To describe differences in the number of visits and in the number of diagnostic lenses (DL) necessary to fit rigid gas permeable (RGP), traditional hydrogel and silicone hydrogel contact lenses (CL) in non-pathological eyes.
MethodsRetrospective analysis of 196 refractive or cosmetic CL fittings (Optometry Unit, IOBA Eye Institute). Only daily wearers of CL were included. Patients with ocular pathology, orthokeratology, etc. were excluded.
ResultsOf all CL fitted, 21 % were RGP, 51 % were traditional hydrogel CL and 28 % were silicone hydrogel. RGP required slightly more visits (median 4, range 2–6; p<0.001 ANOVA Kruskal-Wallis) when compared to traditional (median 3, range 2–5) and silicone hydrogel CLs (median 3, range 2–5). No differences were found (p>0.05 ANOVA Kruskal-Wallis) between new and previous wearers. RPG requires more DL (median 3, range 1–5; p<0.001 ANOVA Kruskal-Wallis) when compared to traditional (median 2, range 1–4) or silicone (median 2, range 1–4) hydrogel CLs. No differences in visits (p=0.31 ANOVA Kruskal-Wallis) and DL (p = 0.65 ANOVA Kruskal-Wallis) were found between traditional and silicone hydrogel lenses.
ConclusionsRGP fitting requires slightly more visits and DL than fitting of traditional or silicone hydrogel CL. No difference in the number of visits and DL required between traditional and silicone hydrogel CL were found. An estimated three to four visits could be necessary to fit daily wear CL in non-pathological eyes. This clinical evidence (grade IV) could be used to improve the clinical guidelines for fitting and care of patients with CL.
Describir las diferencias en el número de visitas y en el número de lentes de diagnóstico (LD) probadas para prescribir lentes de contacto (LC) rígidas permeables al gas (RPG), de hidrogel tradicional o de hidrogel de silicona en ojos sin patología.
MétodosAnálisis retrospectivo de la adaptación a 196 lentes de contacto correctoras o cosméticas (Unidad de Optometría, Instituto de Oftalmología Aplicada - IOBA). Sólo participaron usuarios de LC diarias. Fueron excluidos los pacientes con patología ocular, ortoqueratología, etc.
ResultadosDe todas las LC adaptadas, el 21 % fueron RPG, el 51 % hidrogel tradicional y el 28 % hidrogel de silicona. Las RPG precisaron ligeramente más visitas (mediana 4, rango 2–6; ANOVA de Kruskal-Wallis p<0,001) comparadas con las LC tradicionales (mediana 3, rango 2–5) y las de hidrogel de silicona (mediana 3, rango 2–5). No se observaron diferencias (ANOVA de Kruskal-Wallis p>0,05) entre las personas que las llevaban por primera vez y los usuarios previos. Las RPG requirieron más LD (mediana 3, rango 1–5; p<0,001 ANOVA de Kruskal-Wallis) comparadas con las LC de hidrogel tradicional (mediana 2, rango 1–4) o de silicona (mediana 2, rango 1–4). No se encontraron diferencias en el número de visitas (p=0,31 ANOVA de Kruskal-Wallis) ni de LD (ANOVA de Kruskal-Wallis p=0,65) entre las lentes de hidrogel tradicionales y las de silicona.
ConclusionesLa adaptación de RPG requirió levemente más visitas y LD que las LC de hidrogel tradicional o de silicona. No se obtuvieron diferencias en el número de visitas ni en el LD requeridas para la adaptación de las LC de hidrogel tradicional y las de hidrogel de silicona. Se estimó que para adaptar LC en régimen de uso diario se precisan entre tres y cuatro visitas. Estas evidencias clínicas (grado IV) podrían utilizarse para mejorar las recomendaciones clínicas durante la adaptación de las LC y el cuidado de los usuarios de LC.
Contact lenses (CL) are a convenient and popular means of correcting ametropias, with approximately 125million wearers worldwide.1
Different guidelines2–7 have been proposed to care for CL wearers; these describe the fitting procedures and aftercare. Normally, they contain a number of recommendations including patient selection, pre-fitting considerations, lens examination, dispensing of lenses, patient education, and after care management. However, there is no detailed description of the number of visits and diagnostic or trial lenses required to fit CL.
