI among young adult university students. A higher CISS score among this young adult population is indicative of the severity of many signs of convergence insufficiency and vice versa. A higher CISS score (which directly predicts a greater likelihood of the presence of CI) was associated with all the signs of CI namely receded NPC break and recovery, higher decompensated exophoria at near, lower positive fusional vergence amplitudes and lower AC/A ratios. This result is not comparable with that found in children with three sign symptomatic convergence insufficiency.9 The present study further emphasizes the difference in the relationship between symptoms and signs of CI in adults and children, as earlier indicated in difference in cut-off point for CISS.12,13
The linear relationships observed between the signs and symptoms of CI emphasize the point that treatment directed towards improving NPC, PFV, compensating for near exophoria and improving AC/A ratio goes a long way to treating this condition as seen in the African case report.6 The linear relationship between the CISS score, and the clinical signs of NPC break and near exophoria in this young adult population is inconsistent with that among symptomatic presbyopes with CI (for base line CISS scores)21 and that among children 9 to 17 years old.9
The negative correlation between positive fusional vergence amplitudes and CISS score among the young adult population is not comparable to that for base line CISS scores in the study by Yi Pang et al. 21 Authors found no study that has compared AC/A ratio to CISS score. As high CISS score predict the presence of CI, low AC/A ratio is already known to be one of the clinical signs of CI.3
The present study results indicate that there is a greater likelihood for identifying symptomatic CI compared to asymptomatic CI using the CISS score. It also indicates that even though the chances are small, there is likelihood that asymptomatic participants (based on the CISS score) have CI. This indicates a limitation with the use of the CISS to screen for CI in young African adults; this observation was also emphasized by Horwood et al.11 in their study among young adults. The diagnosis of CI should be based primarily on identifying the clinical signs rather than dependence on the CISS score. The CISS score when used in addition to clinical investigative testing for signs will give a definitive diagnosis of asymptomatic or symptomatic CI.
Of all the signs of CI investigated, only NPC was significantly higher among participants with symptomatic CI than asymptomatic ones. The mean difference in NPC break (5.62 cm) is higher than the mean standard deviations of 3.78 cm and 2.00 cm respectively for the symptomatic and asymptomatic CI groups being compared. Also, the mean difference of 6.48 cm in NPC recovery is higher than the mean standard deviations of 3.90 cm and 2.52 cm respectively for the two groups. These differences in NPC break and recovery (between symptomatic and asymptomatic CI groups), therefore, are considered clinically meaningful. It can be inferred from this result that the sign of receded NPC may be accounting for the presence of significant symptoms among participants with CI. Symptomatic CI thus may result from the higher demand on convergence of the visual system during near focus. The CISS score cannot be used to predict ametropia within the population. This was further emphasized as participants with ametropia were asymptomatic and showed no differences per the CISS score (Table 2).
The validity and reliability of the CISS have been established in both children and adults.12,13 A score of 21 or higher differentiate adults with symptomatic CI from normal adults.12 In our study, the average CISS score for all the subjects (15.21) suggest that averagely, participants were asymptomatic. The average CISS score (30.24) for participants diagnosed with CI is consistent with that of the CITT study group.9 Generally, the diagnosis of CI in previous studies have been made using three9,22 or four3,19 of the clinical signs as employed in the present study. The prevalence of CI among the young adult Ghanaian university students (9.7%) is comparable to the 10% among young adult British university undergraduate and postgraduate students,11 7.7% among 65 Spanish university students (in a study where CI was diagnosed based on four clinical signs),23 higher compared to 1.6% among Optometry students in Ghana2 and lower compared to 29.6% among first year students in Nigeria.1
The study participants (university students) easily understood the concepts of blur and double vision and gave clear and reliable responses during testing. Authors, however, acknowledge as a limitation, the use of a less repeatable phoria measurement technique (von Graefe) in the present study, instead of a more repeatable technique like cover test.24 von Graefe phoria technique produces greater heterophoria values than cover test among non-presbyopic patients.25 It is thus possible that near phoria values in the present study may have been overestimated. The results in the present study are delimited to the procedures used.
ConclusionThe CISS score is correlated with the severity and number of signs of CI and has a good sensitivity and specificity to predict CI in young adult Ghanaian students. The CISS poorly predicts the presence of ametropia among the young adult population. Its use in addition to clinical investigative testing gives a definitive diagnosis of symptomatic CI.


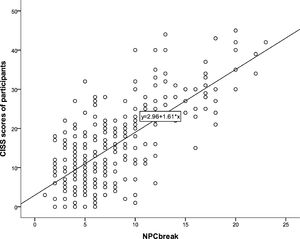 CISS score and
CISS score and 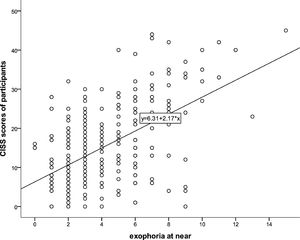 CISS score and exophoria at near.' title='Positive correlation between
CISS score and exophoria at near.' title='Positive correlation between 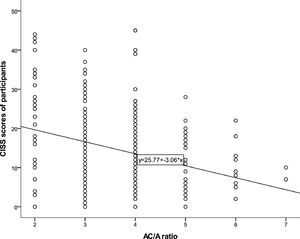 CISS score and AC/A ratio.' title='Negative correlation between
CISS score and AC/A ratio.' title='Negative correlation between 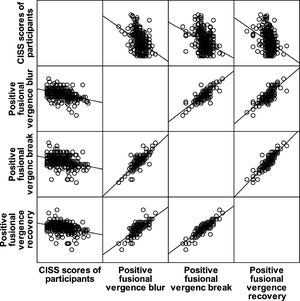 CISS score and
CISS score and 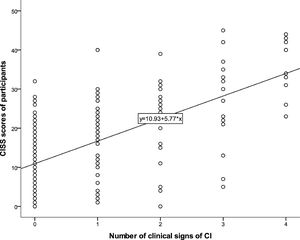 CISS score and number of signs of CI.' title='Positive correlation between
CISS score and number of signs of CI.' title='Positive correlation between 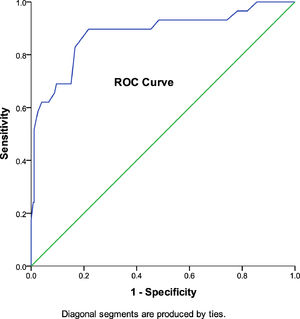 ROC Curve indicating good sensitivity and specificity of
ROC Curve indicating good sensitivity and specificity of 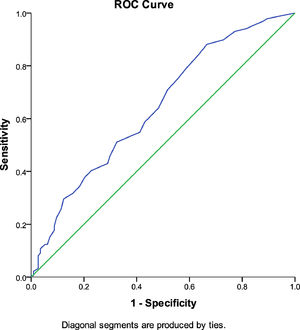 ROC Curve indicating poor sensitivity and specificity of
ROC Curve indicating poor sensitivity and specificity of 