Each manufacturer8–10 provides different recommendations for the fitting of their CL, with different numbers of visits and follow-up care schedules. The manufacturers also urge the wearer to follow the practitioner's recommendations. These manufacturer fitting guides normally recommend 3 to 6 follow-up visits: the first or evaluation visit, the dispensing visit, and visits after 24hours, one week, and one month of wear, as well as visits every 3 to 6 months thereafter.
Although studies have described the number of diagnostic lenses (DL) or the number of visits required to complete a successful fit in complicated cases such as keratoconus or irregular cornea after corneal refractive surgery. However, little information is available for more commonly encountered situation or about the differences in the number of visits required for the various CL types, such as soft (traditional and silicone hydrogel CL) versus RGP etc.2,11,12 Traditional hydrogel CL are defined as those in which oxygen permeability is logarithmically linked to the water content.4
Thus, some need exists for clinical evidence regarding the number of visits or DL necessary to fit CL in non-pathological eyes (refractive or cosmetic CL fittings). This information could be useful for assisting with practitioner and patient decisions about appropriate lens wear,13 especially enabling novice practitioners to improve their clinical practice.
The purpose of this study was to describe the differences in the number of visits necessary to fit RGP, hydrogel and silicone hydrogel CL in non-pathological eyes. This information could be useful to propose clinical evidence-based recommendation or guide-lines for fitting daily wear lenses.
Materials and methodsSubjectsThe clinical history of 196 daily wear CL subjects was retrospectively analyzed; these were subjects who received an initial eye examination at the Optometry Unit of the IOBA Eye Institute, School of Optometry, University of Valladolid (Spain). All subjects were fitted by the same experienced practitioner (RM).
Patients with ocular pathology, e.g., keratoconus and orthokeratology and extended CL wearers were excluded to guarantee that difficult cases did not affect the study results. Daily disposable wearers were also excluded.
Of all patients, 62 % were non-CL wearers and 38 % were previous lens wearers who came to the Optometry Unit for the first time and they have been previously fitted by other practitioners (they were re-fitted with new CL). There were 60 % women and 40 % men (mean age, 33.1±10.2 years; range, 10–51). The spherical refractive error ranged from −21.00 to + 11.25 D (−2.70±4.45 D) with an astigmatic refraction range of 0.00 to 7.00 D (0.93±1.16 D).
Contact lenses fit protocol and visitsA CL fitting protocol was defined in accordance with previous clinical guideline2,14 recommendations. This protocol is summarized in four steps:
Step #1. Patient evaluationA detailed examination of the anterior eye with a biomicroscope, a record of the visual acuity, refraction and keratometry of both eyes (other optometric evaluations such as binocular vision and accommodation were also recorded if necessary). The lens options (materials, wear options, frequency of replacement, cleaning and care, etc.) were discussed with the patient to assist with making an informed decision.
The objective of this first step was to determine whether the patient was a suitable candidate for wearing CL and to prescribe a lens constructed from a physiologically adequate material that would have minimal mechanical impact on the corneal surface while providing the required optical correction.
Step #2. Diagnostic lens evaluationPatients were fitted with DL (RGP, hydrogel or silicone hydrogel CL) and evaluated after 5-20minutes of wear. This evaluation determined adequate CL position, movement and over-refraction in order to obtain the optimal visual acuity. Changes in parameters were considered if position and movement were unacceptable.2,14 Vertex distance was considered in cases of refraction or over-refraction greater than±4.00 D.
The initial selection of a DL was typically guided by the recommended parameters from the manufacturer's fitting guide.
We defined DL as those CL fitted for the purpose of defining their parameters.15 These could be a trial RPG CL to define base curve radius and lens parameters, or lenses ordered directly from the manufacturer (RGP, hydrogel or silicone hydrogel lenses), especially in the case of disposable or toric lenses.
Step #3. Trial CL fitting and dispensingBefore receiving their CL, patients must demonstrate the ability to insert, remove and take care of their lenses, as well as to follow strict personal and CL hygiene and to adhere to the daily wearing schedule.
Before patients left the office, an assessment of the ability to handle the lenses was recorded. An appropriate cleaning and disinfecting system was provided.
Step #4. Trial CL evaluationAn eye evaluation was scheduled after the initial 3-4 weeks of lens wear to allow any necessary mechanical or optical refinements in the lens prescription, to monitor adaptation, to minimize ocular complications and to reinforce appropriate lens care. CL were required to be worn for at least 4 to 6hours prior to examination.
If the lens provided acceptable fit, vision, comfort, and binocular vision, the fitting procedure was satisfactorily concluded and the patient was scheduled for follow-up visits every 6–12 months. However, if patients were uncomfortable, had surface ocular complications or presented a lack of adequate visual acuity, new lenses were reordered with the appropriate changes and a new follow up visit was scheduled.
Follow-up visits included a case history, recording of the patient's symptoms, visual acuity evaluation, over-refraction (if necessary), detailed biomicroscopic examination of the anterior eye, including tarsal conjunctiva after upper lid eversion, CL surface observation, fluorescein instillation and management of patient problems. Keratometry and spectacle refractions were performed periodically for comparison with baseline measurements. Also, lenses and patient hygiene were checked.
The practitioner could often complete the first 3 steps of this protocol in the first visit, particularly in the cases of hydrogel and silicone hydrogel CL and RGP without eye complications. Astigmatic patients may require special DL because it is difficult to have all spherical and cylinder possibilities for trial lenses available in the office. After the dispensing visit, an eye evaluation was scheduled in 3 or 4 weeks of wear to evaluate the ocular surface and patient tolerance. If no complications were detected, definitive CL could be ordered and a follow-up schedule was created.
This four-step protocol permitted CL fitting with only two visits: the first visit (patient evaluation, DL evaluation and dispensing) and the second visit (lens evaluation, after-care and follow-up program prescription). However, it was sometimes necessary to modify the CL parameters to improve position, movement and patient visual acuity. Also, some patients needed more time to manipulate, insert and remove lenses with skill. In these cases, more visits were sometimes necessary to complete the CL fitting.
Statistical analysisStatistical analysis was performed using commercially available software (SPSS 15.0; statistical package for Windows; SPSS, Chicago, IL). A descriptive analysis with mode, median and range was made in order to determine the number of visits and DL necessary to fit RGP, traditional and silicone hydrogel CL.
Non-parametric analyses of variance (ANOVA Kruskal-Wallis) were used to assess differences in the number of visits and number of DL between CL types (RGP, traditional and silicone hydrogel), between spherical and astigmatic CL fitting, and between patient types (new CL wearers versus previous CL wearers). A p<0.05 was considered statistically significant.
ResultsOne hundred fifty-five patients (79.1 %) were fitted with soft CL [100 (51.0 %) with hydrogel CL and 55 (28.0 %) with silicone hydrogel lenses] and 41 (20.9 %) were fitted with RGP lenses.
Spherical CL were fitted in 145 (74.0 %) of the cases [70 (48.3 %) with hydrogel CL, 34 (23.4 %) with silicone hydrogel and 41 (28.4 %) with RGP lenses]. Astigmatic lenses were fitted in 42 (21.4 %) patients [26 (61.9 %) with hydrogel CL, 16 (38.1 %) with silicone hydrogel and no one with RGP].
Only 10 patients (4.6 %) received multifocal CL to correct presbyopia [4 (44.4 %) with hydrogel CL, 5 (55.6 %) with silicone hydrogel and no one with RPG]. Most patients (59.7 %) were fitted with monthly disposable CL and less than 3 % were fitted with daily disposable lenses.
No subjects had significant biomicroscopic signs (grade > 2, Efron grading scale) of CL complications (corneal staining, limbal injection, striae, folds, or other) or other severe complications, such as microbial keratitis, after CL fitting.
Number of contact lenses fit visitsThe median number of 3 visits was necessary to complete the CL fitting, range 2–6. There were significant differences (p<0.001 ANOVA Kruskal-Wallis) between the number of visits necessary to fit RGP (median 4, range 2–6) and hydrogel (median 3, range 2–5), or silicone hydrogel (median 3, range 2–5) lenses. No differences were found between the number of visits required to fit traditional hydrogel and silicone hydrogel CL (p=0.31 ANOVA Kruskal-Wallis statistical power of 90 %).
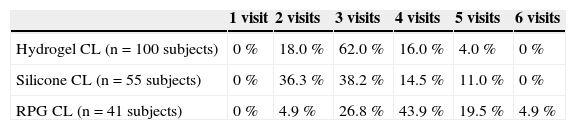
The minimum number of visits necessary to complete the fitting procedure was different between CL types (Table 1).
Number of visits necessary to complete the fitting procedure
| 1 visit | 2 visits | 3 visits | 4 visits | 5 visits | 6 visits | |
| Hydrogel CL (n=100 subjects) | 0 % | 18.0 % | 62.0 % | 16.0 % | 4.0 % | 0 % |
| Silicone CL (n=55 subjects) | 0 % | 36.3 % | 38.2 % | 14.5 % | 11.0 % | 0 % |
| RPG CL (n=41 subjects) | 0 % | 4.9 % | 26.8 % | 43.9 % | 19.5 % | 4.9 % |
The difference in the number of visits between spherical (mode and median of 3 visits, range 2–6) and toric (mode and median of 3 visits, range 2–5) lenses was not statistically significant (p=0.05 ANOVA Kruskal-Wallis, statistical power of 44 %). Patients fitted with toric soft CL required between 3 visits (63 % hydrogel and 36 % silicone hydrogel) and 4 visits (37 % hydrogel, 43 % silicone hydrogel) to complete the CL fitting.
No differences were found in the number of required visits between new (mode and median of 3 visits, range 2–5) and previous (mode and median of 3 visits, range 2–6) CL wearers (p=0.28 ANOVA Kruskal-Wallis).
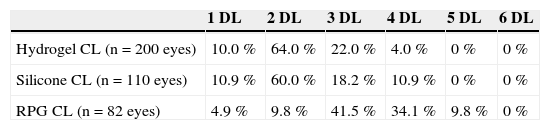
Number of diagnostic CLStatistical differences were found (p<0.001 ANOVA Kruskal-Wallis) between the number of DL necessary to fit RGP (mode and median of 3 lenses, range 1–5) when compared to traditional (mode and median of 2 lenses, range 1–4) or silicone (mode and median of 2 lenses, range 1–4) hydrogel CL. No differences were found between the number of DL required to fit traditional and silicone hydrogel CL (p=0.65 ANOVA Kruskal-Wallis).
The minimum number of DL required to complete the fitting procedure is summarized in Table 2.
No difference in the required number of DL was found between spherical (mode and median of 2 lenses, range 1–5) and toric (mode and median of 2 lenses, range 1–4) lenses (p=0.52 ANOVA Kruskal-Wallis, statistical power of 67 %). Also, the difference between new (mode and median of 2 lenses, range 1–5) and previous CL wearers (mode and median of 2 lenses, range 1–5) was not statistically significant (p=0.28 ANOVA Kruskal-Wallis).
DiscussionThis retrospective study analyzed the clinical history of 196 CL fittings (62.2 % non-CL wearers and 37.8 % previous CL wearers), in order to define the differences in the number of visits and the number of DL necessary to complete a CL fitting for daily wear in non-pathological eyes. To the best of our knowledge, little information and few studies have focused on this topic.
We included only refractive or cosmetic CL daily wearers because it is well known that patients with pathologies such as keratoconus or irregular cornea, as well as others requiring special CL (extended wear, after radial keratotomy, PRK, LASIK or other corneal refractive procedure, orthokeratology, etc.), need more visits and diagnostic DL.2,11,12,16,17 In the current study, the proportions of daily wear CL [79.1 % soft CL (51.0 % with hydrogel lenses and 28.0 % with silicone hydrogel lenses) and 20.9 % RGP] are in agreement with previous studies,18 which reported that 90 % of prescriptions were for daily wear soft CL with 29 % for silicone hydrogel lenses. The small proportion in the silicone hydrogel daily wear lenses prescription18 cannot account for the observed differences in the fitting procedure, because we did not find (p>0.05 ANOVA Kruskal-Wallis) differences in the number of required visits between hydrogel or silicone hydrogel lenses. Differences were also not found in the number of trial CL necessary to complete the CL fitting. This result must be interpreted with cautions, because we found a statistical power of only 44 %. For this reason, more research could be necessary with higher size sample, more centers and lens designs to confirm the absence of differences between the fitting procedure for spherical and toric lenses.
The non parametric description (mode, median and range) revealed that around than 3 visits were necessary to fit soft (hydrogel or silicone hydrogel) lenses and around than 4 visits were needed to fit RGP lenses. Fitting of RGP CL required statistically significantly more visits (mode and median of 4 visits) when compared to hydrogel (mode and median of 3 visits) or silicone hydrogel (mode and median of 3 visits) lenses. This difference (between RGP with soft CL) approximately represented a single visit.
We included two visits as the minimum number necessary to fit CL, because a successful lens fitting requires that the subjects can continue to wear the lenses after the first visit. The success rate, based on the physical fit alone in a single visit, is probably higher if the subjects wear the lenses over a longer period of time19 (we recommended approximately 3–4 weeks), because other factors such as physiological response, lens deposits, solution reactions, and others could affect the lens fit, comfort and anterior eye physiology.
The minimum number of visits required to complete the fitting procedure was different between soft (hydrogel and silicone hydrogel) and RGP CL (Table 1). The CL fit procedure described in our study permits lenses to be fitted with less than 3 visits for most of the soft CL patients (80 % and 74.5 % of hydrogel and silicone hydrogel lenses, respectively) and less than 4 visits for most (75.6 %) of the RPG patients.
The number of DL was similar between hydrogel and silicone hydrogel CL, but RGP fitting required more DL. Less than 3 diagnostic CL were required for fitting most of the soft CL patients (74 % and 70.9 % of hydrogel and silicone hydrogel, respectively) (Table 2). However, RGP CL fitting, on average, required slightly more DL (mode and median of 3 lenses) than hydrogel (mode and median of 2 lenses) or silicone hydrogel (mode and median of 2 lenses) lens fitting.
We found no differences (p=0.52) in the DL number between spherical and toric soft CL. Wong et al.19 found optimal fitting with one set of trial soft toric lenses in only 22 % of astigmatic Chinese eyes. The lens fit (centration, movement and rotation), patient vision and comfort were studied in a single session, and it was concluded that trial fitting is always useful before ordering toric lenses because the fitting of toric lenses is complex and there may be a combination of lens and patient factors that may affect the physical fit of the lens. Our results suggest that soft toric CL fitting it is not significantly different from soft spherical CL fitting in terms of the number of trial lenses required. This result must be confirmed with more research as had been commented previously.
Different guidelines for fitting CL from have been provided by different associations2–7 or manufacturers,8–10 but these guidelines do not define or estimate the number of visits or DL necessary to successfully complete the CL fitting. This information could be useful to novice practitioners and institutions concerned with the teaching and practice of CL fitting. Some manufacturers recommend patient examination after 24hours of daily wear,9 whereas others do not define a CL fit schedule8 and recommend following the practitioner's instructions. However, most of these guidelines do not use clinical evidence to generate recommendations.
According to Australian National Health and Medical Research Council recommendations,13 evidence-based clinical guidelines are based on randomized controlled trials (grade I or II), clinical studies (grade III), case series (grade IV) and meta-analyses of published research studies, rather than the consensus of expert panels. Therefore, the results of this study constitute grade IV clinical evidence. This clinical evidence could improve the available CL fitting guidelines and could be useful for informing patients and facilitating decisions. In addition, practitioners could improve the CL fitting procedure. For example, definition of the schedule and analysis of the cost of the CL fitting procedure could be performed using evidence-based information.13 The present results confirm the decreased cost and time consumption previously described.20
Finally, these results could be useful for defense of the provision of care in the event of a legal dispute. Daily wear of CL has been the most frequent cause for litigation brought against optometrists4 because CL wear is not innocuous to the eye. There are different sources of legal action in CL, with some related to negligence, failure to verify lenses and inadequate monitoring of ocular health.21,22 All of these issues are relevant to the topic of this study (number of DL and visits used to complete CL fitting).
In conclusion, this study presents clinical evidence (grade IV) about the number of visits and DL necessary for daily wear CL fitting. No differences were found between the fitting of hydrogel and silicone hydrogel lenses. RGP CL fitting required slightly more visits and DL. An estimated of three to four visits and two to three diagnostic lenses per eye are likely necessary to successfully fit daily wear CL in non-pathological eyes. These results of this study could be used to improve clinical guidelines for fitting of daily-wear CL and care of wearers. More research could be necessary improve the results of this study and to propose clinical evidence-based recommendations for fitting daily wear lenses.
Conflict of interestThe authors have no proprietary, financial or commercial interest in any material or method mentioned in this study.